Atypical Kawasaki presentation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Atypical Kawasaki presentation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Atypical Kawasaki presentation US Medical PG Question 1: A 6-year-old boy presents to his pediatrician accompanied by his mother for evaluation of a rash. The rash appeared a little over a week ago, and since that time the boy has felt tired. He is less interested in playing outside, preferring to remain indoors because his knees and stomach hurt. His past medical history is significant for an upper respiratory infection that resolved uneventfully without treatment 2 weeks ago. Temperature is 99.5°F (37.5°C), blood pressure is 115/70 mmHg, pulse is 90/min, and respirations are 18/min. Physical exam shows scattered maroon macules and papules on the lower extremities. The abdomen is diffusely tender to palpation. There is no cervical lymphadenopathy or conjunctival injection. Which of the following will most likely be found in this patient?
- A. Coronary artery aneurysms
- B. Leukocytoclastic vasculitis (Correct Answer)
- C. Thrombocytopenia
- D. Mitral regurgitation
- E. Occult malignancy
Atypical Kawasaki presentation Explanation: ***Leukocytoclastic vasculitis***
- This patient presents with symptoms highly suggestive of **Henoch-Schönlein Purpura (HSP)**, including a preceding URI, fatigue, low-grade fever, **abdominal pain**, and a **palpable purpura** primarily on the lower extremities.
- HSP is characterized by IgA-mediated **small-vessel vasculitis**, which histologically presents as leukocytoclastic vasculitis with IgA deposition on immunofluorescence.
*Coronary artery aneurysms*
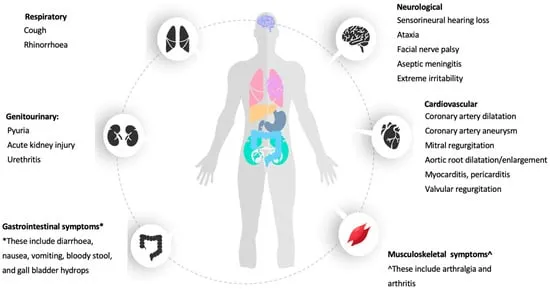
- **Coronary artery aneurysms** are a classic complication of **Kawasaki disease**, not Henoch-Schönlein Purpura.
- Kawasaki disease presents with different clinical features, including prolonged fever, conjunctival injection, oral changes, and cervical lymphadenopathy.
*Thrombocytopenia*
- **Thrombocytopenia** is characterized by a low platelet count and often presents with petechiae, purpura, and bleeding, but the rash in HSP is due to inflammation and extravasation of red blood cells, not low platelets.
- Platelet counts in HSP are typically **normal** or can be slightly elevated as an acute phase reactant.
*Mitral regurgitation*
- **Mitral regurgitation** is a common manifestation of **rheumatic fever**, particularly after recurrent episodes, caused by valvular damage.
- Rheumatic fever is also preceded by infection (Group A Strep) but involves different symptoms like migratory polyarthritis, carditis, chorea, erythema marginatum, and subcutaneous nodules, which are not described here.
*Occult malignancy*
- While an **occult malignancy** can cause paraneoplastic syndromes or constitutional symptoms, the specific constellation of symptoms, including the migratory rash, abdominal pain, and preceding URI, points much more strongly to **HSP** in a 6-year-old.
- The presentation is more consistent with an acute, inflammatory process rather than a chronic, insidious malignant one.
Atypical Kawasaki presentation US Medical PG Question 2: A 9-year-old boy is brought to the emergency department because of progressively worsening shortness of breath for 3 days. He has had fever and malaise for the past 5 days. He had a sore throat 3 weeks ago that resolved without treatment. He appears ill. His temperature is 38.6°C (101.5°F), pulse is 98/min and blood pressure is 84/62 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 93%. Examination shows jugular venous distension and bilateral ankle edema. There are erythematous, ring-shaped macules and patches over his trunk that are well-demarcated. Auscultation of the chest shows crackles at the lung bases bilaterally. An S3 is heard on cardiac auscultation. His hemoglobin concentration is 12.2 g/dL, leukocyte count is 13,600/mm3, and platelet count is 280,000/mm3. A urinalysis is normal. An x-ray of the chest shows cardiac silhouette enlargement with prominent vascular markings in both the lung fields. Which of the following is the most likely etiology of this patient's symptoms?
- A. Systemic lupus erythematosus
- B. Acute rheumatic fever (Correct Answer)
- C. Kawasaki disease
- D. Viral myocarditis
- E. Infection with Borrelia burgdorferi
Atypical Kawasaki presentation Explanation: ***Acute rheumatic fever***
- This patient presents with signs of cardiac involvement (**shortness of breath**, **S3 gallop**, **cardiomegaly**, **pulmonary edema**), a history of a recent **strep throat infection**, and **erythema marginatum** (the ring-shaped rash), all consistent with **acute rheumatic fever**.
- **Acute rheumatic fever** is a delayed, non-suppurative complication of Group A Streptococcus pharyngitis, leading to systemic inflammation, particularly affecting the heart, joints, brain, and skin.
*Systemic lupus erythematosus*
- SLE can cause cardiac complications like pericarditis or myocarditis, but the characteristic rash of SLE (malar or discoid) differs from the described **erythema marginatum**.
- While SLE can cause systemic symptoms, the clear history of a preceding **sore throat** and the specific rash point away from SLE.
*Kawasaki disease*
- Kawasaki disease primarily affects **children under 5 years old** and is characterized by fever, conjunctivitis, oral changes, rash, lymphadenopathy, and extreme irritability.
- The patient's age (9 years) and the specific rash described (erythema marginatum) are not typical for Kawasaki disease.
*Viral myocarditis*
- Viral myocarditis can cause **heart failure** symptoms (shortness of breath, S3, cardiomegaly), but it typically lacks the preceding **sore throat** and the specific skin findings of **erythema marginatum** seen in this patient.
- While a viral infection could cause myocarditis, the constellation of symptoms points strongly to a specific post-streptococcal etiology.
*Infection with Borrelia burgdorferi*
- *Borrelia burgdorferi* (Lyme disease) can cause cardiac manifestations like **carditis** (often AV block) and a characteristic rash called **erythema migrans**.
- However, **erythema migrans** is typically a single, expanding bull's-eye rash, which is different from the described **erythematous, ring-shaped macules and patches** of erythema marginatum.
Atypical Kawasaki presentation US Medical PG Question 3: A 4-year-old boy is brought to the emergency department by his parents after 10 days of fever, varying from 38.0–40.0°C (100.4–104.0°F). On physical examination, the child is ill-looking with an extensive rash over his trunk with patchy desquamation. His hands are swollen, and he also shows signs of a bilateral conjunctivitis. The laboratory test results are as follows:
Hemoglobin 12.9 g/dL
Hematocrit 37.7%
Mean corpuscular volume 82.2 μm3
Leukocyte count 10,500/mm3
Neutrophils 65%
Lymphocytes 30%
Monocytes 5%
Platelet count 290,000/mm3
Erythrocyte sedimentation rate (ESR) 35 mm/h
What is the next best step in the management of this patient’s condition?
- A. High-dose aspirin (Correct Answer)
- B. Influenza vaccine
- C. Echocardiography
- D. Low-dose aspirin
- E. Corticosteroids
Atypical Kawasaki presentation Explanation: ***High-dose aspirin***
- This patient presents with classic **Kawasaki disease**: prolonged fever (10 days), bilateral conjunctivitis, rash with desquamation, and extremity changes (swollen hands).
- Standard treatment for Kawasaki disease includes **IVIG (2 g/kg) plus high-dose aspirin (80-100 mg/kg/day)**. While both should be given together, **high-dose aspirin** is the best *therapeutic* option among those listed.
- High-dose aspirin provides anti-inflammatory effects during the acute phase and helps reduce fever and systemic inflammation.
- Treatment should be initiated promptly (ideally within 10 days of fever onset) to reduce the risk of **coronary artery aneurysms**.
*Influenza vaccine*
- The influenza vaccine is not a treatment for acute illness and has no role in managing Kawasaki disease.
- Vaccination would not address the ongoing systemic inflammation or prevent cardiac complications.
*Echocardiography*
- **Echocardiography should be performed** in all cases of Kawasaki disease to assess for coronary artery abnormalities, both at diagnosis and during follow-up.
- However, it is a **diagnostic/monitoring tool**, not a therapeutic intervention. Medical treatment to reduce inflammation takes priority over imaging.
- The question asks for the "next best step in management," which implies therapeutic action rather than diagnostic testing.
*Low-dose aspirin*
- Low-dose aspirin (3-5 mg/kg/day) is used during the **convalescent phase** for its antiplatelet effects, typically after fever resolution.
- It is transitioned to after the acute inflammatory phase is controlled with high-dose aspirin.
- Not appropriate for initial acute management where anti-inflammatory dosing is needed.
*Corticosteroids*
- Corticosteroids are reserved for **IVIG-refractory cases** or patients with severe coronary artery involvement.
- They are not part of initial first-line therapy and should not be used before IVIG administration.
- Their use is indicated only when standard therapy fails.
Atypical Kawasaki presentation US Medical PG Question 4: A 2-year-old girl is brought to her pediatrician’s office with intermittent and severe stomach ache and vomiting for the last 2 days. Last week the whole family had a stomach bug involving a few days of mild fever, lack of appetite, and diarrhea but they have all made a full recovery since. This current pain is different from the type she had during infection. With the onset of pain, the child cries and kicks her legs up in the air or pulls them to her chest. The parents have also observed mucousy stools and occasional bloody stools that are bright red and mucousy. After a while, the pain subsides and she returns to her normal activity. Which of the following would be the next step in the management of this patient?
- A. Abdominal radiograph
- B. Air enema (Correct Answer)
- C. Abdominal CT scan
- D. Surgical reduction
- E. Observe for 24 hours
Atypical Kawasaki presentation Explanation: ***Air enema***
- The clinical presentation with intermittent abdominal pain, leg drawing to the chest, "currant jelly" stools (bloody and mucousy), and a recent viral illness is highly suggestive of **intussusception**. An **air enema** is the diagnostic and therapeutic modality of choice for intussusception.
- It uses pneumatic pressure to reduce the telescoping of the bowel, and if successful, avoids the need for surgery.
*Abdominal radiograph*
- An **abdominal radiograph** may show signs of obstruction or a "target sign" (if present), but it is not sensitive or specific enough to definitively diagnose intussusception.
- It is primarily used to rule out perforation before performing an air enema if there are concerns about peritonitis.
*Abdominal CT scan*
- While an **abdominal CT scan** can diagnose intussusception, it exposes the child to significant radiation and is not typically the first-line imaging modality.
- It is usually reserved for cases where other diagnostic methods are inconclusive or if complications like perforation are suspected.
*Surgical reduction*
- **Surgical reduction** is indicated if an air enema fails to reduce the intussusception, if there are signs of bowel perforation or peritonitis, or if the patient is unstable.
- It is an invasive procedure and should not be the initial step in management unless there are clear contraindications to pneumatic reduction.
*Observe for 24 hours*
- Observing the child for 24 hours without intervention is inappropriate and can lead to serious complications, such as **bowel ischemia, necrosis, perforation, and sepsis**.
- Intussusception is a medical emergency that requires prompt diagnosis and treatment.
Atypical Kawasaki presentation US Medical PG Question 5: A 2-year-old boy is brought to the emergency department by his parents because of facial swelling that has now progressed to total body swelling. He also complains of nausea and abdominal pain. The child was in his usual state of health a week ago when they first notice swelling around his eyes. A few days later his legs started to swell. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. Today, his blood pressure is 104/60 mm Hg, the heart rate is 90/min, the respiratory rate is 25/min, and the temperature is 37.1°C (98.8°F). On examination, he has facial edema, abdominal shifting dullness, and bilateral leg edema up to the knees. Urine dipstick shows 4+ protein and urinalysis shows fatty casts. Serum albumin is 2.2 g/dL. Which of the following is the most likely etiology of this patient condition?
- A. Acute glomerulonephritis
- B. Minimal change disease (Correct Answer)
- C. Congestive heart failure
- D. Kwashiorkor
- E. Protein-losing enteropathy
Atypical Kawasaki presentation Explanation: ***Minimal change disease***
- This patient presents with **generalized edema**, **heavy proteinuria** (4+ protein with fatty casts), and **hypoalbuminemia** (< 2.5 g/dL), classic findings of **nephrotic syndrome**.
- **Minimal change disease** is the most common cause of nephrotic syndrome in children, typically presenting between 2 and 6 years of age, matching the patient's age and clinical picture.
*Acute glomerulonephritis*
- This condition is typically characterized by **hematuria**, **hypertension**, and **mild proteinuria**, often following a streptococcal infection.
- The patient's presentation with **massive proteinuria** and absence of hematuria or significant hypertension makes acute glomerulonephritis less likely.
*Congestive heart failure*
- While CHF can cause edema, it is usually accompanied by signs of **cardiac dysfunction** such as tachycardia, tachypnea, and an enlarged heart on imaging, which are not described.
- The primary cause of edema in CHF is **fluid overload** due to impaired cardiac output, not massive proteinuria and hypoalbuminemia as seen here.
*Kwashiorkor*
- This is a form of **severe protein malnutrition** leading to edema and abdominal distension, often seen in regions with food scarcity.
- The clinical context does not suggest malnutrition, and the presence of **heavy proteinuria** points to a renal pathology rather than a primary nutritional deficiency.
*Protein-losing enteropathy*
- This condition involves excessive protein loss through the **gastrointestinal tract**, leading to hypoalbuminemia and edema.
- However, it typically presents with **diarrhea** and malabsorption symptoms, which are not reported in this patient.
Atypical Kawasaki presentation US Medical PG Question 6: A 9-month-old boy is brought to the physician because of increased irritability, continual crying, and fever for 1 day. His mother has noticed that he refuses to lie down on his right side and keeps tugging at his right ear. One week ago, he had a runny nose that has since improved. He was born at term and has been otherwise healthy. He was exclusively breastfed until 2 months of age and is currently bottle-fed with some solid foods introduced. He has been attending a daycare center for the past 5 months. His temperature is 38.4°C (101.1°F) and pulse is 144/min. Otoscopic examination in this child is most likely to show which of the following?
- A. Erythematous external auditory canal
- B. Vesicles in the ear canal
- C. Bulging erythematous tympanic membrane (Correct Answer)
- D. Brown mass within the ear canal
- E. Retracted opacified tympanic membrane
Atypical Kawasaki presentation Explanation: ***Bulging erythematous tympanic membrane***
- The child's symptoms of **irritability**, **crying**, **fever**, **ear tugging**, and refusal to lie on one side, especially after a recent upper respiratory infection, are highly suggestive of **acute otitis media (AOM)**.
- In AOM, the **tympanic membrane (eardrum)** becomes inflamed, red (**erythematous**), and often **bulges** outwards due to the accumulation of fluid and pus in the middle ear.
*Erythematous external auditory canal*
- An **erythematous external auditory canal** is characteristic of **otitis externa** (swimmer's ear), which typically presents with pain upon manipulation of the tragus or pinna, and discharge, rather than the systemic symptoms like fever and irritability seen here.
- While some inflammation may extend to the external canal in AOM, the primary and most diagnostic finding for AOM is changes to the tympanic membrane itself.
*Vesicles in the ear canal*
- **Vesicles** in the ear canal or on the tympanic membrane, often accompanied by severe pain and possibly facial nerve palsy, are characteristic of **herpes zoster oticus** (Ramsay Hunt syndrome).
- This condition is caused by viral reactivation and does not fit the common presentation of fever, irritability, and ear tugging in an infant following a runny nose.
*Brown mass within the ear canal*
- A **brown mass** within the ear canal could indicate a cerumen impaction (earwax plug), a foreign body, or potentially a **cholesteatoma** (a benign skin growth that can erode bone).
- None of these conditions typically present with acute onset fever, irritability, and ear tugging in an infant, nor do they usually follow a recent upper respiratory infection.
*Retracted opacified tympanic membrane*
- A **retracted and opacified tympanic membrane** suggests changes in middle ear pressure, often seen in **eustachian tube dysfunction** or **otitis media with effusion (OME)**, where there is fluid but no acute infection.
- While OME can precede AOM, the presence of fever, acute irritability, and significant pain (implied by ear tugging and refusal to lie down) points strongly to an active, acute infection rather than just effusion or retraction.
Atypical Kawasaki presentation US Medical PG Question 7: An 11-month-old boy presents with the recent loss of appetite and inability to gain weight. His diet consists mainly of cow’s milk and fruits. Family history is unremarkable. Physical examination shows conjunctival pallor. Laboratory findings are significant for the following:
Hemoglobin 9.1 g/dL
Mean corpuscular volume 75 μm3
Mean corpuscular hemoglobin 20 pg/cell
Red cell distribution width 18%
The patient is presumptively diagnosed with iron deficiency anemia (IDA) and ferrous sulfate syrup is prescribed. Which of the following laboratory values would most likely change 1st in response to this treatment?
- A. ↓ Mentzer index
- B. ↑ mean corpuscular hemoglobin
- C. ↑ reticulocyte count (Correct Answer)
- D. Normalization of hemoglobin
- E. ↓ Anisocytosis
Atypical Kawasaki presentation Explanation: ***↑ reticulocyte count***
- An increase in the **reticulocyte count** is the earliest sign of a bone marrow response to iron supplementation. Reticulocytes are immature red blood cells, and their production rapidly increases as the bone marrow utilizes available iron to make new healthy red blood cells.
- This typically occurs within **3-7 days** of initiating iron therapy, reflecting effective erythropoiesis before changes in hemoglobin or other red cell indices become apparent.
*↓ Mentzer index*
- The **Mentzer index** is used to differentiate between iron deficiency anemia and thalassemia trait; it is not a direct measure of treatment response.
- A low Mentzer index (MCV/RBC count < 13) suggests thalassemia, while a high index (MCV/RBC count > 13) suggests iron deficiency. This value would not be the first to change post-treatment.
*↑ mean corpuscular hemoglobin*
- **Mean corpuscular hemoglobin (MCH)** reflects the average amount of hemoglobin in a single red blood cell. While it will eventually increase with successful treatment, this change occurs after the reticulocyte count elevation.
- MCH improvement signifies the production of fully hemoglobinized red blood cells, which takes longer than the initial surge in immature red cell release.
*Normalization of hemoglobin*
- **Hemoglobin levels** will gradually rise and normalize with effective iron therapy, typically over several weeks to months.
- This is a later indicator of treatment success, occurring after the initial reticulocytosis.
*↓ Anisocytosis*
- **Anisocytosis** refers to variation in red blood cell size, measured by **red cell distribution width (RDW)**. In iron deficiency anemia, RDW is typically elevated.
- While RDW will eventually decrease as the red blood cell population becomes more uniform with treatment, this change is not the earliest response. The initial production of new red cells can even temporarily increase RDW before it normalizes.
Atypical Kawasaki presentation US Medical PG Question 8: An 8-month-old girl is brought to the emergency department because of fever, vomiting, and diarrhea for 3 days. Her parents report at least 10 watery stools daily. She has had three upper respiratory tract infections since she started daycare 2 months ago, but has otherwise been developing normally. Her mother has a history of celiac disease. The patient is at the 57th percentile for height and the 65th percentile for weight. Her immunizations are incomplete. Her temperature is 38.5°C (101.3°F), pulse is 145/min, and blood pressure is 92/54 mm Hg. Examination shows dry mucous membranes and decreased skin turgor. Bowel sounds are hyperactive. A complete blood count and serum concentrations of glucose, urea nitrogen, and creatinine are within the reference range; there is hypokalemia. In addition to intravenous fluid resuscitation, which of the following is the most appropriate next step in management?
- A. Examination of the stool for ova and parasites
- B. Sonography of the abdomen
- C. Administration of antidiarrheal medication
- D. Enzyme immunoassay of stool (Correct Answer)
- E. Blood cultures
Atypical Kawasaki presentation Explanation: ***Enzyme immunoassay of stool***
- The patient presents with classic symptoms of **rotavirus gastroenteritis**, including fever, vomiting, and voluminous watery diarrhea, especially given her age, daycare exposure, and **incomplete immunization status** (missing rotavirus vaccine).
- **Enzyme immunoassay (EIA)** is a rapid, accurate test for detecting rotavirus antigens in stool, providing diagnosis confirmation within hours.
- While rotavirus gastroenteritis is managed primarily with **supportive care and rehydration** (already initiated), diagnostic testing is indicated here for: (1) **confirming the diagnosis** in an incompletely immunized child, (2) **infection control measures** in daycare/hospital settings, and (3) guiding parental counseling about immunization completion.
- EIA is the most appropriate next diagnostic step after stabilization has begun.
*Examination of the stool for ova and parasites*
- Stool O&P examination is appropriate for **persistent or chronic diarrhea** (>7-14 days), travel history, or suspected parasitic infection.
- Acute viral gastroenteritis typically presents with sudden onset of severe watery diarrhea, as seen here, rather than the more protracted course typical of parasitic infections.
- Parasitic causes are less likely in an otherwise healthy infant in a developed country without travel history.
*Sonography of the abdomen*
- **Abdominal sonography** would be indicated if there were concerns for **intussusception** (intermittent colicky pain, currant jelly stools, palpable mass) or other structural abnormalities.
- The patient's presentation with **diffuse watery diarrhea**, fever, and vomiting is classic for infectious gastroenteritis, not a surgical abdomen.
- Hyperactive bowel sounds further support an infectious rather than obstructive process.
*Administration of antidiarrheal medication*
- **Antidiarrheal medications are contraindicated** in infants and young children with acute infectious diarrhea.
- These agents (e.g., loperamide, bismuth subsalicylate) do not treat the underlying infection, can **prolong illness** by retaining pathogens, and risk serious complications including **toxic megacolon**, ileus, and CNS depression.
- The mainstay of treatment remains **oral or intravenous rehydration** and electrolyte replacement.
*Blood cultures*
- **Blood cultures** are indicated when there is concern for **bacteremia or sepsis**, typically suggested by high fever (>39°C), severe systemic toxicity, immunocompromise, or abnormal laboratory findings.
- This patient, while febrile, has **normal CBC, glucose, BUN, and creatinine**, making invasive bacterial infection less likely.
- The clinical picture is most consistent with **viral gastroenteritis**, which rarely causes bacteremia in immunocompetent children.
Atypical Kawasaki presentation US Medical PG Question 9: A 5-week-old male infant is brought to the Emergency Department with the complaint of vomiting. His parents state he has been unable to keep normal feedings down for the past week and now has projectile non-bilious vomiting after each meal. He was given a short course of oral erythromycin at 4 days of life for suspected bacterial conjunctivitis. Physical examination is significant for sunken fontanelles and dry mucous membranes. A palpable, ball shaped mass is noted just to the right of the epigastrium. Which of the following conditions is most likely in this patient?
- A. Milk-protein allergy
- B. Gastroesophageal reflux
- C. Intussusception
- D. Midgut volvulus
- E. Hypertrophic pyloric stenosis (Correct Answer)
Atypical Kawasaki presentation Explanation: ***Hypertrophic pyloric stenosis***
- The classic presentation includes **projectile non-bilious vomiting** in a 2-8 week old infant, a **palpable olive-shaped mass** in the epigastrium, and signs of **dehydration** (sunken fontanelles, dry mucous membranes).
- Exposure to **erythromycin** in early infancy is a recognized risk factor for developing pyloric stenosis due to its effect on gastrointestinal motility.
*Milk-protein allergy*
- Typically presents with symptoms like **bloody stools**, **diarrhea**, or **eczema**, rather than forceful projectile non-bilious vomiting.
- A palpable epigastric mass is not a feature of milk-protein allergy.
*Gastroesophageal reflux*
- While common in infants, GERD usually involves effortless spitting up or vomiting that is **not projectile** and generally **does not lead to significant dehydration** or a palpable mass.
- Symptoms tend to improve with age and positioning, unlike the progressive worsening seen here.
*Intussusception*
- Characterized by sudden onset of **crampy abdominal pain**, **currant jelly stools** (blood and mucus), and a sausage-shaped mass, usually in the right upper quadrant.
- The vomiting is typically **bilious** due to bowel obstruction, and it occurs later in presentation.
*Midgut volvulus*
- This is an acute surgical emergency presenting with sudden onset of **bilious vomiting** and signs of **intestinal obstruction**.
- It is associated with **malrotation** and can rapidly lead to bowel ischemia, which is a more severe and sudden presentation than described.
Atypical Kawasaki presentation US Medical PG Question 10: A 1-month-old boy is brought to the physician because of a 5-day history of generalized fatigue and multiple episodes of vomiting which is most pronounced after formula feeding. His vomiting progressed from 2–3 episodes on the first day to 6–8 episodes at present. The vomitus is whitish in color. The mother reports that he has been very hungry after each episode of vomiting. The patient was born at 38 weeks' gestation and weighed 3100 g (6 lb 13 oz); he currently weighs 3500 g (7 lb 11 oz). He appears irritable. His temperature is 37.1°C (98.8°F), pulse is 130/min, respirations are 43/min, and blood pressure is 74/36 mm Hg. Examination shows dry mucous membranes. The abdomen is soft and not distended. There is a round mass palpable in the epigastric region. The liver is palpated 1 cm below the right costal margin. Laboratory studies show:
Hemoglobin 15.3 g/dL
Leukocyte count 6300/mm3
Platelet count 230,000/mm3
Serum
Na+ 133 mEq/L
K+ 3.4 mEq/L
Cl- 92 mEq/L
Glucose 77 mg/dL
Creatinine 1.0 mg/dL
A urinalysis shows a decreased pH. Which of the following is the most appropriate next step in the management of this patient?
- A. Measure serum cortisol levels
- B. Perform upper GI endoscopy
- C. Administer IV 0.9% NaCl and replace electrolytes (Correct Answer)
- D. Perform emergency pyloromyotomy
- E. Obtain CT scan of the abdomen with contrast
Atypical Kawasaki presentation Explanation: ***Administer IV 0.9% NaCl and replace electrolytes***
- The patient exhibits signs of **dehydration** (dry mucous membranes, irritability) and **hypochloremic metabolic alkalosis** (low Na+ 133, K+ 3.4, Cl- 92) secondary to persistent vomiting.
- The clinical presentation strongly suggests **pyloric stenosis** (progressive non-bilious vomiting, palpable epigastric mass, hungry after vomiting), but the patient's **electrolyte imbalances and dehydration must be corrected before any surgical intervention** to minimize operative risks.
- The paradoxical aciduria (decreased urine pH) occurs because severe volume depletion triggers aldosterone secretion, leading to preferential H+ excretion over HCO3- despite metabolic alkalosis.
*Measure serum cortisol levels*
- While adrenal insufficiency can cause vomiting and electrolyte abnormalities, the specific presentation of **non-bilious vomiting** with an **epigastric mass** and **hunger after vomiting** strongly points to **pyloric stenosis**.
- There are no other clear signs of adrenal insufficiency such as **hyperpigmentation**, **significant hypoglycemia**, or **hyperkalemia** that would make this the immediate priority over correcting dehydration and electrolytes.
*Perform upper GI endoscopy*
- Upper GI endoscopy is primarily used to visualize the upper digestive tract for conditions like **esophagitis**, **gastritis**, or **ulcers**.
- It is not the initial diagnostic test for **pyloric stenosis**; an **abdominal ultrasound** is preferred for confirming the diagnosis (showing pyloric wall thickness >3mm and channel length >15mm).
- Correcting the patient's severe dehydration and electrolyte imbalances takes precedence over diagnostic procedures.
*Perform emergency pyloromyotomy*
- Although pyloric stenosis is strongly suspected and **pyloromyotomy** is the definitive treatment, it is an elective surgical procedure.
- The patient is currently **dehydrated** with **electrolyte abnormalities** (hypochloremic, hypokalemic metabolic alkalosis), which must be corrected *before* surgery to minimize anesthetic and surgical risks and improve outcomes.
- Pyloric stenosis is **not a surgical emergency**; stabilization always precedes surgery.
*Obtain CT scan of the abdomen with contrast*
- A CT scan uses **ionizing radiation** and **contrast agents**, which are generally avoided in infants unless absolutely necessary.
- An **abdominal ultrasound** is the diagnostic study of choice for **pyloric stenosis** due to its non-invasiveness, lack of radiation exposure, and effectiveness in identifying the characteristic hypertrophied pylorus ("olive" or "target sign").
More Atypical Kawasaki presentation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.