Diagnostic criteria and clinical features US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diagnostic criteria and clinical features. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diagnostic criteria and clinical features US Medical PG Question 1: A 46-year-old woman presents to your medical office complaining of ‘feeling tired’. The patient states that she has been having some trouble eating because her ‘tongue hurts’, but she has no other complaints. On examination, the patient has pale conjunctiva and skin and also appears tired. She has a smooth, red tongue that is tender to touch with a tongue depressor. The patient’s hands and feet feel cold. Fluoroscopic evaluation of the swallowing mechanism and esophagus is normal. Which of the following diagnoses is most likely?
- A. Herpes simplex virus-1 infection
- B. Oral candidiasis infection
- C. Kawasaki disease
- D. Pernicious anemia (Correct Answer)
- E. Plummer-Vinson syndrome
Diagnostic criteria and clinical features Explanation: ***Pernicious anemia***
- The symptoms, including **fatigue**, **pale conjunctiva and skin**, **smooth red tongue (atrophic glossitis)**, and cold extremities, are classic manifestations of **vitamin B12 deficiency**, often caused by pernicious anemia.
- Pernicious anemia results from impaired absorption of vitamin B12 due to a lack of **intrinsic factor**, leading to **megaloblastic anemia** with neurological symptoms often observed in later stages.
*Herpes simplex virus-1 infection*
- HSV-1 typically causes **oral lesions** like cold sores or fever blisters, which are usually painful vesicles and ulcers, not a diffuse smooth, red tongue.
- While it can cause oral discomfort, it does not explain the systemic symptoms of **fatigue** and **pallor** suggestive of anemia.
*Oral candidiasis infection*
- Oral candidiasis (thrush) presents as **white, creamy patches** on the tongue and oral mucosa that can be scraped off, often associated with immunocompromise.
- This presentation does not match the **smooth, red tongue** described, nor does it typically cause profound systemic fatigue and pallor in an otherwise healthy adult.
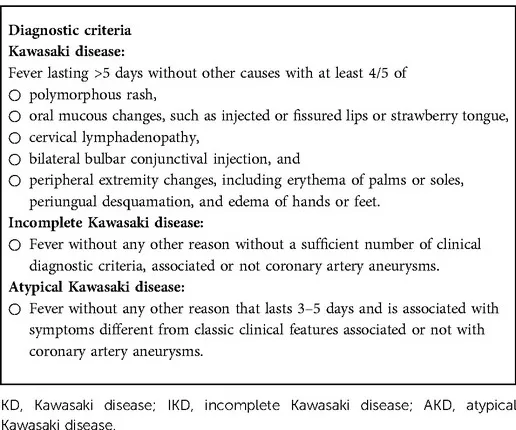
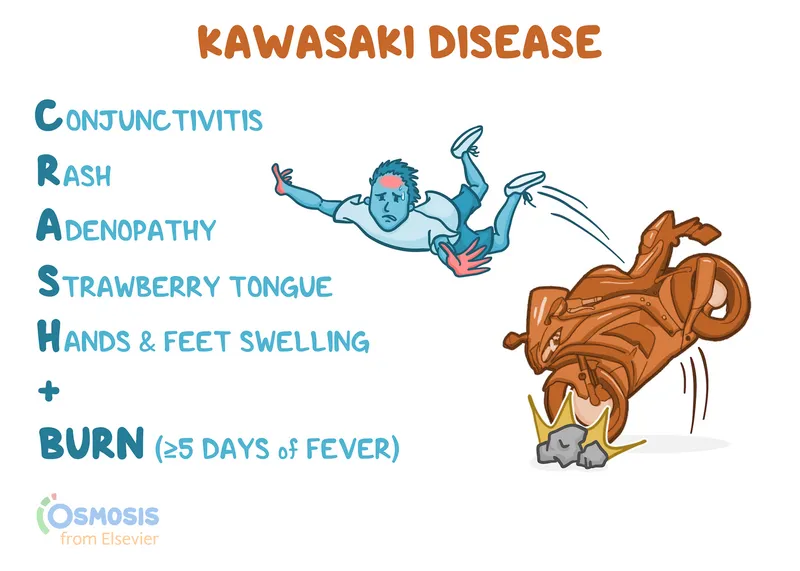
*Kawasaki disease*
- Kawasaki disease is a **vasculitis primarily affecting children**, characterized by fever, conjunctivitis, rash, lymphadenopathy, and a **strawberry tongue**.
- It is highly unlikely in a 46-year-old woman and does not manifest with the **pale skin** or classic presentation of **pernicious anemia**.
*Plummer-Vinson syndrome*
- Plummer-Vinson syndrome is characterized by the triad of **iron deficiency anemia**, **dysphagia** (due to esophageal webs), and **glossitis**.
- While glossitis and anemia are present, the history notes **normal fluoroscopic evaluation of the swallowing mechanism and esophagus**, ruling out esophageal webs, which are a hallmark of Plummer-Vinson syndrome.
Diagnostic criteria and clinical features US Medical PG Question 2: A 4-year-old boy is brought to the emergency department by his mother with a rash on his trunk, malaise, and fever with spikes up to 38.5°C (101.3°F) for the past 2 weeks. The patient's mother says she tried giving him Tylenol with little improvement. Past medical history includes a spontaneous vaginal delivery at full term. The patient's vaccines are up-to-date and he has met all developmental milestones. On physical examination, his lips are cracking, and he has painful cervical lymphadenopathy. The rash is morbilliform and involves his trunk, palms, and the soles of his feet. There is fine desquamation of the skin of the perianal region. Which of the following anatomical structures is most important to screen for possible complications in this patient?
- A. Mitral valve
- B. Kidneys
- C. Gallbladder
- D. Coronary artery (Correct Answer)
- E. Pylorus
Diagnostic criteria and clinical features Explanation: ***Coronary artery***
- The constellation of symptoms, including prolonged fever, rash on trunk, palms, and soles, cracked lips, cervical lymphadenopathy, and perianal desquamation, is highly indicative of **Kawasaki disease**.
- **Coronary artery aneurysms** are the most serious complication of Kawasaki disease, occurring in 15-25% of untreated children, necessitating close monitoring and screening.
*Mitral valve*
- While other forms of vasculitis or rheumatic fever can affect heart valves, **mitral valve** involvement is not a primary or characteristic complication of Kawasaki disease.
- The main cardiac concern in Kawasaki disease is direct arterial inflammation, not valvular dysfunction.
*Kidneys*
- **Renal involvement**, such as acute kidney injury, is not a typical or prominent feature of Kawasaki disease.
- Kawasaki disease primarily targets medium-sized muscular arteries throughout the body, with a predilection for the coronary arteries.
*Gallbladder*
- **Hydrops of the gallbladder** can occur in Kawasaki disease, leading to acute cholecystitis-like symptoms, but it is generally a self-limiting complication.
- While it's a potential finding, it is not as life-threatening or essential to screen for as coronary artery complications.
*Pylorus*
- There is no direct association between Kawasaki disease and primary involvement or complications of the **pylorus**.
- Gastrointestinal symptoms can occur, but these are typically non-specific and do not involve anatomical changes to the pylorus.
Diagnostic criteria and clinical features US Medical PG Question 3: A 5-year-old boy is brought to the emergency department for evaluation of a progressive rash that started 2 days ago. The rash began on the face and progressed to the trunk and extremities. Over the past week, he has had a runny nose, a cough, and red, crusty eyes. He immigrated with his family from Turkey 3 months ago. His father and his older brother have Behcet disease. Immunization records are unavailable. The patient appears irritable and cries during the examination. His temperature is 40.0°C (104°F). Examination shows general lymphadenopathy and dry mucous membranes. Skin turgor is decreased. There is a blanching, partially confluent erythematous maculopapular exanthema. Examination of the oral cavity shows small white spots with erythematous halos on the buccal mucosa. His hemoglobin concentration is 11.5 g/dL, leukocyte count is 6,000/mm3, and platelet count is 215,000/mm3. Serology confirms the diagnosis. Which of the following is the most appropriate next step in management?
- A. Oral acyclovir
- B. Oral penicillin V
- C. Reassurance and follow-up in 3 days
- D. Vitamin A supplementation (Correct Answer)
- E. Intravenous immunoglobulin (IVIG)
Diagnostic criteria and clinical features Explanation: ***Vitamin A supplementation***
- The patient's symptoms (fever, rash, cough, conjunctivitis, oral ulcers, progressive rash starting on face) coupled with a history of recent immigration and unconfirmed immunization status are highly suggestive of **measles**.
- **Vitamin A supplementation** is recommended for all children with measles, especially in settings with a high prevalence of vitamin A deficiency or in patients with complicated measles, as it reduces morbidity and mortality.
*Oral acyclovir*
- **Acyclovir** is an antiviral medication used primarily for **herpes simplex virus (HSV)** or **varicella-zoster virus (VZV)** infections.
- The clinical presentation with a **maculopapular rash** and lack of vesicular lesions makes HSV or VZV unlikely.
*Oral penicillin V*
- **Penicillin V** is an antibiotic used to treat bacterial infections, such as streptococcal pharyngitis.
- The patient's symptoms are consistent with a viral illness (**measles**), making antibiotic treatment inappropriate.
*Reassurance and follow-up in 3 days*
- Given the high fever, dehydration, irritability, and the potential for serious complications of **measles** (e.g., pneumonia, encephalitis), simple reassurance and delayed follow-up are insufficient.
- The patient requires immediate medical intervention and supportive care.
*Intravenous immunoglobulin (IVIG)*
- **IVIG** is used for certain severe infections or autoimmune conditions, or to provide passive immunity (e.g., post-exposure prophylaxis for measles in susceptible high-risk individuals).
- While IVIG might be considered for measles post-exposure prophylaxis in unimmunized, immunocompromised individuals, it is not the primary treatment for active measles infection, nor is it a standard supportive measure like Vitamin A.
Diagnostic criteria and clinical features US Medical PG Question 4: A 6-year-old girl is brought to the physician because of a generalized pruritic rash for 3 days. Her mother has noticed fluid oozing from some of the lesions. She was born at term and has been healthy except for an episode of bronchitis 4 months ago that was treated with azithromycin. There is no family history of serious illness. Her immunization records are unavailable. She attends elementary school but has missed the last 5 days. She appears healthy. Her temperature is 38°C (100.4°F). Examination shows a maculopapular rash with crusted lesions and vesicles over the entire integument, including the scalp. Her hemoglobin concentration is 13.1 g/dL, leukocyte count is 9800/mm3, and platelet count is 319,000/mm3. Which of the following is the most appropriate next best step?
- A. Vitamin A therapy
- B. Measles IgM titer
- C. Calamine lotion (Correct Answer)
- D. Rapid strep test
- E. Tzanck test
Diagnostic criteria and clinical features Explanation: ***Calamine lotion***
- The clinical presentation with **vesicles, crusted lesions, and maculopapular rash** in different stages of evolution, along with **pruritus, low-grade fever**, and **exposure history** (missed school days), is **pathognomonic for varicella (chickenpox)**.
- **Diagnosis is clinical** and does not require laboratory confirmation in uncomplicated cases.
- The most appropriate next step is **symptomatic management** with **calamine lotion** to relieve pruritus and prevent secondary bacterial infection from scratching.
- Other supportive measures include antihistamines, acetaminophen for fever (avoid aspirin due to Reye syndrome risk), and keeping nails trimmed.
- **Acyclovir** may be considered if seen within 24 hours of rash onset or in high-risk patients, but this patient presents on day 3 with uncomplicated disease.
*Tzanck test*
- A **Tzanck test** can identify multinucleated giant cells in herpes virus infections, but it is **not routinely needed** for clinical varicella diagnosis.
- This test is **outdated** and has largely been replaced by PCR or direct fluorescent antibody (DFA) testing when laboratory confirmation is required.
- Laboratory confirmation would only be necessary in **atypical presentations, immunocompromised patients, or outbreak investigations**—none of which apply here.
*Vitamin A therapy*
- **Vitamin A** is indicated for **measles** to reduce morbidity and mortality, especially in malnourished or vitamin A-deficient children.
- Measles presents with **Koplik spots**, cough, coryza, conjunctivitis (3 C's), and a maculopapular rash that starts on the face and spreads caudally—**without vesicles**.
- This patient's vesicular rash in multiple stages is not consistent with measles.
*Measles IgM titer*
- While measles can present with fever and rash, the **vesicular and crusted lesions** are pathognomonic for varicella, not measles.
- Measles typically has a **confluent maculopapular rash** without vesicles, along with the classic prodrome of cough, coryza, and conjunctivitis.
- Serologic testing would delay management and is unnecessary given the classic varicella presentation.
*Rapid strep test*
- A **rapid strep test** diagnoses **Group A Streptococcal pharyngitis**, which presents with **sore throat, fever, tonsillar exudates**, and sometimes a **scarlatiniform (sandpaper-like) rash**.
- Scarlet fever rash is erythematous and blanching, not vesicular, and typically spares the face while being prominent in skin folds.
- The generalized pruritic vesicular rash makes streptococcal infection highly unlikely.
Diagnostic criteria and clinical features US Medical PG Question 5: A 13-month-old girl is brought to the physician because of a pruritic rash for 2 days. The girl's mother says she noticed a few isolated skin lesions on her trunk two days ago that appear to be itching. The girl received her routine immunizations 18 days ago. Her mother has been giving her ibuprofen for her symptoms. The patient has no known sick contacts. She is at the 71st percentile for height and the 64th percentile for weight. She is in no acute distress. Her temperature is 38.1°C (100.6°F), pulse is 120/min, and respirations are 26/min. Examination shows a few maculopapular and pustular lesions distributed over the face and trunk. There are some excoriation marks and crusted lesions as well. Which of the following is the most likely explanation for these findings?
- A. Antigen contact with presensitized T-lymphocytes
- B. Reactivation of virus dormant in dorsal root ganglion
- C. Immune complex formation and deposition
- D. Crosslinking of preformed IgE antibodies
- E. Replication of the attenuated vaccine strain (Correct Answer)
Diagnostic criteria and clinical features Explanation: ***Replication of the attenuated vaccine strain***
- The presentation of a **pruritic rash with maculopapular and pustular lesions**, along with crusted lesions, describes the classic **polymorphic rash** of **varicella (chickenpox)**.
- The timing of the rash, appearing **18 days after routine immunizations** (which commonly include the attenuated **MMRV vaccine** at 12-15 months), strongly suggests a vaccine-induced varicella rash due to the replication of the live attenuated virus.
*Antigen contact with presensitized T-lymphocytes*
- This mechanism describes a **Type IV hypersensitivity reaction** (delayed-type hypersensitivity), such as **contact dermatitis** or a **tuberculin skin test**.
- While it can cause a rash, it typically presents differently (e.g., vesicles in contact dermatitis) and the timeline of 18 days post-vaccination is less consistent with a primary contact-mediated reaction causing widespread varicella-like lesions.
*Reactivation of virus dormant in dorsal root ganglion*
- This process describes the pathogenesis of **herpes zoster (shingles)**, which occurs due to the reactivation of the **latent varicella-zoster virus (VZV)** from the dorsal root ganglia.
- Shingles typically presents with a **dermatomal rash** in older individuals or immunocompromised patients, not a widespread polymorphic rash in an otherwise healthy toddler.
*Immune complex formation and deposition*
- This mechanism describes a **Type III hypersensitivity reaction**, where antigen-antibody complexes deposit in tissues, leading to inflammation.
- Conditions like **serum sickness**, **lupus**, or some forms of **vasculitis** are examples, which present with fever, arthralgia, and urticarial or purpuric rashes, differing from the described varicella-like lesions.
*Crosslinking of preformed IgE antibodies*
- This mechanism describes a **Type I hypersensitivity reaction**, commonly known as an **allergic reaction**.
- It typically results in **urticaria (hives)**, angioedema, or anaphylaxis, which are acute reactions characterized by wheals and pruritus, rather than the polymorphic rash with pustules and crusts seen here.
Diagnostic criteria and clinical features US Medical PG Question 6: A 2-year-old girl presents with a rash on her body. Patient’s mother says she noticed the rash onset about 5 hours ago. For the previous 3 days, she says the patient has had a high fever of 39.0°C (102.2°F). Today the fever abruptly subsided but the rash appeared. Vitals are temperature 37.0°C (98.6°F), blood pressure 95/55 mm Hg, pulse 110/min, respiratory rate 30/min, and oxygen saturation 99% on room air. Physical examination reveals a maculopapular, non-confluent, blanchable rash on her back, abdomen, and chest extending superiorly towards the nape of the patient’s neck. Which of the following is this patient’s most likely diagnosis?
- A. Measles
- B. Rubella
- C. Varicella
- D. Roseola (Correct Answer)
- E. Erythema infectiosum (fifth disease)
Diagnostic criteria and clinical features Explanation: ***Roseola***
- This diagnosis is characterized by a **high fever lasting 3-5 days**, which **abruptly subsides**, followed by the appearance of a **maculopapular rash**. This "fever-then-rash" pattern is classic for roseola, also known as exanthem subitum.
- Roseola is caused by **Human Herpesvirus 6 (HHV-6)** and commonly affects children aged 6 months to 3 years.
*Measles*
- Measles typically presents with a **prodrome of cough, coryza, conjunctivitis, and Koplik spots** before the rash appears. The rash typically starts on the face and spreads downwards, often becoming **confluent**.
- Fever in measles usually **persists or even increases** after the rash appears, unlike the abrupt resolution seen in this patient.
*Rubella*
- Rubella, or German measles, is characterized by a **milder fever** and a rash that typically starts on the face and spreads rapidly downwards. Symptoms often include **posterior auricular and suboccipital lymphadenopathy**.
- The rash is usually **finer** and less prominent than measles, and the fever patterns do not match the abrupt resolution described.
*Varicella*
- Varicella (chickenpox) presents with a characteristic **pruritic vesicular rash** that appears in sequential crops, evolving from macules to papules to vesicles and crusts, often described as "dewdrops on a rose petal."
- The fever in varicella typically accompanies the rash, not preceding it with an abrupt resolution as in this case.
*Erythema infectiosum (fifth disease)*
- This condition is caused by **Parvovirus B19** and is characterized by a "slapped cheek" rash on the face, followed by a **lacy, reticular rash** on the trunk and extremities.
- Fever is usually **mild or absent** and does not typically precede the rash in the classic high-fever-then-abrupt-resolution pattern seen here.
Diagnostic criteria and clinical features US Medical PG Question 7: A 4-year-old boy is brought to the pediatrician with fever, diarrhea and bilateral red eye for 7 days. His parents noted that he has never had an episode of diarrhea this prolonged, but several other children at daycare had been ill. His immunization history is up to date. His vitals are normal except for a temperature of 37.5°C (99°F). A physical exam is significant for mild dehydration, preauricular adenopathy, and bilateral conjunctival injection with watery discharge. What is the most likely diagnosis?
- A. C. difficile colitis
- B. Rotavirus infection
- C. Adenovirus infection (Correct Answer)
- D. Vibrio parahaemolyticus infection
- E. Norovirus infection
Diagnostic criteria and clinical features Explanation: ***Adenovirus infection***
- The combination of **fever**, **prolonged diarrhea**, **bilateral conjunctivitis with watery discharge**, and **preauricular adenopathy** in a young child strongly suggests adenovirus infection, particularly the **pharyngoconjunctival fever** syndrome.
- This virus is highly contagious and commonly spreads in communal settings like daycares, aligning with the "several other children at daycare had been ill" observation.
*C. difficile colitis*
- While it causes diarrhea, **_C. difficile_ colitis** is typically associated with **antibiotic use** or hospitalization, and usually presents with more severe, often bloody, diarrhea and abdominal pain, without conjunctivitis or preauricular adenopathy as primary features.
- It is less common as a primary cause of prolonged diarrhea in healthy, ambulatory young children unless there's a clear predisposing factor.
*Rotavirus infection*
- **Rotavirus** is a common cause of **severe watery diarrhea** and vomiting in young children, often accompanied by fever.
- However, **conjunctivitis** and **preauricular adenopathy** are not typical symptoms of rotavirus infection, making it a less likely diagnosis in this scenario.
*Vibrio parahaemolyticus infection*
- **_Vibrio parahaemolyticus_** typically causes **gastroenteritis** after consumption of **contaminated seafood**, presenting with watery diarrhea, abdominal cramps, and fever.
- This type of infection does not commonly cause conjunctivitis or preauricular adenopathy, nor is the daycare setting typical for its transmission.
*Norovirus infection*
- **Norovirus** is a common cause of acute **gastroenteritis** outbreaks, characterized by sudden onset of vomiting and watery diarrhea, sometimes with fever and abdominal cramps.
- Similar to rotavirus, **conjunctivitis** and **preauricular adenopathy** are not characteristic features of norovirus infection.
Diagnostic criteria and clinical features US Medical PG Question 8: A 4-year-old boy is brought to the physician by his parents because of fever and mild abdominal pain for 7 days. His parents report that he developed a rash 2 days ago. He has had no diarrhea or vomiting. Four weeks ago, he returned from a camping trip to Colorado with his family. His immunization records are unavailable. His temperature is 39.4°C (102.9°F), pulse is 111/min, respirations are 27/min, and blood pressure is 96/65 mm Hg. Examination shows bilateral conjunctival injections and fissures on his lower lips. The pharynx is erythematous. There is tender cervical lymphadenopathy. The hands and feet appear edematous. A macular morbilliform rash is present over the trunk. Bilateral knee joints are swollen and tender; range of motion is limited by pain. Which of the following is the most appropriate treatment for this patient's condition?
- A. Supportive treatment only
- B. Intravenous immunoglobulin (Correct Answer)
- C. Oral ibuprofen
- D. Oral penicillin
- E. Oral doxycycline
Diagnostic criteria and clinical features Explanation: ***Intravenous immunoglobulin***
- This patient presents with symptoms highly suggestive of **Kawasaki disease**, including a persistent fever for over 5 days, **bilateral conjunctival injection**, **lip fissures**, **erythematous pharynx**, **cervical lymphadenopathy**, and **edema of hands and feet** followed by a rash.
- **IV immunoglobulin (IVIG)** is the cornerstone of treatment for Kawasaki disease, significantly reducing the risk of **coronary artery aneurysms** if given early in the disease course.
*Supportive treatment only*
- While supportive care (fever reduction, hydration) is important, relying solely on it for **Kawasaki disease** would increase the risk of severe complications, particularly **coronary artery involvement**.
- **Kawasaki disease** is a systemic vasculitis requiring specific immunomodulatory therapy to prevent long-term cardiac sequelae.
*Oral ibuprofen*
- **Ibuprofen**, a non-steroidal anti-inflammatory drug (**NSAID**), can help manage fever and joint pain, but it does not address the underlying **vasculitis** or prevent the cardiac complications of **Kawasaki disease**.
- **Aspirin** (high-dose initially, then low-dose) is part of Kawasaki disease treatment, but ibuprofen alone is insufficient as primary therapy.
*Oral penicillin*
- **Penicillin** is an antibiotic used to treat bacterial infections, such as **streptococcal pharyngitis**.
- This patient's symptoms are inconsistent with a typical bacterial infection requiring penicillin and are more indicative of a **systemic inflammatory condition** like Kawasaki disease, which is not bacterial.
*Oral doxycycline*
- **Doxycycline** is an antibiotic often used for **rickettsial infections** (e.g., Rocky Mountain spotted fever) or Lyme disease, which might be considered given the camping trip.
- However, the classic constellation of symptoms (conjunctival injection, lip changes, edema of extremities, diffuse rash) points strongly away from these and towards **Kawasaki disease**, for which doxycycline is ineffective.
Diagnostic criteria and clinical features US Medical PG Question 9: A 4-year-old boy is brought to a pediatrician by his parents with a history of fever for the last 5 days and irritability, decreased appetite, vomiting, and swelling of the hands and feet for the last 3 days. The patient’s mother mentions that he has been taking antibiotics and antipyretics prescribed by another physician for the last 3 days, but there has been no improvement His temperature is 39.4°C (103.0°F), pulse is 128/min, respiratory rate is 24/min, and blood pressure is 96/64 mm Hg. On physical examination, there is significant edema of the hands and feet bilaterally. There is a 2.5 cm diameter freely moveable, nontender cervical lymph node is palpable on the right side. A strawberry tongue and perianal erythema are noted. Conjunctival injection is present bilaterally. Laboratory findings reveal mild anemia and a leukocytosis with a left-shift. Erythrocyte sedimentation rate (ESR) and serum C-reactive protein (CRP) are increased. If not treated appropriately, this patient is at increased risk of developing which of the following complications?
- A. Lower gastrointestinal hemorrhage
- B. Coronary artery ectasia (Correct Answer)
- C. Acute renal failure
- D. Pulmonary embolism
- E. Acute disseminated encephalomyelitis (ADEM)
Diagnostic criteria and clinical features Explanation: ***Coronary artery ectasia***
- The patient's symptoms, including **prolonged fever**, **conjunctival injection**, **strawberry tongue**, **cervical lymphadenopathy**, **edema of hands and feet**, and **perianal erythema**, are characteristic of **Kawasaki disease**.
- If left untreated, **Kawasaki disease** can lead to significant cardiovascular complications, most notably **coronary artery aneurysms** or ectasia, due to vasculitis of medium-sized arteries.
*Lower gastrointestinal hemorrhage*
- While **gastrointestinal symptoms** such as vomiting and diarrhea can occur in **Kawasaki disease**, severe complications like **lower gastrointestinal hemorrhage** are rare and not the most common or critical untreated complication.
- Other conditions, like **Meckel's diverticulum** or **inflammatory bowel disease**, are more typically associated with lower GI hemorrhage in children.
*Acute renal failure*
- **Renal involvement** in **Kawasaki disease** is uncommon and usually presents as **mild proteinuria** or **sterile pyuria**; **acute renal failure** is an extremely rare complication.
- Significant renal dysfunction is more commonly seen in conditions like **hemolytic-uremic syndrome** or severe dehydration.
*Pulmonary embolism*
- **Pulmonary embolism** is rare in young children and not a typical complication of untreated **Kawasaki disease**.
- It is more commonly associated with conditions causing **hypercoagulability** or prolonged immobility.
*Acute disseminated encephalomyelitis (ADEM)*
- **ADEM** is an **immune-mediated demyelinating disorder** of the central nervous system that typically follows an infection or vaccination.
- It is not a recognized complication of untreated **Kawasaki disease**, whose primary pathology involves systemic vasculitis.
Diagnostic criteria and clinical features US Medical PG Question 10: A 5-year-old girl presents with a rash and a persistent fever of 41.0°C (105.8°F), not relieved by Tylenol. The patient's mother says that her symptoms started 5 days ago and have not improved. The rash started on her trunk and now is present everywhere including the palms and soles. Her birth history is normal. Her pulse is 120/min and respiratory rate is 22/min. On physical examination, the patient is agitated and ill-appearing. There is significant swelling of the distal upper and lower extremities bilaterally. The pharynx is hyperemic (see image). Generalized edema with palpable cervical lymphadenopathy is noted. Muscle tone is normal. Remainder of exam is unremarkable. Laboratory findings are significant for the following:
Laboratory test
Hb 9 g/dL
RBC 3.3/mm3
Neutrophilic leukocytosis 28,000/mm3
Normal platelet count 200,000/mm3
Serum ɣ-GT increased
Hyperbilirubinemia 2.98 mg/dL
AST and ALT are normal, but there is markedly increased serum CRP. Which of the following is the most likely diagnosis in this patient?
- A. Juvenile rheumatoid arthritis
- B. Scarlet fever
- C. Adenovirus infection
- D. Staphylococcal scalded skin syndrome
- E. Kawasaki disease (Correct Answer)
Diagnostic criteria and clinical features Explanation: ***Kawasaki disease***
- The constellation of **prolonged fever, rash (including palms and soles), swollen extremities, hyperemic pharynx, and cervical lymphadenopathy** in a young child is highly suggestive of **Kawasaki disease**.
- Laboratory findings such as **neutrophilic leukocytosis, elevated CRP, and increased γ-GT** further support this diagnosis, which is a **vasculitis** of medium-sized arteries.
*Juvenile rheumatoid arthritis*
- While juvenile rheumatoid arthritis (JRA) can cause **fever and joint swelling**, it typically does not present with the specific rash distribution, **hyperemic pharynx**, or **cervical lymphadenopathy** seen in this patient.
- The **acute onset and severity** of systemic symptoms are more characteristic of Kawasaki disease than typical JRA.
*Scarlet fever*
- Scarlet fever is caused by *Streptococcus pyogenes* and presents with a characteristic **sandpaper-like rash**, **strawberry tongue**, and **fever**.
- It does not typically cause **swelling of the extremities** or the specific laboratory abnormalities like **increased γ-GT** as seen here, and the rash of Kawasaki disease is often polymorphous rather than sandpaper-like.
*Adenovirus infection*
- Adenovirus infections can cause **fever, pharyngitis, and conjunctivitis**, but they do not typically lead to the characteristic widespread rash (including palms and soles), marked **extremity swelling**, or significantly elevated inflammatory markers observed in this case.
- The clinical picture presented is much more severe and specific for a systemic inflammatory condition.
*Staphylococcal scalded skin syndrome*
- **Staphylococcal scalded skin syndrome (SSSS)** is characterized by **erythema and superficial blistering/peeling of the skin**, giving a "scalded" appearance, often starting around the mouth.
- It does not typically cause the **hyperemic pharynx, swollen extremities, or cervical lymphadenopathy** described, and the rash in this patient is not described as blistering or peeling.
More Diagnostic criteria and clinical features US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.