Coronary artery aneurysms US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Coronary artery aneurysms. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Coronary artery aneurysms US Medical PG Question 1: A 6-year-old boy presents to his pediatrician accompanied by his mother for evaluation of a rash. The rash appeared a little over a week ago, and since that time the boy has felt tired. He is less interested in playing outside, preferring to remain indoors because his knees and stomach hurt. His past medical history is significant for an upper respiratory infection that resolved uneventfully without treatment 2 weeks ago. Temperature is 99.5°F (37.5°C), blood pressure is 115/70 mmHg, pulse is 90/min, and respirations are 18/min. Physical exam shows scattered maroon macules and papules on the lower extremities. The abdomen is diffusely tender to palpation. There is no cervical lymphadenopathy or conjunctival injection. Which of the following will most likely be found in this patient?
- A. Coronary artery aneurysms
- B. Leukocytoclastic vasculitis (Correct Answer)
- C. Thrombocytopenia
- D. Mitral regurgitation
- E. Occult malignancy
Coronary artery aneurysms Explanation: ***Leukocytoclastic vasculitis***
- This patient presents with symptoms highly suggestive of **Henoch-Schönlein Purpura (HSP)**, including a preceding URI, fatigue, low-grade fever, **abdominal pain**, and a **palpable purpura** primarily on the lower extremities.
- HSP is characterized by IgA-mediated **small-vessel vasculitis**, which histologically presents as leukocytoclastic vasculitis with IgA deposition on immunofluorescence.
*Coronary artery aneurysms*
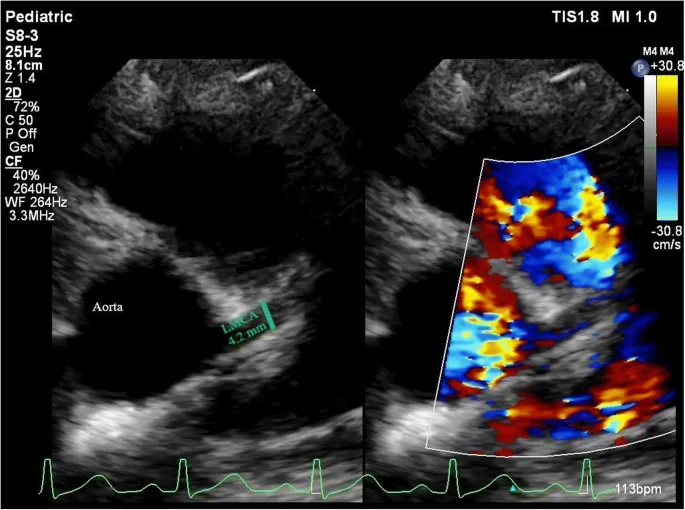
- **Coronary artery aneurysms** are a classic complication of **Kawasaki disease**, not Henoch-Schönlein Purpura.
- Kawasaki disease presents with different clinical features, including prolonged fever, conjunctival injection, oral changes, and cervical lymphadenopathy.
*Thrombocytopenia*
- **Thrombocytopenia** is characterized by a low platelet count and often presents with petechiae, purpura, and bleeding, but the rash in HSP is due to inflammation and extravasation of red blood cells, not low platelets.
- Platelet counts in HSP are typically **normal** or can be slightly elevated as an acute phase reactant.
*Mitral regurgitation*
- **Mitral regurgitation** is a common manifestation of **rheumatic fever**, particularly after recurrent episodes, caused by valvular damage.
- Rheumatic fever is also preceded by infection (Group A Strep) but involves different symptoms like migratory polyarthritis, carditis, chorea, erythema marginatum, and subcutaneous nodules, which are not described here.
*Occult malignancy*
- While an **occult malignancy** can cause paraneoplastic syndromes or constitutional symptoms, the specific constellation of symptoms, including the migratory rash, abdominal pain, and preceding URI, points much more strongly to **HSP** in a 6-year-old.
- The presentation is more consistent with an acute, inflammatory process rather than a chronic, insidious malignant one.
Coronary artery aneurysms US Medical PG Question 2: A 4-year-old boy is brought to the emergency department by his mother with a rash on his trunk, malaise, and fever with spikes up to 38.5°C (101.3°F) for the past 2 weeks. The patient's mother says she tried giving him Tylenol with little improvement. Past medical history includes a spontaneous vaginal delivery at full term. The patient's vaccines are up-to-date and he has met all developmental milestones. On physical examination, his lips are cracking, and he has painful cervical lymphadenopathy. The rash is morbilliform and involves his trunk, palms, and the soles of his feet. There is fine desquamation of the skin of the perianal region. Which of the following anatomical structures is most important to screen for possible complications in this patient?
- A. Mitral valve
- B. Kidneys
- C. Gallbladder
- D. Coronary artery (Correct Answer)
- E. Pylorus
Coronary artery aneurysms Explanation: ***Coronary artery***
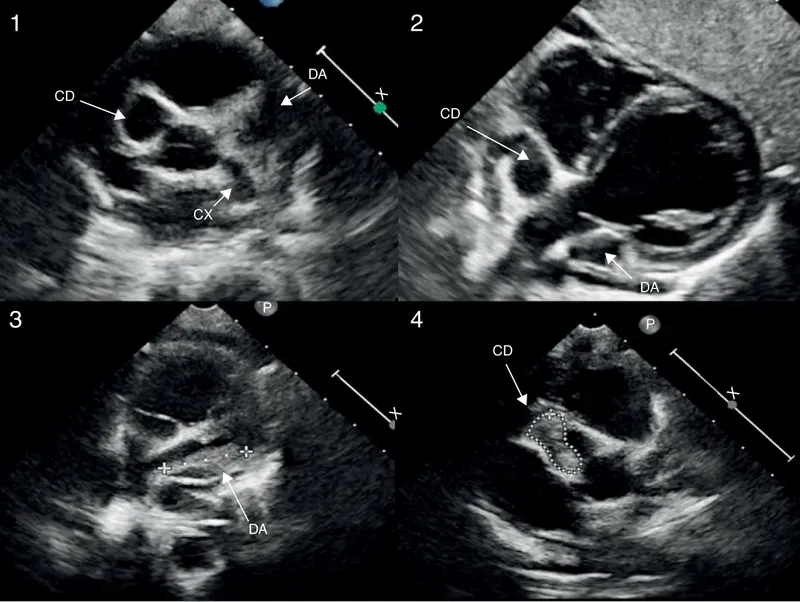
- The constellation of symptoms, including prolonged fever, rash on trunk, palms, and soles, cracked lips, cervical lymphadenopathy, and perianal desquamation, is highly indicative of **Kawasaki disease**.
- **Coronary artery aneurysms** are the most serious complication of Kawasaki disease, occurring in 15-25% of untreated children, necessitating close monitoring and screening.
*Mitral valve*
- While other forms of vasculitis or rheumatic fever can affect heart valves, **mitral valve** involvement is not a primary or characteristic complication of Kawasaki disease.
- The main cardiac concern in Kawasaki disease is direct arterial inflammation, not valvular dysfunction.
*Kidneys*
- **Renal involvement**, such as acute kidney injury, is not a typical or prominent feature of Kawasaki disease.
- Kawasaki disease primarily targets medium-sized muscular arteries throughout the body, with a predilection for the coronary arteries.
*Gallbladder*
- **Hydrops of the gallbladder** can occur in Kawasaki disease, leading to acute cholecystitis-like symptoms, but it is generally a self-limiting complication.
- While it's a potential finding, it is not as life-threatening or essential to screen for as coronary artery complications.
*Pylorus*
- There is no direct association between Kawasaki disease and primary involvement or complications of the **pylorus**.
- Gastrointestinal symptoms can occur, but these are typically non-specific and do not involve anatomical changes to the pylorus.
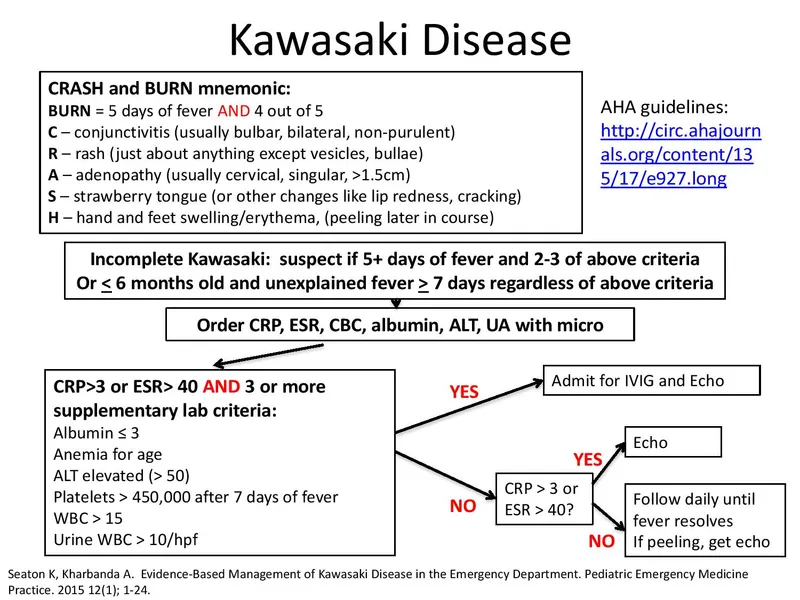
Coronary artery aneurysms US Medical PG Question 3: A 5-year-old girl is brought to the emergency department by her father due to a 6-day history of fevers and irritability. His father reports that the fevers have ranged from 101-104°F (38.3-40°C). He tried to give her ibuprofen, but the fevers have been unresponsive. Additionally, she developed a rash 3 days ago and has refused to wear shoes because they feel "tight." Her father reports that other than 2 ear infections she had when she was younger, the patient has been healthy. She is up-to-date on her vaccinations except for the vaccine boosters scheduled for ages 4-6. The patient's temperature is 103.5°F (39.7°C), blood pressure is 110/67 mmHg, pulse is 115/min, and respirations are 19/min with an oxygen saturation of 98% O2 on room air. Physical examination shows bilateral conjunctivitis, palpable cervical lymph nodes, a diffuse morbilliform rash, and desquamation of the palms and soles with swollen hands and feet. Which of the following is the next step in management?
- A. Acetaminophen
- B. High dose aspirin
- C. IVIG and high-dose aspirin (Correct Answer)
- D. Nafcillin
- E. Penicillin V
Coronary artery aneurysms Explanation: ***IVIG and high-dose aspirin***
- The patient's symptoms (prolonged fever >5 days, bilateral conjunctivitis, diffuse rash, extremity changes with edema and desquamation, cervical lymphadenopathy) meet diagnostic criteria for **Kawasaki disease**.
- **IVIG (Intravenous Immunoglobulin)** is the PRIMARY treatment and must be given within 10 days of fever onset to reduce the risk of **coronary artery aneurysms** from 25% to <5%.
- **High-dose aspirin** is given as ADJUNCTIVE therapy for its anti-inflammatory effects, then transitioned to low-dose aspirin for antiplatelet effects once fever resolves.
- This combination is the **standard of care** and should be initiated as soon as the diagnosis is suspected.
*High dose aspirin*
- While aspirin is an essential component of Kawasaki disease treatment, it should **not be given as monotherapy**.
- Aspirin alone without **IVIG** is insufficient and fails to adequately reduce the risk of coronary complications.
- The question asks for the "next step in management," which requires **both IVIG and aspirin** together.
*Acetaminophen*
- Acetaminophen is an antipyretic but lacks the anti-inflammatory effects needed for **Kawasaki disease**.
- The patient's fever has already been unresponsive to **ibuprofen**, indicating that simple antipyretics are inadequate.
- It has no role in preventing the vascular complications of Kawasaki disease.
*Nafcillin*
- **Nafcillin** is an antibiotic for bacterial infections, particularly *Staphylococcus aureus*.
- **Kawasaki disease** is a vasculitis of unknown etiology (possibly post-infectious immune response) and is **not treated with antibiotics**.
- The clinical presentation does not suggest an acute bacterial infection requiring antibiotic therapy.
*Penicillin V*
- **Penicillin V** is used for streptococcal infections such as strep pharyngitis.
- The constellation of findings (persistent fever, conjunctivitis, rash, extremity changes, lymphadenopathy) is classic for **Kawasaki disease**, not a bacterial infection.
- Antibiotics have no role in the management of Kawasaki disease.
Coronary artery aneurysms US Medical PG Question 4: A 62-year-old man with a past medical history of previous myocardial infarction, angina, hypertension, hyperlipidemia, diabetes mellitus, peripheral vascular disease, and below knee amputation has developed new chest pain. His medication includes insulin, hydrochlorothiazide, lisinopril, metoprolol, daily aspirin, atorvastatin, and nitroglycerin as needed. His vitals include: blood pressure 135/87 mm Hg, pulse 52/min, and respirations 17/min. Coronary arteriography shows a reduced ejection fraction, a 65% stenosis of the left anterior descending artery, and a 75% stenosis of the left circumflex artery. Which of the following is the recommended treatment for the patient?
- A. Increased beta blocker dosage
- B. Coronary artery bypass grafting (CABG) (Correct Answer)
- C. Angioplasty with stent placement
- D. Extended release nitrate therapy
- E. Heparin
Coronary artery aneurysms Explanation: ***Coronary artery bypass grafting (CABG)***
- This patient has complex **multivessel coronary artery disease** (LAD and circumflex stenosis) with a **reduced ejection fraction** and a history of multiple comorbidities, making CABG the preferred revascularization strategy for improved outcomes.
- CABG offers a more complete revascularization in patients with significant disease burden and reduced left ventricular function, leading to better long-term survival and symptom relief compared to PCI in this population.
*Increased beta blocker dosage*
- The patient's current heart rate is 52/min, which is already at the lower end of the target range for beta-blocker therapy in cardiac patients, and further increasing the dose could lead to **bradycardia** and worsening symptoms.
- While beta-blockers are crucial for managing angina and improving outcomes post-MI, increasing the dose wouldn't address the underlying anatomical severe multi-vessel coronary artery disease.
*Angioplasty with stent placement*
- Although PCI (angioplasty with stent placement) can be used for coronary stenosis, in patients with **multivessel disease**, **reduced ejection fraction**, and **diabetes mellitus**, CABG generally offers superior long-term results and survival benefits.
- The complexity of the lesions (65% LAD, 75% circumflex) in a patient with significant comorbidities and extensive atherosclerotic disease makes PCI a less optimal choice here.
*Extended release nitrate therapy*
- Nitrates primarily provide **symptomatic relief** by causing vasodilation, but they do not address the severe underlying coronary stenoses or improve long-term outcomes in patients with complex, multivessel disease.
- The patient is already on PRN nitroglycerin, and while extended-release nitrates could help with angina, they are not a definitive treatment for significant arterial blockages requiring revascularization.
*Heparin*
- Heparin is an **anticoagulant** that may be used as part of initial management of acute coronary syndromes, but it provides only temporary stabilization and does not address the **definitive need for revascularization**.
- While anticoagulation plays a role in acute management, this patient requires **definitive anatomical correction** of his multivessel disease with significant stenoses, which only surgical or percutaneous revascularization can provide, with CABG being superior given his clinical profile.
Coronary artery aneurysms US Medical PG Question 5: A 49-year-old man was brought to the emergency department by ambulance with complaints of sudden-onset chest pain that radiates into his neck and down his left arm. This substernal pain started 2 hours ago while he was having dinner. His past medical history is remarkable for hypercholesterolemia that is responsive to therapy with statins and coronary artery disease. His temperature is 37.0°C (98.6°F), blood pressure is 155/90 mm Hg, pulse is 112/min, and respiratory rate is 25/min. Troponin I levels are elevated. A 12-lead ECG was performed (see image). What is the most likely etiology of this patient’s presentation?
- A. Coronary vasospasm
- B. Right coronary artery occlusion (Correct Answer)
- C. Left circumflex artery occlusion
- D. Left anterior descending artery occlusion
- E. Left main coronary artery occlusion
Coronary artery aneurysms Explanation: ***Right coronary artery occlusion***
- The ECG shows significant **ST elevation in inferior leads (II, III, aVF)** and **ST depression in anterior leads (V1-V4)**, which is characteristic of an **inferior wall myocardial infarction**.
- **Inferior wall MIs** are typically caused by occlusion of the **right coronary artery (RCA)**. The reciprocal changes (ST depression in anterior leads) support this, indicating involvement of the posterolateral wall often supplied by the RCA.
*Coronary vasospasm*
- While coronary vasospasm (e.g., in **Prinzmetal angina**) can cause ST elevation, it usually presents with more transient symptoms that resolve with vasodilators, and the ST segment elevations are typically regional but often more widespread or dynamic.
- The patient's history of **coronary artery disease (CAD)** and persistent symptoms with elevated troponin point towards a fixed obstruction rather than vasospasm.
*Left circumflex artery occlusion*
- **Left circumflex artery occlusion** typically causes changes in leads I, aVL, V5, and V6 (high lateral or lateral wall MI), and sometimes posterior leads.
- The predominant ST elevation in leads II, III, and aVF is not characteristic of a primary **left circumflex artery occlusion**.
*Left anterior descending artery occlusion*
- **Left anterior descending (LAD) artery occlusion** usually results in **anterior or anteroseptal MI**, characterized by ST elevation in leads V1-V4 and potentially I and aVL.
- The ECG shows ST depression in V1-V4, which are reciprocal changes rather than direct signs of an **LAD occlusion**.
*Left main coronary artery occlusion*
- **Left main coronary artery occlusion** is a catastrophic event, often presenting with widespread ST depression in multiple leads with ST elevation in aVR (and sometimes V1).
- While life-threatening, the ECG pattern here with prominent inferior ST elevation and reciprocal anterior depression is more indicative of an **RCA occlusion** than a left main occlusion.
Coronary artery aneurysms US Medical PG Question 6: A 75-year-old Caucasian man presents to the emergency department with abdominal pain. The patient states he was at home eating dinner when he began to experience severe abdominal pain. The patient has a past medical history of diabetes, hypertension, and atherosclerosis. He lives at home alone, smokes cigarettes, and drinks 1 to 2 alcoholic drinks per day. The patient is given IV morphine and an ultrasound is obtained demonstrating a dilated abdominal aorta. The patient states that his father died of a similar finding and is concerned about his prognosis. Which of the following is the greatest risk factor for this patient's presentation?
- A. Male gender and age
- B. Caucasian race
- C. Cigarette smoking (Correct Answer)
- D. Family history
- E. Atherosclerosis
Coronary artery aneurysms Explanation: ***Cigarette smoking***
- **Cigarette smoking** is the most significant modifiable risk factor for the development and expansion of **abdominal aortic aneurysms (AAAs)**, directly contributing to vascular inflammation and degradation.
- The patient's history of smoking suggests a strong causal link to his current presentation of a dilated aorta, which is highly indicative of an AAA.
*Male gender and age*
- While **male gender** and **advanced age (over 65)** are significant demographic risk factors for AAA, they are considered non-modifiable and less impactful than smoking in terms of risk magnitude.
- These factors increase predisposition but do not exert the same direct, damaging effect on the arterial wall as chronic smoking.
*Caucasian race*
- **Caucasian race** is a known demographic risk factor for AAA, with higher prevalence rates compared to other ethnic groups.
- However, this is a non-modifiable genetic predisposition and contributes less to the overall risk than modifiable lifestyle factors like smoking.
*Family history*
- A **family history** of AAA, as suggested by the patient's father having a similar condition, increases an individual's susceptibility.
- This is a significant non-modifiable risk factor, indicating genetic predisposition, but its overall impact on aneurysm formation and progression is typically less than that of active smoking.
*Atherosclerosis*
- **Atherosclerosis** is a strong associated condition with AAA, as both share common risk factors and pathology related to arterial wall degeneration.
- While atherosclerosis contributes to the overall vascular compromise, smoking specifically has a more direct and potent effect on promoting aneurysm formation and rupture independently.
Coronary artery aneurysms US Medical PG Question 7: A 65-year-old man is brought to the emergency department with central chest pain for the last hour. He rates his pain as 8/10, dull in character, and says it is associated with profuse sweating and shortness of breath. He used to have heartburn and upper abdominal pain associated with food intake but had never experienced chest pain this severe. He has a history of diabetes, hypertension, and hypercholesterolemia. His current medication list includes amlodipine, aspirin, atorvastatin, insulin, valsartan, and esomeprazole. He has smoked 1 pack of cigarettes per day for the past 35 years. Physical examination reveals: blood pressure 94/68 mm Hg, pulse 112/min, oxygen saturation 95% on room air, and BMI 31.8 kg/m2. His lungs are clear to auscultation. An electrocardiogram (ECG) shows ST-segment elevations in the inferior leads. The patient is discharged home after 3 days on aspirin, clopidogrel, and atenolol in addition to his previous medications. He is advised to get an exercise tolerance test (ETT) in one month. A month later at his ETT, his resting blood pressure is 145/86 mm Hg. The pre-exercise ECG shows normal sinus rhythm with Q waves in the inferior leads. After 3 minutes of exercise, the patient develops chest pain that is gradually worsening, and repeat blood pressure is 121/62 mm Hg. No ischemic changes are noted on the ECG. What is the most appropriate next step?
- A. Stop exercise and order a coronary angiography (Correct Answer)
- B. Stop exercise and order a pharmacological stress test
- C. Stop exercise and order an echo stress test
- D. Continue exercise since ECG does not show ischemic changes
- E. Repeat exercise tolerance testing after one month
Coronary artery aneurysms Explanation: **Stop exercise and order a coronary angiography**
- The patient's developing chest pain during the exercise tolerance test, despite no ECG changes, is highly suggestive of **myocardial ischemia** due to his extensive cardiac risk factors and prior STEMI. The **drop in blood pressure** during exercise indicates possible cardiac dysfunction or severe ischemia, making immediate investigation with **coronary angiography** critical.
- Given the patient's strong history of coronary artery disease (CAD), including a recent myocardial infarction, an exercise-induced symptom warrants immediate and definitive evaluation for **obstructive CAD** to guide further management.
*Stop exercise and order a pharmacological stress test*
- While pharmacological stress tests are useful for patients unable to exercise, this patient is already undergoing an exercise test and has demonstrated a symptom during exertion.
- A pharmacological stress test would provide functional information but would not directly image the coronary arteries, which is crucial given the high suspicion for severe CAD.
*Stop exercise and order an echo stress test*
- An echo stress test would assess wall motion abnormalities indicative of ischemia, but similar to other stress tests, it provides functional information rather than direct anatomical visualization of coronary blockages.
- While valuable, in the context of this patient's acute symptoms and risk profile, **coronary angiography** offers a more direct and definitive diagnostic approach to identify and potentially intervene on arterial blockages.
*Continue exercise since ECG does not show ischemic changes*
- Continuing exercise when a patient develops chest pain and a drop in blood pressure is **contraindicated** and dangerous.
- **Symptoms (chest pain)** and **hemodynamic changes (blood pressure drop)** are critical indicators of ischemia, even if ECG changes are absent, as ECG sensitivity for detecting ischemia is not 100%.
*Repeat exercise tolerance testing after one month*
- Repeating the test ignores the significant and alarming symptoms the patient experienced during this test.
- It would delay definitive diagnosis and treatment, putting the patient at unnecessarily high risk of another cardiac event.
Coronary artery aneurysms US Medical PG Question 8: A 60-year-old male presents for a routine health check-up. The patient complains of reduced exercise tolerance for the past 2 years. Also, in the past year, he has noticed chest pain after climbing the stairs in his home. He has no significant past medical history or current medications. The patient reports a 45-pack-year smoking history. The vital signs include temperature 37.0°C (98.6°F), blood pressure 160/100 mm Hg, pulse 72/min, respiratory rate 15/min, and oxygen saturation 99% on room air. His body mass index (BMI) is 34 kg/m2. Physical examination is unremarkable. Laboratory studies show:
Serum total cholesterol 265 mg/dL
HDL 22 mg/dL
LDL 130 mg/dL
Triglycerides 175 mg/dL
HDL: high-density lipoprotein; LDL: low-density lipoprotein
Which of the following vascular pathologies is most likely present in this patient?
- A. Medial calcific sclerosis
- B. Deep venous thrombosis
- C. Lymphedema
- D. Atherosclerosis (Correct Answer)
- E. Hyperplastic arteriosclerosis
Coronary artery aneurysms Explanation: ***Atherosclerosis***
- This patient presents with multiple **risk factors for atherosclerosis**, including **hyperlipidemia** (elevated total cholesterol, LDL, and triglycerides with low HDL), **hypertension**, **obesity**, and a significant **smoking history**.
- His symptoms of **reduced exercise tolerance** and **exertional chest pain** are classic manifestations of **angina pectoris**, which is caused by narrowed coronary arteries due to atherosclerosis.
*Medial calcific sclerosis*
- Also known as **Mönckeberg arteriosclerosis**, involves calcification of the **tunica media** of muscular arteries, without significant luminal narrowing.
- While it can lead to **artery hardening**, it typically does not obstruct blood flow or cause angina, and is more common in **elderly** and **diabetic** individuals.
*Deep venous thrombosis*
- This condition involves the formation of a **blood clot in a deep vein**, usually in the legs, leading to symptoms like **leg swelling, pain, and redness**.
- The patient's symptoms of chest pain and reduced exercise tolerance are not characteristic of DVT.
*Lymphedema*
- Characterized by **swelling** in one or more limbs due to an impaired **lymphatic drainage system**.
- It does not present with chest pain or reduced exercise tolerance and is distinct from vascular pathologies affecting blood flow.
*Hyperplastic arteriosclerosis*
- This is a form of **arteriolar sclerosis** primarily seen in severe **hypertension**, characterized by **concentric thickening of arteriolar walls** due to smooth muscle cell proliferation and basement membrane duplication.
- While the patient has hypertension, his symptoms point towards obstruction of larger coronary arteries rather than widespread arteriolar changes, and his lipid profile is more indicative of atherosclerosis.
Coronary artery aneurysms US Medical PG Question 9: A 26-year-old man comes to the physician because of a 1-week history of left-sided chest pain. The pain is worse when he takes deep breaths. Over the past 6 weeks, he had been training daily for an upcoming hockey tournament. He does not smoke cigarettes or drink alcohol but has used cocaine once. His temperature is 37.1°C (98.7°F), pulse is 75/min, and blood pressure is 128/85 mm Hg. Physical examination shows tenderness to palpation of the left chest. An x-ray of the chest is shown. Which of the following is the most appropriate initial pharmacotherapy?
- A. Heparin
- B. Nitroglycerin
- C. Alteplase
- D. Naproxen (Correct Answer)
- E. Alprazolam
Coronary artery aneurysms Explanation: ***Naproxen***
- This patient presents with symptoms highly suggestive of **costochondritis** or a **musculoskeletal chest wall pain**. Key features include **tenderness to palpation of the chest wall**, pain made worse by **deep breaths** (pleuritic nature), and a history of strenuous activity (hockey training).
- An X-ray of the chest appears normal, ruling out other serious causes of chest pain like pneumothorax or significant infiltrates. Given the musculoskeletal nature of the pain, a **nonsteroidal anti-inflammatory drug (NSAID)** like naproxen is the most appropriate initial treatment to reduce pain and inflammation.
*Heparin*
- Heparin is an **anticoagulant** used to treat or prevent blood clots, such as in **pulmonary embolism** or deep vein thrombosis.
- While chest pain can be a symptom of pulmonary embolism, the physical exam finding of **localized tenderness to palpation** is not characteristic of a pulmonary embolism, and the normal chest X-ray makes it less likely.
*Nitroglycerin*
- Nitroglycerin is primarily used to treat **angina pectoris** (chest pain due to reduced blood flow to the heart) by causing vasodilation and reducing cardiac workload.
- The patient's age (26), absence of typical cardiac risk factors (except for prior cocaine use, which can cause vasospasm but is not suggested by the clinical picture or exam), and the **pleuritic nature of the pain** with **chest wall tenderness** make angina unlikely.
*Alteplase*
- Alteplase is a **thrombolytic agent** used to dissolve existing blood clots, typically in conditions like **acute myocardial infarction**, **pulmonary embolism**, or **ischemic stroke**.
- There is no clinical or radiological evidence (normal chest X-ray) to suggest a life-threatening thrombotic event requiring thrombolysis in this patient.
*Alprazolam*
- Alprazolam is a **benzodiazepine** used to treat **anxiety and panic disorders**.
- While anxiety can sometimes manifest as chest pain, the clear physical finding of **localized chest wall tenderness** points to a physical cause, and thus, an anxiolytic is not the most appropriate initial pharmacotherapy.
Coronary artery aneurysms US Medical PG Question 10: A 49-year-old man with a past medical history of hypertension on amlodipine presents to your office to discuss ways to lessen his risk of complications from heart disease. After a long discussion, he decides to significantly decrease his intake of trans fats in an attempt to lower his risk of coronary artery disease. Which type of prevention is this patient initiating?
- A. Secondary prevention
- B. Delayed prevention
- C. Quaternary prevention
- D. Tertiary prevention
- E. Primary prevention (Correct Answer)
Coronary artery aneurysms Explanation: ***Primary prevention***
- This patient is initiating primary prevention by **modifying lifestyle choices** (decreasing trans fats) to **prevent the initial onset of coronary artery disease**, as he has a risk factor (hypertension) but no established heart disease.
- Primary prevention focuses on **preventing disease before it occurs** through health promotion and risk reduction.
*Secondary prevention*
- Secondary prevention involves **early detection and treatment of existing disease** to prevent progression or recurrence.
- Examples include **screening tests** like mammography or **medications for individuals already diagnosed** with a condition.
*Delayed prevention*
- This is **not a recognized category** of prevention in public health or medical practice.
- Prevention stages are typically classified as primary, secondary, tertiary, and sometimes quaternary.
*Quaternary prevention*
- Quaternary prevention aims to **protect patients from medical interventions** that may cause harm, such as over-medicalization or unnecessary procedures.
- It focuses on **reducing the burden of iatrogenic disease** and ensuring appropriate care.
*Tertiary prevention*
- Tertiary prevention focuses on **reducing the impact of an existing disease** or disability through rehabilitation and managing complications.
- It applies to patients who **already have an established disease** and seeks to improve their quality of life and functionality.
More Coronary artery aneurysms US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.