Kawasaki disease

On this page
🔥 The Kawasaki Syndrome: Decoding Pediatric Vasculitis
Kawasaki disease transforms healthy children into puzzles of fever, rash, and inflamed vessels-and missing it means risking coronary artery aneurysms that shadow a lifetime. You'll learn to recognize its deceptive clinical patterns, understand the immune storm driving vascular injury, navigate diagnostic criteria when no single test confirms it, and master time-sensitive treatment protocols that prevent cardiac complications. This lesson builds your pattern recognition from first presentation through long-term surveillance, integrating immunology, cardiology, and clinical reasoning into a framework that turns diagnostic uncertainty into confident action.
The CRASH Diagnostic Framework
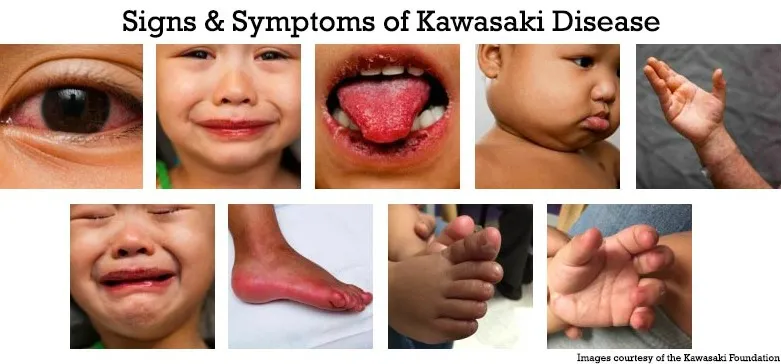
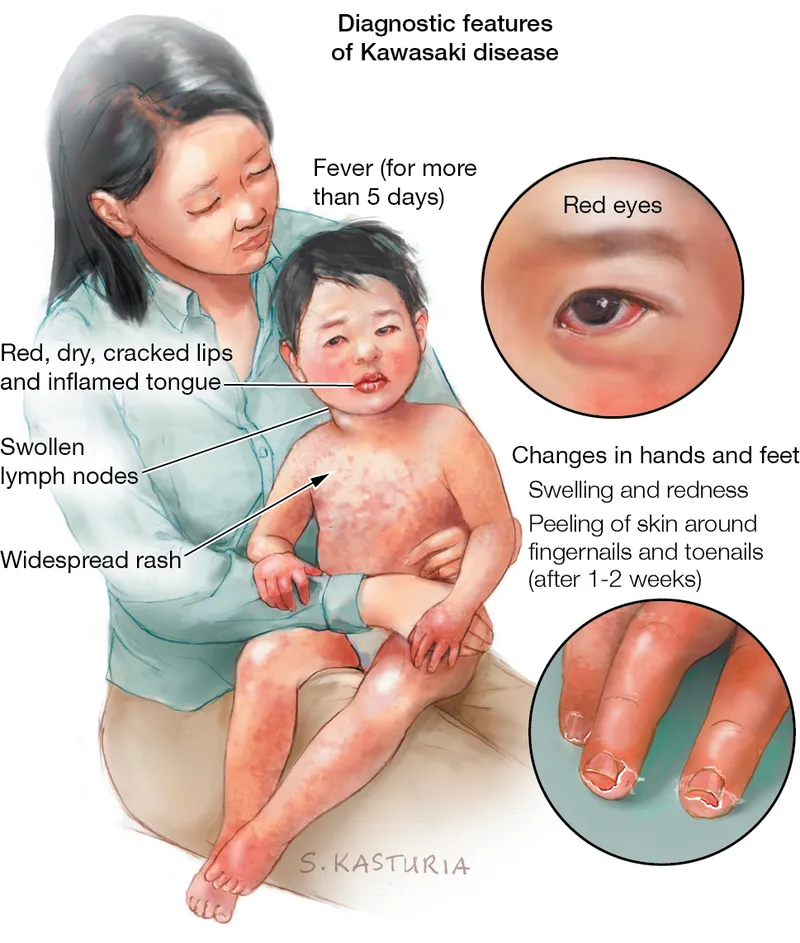
Kawasaki disease diagnosis centers on 5 principal criteria plus persistent fever lasting ≥5 days. The systematic CRASH mnemonic captures the essential clinical constellation:
📌 CRASH Mnemonic: Conjunctivitis (bilateral, non-purulent), Rash (polymorphous), Adenopathy (cervical >1.5cm), Strawberry tongue/oral changes, Hand/foot changes (erythema, edema, desquamation)
-
Fever Requirements
- Duration: ≥5 days (can be ≥4 days if other criteria met)
- Pattern: High-grade, often >39°C (102.2°F)
- Characteristic: Unresponsive to antibiotics
- Timeline: Must be present to consider diagnosis
-
Conjunctival Changes (85% of cases)
- Bilateral bulbar conjunctival injection
- Non-purulent (distinguishes from bacterial)
- Spares limbus (peripheral corneal sparing)
- No exudate or discharge
-
Oral Mucosa Changes (90% of cases)
- Strawberry tongue (prominent papillae)
- Erythematous, dry, fissured lips
- Diffuse oral and pharyngeal erythema
- No ulcerations or vesicles

Rash Patterns and Distribution
The polymorphous rash appears in 80% of patients, typically within 5 days of fever onset:
-
Morphology Variations
- Maculopapular (most common): 60% of rash cases
- Urticarial plaques: 25% of presentations
- Scarlatiniform: 15% of cases
- Never vesicular or bullous (key differentiator)
-
Distribution Patterns
- Truncal predominance with centrifugal spread
- Accentuation in perineal area (early sign)
- Spares palms and soles initially
- Fades within 1-2 weeks without scarring
⭐ Clinical Pearl: Perineal desquamation occurs in 67% of Kawasaki patients within 2-3 days of fever onset, often preceding classic hand/foot changes by 5-7 days.
Extremity Changes Through Disease Phases
Hand and foot manifestations follow predictable temporal patterns:
| Phase | Timing | Acute Changes | Subacute Changes | Frequency |
|---|---|---|---|---|
| Acute | Days 1-10 | Erythema, edema | Induration | 70% |
| Subacute | Days 10-25 | Pain, swelling | Periungual desquamation | 95% |
| Convalescent | Days 25+ | Resolution | Beau's lines | 40% |
| Late | Weeks-months | Normal | Nail changes persist | 15% |
Understanding these foundational criteria establishes the diagnostic framework essential for recognizing incomplete presentations and preventing cardiac complications through the inflammatory mechanisms that drive coronary artery involvement.
🔥 The Kawasaki Syndrome: Decoding Pediatric Vasculitis
⚡ Inflammatory Cascade: The Vasculitic Storm
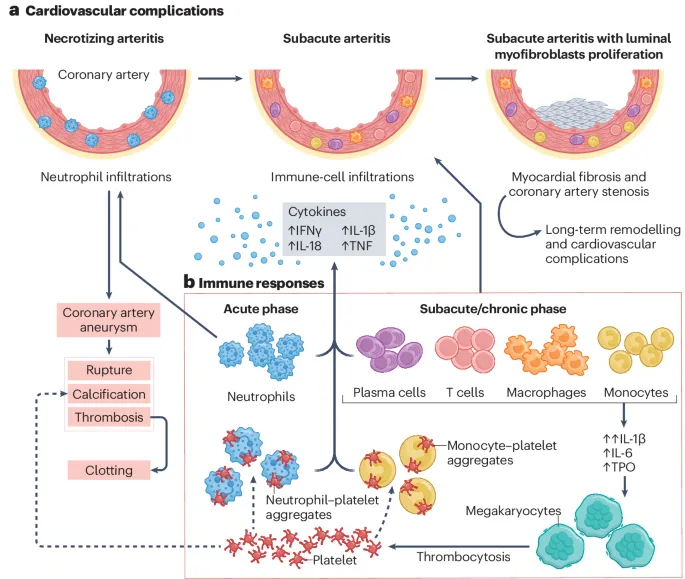
The Superantigen Hypothesis
Current evidence supports superantigen-triggered immune activation as the primary mechanism:
-
Superantigen Characteristics
- Bypasses normal antigen processing
- Activates 5-20% of T-cell population (vs 0.01% normal)
- Triggers 100-fold increase in cytokine production
- Creates polyclonal T-cell activation pattern
-
Cytokine Profile (Peak levels at days 3-7)
- TNF-α: Elevated 10-50x normal levels
- IL-1β: Increased 20-100x baseline
- IL-6: Rises 50-200x normal values
- Interferon-γ: Elevated 5-25x typical levels
📌 Inflammatory Sequence: Superantigen → T-cell activation → Orchestrated cytokine release → Rapid endothelial damage → Medium artery targeting (STORM mnemonic)
Vascular Targeting Mechanisms
The inflammatory process shows selective tropism for coronary arteries through specific mechanisms:
-
Coronary Vulnerability Factors
- Turbulent flow at branch points increases susceptibility
- Medium-sized vessels (2-4mm diameter) preferentially affected
- Elastic lamina disruption occurs within 48-72 hours
- Smooth muscle necrosis peaks at days 7-14
-
Temporal Inflammatory Phases
- Days 1-9: Acute necrotizing arteritis
- Days 10-25: Subacute/granulomatous inflammation
- Days 26-40: Scarring and remodeling phase
- >40 days: Chronic fibrotic changes
⭐ Clinical Pearl: Coronary artery aneurysms develop in 25% of untreated patients, with giant aneurysms (>8mm) occurring in 2-3% of cases, carrying 20-fold increased thrombosis risk.
Laboratory Inflammatory Markers
Systematic monitoring reveals predictable inflammatory patterns:
| Marker | Peak Timing | Typical Values | Clinical Significance | Normalization |
|---|---|---|---|---|
| ESR | Days 2-4 | 80-120 mm/hr | Disease activity | 6-10 weeks |
| CRP | Days 3-5 | 100-200 mg/L | Acute inflammation | 2-4 weeks |
| WBC | Days 1-3 | 15,000-25,000/μL | Neutrophilic response | 1-2 weeks |
| Platelets | Days 10-14 | 600,000-1,000,000/μL | Thrombocytosis phase | 4-8 weeks |
| ALT | Days 5-10 | 100-300 U/L | Hepatic involvement | 2-6 weeks |
This inflammatory understanding provides the mechanistic foundation for recognizing atypical presentations and optimizing treatment timing to prevent irreversible coronary damage through targeted anti-inflammatory interventions.
⚡ Inflammatory Cascade: The Vasculitic Storm
🎯 Pattern Recognition: The Clinical Detective Framework
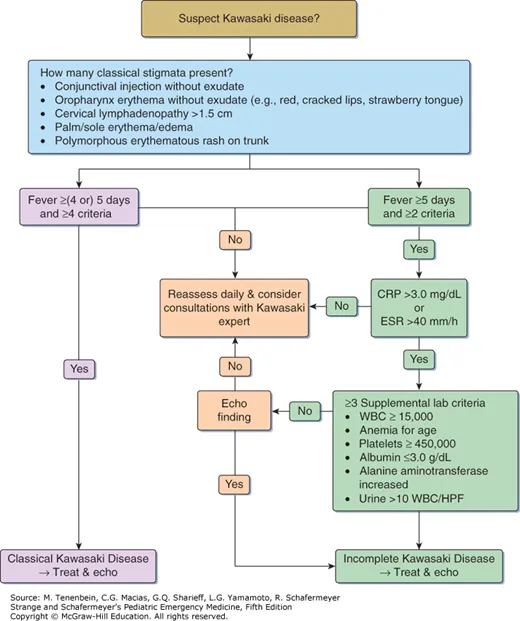
The Complete vs Incomplete Diagnostic Framework
Recognition patterns follow evidence-based hierarchies distinguishing presentation types:
-
Complete Kawasaki Disease (60-70% of cases)
- Fever ≥5 days PLUS ≥4 of 5 principal criteria
- Diagnosis confidence: >95% specificity
- Treatment indication: Immediate IVIG + aspirin
- Coronary risk: 15-20% if untreated
-
Incomplete Kawasaki Disease (30-40% of cases)
- Fever ≥5 days PLUS 2-3 principal criteria
- Requires laboratory and echocardiographic support
- Higher suspicion in infants <12 months and children >8 years
- Equal coronary risk to complete disease
📌 High-Risk Incomplete Pattern: Infants <1 year + Non-specific fever + Coronary changes + Other lab abnormalities + Missing classic criteria + Persistent inflammation + Low albumin + Elevated liver enzymes + Thrombocytosis + ESR elevation (INCOMPLETE mnemonic)
Age-Specific Recognition Patterns
Clinical presentations vary systematically by age group, requiring tailored recognition approaches:
-
Infants <12 months (20% of cases)
- Incomplete presentation: 85% of infant cases
- Fever only may be presenting sign in 40%
- Coronary involvement: Higher risk (35-40%)
- Diagnostic threshold: Lower criteria requirement
-
Peak Age Group 1-5 years (65% of cases)
- Classic CRASH criteria: 90% complete presentations
- Seasonal clustering: Winter/spring predominance
- Male predominance: 1.5:1 male-to-female ratio
- Asian ethnicity: 2-3x higher incidence
-
Older Children >8 years (15% of cases)
- Cervical adenopathy: More prominent (75% vs 50%)
- Arthritis: More common (30% vs 15%)
- Differential challenges: EBV, streptococcal infections
- Incomplete risk: 60% of older children
⭐ Clinical Pearl: Infants with fever >7 days plus any 2 criteria warrant immediate laboratory evaluation and echocardiography, as 40% will have coronary abnormalities despite incomplete presentations.
Differential Diagnosis Decision Matrix
Systematic discrimination prevents misdiagnosis through quantitative differentiators:
| Condition | Fever Pattern | Rash Type | Key Discriminator | Lab Distinction | Frequency |
|---|---|---|---|---|---|
| Kawasaki | >5 days, high | Polymorphous | Coronary involvement | Thrombocytosis | 1:10,000 |
| Scarlet Fever | 2-3 days | Sandpaper | Strawberry tongue | ASO positive | 1:1,000 |
| EBV | Variable | Maculopapular | Lymphadenopathy | Monospot positive | 1:500 |
| Adenovirus | 3-5 days | Variable | Conjunctivitis | PCR positive | 1:100 |
| Drug Reaction | 1-2 days | Urticarial | Medication history | Eosinophilia | Variable |
This pattern recognition framework transitions into systematic evaluation protocols that distinguish true Kawasaki disease from inflammatory mimics through evidence-based discrimination criteria and targeted diagnostic testing.
🎯 Pattern Recognition: The Clinical Detective Framework
🔬 Systematic Evaluation: The Diagnostic Laboratory Matrix
Essential Laboratory Panel Architecture
The diagnostic laboratory matrix combines acute-phase reactants, organ function markers, and cardiac biomarkers in systematic patterns:
-
Inflammatory Markers (Obtained within 24 hours)
- ESR: Typically >40 mm/hr (elevated in 95% of cases)
- CRP: Usually >30 mg/L (abnormal in 90% of patients)
- Procalcitonin: Often <0.5 ng/mL (helps exclude bacterial)
- Ferritin: May reach >500 ng/mL in severe cases
-
Hematologic Parameters
- WBC count: 12,000-25,000/μL with left shift
- Hemoglobin: Normocytic anemia in 60% (Hgb <10 g/dL)
- Platelet count: Normal acutely, then >450,000/μL by day 14
- Neutrophil predominance: >80% neutrophils typical
📌 Laboratory Timeline: Acute inflammation (days 1-7) → Normalization begins (days 8-14) → Thrombocytosis peaks (days 14-21) → Inflammatory resolution (weeks 4-8) (ANTI mnemonic)
Organ System Assessment Matrix
Systematic evaluation reveals multi-organ involvement patterns that support diagnosis:
-
Hepatic Involvement (65% of cases)
- ALT elevation: >40 U/L in 60% of patients
- AST elevation: >50 U/L in 55% of cases
- Bilirubin: Mild elevation (<3 mg/dL) in 25%
- GGT: Elevated in 40% of patients
-
Renal Function (30% of cases)
- Proteinuria: 1+ protein in 25% of patients
- Sterile pyuria: >10 WBC/hpf in 30% of cases
- Creatinine: Usually normal (elevation suggests complications)
- Hyponatremia: <135 mEq/L in 20% of patients
-
Nutritional/Inflammatory Status
- Hypoalbuminemia: <3.0 g/dL in 70% of cases
- Low cholesterol: <100 mg/dL during acute phase
- Elevated CK: >200 U/L in 15% of patients
- Low complement: C3/C4 decreased in 40%
⭐ Clinical Pearl: The combination of hypoalbuminemia (<3.0 g/dL), elevated ALT (>60 U/L), and sterile pyuria occurs in 45% of Kawasaki patients and has 85% specificity for the diagnosis.
Cardiac Biomarker Integration
Cardiac assessment combines structural evaluation with biomarker analysis for comprehensive risk stratification:
| Assessment | Normal Values | Kawasaki Abnormal | Clinical Significance | Timing |
|---|---|---|---|---|
| BNP/NT-proBNP | <100 pg/mL | >400 pg/mL | Myocardial dysfunction | Days 3-10 |
| Troponin I | <0.04 ng/mL | >0.1 ng/mL | Myocardial injury | Days 5-14 |
| CK-MB | <5 ng/mL | >10 ng/mL | Cardiac muscle damage | Days 7-21 |
| Echo Z-score | <2.0 | ≥2.5 | Coronary dilation | Days 7-14 |
| Coronary diameter | Age-specific | >3mm (<5yr) | Aneurysm formation | Days 10+ |
Incomplete Kawasaki Laboratory Algorithm
For patients with fever ≥5 days plus 2-3 criteria, systematic laboratory evaluation guides treatment decisions:
-
High-Risk Laboratory Pattern (Treat with IVIG)
- CRP ≥30 mg/L AND ESR ≥40 mm/hr
- Plus ≥3 of: Albumin <3.0 g/dL, ALT >50 U/L, Platelets >450,000/μL, WBC >15,000/μL, Urine >10 WBC/hpf
-
Moderate-Risk Pattern (Obtain echocardiogram)
- CRP 10-30 mg/L OR ESR 20-40 mm/hr
- Plus ≥2 supplemental laboratory criteria
- Echo abnormal → Treat as Kawasaki disease
-
Low-Risk Pattern (Observe with repeat labs)
- CRP <10 mg/L AND ESR <20 mm/hr
- <2 supplemental criteria
- Normal echocardiogram
This systematic evaluation framework provides the evidence-based foundation for treatment algorithms that optimize outcomes through precise risk stratification and targeted therapeutic interventions.
🔬 Systematic Evaluation: The Diagnostic Laboratory Matrix
⚖️ Treatment Algorithms: Evidence-Based Intervention Protocols
First-Line Treatment Protocol
The standard treatment combines IVIG and aspirin with specific dosing and timing requirements:
-
IVIG Administration Protocol
- Dose: 2 g/kg as single infusion over 10-12 hours
- Timing: Optimal within 7 days, beneficial up to day 10
- Response rate: 85-90% fever resolution within 48 hours
- Mechanism: Fc receptor blockade + anti-inflammatory effects
-
Aspirin Dosing Strategy
- High-dose phase: 80-100 mg/kg/day divided q6h until fever resolves
- Low-dose phase: 3-5 mg/kg/day once daily for 6-8 weeks
- Antiplatelet effect: Achieved at low doses (3-5 mg/kg)
- Anti-inflammatory: Requires high doses (80-100 mg/kg)
📌 IVIG Response Criteria: Fever resolution <24-48 hours, ESR/CRP trending down, Vital signs stable, Energy/appetite improving, Rash fading (FEVER mnemonic)
Refractory Kawasaki Management
IVIG-resistant patients (10-20% of cases) require escalated treatment protocols with higher aneurysm risk (15-25%):
-
Definition of IVIG Resistance
- Persistent fever (≥38°C) 36 hours after IVIG completion
- Recurrent fever within 48-72 hours of initial response
- Continued inflammatory markers: ESR/CRP remain elevated
- Clinical deterioration: Worsening symptoms or new findings
-
Second-Line Treatment Options
- Repeat IVIG: 2 g/kg (response rate 70-80%)
- Methylprednisolone: 30 mg/kg/day x 3 days (pulse therapy)
- Infliximab: 5 mg/kg single dose (TNF-α inhibitor)
- Combination therapy: IVIG + steroids for high-risk cases
⭐ Clinical Pearl: Infliximab shows 85% response rates in IVIG-resistant cases and reduces coronary artery Z-scores more effectively than repeat IVIG, with fever resolution typically within 24 hours of administration.
Risk Stratification Treatment Matrix
Treatment intensity varies based on coronary risk assessment and clinical severity:
| Risk Category | Coronary Status | Treatment Protocol | Monitoring Frequency | Duration |
|---|---|---|---|---|
| Standard Risk | Normal echo | IVIG + ASA | Weekly x 2, then monthly | 6-8 weeks |
| Moderate Risk | Z-score 2.0-2.5 | IVIG + ASA + Close F/U | Every 3 days x 2 weeks | 3-6 months |
| High Risk | Z-score >2.5 | IVIG + ASA + Cardiology | Daily until stable | ≥1 year |
| Giant Aneurysm | >8mm diameter | IVIG + ASA + Anticoagulation | Continuous monitoring | Lifelong |
| Refractory | Any + IVIG resistance | Escalated protocol | ICU-level monitoring | Variable |
Giant coronary aneurysms (>8mm or Z-score >10) require anticoagulation due to thrombosis risk:
-
Anticoagulation Indications
- Giant aneurysms: >8mm in children <5 years
- Z-score >10: Regardless of absolute diameter
- Multiple aneurysms: ≥3 coronary segments involved
- Decreased flow: Doppler evidence of sluggish flow
-
Anticoagulation Protocols
- Warfarin: Target INR 2.0-3.0 for giant aneurysms
- Low molecular weight heparin: Enoxaparin 1 mg/kg q12h
- Aspirin continuation: 3-5 mg/kg/day with anticoagulation
- Monitoring: Weekly INR until stable, then monthly
💡 Master This: The "Triple therapy" approach - IVIG + high-dose aspirin + anticoagulation - reduces thrombotic events in giant aneurysms from 15% to <2%, but requires expert cardiology management due to bleeding risks (3-5% incidence).
This evidence-based treatment framework establishes the therapeutic foundation for long-term cardiac monitoring protocols that ensure optimal outcomes through systematic follow-up and complication prevention strategies.
⚖️ Treatment Algorithms: Evidence-Based Intervention Protocols
🔗 Multi-System Integration: The Kawasaki Connectome
Cardiovascular-Immunologic Interface
The immune-cardiac axis drives both acute inflammation and chronic remodeling through interconnected mechanisms:
-
Acute Phase Interactions (Days 1-14)
- Cytokine storm → Endothelial dysfunction → Coronary vasodilation
- TNF-α elevation → Myocardial depression → Reduced ejection fraction
- IL-1β surge → Pericardial inflammation → Effusion in 15% of cases
- Complement activation → Vessel wall damage → Aneurysm formation
-
Subacute Integration (Days 15-40)
- Thrombocytosis → Hypercoagulable state → Thrombosis risk
- Autoantibody formation → Chronic inflammation → Stenosis development
- Tissue remodeling → Fibrosis → Long-term dysfunction
- Immune memory → Recurrence susceptibility → 2-3% repeat episodes
📌 Cardio-Immune Timeline: Inflammation peaks (days 3-7) → Myocardial involvement (days 5-14) → Matrix remodeling (days 15-40) → Ultimate scarring (>40 days) → New baseline established → Enduring surveillance needed (IMMUNE mnemonic)
Genetic-Environmental Integration Matrix
Host susceptibility combines with environmental triggers to determine disease expression and severity:
-
High-Risk Genetic Patterns
- Asian ancestry: 2-3x higher incidence rates
- HLA-B51: Associated with severe coronary involvement
- ITPKC polymorphisms: Increased IVIG resistance risk
- CASP3 variants: Enhanced inflammatory response
-
Environmental Modifiers
- Seasonal clustering: Winter/spring peaks (60% of cases)
- Geographic patterns: Higher latitude correlations
- Infectious triggers: Respiratory virus associations
- Socioeconomic factors: Access to care affects outcomes
⭐ Clinical Pearl: Children with Asian ancestry plus winter onset have 40% higher risk of coronary abnormalities and 2x increased IVIG resistance rates, warranting enhanced monitoring and lower treatment thresholds.
Age-Outcome Integration Patterns
Developmental stage significantly influences disease expression, treatment response, and long-term prognosis:
| Age Group | Presentation Pattern | Coronary Risk | Treatment Response | Long-term Monitoring |
|---|---|---|---|---|
| <6 months | Incomplete (85%) | Very High (40%) | IVIG resistance (25%) | Lifelong cardiology |
| 6mo-2yr | Classic (75%) | High (25%) | Standard response (85%) | Annual echo x 5yr |
| 2-5yr | Complete (90%) | Moderate (15%) | Excellent response (95%) | Standard protocol |
| 5-8yr | Typical (80%) | Low (10%) | Good response (90%) | Reduced intensity |
| >8yr | Atypical (60%) | Variable (15%) | Delayed response (75%) | Extended monitoring |
Multi-system monitoring optimizes treatment decisions through integrated biomarker assessment:
-
Cardiovascular Response Markers
- BNP normalization: <100 pg/mL by day 14
- Echo Z-score improvement: >0.5 reduction by week 2
- Ejection fraction: >55% maintained throughout
- Coronary flow: Normal Doppler patterns restored
-
Immunologic Response Indicators
- CRP decline: >50% reduction within 48 hours
- ESR normalization: <40 mm/hr by week 2
- Neutrophil shift: <70% neutrophils by day 7
- Lymphocyte recovery: >30% lymphocytes by day 10
-
Systemic Integration Markers
- Albumin recovery: >3.0 g/dL by week 2
- Liver function: ALT <40 U/L by week 3
- Platelet normalization: <450,000/μL by week 6
- Energy/appetite: Full recovery by week 2
💡 Master This: Integrated response assessment using cardiovascular (BNP, echo), inflammatory (CRP, ESR), and systemic (albumin, platelets) markers predicts long-term outcomes with 90% accuracy and identifies refractory cases requiring escalated therapy within 48-72 hours.
This comprehensive integration framework provides the foundation for developing personalized monitoring strategies that optimize long-term outcomes through systematic surveillance and early intervention protocols.
🔗 Multi-System Integration: The Kawasaki Connectome
🎯 Clinical Mastery Arsenal: The Kawasaki Command Center
Rapid Recognition Arsenal
30-Second Assessment Protocol for emergency department and clinic encounters:
- CRASH-FEVER Quick Screen
- Conjunctivitis (bilateral, non-purulent) ✓
- Rash (polymorphous, not vesicular) ✓
- Adenopathy (cervical >1.5cm, unilateral) ✓
- Strawberry tongue/oral changes ✓
- Hand/foot erythema/edema/desquamation ✓
- FEVER >5 days, high-grade, antibiotic-resistant ✓
📌 Emergency Decision Rule: Fever ≥5 days + ≥2 CRASH criteria + Age <8 years = Immediate lab workup + echo + pediatric consultation within 4 hours
- High-Yield Discriminators (Memorize these 5 patterns)
- Perineal desquamation: 67% of KD, <5% of mimics
- Bilateral conjunctivitis WITHOUT purulence: 85% KD specificity
- Strawberry tongue + cracked lips: 90% KD when combined
- Thrombocytosis after day 10: 95% KD, rare in infections
- Coronary changes on echo: 100% specific for KD
Treatment Decision Matrix
Evidence-based protocols for immediate clinical decisions:
| Clinical Scenario | Action Required | Timeframe | Success Rate | Monitoring |
|---|---|---|---|---|
| Complete KD | IVIG 2g/kg + ASA | <24 hours | 90% response | Daily x 3 days |
| Incomplete KD | Labs + Echo → Treat if + | <12 hours | 85% response | q8h x 48hr |
| IVIG Resistant | Repeat IVIG or Infliximab | <36 hours | 75% response | Continuous |
| Giant Aneurysm | IVIG + ASA + Anticoag | <6 hours | 95% thrombosis prevention | ICU level |
| Shock/Severe | ICU + IVIG + Steroids | <2 hours | 80% recovery | Intensive |
Laboratory Command Protocols
Systematic lab interpretation for real-time decision making:
- Critical Lab Thresholds (Memorize these numbers)
- ESR >40 mm/hr: 95% sensitivity for active KD
- CRP >30 mg/L: 90% sensitivity for acute inflammation
- Albumin <3.0 g/dL: 70% of KD cases, high specificity
- ALT >50 U/L: 60% of KD, helps distinguish from viral
- Platelets >450,000/μL: Subacute phase marker (day 14+)
Monitoring Excellence Framework
Systematic surveillance protocols for optimal outcomes:
-
Acute Phase Monitoring (Days 1-14)
- Daily: Vital signs, clinical exam, symptom assessment
- 48-72 hours: Post-IVIG response evaluation
- Day 7-10: Repeat echo if initial abnormal
- Weekly: Lab trending (ESR, CRP, CBC, comprehensive panel)
-
Subacute Surveillance (Days 15-40)
- Weekly visits: Clinical assessment + targeted labs
- Echo timing: Week 2, week 6-8, then per protocol
- Aspirin monitoring: Switch to low-dose when fever-free 48hr
- Activity restriction: No contact sports until echo normal
-
Long-term Strategy (Beyond 40 days)
- Standard risk: Annual echo x 5 years, then discharge
- Coronary abnormalities: Lifelong cardiology follow-up
- Giant aneurysms: Anticoagulation + stress testing + angiography
💡 Master This: The "Rule of 3s" - 3 days for IVIG response, 3 weeks for acute resolution, 3 months for inflammatory normalization, 3 years for coronary remodeling, and 30 years for adult cardiac risk assessment.
Emergency Protocols
Crisis management for life-threatening complications:
-
Coronary Thrombosis (<1% incidence)
- Recognition: Chest pain, ECG changes, troponin elevation
- Action: Immediate cardiology, anticoagulation, cardiac cath
- Timeframe: <30 minutes to intervention
-
Kawasaki Shock Syndrome (<5% incidence)
- Recognition: Hypotension, poor perfusion, organ dysfunction
- Action: ICU, fluid resuscitation, inotropes, IVIG + steroids
- Timeframe: <1 hour to stabilization
This comprehensive clinical arsenal provides the complete framework for achieving Kawasaki disease mastery through systematic recognition, evidence-based treatment, and optimal monitoring strategies that ensure excellent patient outcomes across all clinical scenarios.
🎯 Clinical Mastery Arsenal: The Kawasaki Command Center
Practice Questions: Kawasaki disease
Test your understanding with these related questions
A 6-year-old boy presents to his pediatrician accompanied by his mother for evaluation of a rash. The rash appeared a little over a week ago, and since that time the boy has felt tired. He is less interested in playing outside, preferring to remain indoors because his knees and stomach hurt. His past medical history is significant for an upper respiratory infection that resolved uneventfully without treatment 2 weeks ago. Temperature is 99.5°F (37.5°C), blood pressure is 115/70 mmHg, pulse is 90/min, and respirations are 18/min. Physical exam shows scattered maroon macules and papules on the lower extremities. The abdomen is diffusely tender to palpation. There is no cervical lymphadenopathy or conjunctival injection. Which of the following will most likely be found in this patient?











