Cardiac complications and evaluation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cardiac complications and evaluation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cardiac complications and evaluation US Medical PG Question 1: A 72-year-old woman comes to the physician for follow-up care. One year ago, she was diagnosed with a 3.8-cm infrarenal aortic aneurysm found incidentally on abdominal ultrasound. She has no complaints. She has hypertension, type 2 diabetes mellitus, and COPD. Current medications include hydrochlorothiazide, lisinopril, glyburide, and an albuterol inhaler. She has smoked a pack of cigarettes daily for 45 years. Her temperature is 37°C (98.6°F), pulse is 90/min, respirations are 12/min, and blood pressure is 145/85 mm Hg. Examination shows a faint abdominal bruit on auscultation. Ultrasonography of the abdomen shows a 4.9-cm saccular dilation of the infrarenal aorta. Which of the following is the most appropriate next step in management?
- A. Elective endovascular aneurysm repair (Correct Answer)
- B. Adjustment of cardiovascular risk factors and follow-up ultrasound in 12 months
- C. Adjustment of cardiovascular risk factors and follow-up ultrasound in 6 months
- D. Elective open aneurysm repair
- E. Adjustment of cardiovascular risk factors and follow-up CT in 6 months
Cardiac complications and evaluation Explanation: ***Elective endovascular aneurysm repair***
- The patient's **infrarenal aortic aneurysm** has grown from 3.8 cm to 4.9 cm in one year, approaching the **5.0 cm threshold for intervention in women** (compared to 5.5 cm for men). The **rapid growth rate of 1.1 cm/year** (normal is <0.5 cm/year) significantly increases rupture risk and is an indication for intervention even before reaching the absolute size threshold.
- Given her multiple comorbidities (hypertension, diabetes, COPD, 45 pack-year smoking history), **endovascular aneurysm repair (EVAR)** is preferred over open repair due to lower perioperative morbidity and mortality in high-risk surgical candidates.
- The combination of near-threshold size and rapid growth makes elective repair appropriate now rather than continued surveillance.
*Adjustment of cardiovascular risk factors and follow-up ultrasound in 12 months*
- While **risk factor modification** (smoking cessation, blood pressure control) is essential, it is insufficient as the primary management given the aneurysm's significant growth and imminent rupture risk.
- A 12-month follow-up interval is too long for a rapidly growing aneurysm (grew 1.1 cm in the past year), as this increases the risk of rupture without intervention.
*Adjustment of cardiovascular risk factors and follow-up ultrasound in 6 months*
- **Risk factor management** is important but does not address the immediate need for intervention due to the aneurysm's size approaching the threshold and concerning growth rate.
- While 6-month surveillance might be considered for smaller aneurysms with slower growth, this aneurysm's rapid expansion rate suggests it will exceed 5.0 cm well before the next surveillance interval, increasing rupture risk unnecessarily.
*Elective open aneurysm repair*
- **Open aneurysm repair** is an effective treatment but carries significantly higher perioperative risks (30-day mortality 3-5% vs 1-2% for EVAR) compared to endovascular repair, especially in patients with multiple comorbidities.
- Given this patient's COPD, smoking history, and cardiovascular risk factors, EVAR is the preferred approach to minimize surgical stress and improve perioperative outcomes.
*Adjustment of cardiovascular risk factors and follow-up CT in 6 months*
- **Risk factor modification** alone is insufficient given the aneurysm's proximity to intervention threshold and rapid growth rate.
- While CT provides more detailed anatomic imaging for surgical planning, continued surveillance is inappropriate when the patient already meets criteria for intervention. Additionally, CT involves radiation exposure and is typically reserved for pre-operative planning rather than routine surveillance.
Cardiac complications and evaluation US Medical PG Question 2: A 6-year-old boy presents to his pediatrician accompanied by his mother for evaluation of a rash. The rash appeared a little over a week ago, and since that time the boy has felt tired. He is less interested in playing outside, preferring to remain indoors because his knees and stomach hurt. His past medical history is significant for an upper respiratory infection that resolved uneventfully without treatment 2 weeks ago. Temperature is 99.5°F (37.5°C), blood pressure is 115/70 mmHg, pulse is 90/min, and respirations are 18/min. Physical exam shows scattered maroon macules and papules on the lower extremities. The abdomen is diffusely tender to palpation. There is no cervical lymphadenopathy or conjunctival injection. Which of the following will most likely be found in this patient?
- A. Coronary artery aneurysms
- B. Leukocytoclastic vasculitis (Correct Answer)
- C. Thrombocytopenia
- D. Mitral regurgitation
- E. Occult malignancy
Cardiac complications and evaluation Explanation: ***Leukocytoclastic vasculitis***
- This patient presents with symptoms highly suggestive of **Henoch-Schönlein Purpura (HSP)**, including a preceding URI, fatigue, low-grade fever, **abdominal pain**, and a **palpable purpura** primarily on the lower extremities.
- HSP is characterized by IgA-mediated **small-vessel vasculitis**, which histologically presents as leukocytoclastic vasculitis with IgA deposition on immunofluorescence.
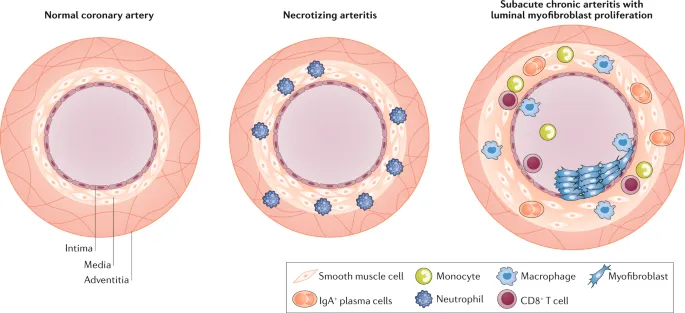
*Coronary artery aneurysms*
- **Coronary artery aneurysms** are a classic complication of **Kawasaki disease**, not Henoch-Schönlein Purpura.
- Kawasaki disease presents with different clinical features, including prolonged fever, conjunctival injection, oral changes, and cervical lymphadenopathy.
*Thrombocytopenia*
- **Thrombocytopenia** is characterized by a low platelet count and often presents with petechiae, purpura, and bleeding, but the rash in HSP is due to inflammation and extravasation of red blood cells, not low platelets.
- Platelet counts in HSP are typically **normal** or can be slightly elevated as an acute phase reactant.
*Mitral regurgitation*
- **Mitral regurgitation** is a common manifestation of **rheumatic fever**, particularly after recurrent episodes, caused by valvular damage.
- Rheumatic fever is also preceded by infection (Group A Strep) but involves different symptoms like migratory polyarthritis, carditis, chorea, erythema marginatum, and subcutaneous nodules, which are not described here.
*Occult malignancy*
- While an **occult malignancy** can cause paraneoplastic syndromes or constitutional symptoms, the specific constellation of symptoms, including the migratory rash, abdominal pain, and preceding URI, points much more strongly to **HSP** in a 6-year-old.
- The presentation is more consistent with an acute, inflammatory process rather than a chronic, insidious malignant one.
Cardiac complications and evaluation US Medical PG Question 3: A 24-year-old man presents with a complaint of breathlessness while jogging. He says that he recently started marathon training. He does not have any family history of asthma nor has any allergies. He currently takes no medication. The blood pressure is 120/80 mm Hg, and the heart rate is 67/min. With each heartbeat, he experiences pounding in his chest, and his head bobs. On physical examination, he has long fingers, funnel chest, and disproportionate body proportions with a decreased upper-to-lower segment ratio. On auscultation over the 2nd right intercostal space, an early diastolic murmur is heard, and 3rd and 4th heart sounds are heard. Echocardiography shows aortic root dilatation. The patient is scheduled for surgery. Which of the following is associated with this patient's condition?
- A. Klinefelter syndrome
- B. Intravenous drug abuse
- C. Marfan's Syndrome (Correct Answer)
- D. Kawasaki syndrome
- E. Gonorrhea
Cardiac complications and evaluation Explanation: ***Marfan's Syndrome***
- The patient presents with **tall stature**, **long fingers (arachnodactyly)**, **funnel chest (pectus excavatum)**, and **aortic root dilation** with **aortic regurgitation** (early diastolic murmur, head bobbing, pounding in the chest), all classic features of Marfan syndrome.
- This is a **connective tissue disorder** caused by a mutation in the **FBN1 gene**, leading to defective **fibrillin-1**, which is crucial for structural integrity in the heart, blood vessels, eyes, and skeleton.
*Klinefelter syndrome*
- Characterized by a **47, XXY karyotype** and typically presents with infertility, small testes, gynecomastia, and tall stature, but not the specific cardiovascular or skeletal features described.
- While it can cause tall stature, it does not explain the **arachnodactyly**, **pectus excavatum**, or the severe **aortic root dilation** and regurgitation.
*Intravenous drug abuse*
- Primarily associated with **infective endocarditis**, particularly affecting the **tricuspid valve**, leading to heart murmurs related to infection, not the skeletal and aortic root abnormalities seen here.
- This history would lead to a different clinical presentation, potentially involving fever, chills, and vegetations on valve leaflets, none of which are mentioned.
*Kawasaki syndrome*
- An **acute inflammatory vasculitis** primarily affecting young children, characterized by fever, rash, conjunctivitis, lymphadenopathy, and oral mucosal changes.
- While it can cause **coronary artery aneurysms**, it does not explain the skeletal abnormalities or the specific presentation of aortic root dilation with regurgitation in an adult.
*Gonorrhea*
- A **sexually transmitted infection** that can lead to disseminated gonococcal infection, causing arthritis, tenosynovitis, and dermatitis.
- It does not cause the specific skeletal abnormalities or the primary cardiac pathology of aortic root dilation and regurgitation described in this patient.
Cardiac complications and evaluation US Medical PG Question 4: A previously healthy 4-year-old boy is brought to the physician by his parents because he has had a fever, diffuse joint pain, and a rash on his abdomen for the past week. Acetaminophen did not improve his symptoms. He emigrated from China with his family 2 years ago. He attends daycare. His immunization records are not available. His temperature is 38.5°C (101.3°F), pulse is 125/min, and blood pressure is 100/60 mm Hg. Examination shows polymorphous truncal rash. The eyes are pink with no exudate. The tongue is shiny and red, and the lips are cracked. The hands and feet are red and swollen. There is right-sided anterior cervical lymphadenopathy. Which of the following is the most appropriate next step in management?
- A. HHV-6 immunoglobulin M (IgM) detection
- B. ANA measurement
- C. Echocardiography (Correct Answer)
- D. Monospot test
- E. Antistreptolysin O titer measurement
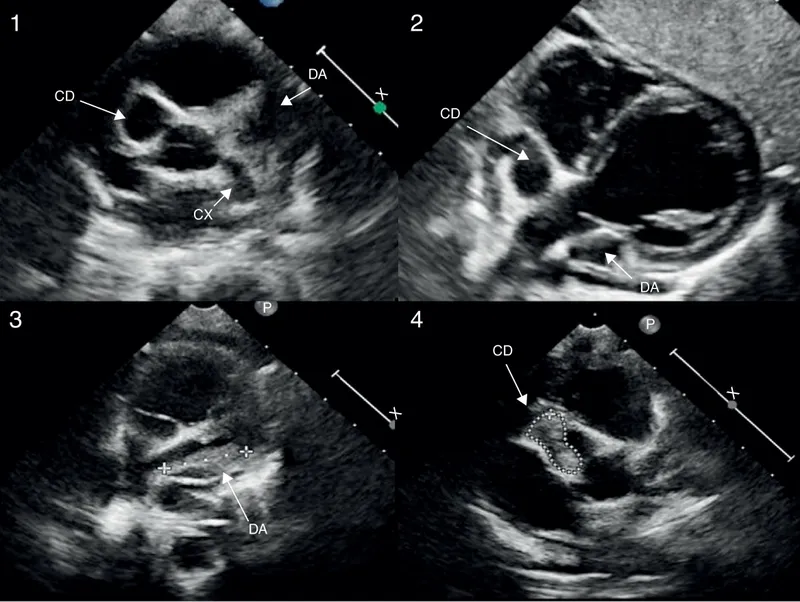
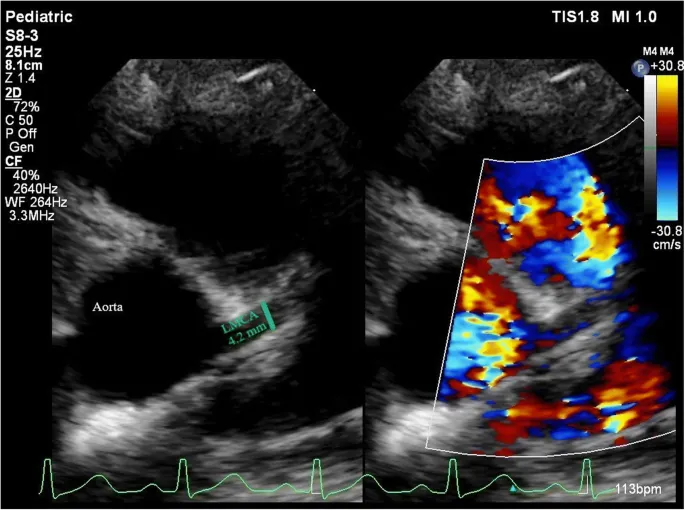
Cardiac complications and evaluation Explanation: ***Echocardiography***
- This patient presents with classic symptoms of **Kawasaki disease**, including protracted fever (>5 days), polymorphous rash, conjunctival injection, cracked lips and red tongue (**strawberry tongue**), swollen hands and feet, and cervical lymphadenopathy.
- The diagnosis can be made clinically when fever ≥5 days plus ≥4 of 5 principal criteria are present, which this patient meets.
- **Echocardiography** is essential to establish a **baseline cardiac assessment** and screen for **coronary artery aneurysms**, which occur in 15-25% of untreated patients.
- Among the diagnostic options listed, echocardiography is the most appropriate next step, though in clinical practice, **treatment with IVIG and high-dose aspirin should be initiated promptly** (ideally within 10 days of fever onset) and should not be delayed pending echocardiography results.
*HHV-6 immunoglobulin M (IgM) detection*
- **Human Herpesvirus 6 (HHV-6)** causes **roseola infantum** (exanthem subitum), which presents with high fever for 3-5 days followed by a rash that appears **as the fever resolves**.
- The mucocutaneous findings in this case (strawberry tongue, cracked lips, conjunctival injection, extremity swelling) are not consistent with roseola.
*ANA measurement*
- **Antinuclear antibody (ANA)** testing screens for **autoimmune diseases** such as systemic lupus erythematosus or juvenile idiopathic arthritis.
- While this patient has fever and joint pain, the specific mucocutaneous changes (strawberry tongue, cracked lips, conjunctival injection, polymorphous rash, extremity edema) and cervical lymphadenopathy are pathognomonic for Kawasaki disease, not typical autoimmune conditions.
*Monospot test*
- The **Monospot test** diagnoses **infectious mononucleosis** caused by **Epstein-Barr virus (EBV)**.
- While EBV can cause fever, rash, and lymphadenopathy (typically posterior cervical), the characteristic mucocutaneous findings of Kawasaki disease (strawberry tongue, cracked lips, conjunctival injection without exudate, extremity changes) are not seen in mononucleosis.
- Additionally, mononucleosis is uncommon in preschool-aged children.
*Antistreptolysin O titer measurement*
- **Antistreptolysin O (ASO) titer** detects recent **Group A Streptococcus** infection and can support a diagnosis of **acute rheumatic fever (ARF)**.
- ARF presents with migratory polyarthritis, carditis, and **erythema marginatum** (not a polymorphous rash), occurring 2-4 weeks after streptococcal pharyngitis.
- The mucocutaneous features in this case are specific to Kawasaki disease and not consistent with ARF.
Cardiac complications and evaluation US Medical PG Question 5: A 44-year-old woman comes to the physician because of progressively worsening shortness of breath with exertion and intermittent palpitations over the last 2 months. She has had neither chest pain nor a cough. Her pulse is 124/min and irregular. Physical examination shows a grade 4/6 high-pitched holosystolic murmur that is best heard at the apex and radiates to the back. The murmur increases in intensity when she clenches her hands into fists. The lungs are clear to auscultation. Further evaluation of this patient is most likely to show which of the following findings?
- A. Obstruction of the right marginal artery on coronary angiogram
- B. Diffuse ST elevations on electrocardiogram
- C. Dilation of left atrium on echocardiogram (Correct Answer)
- D. Reversible area of myocardial ischemia on nuclear stress test
- E. Pulmonary artery thrombus on computed tomography scan
Cardiac complications and evaluation Explanation: ***Dilation of left atrium on echocardiogram***
- The patient's symptoms of **shortness of breath**, **palpitations**, and an **irregular pulse** suggest a cardiac etiology, specifically a **valvular problem**. The **holosystolic murmur** best heard at the **apex** and radiating to the **back**, which increases with handgrip (a maneuver that increases afterload), is highly characteristic of **mitral regurgitation**.
- **Chronic mitral regurgitation** leads to **volume overload** in the left atrium, causing its **dilation** as it tries to accommodate the increased blood flow from both the pulmonary veins and the regurgitant jet from the left ventricle. This can also lead to **atrial fibrillation**, explaining the irregular pulse and palpitations.
*Obstruction of the right marginal artery on coronary angiogram*
- This finding would indicate **coronary artery disease** affecting the right coronary artery, typically presenting with **chest pain** or angina, which the patient explicitly denies.
- While coronary artery disease can cause shortness of breath, the distinctive **holosystolic murmur** and its radiation are not primary features of isolated coronary artery obstruction.
*Diffuse ST elevations on electrocardiogram*
- **Diffuse ST elevations** are typically seen in conditions like **pericarditis**, which often presents with pleuritic chest pain and a pericardial friction rub, none of which are described.
- It could also indicate an ST-elevation myocardial infarction (STEMI), but the 2-month history and the specific murmur point away from an acute coronary event.
*Reversible area of myocardial ischemia on nuclear stress test*
- This would suggest **ischemic heart disease**, again primarily indicated by **angina** or exertional chest discomfort, which is absent in this patient.
- While ischemia can cause shortness of breath and palpitations, it does not explain the characteristic **holosystolic murmur** and its specific radiation.
*Pulmonary artery thrombus on computed tomography scan*
- A **pulmonary artery thrombus** (pulmonary embolism) would typically cause **acute dyspnea**, pleuritic chest pain, and sometimes hemoptysis, which are not mentioned.
- While it can cause palpitations and an irregular pulse (due to right heart strain), it does not account for the **holosystolic murmur** heard at the apex and radiating to the back.
Cardiac complications and evaluation US Medical PG Question 6: A 3-year-old boy is brought to the physician for evaluation of developmental delay. He could sit alone at 12 months and started walking with support at the age of 2 years. He can name only very few familiar objects and uses simple two-word sentences. He cannot stack more than 2 blocks. His parents report that he does not like playing with other children. He is at the 80th percentile for head circumference, 85th percentile for height, and 50th percentile for weight. He has a long and narrow face as well as large protruding ears. His thumbs can be passively flexed to the ipsilateral forearm. This patient is at increased risk of developing which of the following conditions?
- A. Mitral regurgitation (Correct Answer)
- B. Type 2 diabetes mellitus
- C. Acute myeloid leukemia
- D. Aortic dissection
- E. Hyperuricemia
Cardiac complications and evaluation Explanation: ***Mitral regurgitation***
- The patient's presentation with **developmental delay**, **relatively large head circumference** (80th percentile), **long narrow face**, **large protruding ears**, and **hyperextensible joints** (thumbs to forearm) is highly suggestive of **fragile X syndrome**.
- **Mitral valve prolapse** leading to **mitral regurgitation** is a common cardiac manifestation of fragile X syndrome, occurring in **50-80% of adult males** with the condition, due to **connective tissue dysplasia**.
*Type 2 diabetes mellitus*
- This condition is primarily associated with **obesity**, **insulin resistance**, and genetic predispositions unrelated to the features presented in this patient.
- While fragile X patients may have general health concerns, there is **no specific increased risk** of developing type 2 diabetes mellitus directly linked to the syndrome's pathology.
*Acute myeloid leukemia*
- There is **no established association** between fragile X syndrome and an increased risk of developing **acute myeloid leukemia**.
- AML is a **hematologic malignancy** with different risk factors, such as exposure to certain chemicals or prior chemotherapy.
*Aortic dissection*
- Aortic dissection is typically associated with conditions affecting **connective tissue** like **Marfan syndrome** or **Ehlers-Danlos syndrome**, or with **hypertension**.
- While fragile X syndrome involves connective tissue abnormalities, **aortic dissection is not a typical or significantly increased risk** compared to other connective tissue disorders.
*Hyperuricemia*
- **Hyperuricemia** is most commonly associated with conditions like **gout**, **kidney disease**, or certain **genetic metabolic disorders** (e.g., Lesch-Nyhan syndrome).
- There is **no direct link** between fragile X syndrome and an increased risk of hyperuricemia.
Cardiac complications and evaluation US Medical PG Question 7: A 3-month-old male presents to the pediatrician with his mother for a well child visit. The patient drinks 4 ounces of conventional cow’s milk formula every three hours. He usually stools once per day, and urinates up to six times per day. His mother reports that he regurgitates a moderate amount of formula through his nose and mouth after most feeds. He does not seem interested in additional feeding after these episodes of regurgitation, and he has become progressively more irritable around meal times. The patient is starting to refuse some feeds. His mother denies ever seeing blood or streaks of red in his stool, and she denies any family history of food allergies or dermatological problems. The patient’s weight was in the 75th percentile for weight throughout the first month of life. Four weeks ago, he was in the 62nd percentile, and he is now in the 48th percentile. His height and head circumference have followed similar trends. On physical exam, the patient smiles reciprocally and can lift his head and chest when in the prone position. His abdomen is soft, non-tender, and non-distended.
Which of the following is the best next step in management?
- A. Switch to hydrolyzed formula
- B. Obtain abdominal ultrasound
- C. Initiate proton pump inhibitor
- D. Provide reassurance
- E. Counsel on positioning and thickening feeds (Correct Answer)
Cardiac complications and evaluation Explanation: ***Counsel on positioning and thickening feeds***
- The infant's symptoms, including **regurgitation**, **irritability during feeds**, and **dropping weight percentiles**, are indicative of severe gastroesophageal reflux (GER). Initial management should focus on **conservative measures** like positioning modifications (keeping upright after feeds), thickening feeds, and smaller, more frequent feedings.
- Given the absence of **hematemesis**, **hematochezia**, or **projectile vomiting**, further invasive diagnostics or medication are not immediately warranted.
*Switch to hydrolyzed formula*
- This would be considered if there were signs suggestive of a **cow's milk protein allergy**, such as **bloody stools**, **diarrhea**, **eczema**, or a strong family history of allergies, which are all absent in this case.
- Allergy is less likely to be the primary cause of isolated severe regurgitation with failure to thrive without other allergic manifestations.
*Obtain abdominal ultrasound*
- An **abdominal ultrasound** is primarily used to evaluate for conditions like **pyloric stenosis** if there is **projectile vomiting**, an **olive-shaped mass**, or severe dehydration and electrolyte imbalances, none of which are present.
- While it can assess for **malrotation or intussusception**, these conditions typically present with more acute, severe symptoms like **bilious vomiting**, abdominal distension, or currant jelly stools, which are not described.
*Initiate proton pump inhibitor*
- **Proton pump inhibitors (PPIs)** are reserved for infants with confirmed **erosive esophagitis** or severe symptoms unresponsive to lifestyle modifications.
- Starting a PPI without first attempting conservative measures or confirming pathological acid reflux is generally not recommended, especially given potential side effects like increased risk of infections.
*Provide reassurance*
- While **reassurance** is important, it is not the sole appropriate next step. The infant's **dropping weight percentiles** and significant feeding difficulties suggest that this is beyond typical "spitting up" and requires intervention to prevent further impact on growth and comfort.
- Simply reassuring the mother would ignore the clinical signs of **failure to thrive** and significant discomfort during feeds.
Cardiac complications and evaluation US Medical PG Question 8: A 4-year-old boy is brought to the physician by his parents because of fever and mild abdominal pain for 7 days. His parents report that he developed a rash 2 days ago. He has had no diarrhea or vomiting. Four weeks ago, he returned from a camping trip to Colorado with his family. His immunization records are unavailable. His temperature is 39.4°C (102.9°F), pulse is 111/min, respirations are 27/min, and blood pressure is 96/65 mm Hg. Examination shows bilateral conjunctival injections and fissures on his lower lips. The pharynx is erythematous. There is tender cervical lymphadenopathy. The hands and feet appear edematous. A macular morbilliform rash is present over the trunk. Bilateral knee joints are swollen and tender; range of motion is limited by pain. Which of the following is the most appropriate treatment for this patient's condition?
- A. Supportive treatment only
- B. Intravenous immunoglobulin (Correct Answer)
- C. Oral ibuprofen
- D. Oral penicillin
- E. Oral doxycycline
Cardiac complications and evaluation Explanation: ***Intravenous immunoglobulin***
- This patient presents with symptoms highly suggestive of **Kawasaki disease**, including a persistent fever for over 5 days, **bilateral conjunctival injection**, **lip fissures**, **erythematous pharynx**, **cervical lymphadenopathy**, and **edema of hands and feet** followed by a rash.
- **IV immunoglobulin (IVIG)** is the cornerstone of treatment for Kawasaki disease, significantly reducing the risk of **coronary artery aneurysms** if given early in the disease course.
*Supportive treatment only*
- While supportive care (fever reduction, hydration) is important, relying solely on it for **Kawasaki disease** would increase the risk of severe complications, particularly **coronary artery involvement**.
- **Kawasaki disease** is a systemic vasculitis requiring specific immunomodulatory therapy to prevent long-term cardiac sequelae.
*Oral ibuprofen*
- **Ibuprofen**, a non-steroidal anti-inflammatory drug (**NSAID**), can help manage fever and joint pain, but it does not address the underlying **vasculitis** or prevent the cardiac complications of **Kawasaki disease**.
- **Aspirin** (high-dose initially, then low-dose) is part of Kawasaki disease treatment, but ibuprofen alone is insufficient as primary therapy.
*Oral penicillin*
- **Penicillin** is an antibiotic used to treat bacterial infections, such as **streptococcal pharyngitis**.
- This patient's symptoms are inconsistent with a typical bacterial infection requiring penicillin and are more indicative of a **systemic inflammatory condition** like Kawasaki disease, which is not bacterial.
*Oral doxycycline*
- **Doxycycline** is an antibiotic often used for **rickettsial infections** (e.g., Rocky Mountain spotted fever) or Lyme disease, which might be considered given the camping trip.
- However, the classic constellation of symptoms (conjunctival injection, lip changes, edema of extremities, diffuse rash) points strongly away from these and towards **Kawasaki disease**, for which doxycycline is ineffective.
Cardiac complications and evaluation US Medical PG Question 9: A 4-year-old boy is brought to a pediatrician by his parents with a history of fever for the last 5 days and irritability, decreased appetite, vomiting, and swelling of the hands and feet for the last 3 days. The patient’s mother mentions that he has been taking antibiotics and antipyretics prescribed by another physician for the last 3 days, but there has been no improvement His temperature is 39.4°C (103.0°F), pulse is 128/min, respiratory rate is 24/min, and blood pressure is 96/64 mm Hg. On physical examination, there is significant edema of the hands and feet bilaterally. There is a 2.5 cm diameter freely moveable, nontender cervical lymph node is palpable on the right side. A strawberry tongue and perianal erythema are noted. Conjunctival injection is present bilaterally. Laboratory findings reveal mild anemia and a leukocytosis with a left-shift. Erythrocyte sedimentation rate (ESR) and serum C-reactive protein (CRP) are increased. If not treated appropriately, this patient is at increased risk of developing which of the following complications?
- A. Lower gastrointestinal hemorrhage
- B. Coronary artery ectasia (Correct Answer)
- C. Acute renal failure
- D. Pulmonary embolism
- E. Acute disseminated encephalomyelitis (ADEM)
Cardiac complications and evaluation Explanation: ***Coronary artery ectasia***
- The patient's symptoms, including **prolonged fever**, **conjunctival injection**, **strawberry tongue**, **cervical lymphadenopathy**, **edema of hands and feet**, and **perianal erythema**, are characteristic of **Kawasaki disease**.
- If left untreated, **Kawasaki disease** can lead to significant cardiovascular complications, most notably **coronary artery aneurysms** or ectasia, due to vasculitis of medium-sized arteries.
*Lower gastrointestinal hemorrhage*
- While **gastrointestinal symptoms** such as vomiting and diarrhea can occur in **Kawasaki disease**, severe complications like **lower gastrointestinal hemorrhage** are rare and not the most common or critical untreated complication.
- Other conditions, like **Meckel's diverticulum** or **inflammatory bowel disease**, are more typically associated with lower GI hemorrhage in children.
*Acute renal failure*
- **Renal involvement** in **Kawasaki disease** is uncommon and usually presents as **mild proteinuria** or **sterile pyuria**; **acute renal failure** is an extremely rare complication.
- Significant renal dysfunction is more commonly seen in conditions like **hemolytic-uremic syndrome** or severe dehydration.
*Pulmonary embolism*
- **Pulmonary embolism** is rare in young children and not a typical complication of untreated **Kawasaki disease**.
- It is more commonly associated with conditions causing **hypercoagulability** or prolonged immobility.
*Acute disseminated encephalomyelitis (ADEM)*
- **ADEM** is an **immune-mediated demyelinating disorder** of the central nervous system that typically follows an infection or vaccination.
- It is not a recognized complication of untreated **Kawasaki disease**, whose primary pathology involves systemic vasculitis.
Cardiac complications and evaluation US Medical PG Question 10: A 5-year-old girl presents with a rash and a persistent fever of 41.0°C (105.8°F), not relieved by Tylenol. The patient's mother says that her symptoms started 5 days ago and have not improved. The rash started on her trunk and now is present everywhere including the palms and soles. Her birth history is normal. Her pulse is 120/min and respiratory rate is 22/min. On physical examination, the patient is agitated and ill-appearing. There is significant swelling of the distal upper and lower extremities bilaterally. The pharynx is hyperemic (see image). Generalized edema with palpable cervical lymphadenopathy is noted. Muscle tone is normal. Remainder of exam is unremarkable. Laboratory findings are significant for the following:
Laboratory test
Hb 9 g/dL
RBC 3.3/mm3
Neutrophilic leukocytosis 28,000/mm3
Normal platelet count 200,000/mm3
Serum ɣ-GT increased
Hyperbilirubinemia 2.98 mg/dL
AST and ALT are normal, but there is markedly increased serum CRP. Which of the following is the most likely diagnosis in this patient?
- A. Juvenile rheumatoid arthritis
- B. Scarlet fever
- C. Adenovirus infection
- D. Staphylococcal scalded skin syndrome
- E. Kawasaki disease (Correct Answer)
Cardiac complications and evaluation Explanation: ***Kawasaki disease***
- The constellation of **prolonged fever, rash (including palms and soles), swollen extremities, hyperemic pharynx, and cervical lymphadenopathy** in a young child is highly suggestive of **Kawasaki disease**.
- Laboratory findings such as **neutrophilic leukocytosis, elevated CRP, and increased γ-GT** further support this diagnosis, which is a **vasculitis** of medium-sized arteries.
*Juvenile rheumatoid arthritis*
- While juvenile rheumatoid arthritis (JRA) can cause **fever and joint swelling**, it typically does not present with the specific rash distribution, **hyperemic pharynx**, or **cervical lymphadenopathy** seen in this patient.
- The **acute onset and severity** of systemic symptoms are more characteristic of Kawasaki disease than typical JRA.
*Scarlet fever*
- Scarlet fever is caused by *Streptococcus pyogenes* and presents with a characteristic **sandpaper-like rash**, **strawberry tongue**, and **fever**.
- It does not typically cause **swelling of the extremities** or the specific laboratory abnormalities like **increased γ-GT** as seen here, and the rash of Kawasaki disease is often polymorphous rather than sandpaper-like.
*Adenovirus infection*
- Adenovirus infections can cause **fever, pharyngitis, and conjunctivitis**, but they do not typically lead to the characteristic widespread rash (including palms and soles), marked **extremity swelling**, or significantly elevated inflammatory markers observed in this case.
- The clinical picture presented is much more severe and specific for a systemic inflammatory condition.
*Staphylococcal scalded skin syndrome*
- **Staphylococcal scalded skin syndrome (SSSS)** is characterized by **erythema and superficial blistering/peeling of the skin**, giving a "scalded" appearance, often starting around the mouth.
- It does not typically cause the **hyperemic pharynx, swollen extremities, or cervical lymphadenopathy** described, and the rash in this patient is not described as blistering or peeling.
More Cardiac complications and evaluation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.