Acute phase management US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Acute phase management. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Acute phase management US Medical PG Question 1: A 74-year-old woman with no significant past medical history presents with 1 week of fever, unremitting headache and hip and shoulder stiffness. She denies any vision changes. Physical examination is remarkable for right scalp tenderness and range of motion is limited due to pain and stiffness. Neurological testing is normal. Laboratory studies are significant for an erythrocyte sedimentation rate (ESR) at 75 mm/h (normal range 0-22 mm/h for women). Which of the following is the most appropriate next step in management?
- A. Start IV methylprednisolone
- B. Obtain CT head without contrast
- C. Start oral prednisone (Correct Answer)
- D. Perform a temporal artery biopsy
- E. Perform a lumbar puncture
Acute phase management Explanation: **Start oral prednisone**
- The patient's symptoms (fever, headache, hip and shoulder stiffness, scalp tenderness, elevated ESR) are highly suggestive of **giant cell arteritis (GCA)**, which is closely associated with **polymyalgia rheumatica (PMR)**.
- Starting oral prednisone promptly is appropriate to manage the symptoms and prevent potential complications like **vision loss**, especially when classic GCA symptoms are present but there is no acute vision loss.
*Start IV methylprednisolone*
- **IV methylprednisolone** is typically reserved for patients with **acute vision loss** or other severe ischemic complications of GCA, which are not described in this patient.
- While GCA is a serious condition, oral prednisone is usually sufficient for initial management unless impending or active catastrophic events like blindness are present.
*Obtain CT head without contrast*
- A **CT head without contrast** would primarily be useful for evaluating acute neurological deficits or ruling out intracranial pathology like a hemorrhage or mass, which are not indicated by this patient's presentation (normal neurological exam).
- It would not confirm GCA or PMR and would delay appropriate steroid initiation.
*Perform a temporal artery biopsy*
- A **temporal artery biopsy** is the gold standard for confirming GCA, but it is not the most appropriate *next step in management* for a suspected case.
- **Steroid therapy should be initiated immediately** based on clinical suspicion to prevent irreversible vision loss, even before the biopsy results are available. The biopsy can be performed within 1-2 weeks of starting steroids without significantly affecting diagnostic yield.
*Perform a lumbar puncture*
- A **lumbar puncture** is used to diagnose conditions affecting the central nervous system, such as meningitis or subarachnoid hemorrhage.
- The patient's presentation, including normal neurological testing and specific musculoskeletal symptoms, does not point towards an infectious or inflammatory process requiring a lumbar puncture.
Acute phase management US Medical PG Question 2: A 6-year-old boy presents to his pediatrician accompanied by his mother for evaluation of a rash. The rash appeared a little over a week ago, and since that time the boy has felt tired. He is less interested in playing outside, preferring to remain indoors because his knees and stomach hurt. His past medical history is significant for an upper respiratory infection that resolved uneventfully without treatment 2 weeks ago. Temperature is 99.5°F (37.5°C), blood pressure is 115/70 mmHg, pulse is 90/min, and respirations are 18/min. Physical exam shows scattered maroon macules and papules on the lower extremities. The abdomen is diffusely tender to palpation. There is no cervical lymphadenopathy or conjunctival injection. Which of the following will most likely be found in this patient?
- A. Coronary artery aneurysms
- B. Leukocytoclastic vasculitis (Correct Answer)
- C. Thrombocytopenia
- D. Mitral regurgitation
- E. Occult malignancy
Acute phase management Explanation: ***Leukocytoclastic vasculitis***
- This patient presents with symptoms highly suggestive of **Henoch-Schönlein Purpura (HSP)**, including a preceding URI, fatigue, low-grade fever, **abdominal pain**, and a **palpable purpura** primarily on the lower extremities.
- HSP is characterized by IgA-mediated **small-vessel vasculitis**, which histologically presents as leukocytoclastic vasculitis with IgA deposition on immunofluorescence.
*Coronary artery aneurysms*
- **Coronary artery aneurysms** are a classic complication of **Kawasaki disease**, not Henoch-Schönlein Purpura.
- Kawasaki disease presents with different clinical features, including prolonged fever, conjunctival injection, oral changes, and cervical lymphadenopathy.
*Thrombocytopenia*
- **Thrombocytopenia** is characterized by a low platelet count and often presents with petechiae, purpura, and bleeding, but the rash in HSP is due to inflammation and extravasation of red blood cells, not low platelets.
- Platelet counts in HSP are typically **normal** or can be slightly elevated as an acute phase reactant.
*Mitral regurgitation*
- **Mitral regurgitation** is a common manifestation of **rheumatic fever**, particularly after recurrent episodes, caused by valvular damage.
- Rheumatic fever is also preceded by infection (Group A Strep) but involves different symptoms like migratory polyarthritis, carditis, chorea, erythema marginatum, and subcutaneous nodules, which are not described here.
*Occult malignancy*
- While an **occult malignancy** can cause paraneoplastic syndromes or constitutional symptoms, the specific constellation of symptoms, including the migratory rash, abdominal pain, and preceding URI, points much more strongly to **HSP** in a 6-year-old.
- The presentation is more consistent with an acute, inflammatory process rather than a chronic, insidious malignant one.
Acute phase management US Medical PG Question 3: A 25-year-old man of Mediterranean descent makes an appointment with his physician because his skin and sclera have become yellow. He complains of fatigue and fever that started at the same time icterus appeared. On examination, he is tachycardic and tachypneic. The oxygen (O2) saturation is < 90%. He has increased unconjugated bilirubin, hemoglobinemia, and an increased number of reticulocytes in the peripheral blood. What is the most likely diagnosis?
- A. Microcytic anemia caused by iron deficiency
- B. Aplastic anemia
- C. Autoimmune hemolytic anemia (AIHA)
- D. Anemia caused by renal failure
- E. Hemolytic anemia caused by glucose-6-phosphate dehydrogenase deficiency (G6PD deficiency) (Correct Answer)
Acute phase management Explanation: ***Hemolytic anemia caused by glucose-6-phosphate dehydrogenase deficiency (G6PD deficiency)***
- The patient's presentation with **jaundice**, **fatigue**, fever, **tachycardia**, **tachypnea**, and **low oxygen saturation** points to an acute hemolytic crisis.
- The laboratory findings of **increased unconjugated bilirubin**, **hemoglobinemia** (evidence of red blood cell destruction), and **increased reticulocytes** (bone marrow's attempt to compensate for red blood cell loss) are classic for hemolytic anemia. A young man of **Mediterranean descent** makes G6PD deficiency a strong possibility, as it is common in this population and can be triggered by various factors leading to oxidative stress.
*Microcytic anemia caused by iron deficiency*
- **Iron deficiency anemia** typically presents with **microcytic hypochromic red blood cells**, and while it causes fatigue and pallor, it does not typically lead to acute jaundice and hemoglobinemia.
- Reticulocyte count is usually normal or only mildly elevated, not significantly increased as seen in rapid red blood cell destruction.
*Aplastic anemia*
- **Aplastic anemia** is characterized by **pancytopenia** (decreased red blood cells, white blood cells, and platelets) due to bone marrow failure.
- It does not present with signs of hemolytic crisis such as jaundice, hemoglobinemia, or increased reticulocytes.
*Autoimmune hemolytic anemia (AIHA)*
- While AIHA causes **hemolytic anemia** with similar lab findings (jaundice, increased unconjugated bilirubin, reticulocytosis), the context of a young man of **Mediterranean descent** makes G6PD deficiency a more likely primary consideration, especially without specific triggers for AIHA or a positive direct Coombs test result.
- AIHA involves autoantibodies against red blood cells.
*Anemia caused by renal failure*
- Anemia due to **renal failure** is primarily caused by decreased production of **erythropoietin** leading to **normocytic, normochromic anemia**.
- It does not involve acute hemolysis, jaundice, hemoglobinemia, or increased reticulocytes.
Acute phase management US Medical PG Question 4: A 5-year-old boy is brought to see his pediatrician because of painless swelling in both legs and around his eyes. His mother reports that it is worse in the morning and these symptoms have started 4 days ago. The child has just recovered from a severe upper respiratory tract infection 8 days ago. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. Today, his blood pressure is 110/65 mm Hg, the heart rate is 90/min, the respiratory rate is 22/min, and the temperature is 36.8°C (98.2°F). On physical examination, his face is edematous and there is a 2+ pitting edema over both legs up to his hips. Laboratory results are shown.
Serum albumin 2.4 g/dL
Serum triglycerides 250 mg/dL
Serum cholesterol 300 mg/dL
Urine dipstick 4+ protein
Which of the following is the best initial therapy for this patient’s condition?
- A. Enalapril
- B. Prednisolone (Correct Answer)
- C. Prednisolone and cyclophosphamide
- D. Albumin infusion
- E. Oral antibiotic
Acute phase management Explanation: **Prednisolone**
- The patient presents with **edema**, **proteinuria (4+ protein)**, **hypoalbuminemia (2.4 g/dL)**, and **hyperlipidemia (triglycerides 250 mg/dL, cholesterol 300 mg/dL)**, which are the classic hallmarks of **nephrotic syndrome**.
- Given his age (5 years old) and recent upper respiratory tract infection, **minimal change disease (MCD)** is the most likely cause of nephrotic syndrome in children, and **corticosteroids** like prednisolone are the first-line treatment.
*Enalapril*
- **Enalapril** is an **ACE inhibitor** used to reduce proteinuria by decreasing glomerular pressure, but it is not the primary treatment for inducing remission in minimal change disease.
- While it may be used as an adjunct in patients with persistent proteinuria or hypertension, it is not the best initial monotherapy for acute presentation of nephrotic syndrome.
*Prednisolone and cyclophosphamide*
- **Cyclophosphamide** is an **immunosuppressant** reserved for patients who are **steroid-resistant** or **frequently relapsing** on steroid therapy.
- It is not indicated as initial therapy for a first presentation of nephrotic syndrome in a child, where prednisolone alone is usually effective.
*Albumin infusion*
- **Albumin infusion** is used to temporarily increase intravascular volume and reduce severe edema, particularly in cases of severe hypoalbuminemia with hypovolemia or refractory edema.
- It is typically not used as a sole initial therapy because it does not address the underlying pathology (proteinuria) and its effects are transient.
*Oral antibiotic*
- An **oral antibiotic** would be indicated if there was evidence of a bacterial infection, such as **peritonitis** or **skin infections**, which are complications of nephrotic syndrome.
- While the patient had a recent URI, there are no current signs or symptoms of a bacterial infection that would warrant antibiotic treatment as the initial therapy for the nephrotic syndrome.
Acute phase management US Medical PG Question 5: A 5-year-old girl is brought to the emergency department by her father due to a 6-day history of fevers and irritability. His father reports that the fevers have ranged from 101-104°F (38.3-40°C). He tried to give her ibuprofen, but the fevers have been unresponsive. Additionally, she developed a rash 3 days ago and has refused to wear shoes because they feel "tight." Her father reports that other than 2 ear infections she had when she was younger, the patient has been healthy. She is up-to-date on her vaccinations except for the vaccine boosters scheduled for ages 4-6. The patient's temperature is 103.5°F (39.7°C), blood pressure is 110/67 mmHg, pulse is 115/min, and respirations are 19/min with an oxygen saturation of 98% O2 on room air. Physical examination shows bilateral conjunctivitis, palpable cervical lymph nodes, a diffuse morbilliform rash, and desquamation of the palms and soles with swollen hands and feet. Which of the following is the next step in management?
- A. Acetaminophen
- B. High dose aspirin
- C. IVIG and high-dose aspirin (Correct Answer)
- D. Nafcillin
- E. Penicillin V
Acute phase management Explanation: ***IVIG and high-dose aspirin***
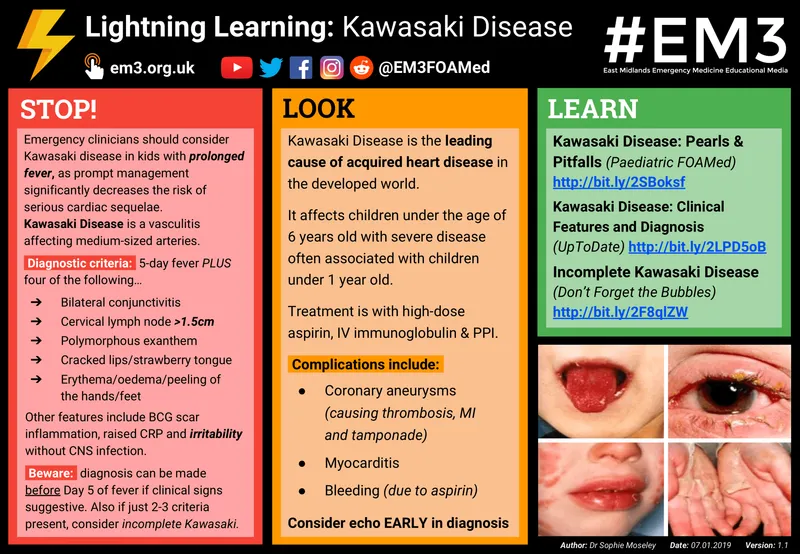
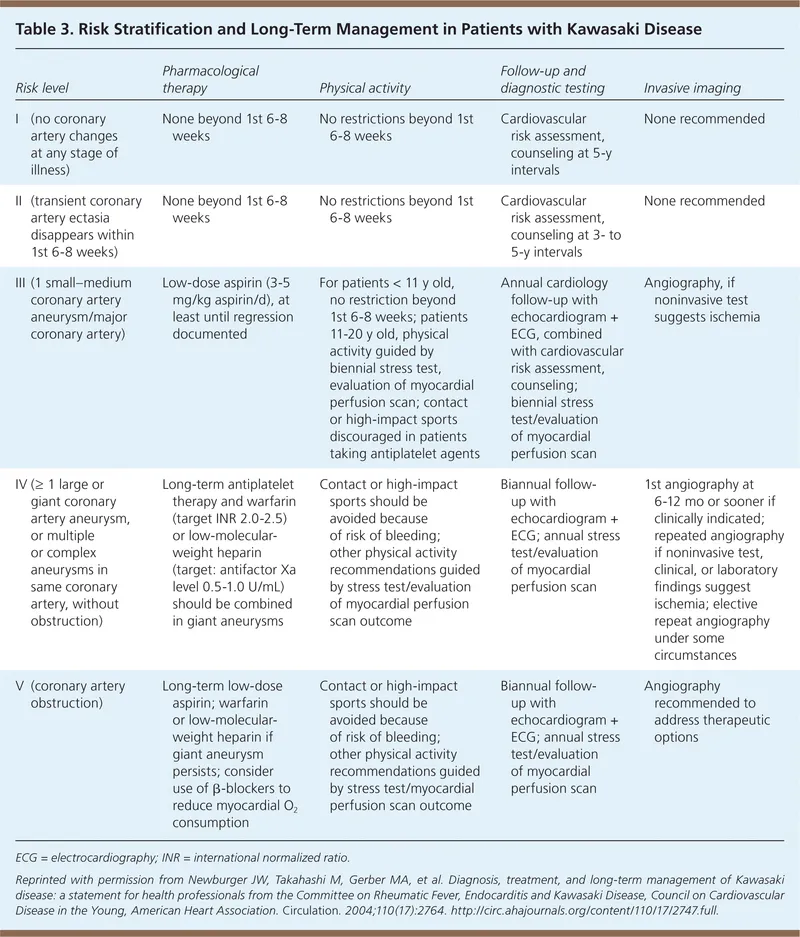
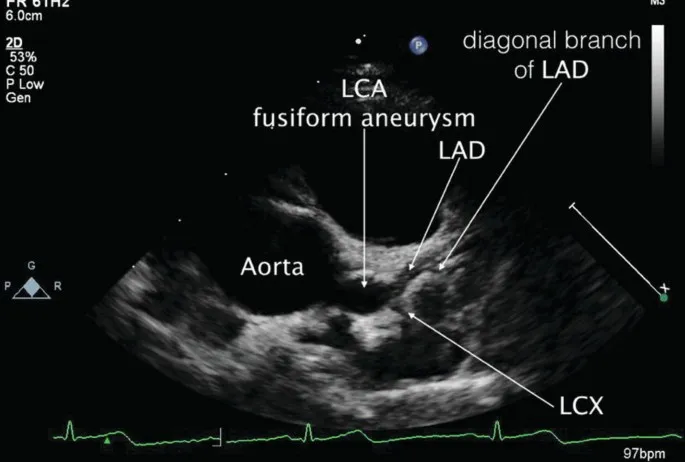
- The patient's symptoms (prolonged fever >5 days, bilateral conjunctivitis, diffuse rash, extremity changes with edema and desquamation, cervical lymphadenopathy) meet diagnostic criteria for **Kawasaki disease**.
- **IVIG (Intravenous Immunoglobulin)** is the PRIMARY treatment and must be given within 10 days of fever onset to reduce the risk of **coronary artery aneurysms** from 25% to <5%.
- **High-dose aspirin** is given as ADJUNCTIVE therapy for its anti-inflammatory effects, then transitioned to low-dose aspirin for antiplatelet effects once fever resolves.
- This combination is the **standard of care** and should be initiated as soon as the diagnosis is suspected.
*High dose aspirin*
- While aspirin is an essential component of Kawasaki disease treatment, it should **not be given as monotherapy**.
- Aspirin alone without **IVIG** is insufficient and fails to adequately reduce the risk of coronary complications.
- The question asks for the "next step in management," which requires **both IVIG and aspirin** together.
*Acetaminophen*
- Acetaminophen is an antipyretic but lacks the anti-inflammatory effects needed for **Kawasaki disease**.
- The patient's fever has already been unresponsive to **ibuprofen**, indicating that simple antipyretics are inadequate.
- It has no role in preventing the vascular complications of Kawasaki disease.
*Nafcillin*
- **Nafcillin** is an antibiotic for bacterial infections, particularly *Staphylococcus aureus*.
- **Kawasaki disease** is a vasculitis of unknown etiology (possibly post-infectious immune response) and is **not treated with antibiotics**.
- The clinical presentation does not suggest an acute bacterial infection requiring antibiotic therapy.
*Penicillin V*
- **Penicillin V** is used for streptococcal infections such as strep pharyngitis.
- The constellation of findings (persistent fever, conjunctivitis, rash, extremity changes, lymphadenopathy) is classic for **Kawasaki disease**, not a bacterial infection.
- Antibiotics have no role in the management of Kawasaki disease.
Acute phase management US Medical PG Question 6: A 1-month-old boy is brought in by his mother for episodes of “not breathing.” She reports noticing that the patient will occasionally stop breathing while he’s sleeping, and that these episodes have been occurring more frequently. The patient was born at 32 weeks due to placental insufficiency. He was in the neonatal intensive care unit for 1 day to be placed on a respirator. During prenatal testing, it was revealed that the mother was not immune to rubella, but she otherwise had an uncomplicated pregnancy. She has no medical conditions and took only prenatal vitamins. The patient has a 3-year-old sister who is healthy. His father has a “heart condition.” The patient’s temperature is 98°F (36.7°C), blood pressure is 91/55 mmHg, pulse is 207/min, and respirations are 50/min with an oxygen saturation of 97% on room air. Physical examination is notable for pale conjunctiva. Labs are obtained, as shown below:
Leukocyte count: 10,000/mm^3 with normal differential
Hemoglobin: 8.2 g/dL
Hematocrit: 28%
Mean corpuscular volume (MCV): 100 um^3
Platelet count: 300,000/mm^3
Reticulocyte count: 0.8% (normal range: 2-6%)
Lactate dehydrogenase: 120 U/L (normal range: 100-250 U/L)
A peripheral smear reveals normocytic and normochromic red blood cells. Which of the following is a mechanism for the patient’s most likely diagnosis?
- A. Red blood cell membrane defect
- B. Minor blood group incompatibility
- C. Hemoglobinopathy
- D. Impaired erythropoietin production (Correct Answer)
- E. Congenital infection
Acute phase management Explanation: ***Impaired erythropoietin production***
- This patient presents with **anemia of prematurity**, indicated by **normocytic, normochromic anemia** with a **low reticulocyte count** in a premature infant.
- The primary mechanism for **anemia of prematurity** is a blunted erythropoietin response to early anemia, leading to **impaired red blood cell production**.
*Red blood cell membrane defect*
- Conditions like **hereditary spherocytosis** or **elliptocytosis** involve red blood cell membrane defects, which typically lead to **hemolytic anemia** with elevated reticulocyte count.
- The patient's **low reticulocyte count** and normal LDH (lactate dehydrogenase is a marker of hemolysis) make a primary membrane defect less likely.
*Minor blood group incompatibility*
- **Minor blood group incompatibilities** (e.g., ABO, Kell, Duffy) typically cause **hemolytic disease of the newborn**, characterized by **elevated reticulocyte count**, **hyperbilirubinemia**, and signs of hemolysis.
- The patient exhibits no signs of hemolysis, such as elevated bilirubin or LDH, and has a normal reticulocyte count.
*Hemoglobinopathy*
- **Hemoglobinopathies** (e.g., sickle cell anemia, thalassemia) involve structural or quantitative defects in hemoglobin, often leading to **microcytic** or **hemolytic anemias** with **elevated reticulocyte counts** or specific red blood cell morphologies.
- The patient's **normocytic, normochromic anemia** and absent signs of hemolysis do not fit typical presentations of common hemoglobinopathies at this age.
*Congenital infection*
- Certain **congenital infections** (e.g., parvovirus B19, congenital syphilis, rubella) can cause anemia by directly suppressing erythropoiesis or causing hemolysis.
- While the mother was not immune to rubella, there are no other clinical signs of congenital infection, and the **normocytic, normochromic anemia** with low reticulocytes is more characteristic of anemia of prematurity.
Acute phase management US Medical PG Question 7: A 4-year-old boy is brought to the physician by his parents because of fever and mild abdominal pain for 7 days. His parents report that he developed a rash 2 days ago. He has had no diarrhea or vomiting. Four weeks ago, he returned from a camping trip to Colorado with his family. His immunization records are unavailable. His temperature is 39.4°C (102.9°F), pulse is 111/min, respirations are 27/min, and blood pressure is 96/65 mm Hg. Examination shows bilateral conjunctival injections and fissures on his lower lips. The pharynx is erythematous. There is tender cervical lymphadenopathy. The hands and feet appear edematous. A macular morbilliform rash is present over the trunk. Bilateral knee joints are swollen and tender; range of motion is limited by pain. Which of the following is the most appropriate treatment for this patient's condition?
- A. Supportive treatment only
- B. Intravenous immunoglobulin (Correct Answer)
- C. Oral ibuprofen
- D. Oral penicillin
- E. Oral doxycycline
Acute phase management Explanation: ***Intravenous immunoglobulin***
- This patient presents with symptoms highly suggestive of **Kawasaki disease**, including a persistent fever for over 5 days, **bilateral conjunctival injection**, **lip fissures**, **erythematous pharynx**, **cervical lymphadenopathy**, and **edema of hands and feet** followed by a rash.
- **IV immunoglobulin (IVIG)** is the cornerstone of treatment for Kawasaki disease, significantly reducing the risk of **coronary artery aneurysms** if given early in the disease course.
*Supportive treatment only*
- While supportive care (fever reduction, hydration) is important, relying solely on it for **Kawasaki disease** would increase the risk of severe complications, particularly **coronary artery involvement**.
- **Kawasaki disease** is a systemic vasculitis requiring specific immunomodulatory therapy to prevent long-term cardiac sequelae.
*Oral ibuprofen*
- **Ibuprofen**, a non-steroidal anti-inflammatory drug (**NSAID**), can help manage fever and joint pain, but it does not address the underlying **vasculitis** or prevent the cardiac complications of **Kawasaki disease**.
- **Aspirin** (high-dose initially, then low-dose) is part of Kawasaki disease treatment, but ibuprofen alone is insufficient as primary therapy.
*Oral penicillin*
- **Penicillin** is an antibiotic used to treat bacterial infections, such as **streptococcal pharyngitis**.
- This patient's symptoms are inconsistent with a typical bacterial infection requiring penicillin and are more indicative of a **systemic inflammatory condition** like Kawasaki disease, which is not bacterial.
*Oral doxycycline*
- **Doxycycline** is an antibiotic often used for **rickettsial infections** (e.g., Rocky Mountain spotted fever) or Lyme disease, which might be considered given the camping trip.
- However, the classic constellation of symptoms (conjunctival injection, lip changes, edema of extremities, diffuse rash) points strongly away from these and towards **Kawasaki disease**, for which doxycycline is ineffective.
Acute phase management US Medical PG Question 8: A 4-year-old boy is brought to a pediatrician by his parents with a history of fever for the last 5 days and irritability, decreased appetite, vomiting, and swelling of the hands and feet for the last 3 days. The patient’s mother mentions that he has been taking antibiotics and antipyretics prescribed by another physician for the last 3 days, but there has been no improvement His temperature is 39.4°C (103.0°F), pulse is 128/min, respiratory rate is 24/min, and blood pressure is 96/64 mm Hg. On physical examination, there is significant edema of the hands and feet bilaterally. There is a 2.5 cm diameter freely moveable, nontender cervical lymph node is palpable on the right side. A strawberry tongue and perianal erythema are noted. Conjunctival injection is present bilaterally. Laboratory findings reveal mild anemia and a leukocytosis with a left-shift. Erythrocyte sedimentation rate (ESR) and serum C-reactive protein (CRP) are increased. If not treated appropriately, this patient is at increased risk of developing which of the following complications?
- A. Lower gastrointestinal hemorrhage
- B. Coronary artery ectasia (Correct Answer)
- C. Acute renal failure
- D. Pulmonary embolism
- E. Acute disseminated encephalomyelitis (ADEM)
Acute phase management Explanation: ***Coronary artery ectasia***
- The patient's symptoms, including **prolonged fever**, **conjunctival injection**, **strawberry tongue**, **cervical lymphadenopathy**, **edema of hands and feet**, and **perianal erythema**, are characteristic of **Kawasaki disease**.
- If left untreated, **Kawasaki disease** can lead to significant cardiovascular complications, most notably **coronary artery aneurysms** or ectasia, due to vasculitis of medium-sized arteries.
*Lower gastrointestinal hemorrhage*
- While **gastrointestinal symptoms** such as vomiting and diarrhea can occur in **Kawasaki disease**, severe complications like **lower gastrointestinal hemorrhage** are rare and not the most common or critical untreated complication.
- Other conditions, like **Meckel's diverticulum** or **inflammatory bowel disease**, are more typically associated with lower GI hemorrhage in children.
*Acute renal failure*
- **Renal involvement** in **Kawasaki disease** is uncommon and usually presents as **mild proteinuria** or **sterile pyuria**; **acute renal failure** is an extremely rare complication.
- Significant renal dysfunction is more commonly seen in conditions like **hemolytic-uremic syndrome** or severe dehydration.
*Pulmonary embolism*
- **Pulmonary embolism** is rare in young children and not a typical complication of untreated **Kawasaki disease**.
- It is more commonly associated with conditions causing **hypercoagulability** or prolonged immobility.
*Acute disseminated encephalomyelitis (ADEM)*
- **ADEM** is an **immune-mediated demyelinating disorder** of the central nervous system that typically follows an infection or vaccination.
- It is not a recognized complication of untreated **Kawasaki disease**, whose primary pathology involves systemic vasculitis.
Acute phase management US Medical PG Question 9: A previously healthy 4-year-old boy is brought to the physician by his parents because he has had a fever, diffuse joint pain, and a rash on his abdomen for the past week. Acetaminophen did not improve his symptoms. He emigrated from China with his family 2 years ago. He attends daycare. His immunization records are not available. His temperature is 38.5°C (101.3°F), pulse is 125/min, and blood pressure is 100/60 mm Hg. Examination shows polymorphous truncal rash. The eyes are pink with no exudate. The tongue is shiny and red, and the lips are cracked. The hands and feet are red and swollen. There is right-sided anterior cervical lymphadenopathy. Which of the following is the most appropriate next step in management?
- A. HHV-6 immunoglobulin M (IgM) detection
- B. ANA measurement
- C. Echocardiography (Correct Answer)
- D. Monospot test
- E. Antistreptolysin O titer measurement
Acute phase management Explanation: ***Echocardiography***
- This patient presents with classic symptoms of **Kawasaki disease**, including protracted fever (>5 days), polymorphous rash, conjunctival injection, cracked lips and red tongue (**strawberry tongue**), swollen hands and feet, and cervical lymphadenopathy.
- The diagnosis can be made clinically when fever ≥5 days plus ≥4 of 5 principal criteria are present, which this patient meets.
- **Echocardiography** is essential to establish a **baseline cardiac assessment** and screen for **coronary artery aneurysms**, which occur in 15-25% of untreated patients.
- Among the diagnostic options listed, echocardiography is the most appropriate next step, though in clinical practice, **treatment with IVIG and high-dose aspirin should be initiated promptly** (ideally within 10 days of fever onset) and should not be delayed pending echocardiography results.
*HHV-6 immunoglobulin M (IgM) detection*
- **Human Herpesvirus 6 (HHV-6)** causes **roseola infantum** (exanthem subitum), which presents with high fever for 3-5 days followed by a rash that appears **as the fever resolves**.
- The mucocutaneous findings in this case (strawberry tongue, cracked lips, conjunctival injection, extremity swelling) are not consistent with roseola.
*ANA measurement*
- **Antinuclear antibody (ANA)** testing screens for **autoimmune diseases** such as systemic lupus erythematosus or juvenile idiopathic arthritis.
- While this patient has fever and joint pain, the specific mucocutaneous changes (strawberry tongue, cracked lips, conjunctival injection, polymorphous rash, extremity edema) and cervical lymphadenopathy are pathognomonic for Kawasaki disease, not typical autoimmune conditions.
*Monospot test*
- The **Monospot test** diagnoses **infectious mononucleosis** caused by **Epstein-Barr virus (EBV)**.
- While EBV can cause fever, rash, and lymphadenopathy (typically posterior cervical), the characteristic mucocutaneous findings of Kawasaki disease (strawberry tongue, cracked lips, conjunctival injection without exudate, extremity changes) are not seen in mononucleosis.
- Additionally, mononucleosis is uncommon in preschool-aged children.
*Antistreptolysin O titer measurement*
- **Antistreptolysin O (ASO) titer** detects recent **Group A Streptococcus** infection and can support a diagnosis of **acute rheumatic fever (ARF)**.
- ARF presents with migratory polyarthritis, carditis, and **erythema marginatum** (not a polymorphous rash), occurring 2-4 weeks after streptococcal pharyngitis.
- The mucocutaneous features in this case are specific to Kawasaki disease and not consistent with ARF.
Acute phase management US Medical PG Question 10: A 4-year-old boy is brought to the emergency department by his mother with a rash on his trunk, malaise, and fever with spikes up to 38.5°C (101.3°F) for the past 2 weeks. The patient's mother says she tried giving him Tylenol with little improvement. Past medical history includes a spontaneous vaginal delivery at full term. The patient's vaccines are up-to-date and he has met all developmental milestones. On physical examination, his lips are cracking, and he has painful cervical lymphadenopathy. The rash is morbilliform and involves his trunk, palms, and the soles of his feet. There is fine desquamation of the skin of the perianal region. Which of the following anatomical structures is most important to screen for possible complications in this patient?
- A. Mitral valve
- B. Kidneys
- C. Gallbladder
- D. Coronary artery (Correct Answer)
- E. Pylorus
Acute phase management Explanation: ***Coronary artery***
- The constellation of symptoms, including prolonged fever, rash on trunk, palms, and soles, cracked lips, cervical lymphadenopathy, and perianal desquamation, is highly indicative of **Kawasaki disease**.
- **Coronary artery aneurysms** are the most serious complication of Kawasaki disease, occurring in 15-25% of untreated children, necessitating close monitoring and screening.
*Mitral valve*
- While other forms of vasculitis or rheumatic fever can affect heart valves, **mitral valve** involvement is not a primary or characteristic complication of Kawasaki disease.
- The main cardiac concern in Kawasaki disease is direct arterial inflammation, not valvular dysfunction.
*Kidneys*
- **Renal involvement**, such as acute kidney injury, is not a typical or prominent feature of Kawasaki disease.
- Kawasaki disease primarily targets medium-sized muscular arteries throughout the body, with a predilection for the coronary arteries.
*Gallbladder*
- **Hydrops of the gallbladder** can occur in Kawasaki disease, leading to acute cholecystitis-like symptoms, but it is generally a self-limiting complication.
- While it's a potential finding, it is not as life-threatening or essential to screen for as coronary artery complications.
*Pylorus*
- There is no direct association between Kawasaki disease and primary involvement or complications of the **pylorus**.
- Gastrointestinal symptoms can occur, but these are typically non-specific and do not involve anatomical changes to the pylorus.
More Acute phase management US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.