Differential diagnosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Differential diagnosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Differential diagnosis US Medical PG Question 1: An 8-year-old girl is brought to the emergency department because of a 2-day history of low-grade fever, itchy rash, and generalized joint pain. The rash initially started in the antecubital and popliteal fossae and then spread to her trunk and distal extremities. One week ago, she was diagnosed with acute sinusitis and was started on amoxicillin. She has no history of adverse drug reactions and immunizations are up-to-date. Her temperature is 37.5°C (99.5°F), pulse is 90/min, and blood pressure is 110/70 mm Hg. Physical examination shows periorbital edema and multiple erythematous, annular plaques of variable sizes over her entire body. One of the lesions in the right popliteal fossa has an area of central clearing and the patient's mother reports that it has been present for over 24 hours. Urinalysis is normal. Which of the following is the most likely diagnosis?
- A. Stevens-Johnson syndrome
- B. Pemphigus vulgaris
- C. Drug reaction with eosinophilia and systemic symptoms
- D. Serum sickness-like reaction (Correct Answer)
- E. IgA vasculitis
Differential diagnosis Explanation: ***Serum sickness-like reaction***
- The patient's symptoms, including **low-grade fever, itchy rash (urticarial or morbilliform), generalized joint pain (arthralgia)**, and **periorbital edema**, developing about a week after starting **amoxicillin**, are classic for a serum sickness-like reaction. This reaction is often triggered by **beta-lactam antibiotics** in children.
- The presence of **annular plaques with central clearing** (targetoid lesions) and the 24-hour duration of lesions further supports this diagnosis, as these are common cutaneous manifestations.
*Stevens-Johnson syndrome*
- SJS is characterized by **extensive epidermal necrosis and detachment**, often involving **mucous membranes (oral, ocular, genital)**, which are not described in this patient.
- The rash in SJS typically consists of irregular, dusky red or purple macules and plaques with blistering, evolving into significant skin sloughing, unlike the described annular, itchy plaques.
*Pemphigus vulgaris*
- Pemphigus vulgaris is an **autoimmune blistering disease** causing flaccid bullae and erosions on the skin and mucous membranes. It is not associated with acute drug exposure.
- The patient's rash is described as itchy, erythematous, annular plaques, without mention of flaccid blisters or extensive erosions typical of pemphigus vulgaris.
*Drug reaction with eosinophilia and systemic symptoms*
- **DRESS syndrome** typically presents with a more severe and widespread morbilliform rash, often with **facial edema**, along with systemic symptoms such as **lymphadenopathy, hepatitis, nephritis, and eosinophilia**, which are not indicated in this case (normal urinalysis).
- The onset of DRESS syndrome is usually **2-6 weeks** after drug exposure, which is longer than the 1-week interval presented here.
*IgA vasculitis*
- **IgA vasculitis (Henoch-Schönlein purpura)** characteristically presents with **palpable purpura**, particularly on the lower extremities and buttocks, often accompanied by **arthralgia, abdominal pain, and renal involvement (hematuria/proteinuria)**.
- While arthritis and rash are present, the rash is described as erythematous, annular, and itchy, rather than the non-blanching palpable purpura typical of IgA vasculitis, and urinalysis is normal, ruling out renal involvement.
Differential diagnosis US Medical PG Question 2: A 9-year-old boy is brought to the emergency department because of progressively worsening shortness of breath for 3 days. He has had fever and malaise for the past 5 days. He had a sore throat 3 weeks ago that resolved without treatment. He appears ill. His temperature is 38.6°C (101.5°F), pulse is 98/min and blood pressure is 84/62 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 93%. Examination shows jugular venous distension and bilateral ankle edema. There are erythematous, ring-shaped macules and patches over his trunk that are well-demarcated. Auscultation of the chest shows crackles at the lung bases bilaterally. An S3 is heard on cardiac auscultation. His hemoglobin concentration is 12.2 g/dL, leukocyte count is 13,600/mm3, and platelet count is 280,000/mm3. A urinalysis is normal. An x-ray of the chest shows cardiac silhouette enlargement with prominent vascular markings in both the lung fields. Which of the following is the most likely etiology of this patient's symptoms?
- A. Systemic lupus erythematosus
- B. Acute rheumatic fever (Correct Answer)
- C. Kawasaki disease
- D. Viral myocarditis
- E. Infection with Borrelia burgdorferi
Differential diagnosis Explanation: ***Acute rheumatic fever***
- This patient presents with signs of cardiac involvement (**shortness of breath**, **S3 gallop**, **cardiomegaly**, **pulmonary edema**), a history of a recent **strep throat infection**, and **erythema marginatum** (the ring-shaped rash), all consistent with **acute rheumatic fever**.
- **Acute rheumatic fever** is a delayed, non-suppurative complication of Group A Streptococcus pharyngitis, leading to systemic inflammation, particularly affecting the heart, joints, brain, and skin.
*Systemic lupus erythematosus*
- SLE can cause cardiac complications like pericarditis or myocarditis, but the characteristic rash of SLE (malar or discoid) differs from the described **erythema marginatum**.
- While SLE can cause systemic symptoms, the clear history of a preceding **sore throat** and the specific rash point away from SLE.
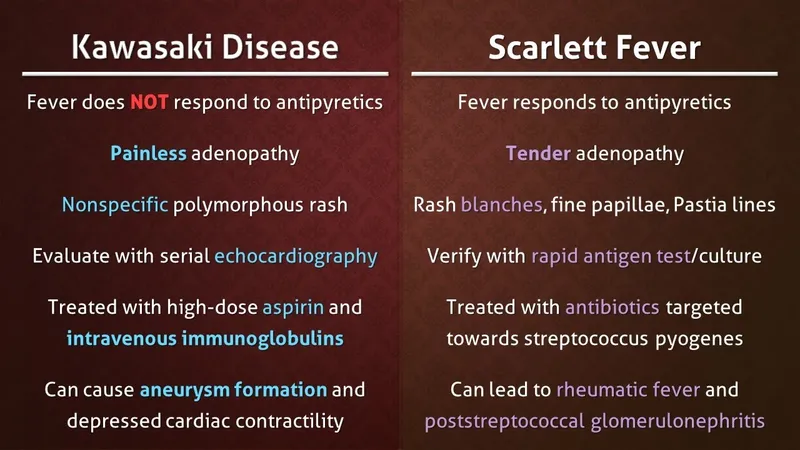
*Kawasaki disease*
- Kawasaki disease primarily affects **children under 5 years old** and is characterized by fever, conjunctivitis, oral changes, rash, lymphadenopathy, and extreme irritability.
- The patient's age (9 years) and the specific rash described (erythema marginatum) are not typical for Kawasaki disease.
*Viral myocarditis*
- Viral myocarditis can cause **heart failure** symptoms (shortness of breath, S3, cardiomegaly), but it typically lacks the preceding **sore throat** and the specific skin findings of **erythema marginatum** seen in this patient.
- While a viral infection could cause myocarditis, the constellation of symptoms points strongly to a specific post-streptococcal etiology.
*Infection with Borrelia burgdorferi*
- *Borrelia burgdorferi* (Lyme disease) can cause cardiac manifestations like **carditis** (often AV block) and a characteristic rash called **erythema migrans**.
- However, **erythema migrans** is typically a single, expanding bull's-eye rash, which is different from the described **erythematous, ring-shaped macules and patches** of erythema marginatum.
Differential diagnosis US Medical PG Question 3: A previously healthy 4-year-old boy is brought to the physician by his parents because he has had a fever, diffuse joint pain, and a rash on his abdomen for the past week. Acetaminophen did not improve his symptoms. He emigrated from China with his family 2 years ago. He attends daycare. His immunization records are not available. His temperature is 38.5°C (101.3°F), pulse is 125/min, and blood pressure is 100/60 mm Hg. Examination shows polymorphous truncal rash. The eyes are pink with no exudate. The tongue is shiny and red, and the lips are cracked. The hands and feet are red and swollen. There is right-sided anterior cervical lymphadenopathy. Which of the following is the most appropriate next step in management?
- A. HHV-6 immunoglobulin M (IgM) detection
- B. ANA measurement
- C. Echocardiography (Correct Answer)
- D. Monospot test
- E. Antistreptolysin O titer measurement
Differential diagnosis Explanation: ***Echocardiography***
- This patient presents with classic symptoms of **Kawasaki disease**, including protracted fever (>5 days), polymorphous rash, conjunctival injection, cracked lips and red tongue (**strawberry tongue**), swollen hands and feet, and cervical lymphadenopathy.
- The diagnosis can be made clinically when fever ≥5 days plus ≥4 of 5 principal criteria are present, which this patient meets.
- **Echocardiography** is essential to establish a **baseline cardiac assessment** and screen for **coronary artery aneurysms**, which occur in 15-25% of untreated patients.
- Among the diagnostic options listed, echocardiography is the most appropriate next step, though in clinical practice, **treatment with IVIG and high-dose aspirin should be initiated promptly** (ideally within 10 days of fever onset) and should not be delayed pending echocardiography results.
*HHV-6 immunoglobulin M (IgM) detection*
- **Human Herpesvirus 6 (HHV-6)** causes **roseola infantum** (exanthem subitum), which presents with high fever for 3-5 days followed by a rash that appears **as the fever resolves**.
- The mucocutaneous findings in this case (strawberry tongue, cracked lips, conjunctival injection, extremity swelling) are not consistent with roseola.
*ANA measurement*
- **Antinuclear antibody (ANA)** testing screens for **autoimmune diseases** such as systemic lupus erythematosus or juvenile idiopathic arthritis.
- While this patient has fever and joint pain, the specific mucocutaneous changes (strawberry tongue, cracked lips, conjunctival injection, polymorphous rash, extremity edema) and cervical lymphadenopathy are pathognomonic for Kawasaki disease, not typical autoimmune conditions.
*Monospot test*
- The **Monospot test** diagnoses **infectious mononucleosis** caused by **Epstein-Barr virus (EBV)**.
- While EBV can cause fever, rash, and lymphadenopathy (typically posterior cervical), the characteristic mucocutaneous findings of Kawasaki disease (strawberry tongue, cracked lips, conjunctival injection without exudate, extremity changes) are not seen in mononucleosis.
- Additionally, mononucleosis is uncommon in preschool-aged children.
*Antistreptolysin O titer measurement*
- **Antistreptolysin O (ASO) titer** detects recent **Group A Streptococcus** infection and can support a diagnosis of **acute rheumatic fever (ARF)**.
- ARF presents with migratory polyarthritis, carditis, and **erythema marginatum** (not a polymorphous rash), occurring 2-4 weeks after streptococcal pharyngitis.
- The mucocutaneous features in this case are specific to Kawasaki disease and not consistent with ARF.
Differential diagnosis US Medical PG Question 4: A 2-year-old boy presents to the pediatrician for evaluation of an elevated temperature, sore throat, runny nose, and lacrimation for the past week, and a rash which he developed yesterday. The rash began on the patient’s face and spread down to the trunk, hands, and feet. The patient’s mother gave him ibuprofen to control the fever. The child has not received mumps, measles, and rubella vaccinations because he was ill when the vaccine was scheduled and was later lost to follow-up. The vital signs include blood pressure 90/50 mm Hg, heart rate 110/min, respiratory rate 22/min, and temperature 37.8°C (100.0℉). On physical examination, the child was drowsy. His face, trunk, and extremities were covered with a maculopapular erythematous rash. Two irregularly-shaped red dots were also noted on the mucosa of the lower lip. The remainder of the physical examination was within normal limits. What is the probable causative agent for this child’s condition?
- A. Group A Streptococcus
- B. Rubulavirus
- C. Influenzavirus
- D. Morbillivirus (Correct Answer)
- E. Herpesvirus
Differential diagnosis Explanation: ***Morbillivirus***
- The constellation of symptoms—**elevated temperature**, **sore throat**, **runny nose**, **lacrimation**, a **maculopapular erythematous rash** that began on the face and spread downward, and especially the **irregularly-shaped red dots on the mucosa of the lower lip** (likely **Koplik spots**)—are classic for **measles**, caused by Morbillivirus.
- The patient's **unvaccinated status** against MMR further supports measles as the most probable diagnosis, as it is a highly contagious disease prevented by vaccination.
*Group A Streptococcus*
- This bacterium causes **scarlet fever**, characterized by a **sandpaper-like rash** and **strawberry tongue**, not a maculopapular rash spreading from face to extremities with Koplik spots.
- While it can cause pharyngitis and fever, the specific rash progression and oral lesions rule out Group A Streptococcus.
*Rubulavirus*
- Rubulavirus causes **mumps**, which primarily presents with **parotitis** (swelling of parotid glands), fever, and headache.
- It does not typically cause a generalized maculopapular rash or Koplik spots, making it an unlikely cause for the described symptoms.
*Influenzavirus*
- Influenzavirus causes **influenza**, characterized by sudden onset of high fever, cough, myalgia, and headache.
- While it can cause fever and respiratory symptoms, it does not typically present with a widespread maculopapular rash or Koplik spots.
*Herpesvirus*
- Herpesviruses cause a variety of conditions, including **chickenpox** (Varicella-zoster virus), which presents with **vesicular lesions** that crust over, and **roseola infantum** (HHV-6/7), which primarily causes a high fever followed by a non-pruritic rash appearing *after* the fever subsides.
- Neither of these typically presents with Koplik spots or the specific maculopapular rash progression described.
Differential diagnosis US Medical PG Question 5: A 3-year-old boy presents to the emergency department with a fever and a rash. This morning the patient was irritable and had a fever which gradually worsened throughout the day. He also developed a rash prior to presentation. He was previously healthy and is not currently taking any medications. His temperature is 102.0°F (38.9°C), blood pressure is 90/50 mmHg, pulse is 160/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for a scarlatiniform rash with flaccid blisters that rupture easily, covering more than 60% of the patient’s body surface. The lesions surround the mouth but do not affect the mucosa, and palpation of the rash is painful. Which of the following is the most likely diagnosis?
- A. Staphylococcal scalded skin syndrome (Correct Answer)
- B. Toxic epidermal necrolysis
- C. Toxic shock syndrome
- D. Urticaria
- E. Stevens Johnson syndrome
Differential diagnosis Explanation: ***Staphylococcal scalded skin syndrome***
- The presentation of a **fever**, **irritability**, and a **scarlatiniform rash with flaccid blisters** that rupture easily, especially with painful lesions and perioral involvement without mucosal lesions, is highly characteristic of **Staphylococcal scalded skin syndrome (SSSS)**.
- SSSS is caused by **exfoliative toxins** produced by *Staphylococcus aureus*, which target **desmoglein-1** in the skin, leading to widespread superficial blistering and epidermal sloughing.
*Toxic epidermal necrolysis*
- **Toxic epidermal necrolysis (TEN)** is a severe mucocutaneous reaction often triggered by **medications**, characterized by widespread **epidermal detachment (>30% BSA)** and **mucosal involvement**.
- TEN typically presents with full-thickness epidermal necrosis and severe systemic symptoms, often after drug exposure, which is not noted in this previously healthy, non-medicated child.
*Toxic shock syndrome*
- **Toxic shock syndrome (TSS)** is characterized by **fever**, **hypotension**, **diffuse erythematous rash**, and **multisystem organ dysfunction**.
- While a rash and fever are present, the hallmark **flaccid blistering** and **skin peeling** seen in SSSS is not typical for TSS; TSS rash is more often a blanching erythroderma.
*Urticaria*
- **Urticaria (hives)** presents as **pruritic, transient, raised erythematous wheals** that blanch with pressure.
- The rash in this patient is described as **scarlatiniform with flaccid blisters** and is painful, which is inconsistent with the typical appearance and symptoms of urticaria.
*Stevens Johnson syndrome*
- **Stevens-Johnson syndrome (SJS)** is a severe adverse drug reaction, similar to TEN but with less extensive skin involvement (**<10% BSA**), and is characterized by **erythematous macules**, **targetoid lesions**, and **mucosal involvement**.
- While blistering can occur, the widespread, painful, easily rupturing flaccid blisters without specific target lesions and prominent perioral involvement (without mucosal affection) point more strongly to SSSS over SJS.
Differential diagnosis US Medical PG Question 6: A 7-year-old boy comes to the physician because of a generalized rash for 3 days. Over the past 5 days, he has also had a high fever and a sore throat. His 16-year-old sister was treated for infectious mononucleosis 2 weeks ago. He returned from a summer camp a week ago. His immunizations are up-to-date. Three years ago, he required intubation after an allergic reaction to dicloxacillin. The patient appears ill. His temperature is 38.2°C (100.8°F). Examination shows circumferential oral pallor. Cervical lymphadenopathy is present. There is tonsillar erythema and exudate. A confluent, blanching, punctate erythematous rash with a rough texture is spread over his trunk and extremities. His hemoglobin concentration is 13.3 g/dL, leukocyte count is 12,000/mm3, and erythrocyte sedimentation rate is 43 mm/h. Which of the following is the most appropriate next step in management?
- A. Amoxicillin therapy
- B. Doxycycline therapy
- C. Azithromycin therapy (Correct Answer)
- D. Cephalexin therapy
- E. Acyclovir therapy
Differential diagnosis Explanation: ***Azithromycin therapy***
- This patient presents with symptoms highly suggestive of **streptococcal pharyngitis** (sore throat, fever, tonsillar exudates, cervical lymphadenopathy) complicated by **scarlet fever** (confluent, blanching, punctate erythematous rash with a rough texture, circumferential oral pallor).
- Given his **history of severe allergic reaction (intubation) to dicloxacillin**, a penicillin-class antibiotic, azithromycin (a macrolide) is the appropriate choice for treating **Group A Streptococcus** (GAS) infection in a penicillin-allergic patient.
*Amoxicillin therapy*
- **Amoxicillin** is a penicillin-class antibiotic and is **contraindicated** due to the patient's severe allergic reaction (intubation) to dicloxacillin, another penicillin.
- Cross-reactivity between penicillins, especially in severe allergic reactions, is a significant concern, making this an unsafe choice.
*Doxycycline therapy*
- **Doxycycline**, a tetracycline, is not a first-line treatment for **streptococcal pharyngitis** and is primarily used for atypical bacterial infections or in specific cases of penicillin allergy where other agents are not suitable.
- While it has some activity against GAS, macrolides like azithromycin are preferred alternatives for penicillin-allergic patients.
*Cephalexin therapy*
- **Cephalexin** is a first-generation cephalosporin, and while it can be used for GAS, roughly 5-10% of patients with a penicillin allergy may have a **cross-reaction** to cephalosporins, especially with a history of severe reactions.
- Therefore, it is generally avoided in patients with a history of anaphylaxis or other severe reactions to penicillin.
*Acyclovir therapy*
- **Acyclovir** is an antiviral medication used to treat herpes simplex and varicella-zoster virus infections.
- The patient's symptoms (pharyngitis, rash consistent with scarlet fever) are indicative of a **bacterial infection (GAS)**, not a viral infection that would respond to acyclovir.
Differential diagnosis US Medical PG Question 7: A previously healthy 4-year-old boy is brought to the physician because of blisters and redness on his neck and chest for 2 days. He has also had a fever. He is lethargic and has not eaten well since the rash appeared. He has not had coughing, wheezing, or dysuria. He is an only child and there is no family history of serious illness. His immunizations are up-to-date. His temperature is 38.9°C (102°F), pulse is 90/min, and blood pressure is 80/40 mm Hg. Examination shows flaccid blisters over his neck and trunk that rupture easily. Areas of erythematous moist skin are also noted. Twirling an eraser over the trunk results in a blister. Oropharyngeal examination is normal. Laboratory studies show:
Hemoglobin 12 g/dL
Leukocyte count 22,000/mm3
Segmented neutrophils 77%
Eosinophils 3%
Lymphocytes 18%
Monocytes 2%
Erythrocyte sedimentation rate 60 mm/h
Urinalysis is normal. Which of the following is the most likely diagnosis?
- A. Staphylococcal scalded skin syndrome (Correct Answer)
- B. Bullous pemphigoid
- C. Pemphigus vulgaris
- D. Scarlet fever
- E. Toxic epidermal necrolysis
Differential diagnosis Explanation: ***Staphylococcal scalded skin syndrome***
- The presented symptoms, including **fever**, generalized **blisters** that rupture easily (Nikolsky sign positive, evidenced by "twirling an eraser over the trunk results in a blister"), and **erythematous moist skin**, in a young child are classic for **Staphylococcal scalded skin syndrome** (SSSS).
- SSSS is caused by **exfoliative toxins** produced by *Staphylococcus aureus*, leading to epidermal splitting within the granular layer.
*Bullous pemphigoid*
- This is an **autoimmune blistering disease** that typically affects **elderly individuals** with tense bullae, unlike the flaccid blisters seen here.
- The disease mechanism involves autoantibodies against **hemidesmosomes**, causing subepidermal blistering.
*Pemphigus vulgaris*
- Pemphigus vulgaris is another **autoimmune blistering disease** characterized by **flaccid blisters** and often presents with **oral lesions**, but it typically affects **middle-aged adults**.
- The pathophysiology involves autoantibodies targeting **desmoglein 1 and 3**, leading to intraepidermal blistering above the basal layer.
*Scarlet fever*
- Scarlet fever is caused by **Streptococcus pyogenes** and presents with a characteristic **fine, sandpaper-like rash**, not blisters.
- Other features include a **strawberry tongue** and **pharyngitis**, which are not described in this patient.
*Toxic epidermal necrolysis*
- Toxic epidermal necrolysis (TEN) is a **severe, life-threatening drug-induced reaction** characterized by widespread epidermal detachment (>30% body surface area) and often involves mucous membranes.
- While it causes blistering and epidermal sloughing, it is distinct from SSSS in its **etiology (usually drug-related)**, **older patient population**, and **histological level of cleavage** (dermal-epidermal junction).
Differential diagnosis US Medical PG Question 8: A 6-year-old girl is brought to the physician because of a generalized pruritic rash for 3 days. Her mother has noticed fluid oozing from some of the lesions. She was born at term and has been healthy except for an episode of bronchitis 4 months ago that was treated with azithromycin. There is no family history of serious illness. Her immunization records are unavailable. She attends elementary school but has missed the last 5 days. She appears healthy. Her temperature is 38°C (100.4°F). Examination shows a maculopapular rash with crusted lesions and vesicles over the entire integument, including the scalp. Her hemoglobin concentration is 13.1 g/dL, leukocyte count is 9800/mm3, and platelet count is 319,000/mm3. Which of the following is the most appropriate next best step?
- A. Vitamin A therapy
- B. Measles IgM titer
- C. Calamine lotion (Correct Answer)
- D. Rapid strep test
- E. Tzanck test
Differential diagnosis Explanation: ***Calamine lotion***
- The clinical presentation with **vesicles, crusted lesions, and maculopapular rash** in different stages of evolution, along with **pruritus, low-grade fever**, and **exposure history** (missed school days), is **pathognomonic for varicella (chickenpox)**.
- **Diagnosis is clinical** and does not require laboratory confirmation in uncomplicated cases.
- The most appropriate next step is **symptomatic management** with **calamine lotion** to relieve pruritus and prevent secondary bacterial infection from scratching.
- Other supportive measures include antihistamines, acetaminophen for fever (avoid aspirin due to Reye syndrome risk), and keeping nails trimmed.
- **Acyclovir** may be considered if seen within 24 hours of rash onset or in high-risk patients, but this patient presents on day 3 with uncomplicated disease.
*Tzanck test*
- A **Tzanck test** can identify multinucleated giant cells in herpes virus infections, but it is **not routinely needed** for clinical varicella diagnosis.
- This test is **outdated** and has largely been replaced by PCR or direct fluorescent antibody (DFA) testing when laboratory confirmation is required.
- Laboratory confirmation would only be necessary in **atypical presentations, immunocompromised patients, or outbreak investigations**—none of which apply here.
*Vitamin A therapy*
- **Vitamin A** is indicated for **measles** to reduce morbidity and mortality, especially in malnourished or vitamin A-deficient children.
- Measles presents with **Koplik spots**, cough, coryza, conjunctivitis (3 C's), and a maculopapular rash that starts on the face and spreads caudally—**without vesicles**.
- This patient's vesicular rash in multiple stages is not consistent with measles.
*Measles IgM titer*
- While measles can present with fever and rash, the **vesicular and crusted lesions** are pathognomonic for varicella, not measles.
- Measles typically has a **confluent maculopapular rash** without vesicles, along with the classic prodrome of cough, coryza, and conjunctivitis.
- Serologic testing would delay management and is unnecessary given the classic varicella presentation.
*Rapid strep test*
- A **rapid strep test** diagnoses **Group A Streptococcal pharyngitis**, which presents with **sore throat, fever, tonsillar exudates**, and sometimes a **scarlatiniform (sandpaper-like) rash**.
- Scarlet fever rash is erythematous and blanching, not vesicular, and typically spares the face while being prominent in skin folds.
- The generalized pruritic vesicular rash makes streptococcal infection highly unlikely.
Differential diagnosis US Medical PG Question 9: A 10-year-old girl with a rash is brought to the clinic by her mother. The patient’s mother says that the onset of the rash occurred 2 days ago. The rash was itchy, red, and initially localized to the cheeks with circumoral pallor, and it gradually spread to the arms and trunk. The patient’s mother also says her daughter had been reporting a high fever of 39.4°C (102.9°F), headaches, myalgia, and flu-like symptoms about a week ago, which resolved in 2 days with acetaminophen. The patient has no significant past medical history. Her vital signs include: temperature 37.0°C (98.6°F), pulse 90/min, blood pressure 125/85 mm Hg, respiratory rate 20/min. Physical examination shows a symmetric erythematous maculopapular rash on both cheeks with circumoral pallor, which extends to the patient’s trunk, arms, and buttocks. The remainder of the exam is unremarkable. Laboratory findings are significant for a leukocyte count of 7,100/mm3 and platelet count of 325,000/mm3. Which of the following is the next best step in the management of this patient?
- A. Administer intravenous immunoglobulin (IVIG)
- B. Discharge home, saying that the patient may return to school after the disappearance of the rash
- C. Transfuse with whole blood
- D. Discharge home with instructions for strict isolation from pregnant women until disappearance of the rash
- E. Discharge home, saying that the patient may immediately return to school (Correct Answer)
Differential diagnosis Explanation: ***Discharge home, saying that the patient may immediately return to school***
- This patient likely has **Fifth Disease (Erythema Infectiosum)**, caused by **Parvovirus B19**, characterized by a **"slapped cheek" rash** and a **lacy, reticular rash** on the trunk and extremities.
- Patients with Fifth Disease are **contagious before the rash appears** and are generally **no longer contagious once the rash develops**, making immediate return to school safe.
*Administer intravenous immunoglobulin (IVIG)*
- **IVIG** is typically reserved for **severe cases of Parvovirus B19 infection** in immunocompromised individuals or those with chronic hemolytic anemias who develop **aplastic crisis**.
- The patient's symptoms are mild and self-limiting, without evidence of severe complications like aplastic anemia (normal leukocyte and platelet counts).
*Discharge home, saying that the patient may return to school after the disappearance of the rash*
- This advice is incorrect because the patient is **no longer contagious once the rash erupts**.
- Requiring isolation until the rash disappears would be unnecessarily disruptive and is not medically indicated for Fifth Disease.
*Transfuse with whole blood*
- **Whole blood transfusion** is not indicated for uncomplicated Fifth Disease, as it can cause significant complications.
- Transfusions are considered only in cases of **severe aplastic crisis** with significant anemia, which is not present in this patient (normal complete blood count).
*Discharge home with instructions for strict isolation from pregnant women until disappearance of the rash*
- While exposure to **Parvovirus B19 in pregnant women** can lead to significant fetal complications (e.g., hydrops fetalis), the patient is **no longer infectious once the rash appears**.
- Therefore, strict isolation from pregnant women **after rash onset** is not necessary, as the risk of transmission has passed.
Differential diagnosis US Medical PG Question 10: A new mother brings in her 4-week-old son who has no significant past medical history but she complains of a new, itchy rash on his body. The patient has an older sister who developed similar symptoms when she was around the same age. The patient's blood pressure is 75/50 mm Hg, pulse is 140/min, respiratory rate is 40/min, and temperature is 37.3°C (99.1°F). Physical examination reveals confluent, erythematous patches and plaques with tiny vesicles and scaling overlying his lower back and abdomen. When questioned about possible etiologies, the mother notes that she has been bathing the patient at least twice a day. Which of the following statements is most appropriate for this patient?
- A. Usually, scabs with a distinctive yellow, gold, or brown crust are seen.
- B. This condition is usually seen on the scalp, face, ears, and neck.
- C. Hot baths that are too long, or too frequent, can dry out the skin. (Correct Answer)
- D. You can expect blisters, fever and large areas of skin that peel or fall away.
- E. This condition is caused by the herpes simplex virus.
Differential diagnosis Explanation: ***Hot baths that are too long, or too frequent, can dry out the skin.***
- The rash described (confluent, erythematous patches and plaques with tiny vesicles and scaling) on a 4-week-old, along with a history of an older sibling with similar symptoms, is highly suggestive of **atopic dermatitis** (eczema).
- Frequent, prolonged hot baths **strip the skin of its natural oils**, exacerbating skin dryness and disrupting the skin barrier, a known trigger for atopic dermatitis flares in infants.
- Given the mother's history of bathing twice daily, counseling about appropriate bathing frequency is the most relevant management advice.
*Usually, scabs with a distinctive yellow, gold, or brown crust are seen.*
- **Yellow, gold, or brown crusts** are characteristic of **impetigo**, a bacterial skin infection, not typically seen as the primary presentation of atopic dermatitis.
- While eczema can become secondarily infected with bacteria (impetiginization), these crusts are not the defining feature of uncomplicated eczema.
*This condition is usually seen on the scalp, face, ears, and neck.*
- While this describes the typical distribution of **seborrheic dermatitis** (cradle cap) in infants, atopic dermatitis in young infants commonly affects the **face (especially cheeks) and extensor surfaces**.
- In this case, the presentation on the lower back and abdomen, while somewhat atypical, is consistent with atopic dermatitis, especially given the family history and identified trigger factor.
*You can expect blisters, fever and large areas of skin that peel or fall away.*
- The description of **blisters, fever, and large areas of peeling skin** is characteristic of severe conditions like **Stevens-Johnson syndrome (SJS)** or **Toxic Epidermal Necrolysis (TEN)**, which are much more severe and life-threatening.
- The rash described in this patient does not indicate such a severe systemic reaction and is consistent with uncomplicated infantile atopic dermatitis.
*This condition is caused by the herpes simplex virus.*
- The herpes simplex virus causes **herpes simplex** infections, which manifest as clustered vesicles on an erythematous base (e.g., eczema herpeticum when it complicates atopic dermatitis).
- **Atopic dermatitis** is a chronic inflammatory skin condition with genetic predisposition and environmental triggers, not a primary viral infection.
More Differential diagnosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.