Post-infectious immune complications US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Post-infectious immune complications. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Post-infectious immune complications US Medical PG Question 1: A 53-year-old female presents with worsening shortness of breath with activity. Physical exam reveals a diastolic murmur with an opening snap. The patient’s medical history is significant for a left hip replacement 10 years ago, and she vaguely recalls an extended period of illness as a child described as several severe episodes of sore throat followed by rash, fever, and joint pains. Administration of which of the following treatments at that time would have been most effective in reducing her risk of developing cardiac disease?
- A. Ciprofloxacin
- B. Vancomycin
- C. Penicillin (Correct Answer)
- D. Acyclovir
- E. Aspirin
Post-infectious immune complications Explanation: ***Penicillin***
- The patient's childhood history of recurrent sore throats, rash, fever, and joint pains is highly suggestive of **rheumatic fever**, a sequela of untreated **Group A Streptococcal (GAS) pharyngitis**.
- **Penicillin** is the most effective antibiotic for treating GAS pharyngitis and preventing subsequent rheumatic fever and its associated **valvular heart disease**, such as the **mitral stenosis** suggested by the diastolic murmur and opening snap.
*Ciprofloxacin*
- **Ciprofloxacin** is a fluoroquinolone antibiotic primarily used for gram-negative bacterial infections and some gram-positive infections, but it is **not the first-line treatment for GAS pharyngitis**.
- Its broad spectrum and potential side effects make it unsuitable for routine use in preventing rheumatic fever.
*Vancomycin*
- **Vancomycin** is a powerful antibiotic reserved for serious infections caused by gram-positive bacteria, particularly **MRSA** and **_Clostridioides difficile_**.
- While it has activity against GAS, it is **not appropriate for treating GAS pharyngitis** due to its reserved status for resistant infections, requirement for IV administration, and potential side effects, making it unsuitable for preventing rheumatic fever.
*Acyclovir*
- **Acyclovir** is an antiviral medication used to treat herpes simplex and varicella-zoster virus infections.
- It has **no antibacterial activity** and would be completely ineffective in treating GAS pharyngitis or preventing rheumatic heart disease.
*Aspirin*
- **Aspirin** is an anti-inflammatory and antiplatelet agent used to manage symptoms of rheumatic fever like **arthralgia** and fever, but it **does not treat the underlying streptococcal infection**.
- While it can alleviate some acute symptoms, it **does not prevent the development of permanent cardiac damage**.
Post-infectious immune complications US Medical PG Question 2: A 6-year-old boy presents to his pediatrician accompanied by his mother for evaluation of a rash. The rash appeared a little over a week ago, and since that time the boy has felt tired. He is less interested in playing outside, preferring to remain indoors because his knees and stomach hurt. His past medical history is significant for an upper respiratory infection that resolved uneventfully without treatment 2 weeks ago. Temperature is 99.5°F (37.5°C), blood pressure is 115/70 mmHg, pulse is 90/min, and respirations are 18/min. Physical exam shows scattered maroon macules and papules on the lower extremities. The abdomen is diffusely tender to palpation. There is no cervical lymphadenopathy or conjunctival injection. Which of the following will most likely be found in this patient?
- A. Coronary artery aneurysms
- B. Leukocytoclastic vasculitis (Correct Answer)
- C. Thrombocytopenia
- D. Mitral regurgitation
- E. Occult malignancy
Post-infectious immune complications Explanation: ***Leukocytoclastic vasculitis***
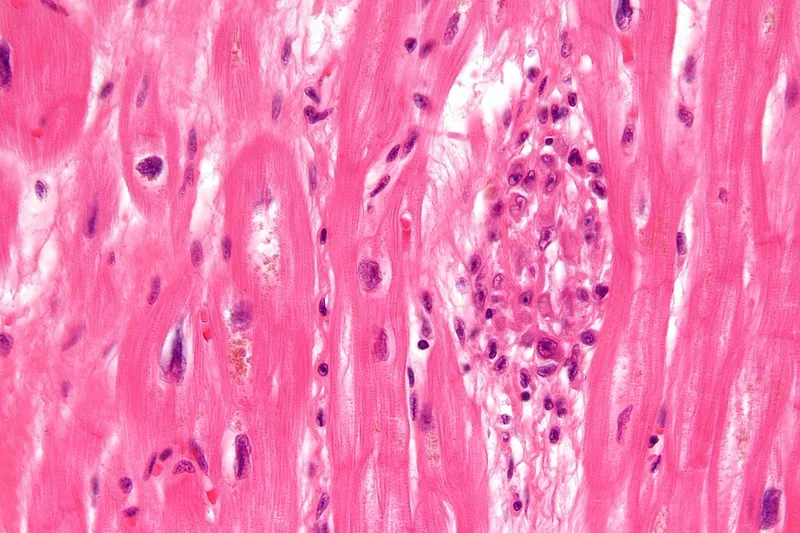
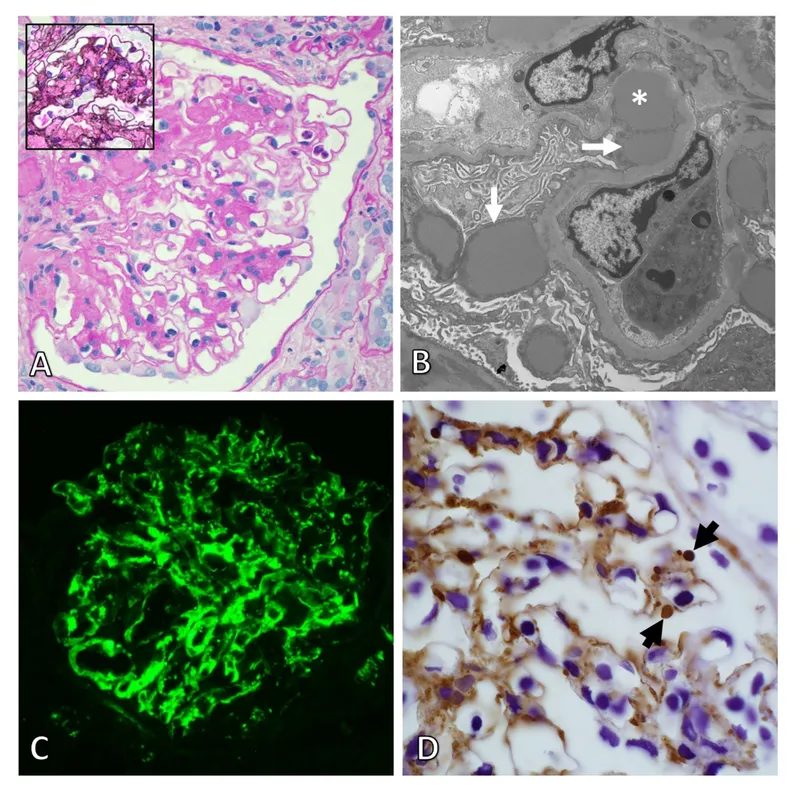
- This patient presents with symptoms highly suggestive of **Henoch-Schönlein Purpura (HSP)**, including a preceding URI, fatigue, low-grade fever, **abdominal pain**, and a **palpable purpura** primarily on the lower extremities.
- HSP is characterized by IgA-mediated **small-vessel vasculitis**, which histologically presents as leukocytoclastic vasculitis with IgA deposition on immunofluorescence.
*Coronary artery aneurysms*
- **Coronary artery aneurysms** are a classic complication of **Kawasaki disease**, not Henoch-Schönlein Purpura.
- Kawasaki disease presents with different clinical features, including prolonged fever, conjunctival injection, oral changes, and cervical lymphadenopathy.
*Thrombocytopenia*
- **Thrombocytopenia** is characterized by a low platelet count and often presents with petechiae, purpura, and bleeding, but the rash in HSP is due to inflammation and extravasation of red blood cells, not low platelets.
- Platelet counts in HSP are typically **normal** or can be slightly elevated as an acute phase reactant.
*Mitral regurgitation*
- **Mitral regurgitation** is a common manifestation of **rheumatic fever**, particularly after recurrent episodes, caused by valvular damage.
- Rheumatic fever is also preceded by infection (Group A Strep) but involves different symptoms like migratory polyarthritis, carditis, chorea, erythema marginatum, and subcutaneous nodules, which are not described here.
*Occult malignancy*
- While an **occult malignancy** can cause paraneoplastic syndromes or constitutional symptoms, the specific constellation of symptoms, including the migratory rash, abdominal pain, and preceding URI, points much more strongly to **HSP** in a 6-year-old.
- The presentation is more consistent with an acute, inflammatory process rather than a chronic, insidious malignant one.
Post-infectious immune complications US Medical PG Question 3: A 7-year-old boy is brought to the physician because of a 5-day history of fever, malaise, and joint pain. He had a sore throat 4 weeks ago that resolved without treatment. His temperature is 38.6°C (101.5°F) and blood pressure is 84/62 mm Hg. Physical examination shows several firm, painless nodules under the skin near his elbows and the dorsal aspect of both wrists. Cardiopulmonary examination shows bilateral basilar crackles and a blowing, holosystolic murmur heard best at the cardiac apex. Both knee joints are warm. Laboratory studies show an erythrocyte sedimentation rate of 129 mm/h. The immune response seen in this patient is most likely due to the presence of which of the following?
- A. M protein (Correct Answer)
- B. CAMP factor
- C. TSST-1
- D. IgA protease
- E. Hyaluronic acid capsule
Post-infectious immune complications Explanation: ***M protein***
- The constellation of symptoms (recent sore throat, fever, joint pain, subcutaneous nodules, and a new heart murmur) is highly suggestive of **acute rheumatic fever (ARF)**, which is triggered by a preceding infection with **Group A Streptococcus (GAS)**.
- The **M protein** is a major virulence factor of GAS that elicits a strong immune response, and antibodies directed against it can cross-react with host tissues (molecular mimicry), leading to the inflammatory damage seen in ARF.
*CAMP factor*
- **CAMP factor** is a virulence factor produced by *Streptococcus agalactiae* (Group B Streptococcus), not Group A Streptococcus, which is responsible for ARF.
- Group B Streptococcus is primarily associated with neonatal infections and does not cause rheumatic fever.
*TSST-1*
- **Toxic Shock Syndrome Toxin-1 (TSST-1)** is a superantigen produced by *Staphylococcus aureus* and is responsible for **toxic shock syndrome**, not acute rheumatic fever.
- Toxic shock syndrome presents with abrupt onset of fever, hypotension, diffuse rash, and multi-organ dysfunction, which differs from the patient's presentation.
*IgA protease*
- **IgA protease** is an enzyme produced by several bacterial species, including *Neisseria meningitidis*, *Haemophilus influenzae*, and *Streptococcus pneumoniae*, that cleaves IgA antibodies.
- While it contributes to bacterial colonization of mucous membranes, it is not the primary virulence factor responsible for the immune response leading to acute rheumatic fever.
*Hyaluronic acid capsule*
- The **hyaluronic acid capsule** of *Streptococcus pyogenes* (GAS) is a virulence factor that helps in evading phagocytosis by mimicking host connective tissue.
- While it prevents immune detection and aids in colonization, it does not directly elicit the cross-reactive immune response responsible for the tissue damage in acute rheumatic fever; that role is attributed primarily to the M protein.
Post-infectious immune complications US Medical PG Question 4: A 14-year-old male is brought to the Emergency Department by his mother. She is worried because his face has become puffy and his urine has turned a tea-color. Patient history reveals the child recently suffered from a sore throat. The physician suspects a bacterial infection. Which of the following describes the likely bacteria responsible?
- A. Gram negative
- B. Bacitracin insensitive
- C. Catalase positive
- D. Beta-hemolytic (Correct Answer)
- E. Coagulase positive
Post-infectious immune complications Explanation: ***Beta-hemolytic***
- The patient's symptoms (puffy face, tea-colored urine, recent sore throat) are classic for **post-streptococcal glomerulonephritis (PSGN)**, which is caused by a prior infection with **Group A Streptococcus (GAS)**.
- **GAS** (Streptococcus pyogenes) is known for its **beta-hemolytic** activity, meaning it completely lyses red blood cells on blood agar, creating clear zones around colonies.
*Gram negative*
- **Group A Streptococcus** (Streptococcus pyogenes) are **Gram-positive cocci**, not Gram-negative.
- Gram-negative bacteria have a different cell wall structure and typically cause different types of infections.
*Bacitracin insensitive*
- **Group A Streptococcus** (Streptococcus pyogenes) is typically **bacitracin sensitive**, meaning its growth is inhibited by bacitracin on a blood agar plate.
- This characteristic is used in laboratory settings to differentiate GAS from other beta-hemolytic streptococci.
*Catalase positive*
- **Group A Streptococcus** (Streptococcus pyogenes) is **catalase negative**, meaning it does not produce the enzyme catalase.
- **Staphylococcus species** are catalase-positive, which is a key differential test between *Staphylococcus* and *Streptococcus*.
*Coagulase positive*
- **Group A Streptococcus** (Streptococcus pyogenes) is **coagulase negative**.
- **Staphylococcus aureus** is a notable coagulase-positive bacterium, and coagulase production is a significant virulence factor for this organism, not for GAS.
Post-infectious immune complications US Medical PG Question 5: A 2-year-old girl who emigrated from Pakistan 2 weeks ago is brought to the emergency department because of lower limb weakness for one-day. One week ago, she had a 3-day episode of flu-like symptoms that resolved without treatment. She has not yet received any routine childhood vaccinations. Deep tendon reflexes are 1+ in the right lower extremity and absent in the left lower extremity. Analysis of cerebrospinal fluid shows a leukocyte count of 38 cells/mm3 (68% lymphocytes), a protein concentration of 49 mg/dL, and a glucose concentration of 60 mg/dL. Which of the following is the most likely diagnosis in this patient?
- A. Poliomyelitis (Correct Answer)
- B. Tetanus
- C. Guillain-Barre syndrome
- D. Botulism
- E. HSV encephalitis
Post-infectious immune complications Explanation: ***Poliomyelitis***
- The patient's presentation with **acute flaccid paralysis** (lower limb weakness with absent reflexes), recent emigration from a region with potential **endemic polio** (Pakistan), and **lack of vaccination** are highly suggestive of poliomyelitis.
- The **CSF findings** (mild pleocytosis with lymphocytic predominance and normal glucose) are consistent with a viral infection of the central nervous system, which is characteristic of polio.
*Tetanus*
- Tetanus typically presents with **spastic paralysis**, muscle rigidity, and **lockjaw**, not flaccid paralysis.
- The onset of symptoms is also usually preceded by a wound contamination, which is not mentioned in this case.
*Guillain-Barre syndrome*
- While GBS can cause **flaccid paralysis** and is often preceded by a viral illness, it typically presents with **ascending paralysis** and the CSF classically shows **albumino-cytological dissociation** (high protein with normal or low cell count), which is not fully consistent with the CSF findings here.
- The rapid onset of significant asymmetry in reflexes is also less typical for GBS.
*Botulism*
- Botulism causes **descending flaccid paralysis**, often starting with cranial nerve palsies (e.g., ptosis, diplopia), and is typically associated with ingestion of contaminated food or honey in infants.
- The patient's symptoms are more focused on lower limb weakness without initial cranial nerve involvement, and the CSF findings are usually normal in botulism.
*HSV encephalitis*
- HSV encephalitis typically presents with **fever, seizures, altered mental status, and focal neurological deficits**, not primarily acute flaccid paralysis.
- While it is a viral encephalitis, the predominant symptom pattern and the specific lower limb weakness are not characteristic of HSV encephalitis.
Post-infectious immune complications US Medical PG Question 6: A 4-year-old boy is brought to the emergency department by his mother with a rash on his trunk, malaise, and fever with spikes up to 38.5°C (101.3°F) for the past 2 weeks. The patient's mother says she tried giving him Tylenol with little improvement. Past medical history includes a spontaneous vaginal delivery at full term. The patient's vaccines are up-to-date and he has met all developmental milestones. On physical examination, his lips are cracking, and he has painful cervical lymphadenopathy. The rash is morbilliform and involves his trunk, palms, and the soles of his feet. There is fine desquamation of the skin of the perianal region. Which of the following anatomical structures is most important to screen for possible complications in this patient?
- A. Mitral valve
- B. Kidneys
- C. Gallbladder
- D. Coronary artery (Correct Answer)
- E. Pylorus
Post-infectious immune complications Explanation: ***Coronary artery***
- The constellation of symptoms, including prolonged fever, rash on trunk, palms, and soles, cracked lips, cervical lymphadenopathy, and perianal desquamation, is highly indicative of **Kawasaki disease**.
- **Coronary artery aneurysms** are the most serious complication of Kawasaki disease, occurring in 15-25% of untreated children, necessitating close monitoring and screening.
*Mitral valve*
- While other forms of vasculitis or rheumatic fever can affect heart valves, **mitral valve** involvement is not a primary or characteristic complication of Kawasaki disease.
- The main cardiac concern in Kawasaki disease is direct arterial inflammation, not valvular dysfunction.
*Kidneys*
- **Renal involvement**, such as acute kidney injury, is not a typical or prominent feature of Kawasaki disease.
- Kawasaki disease primarily targets medium-sized muscular arteries throughout the body, with a predilection for the coronary arteries.
*Gallbladder*
- **Hydrops of the gallbladder** can occur in Kawasaki disease, leading to acute cholecystitis-like symptoms, but it is generally a self-limiting complication.
- While it's a potential finding, it is not as life-threatening or essential to screen for as coronary artery complications.
*Pylorus*
- There is no direct association between Kawasaki disease and primary involvement or complications of the **pylorus**.
- Gastrointestinal symptoms can occur, but these are typically non-specific and do not involve anatomical changes to the pylorus.
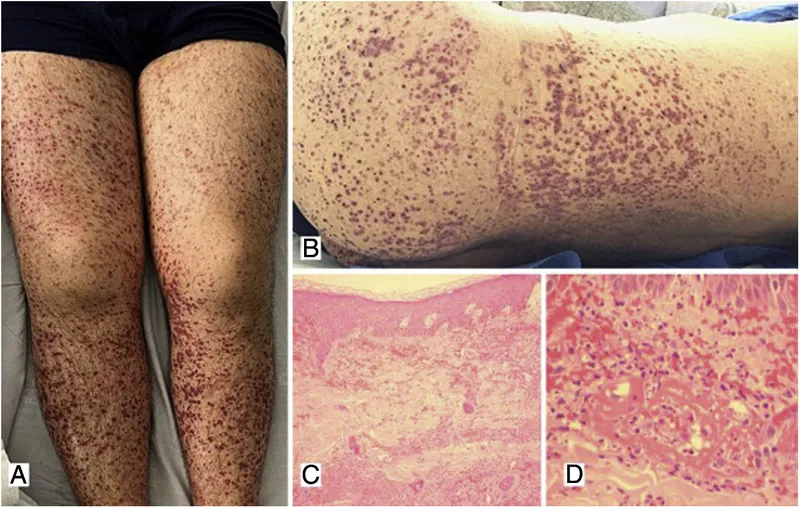
Post-infectious immune complications US Medical PG Question 7: An 11-year-old boy presents with fever and joint pain for the last 3 days. His mother says that he had a sore throat 3 weeks ago but did not seek medical care at that time. The family immigrated from the Middle East 3 years ago. The patient has no past medical history. The current illness started with a fever and a swollen right knee that was very painful. The following day, his knee improved but his left elbow became swollen and painful. While in the waiting room, his left knee is also becoming swollen and painful. Vital signs include: temperature 38.7°C (101.6°F), and blood pressure 110/80 mm Hg. On physical examination, the affected joints are swollen and very tender to touch, and there are circular areas of redness on his back and left forearm (as shown in the image). Which of the following is needed to establish a diagnosis of acute rheumatic fever in this patient?
- A. Elevated erythrocyte sedimentation rate (ESR)
- B. Positive anti-streptococcal serology (Correct Answer)
- C. Elevated leukocyte count
- D. No other criterion is needed to establish the diagnosis of acute rheumatic fever
- E. Prolonged PR interval
Post-infectious immune complications Explanation: ***Positive anti-streptococcal serology***
- A positive anti-streptococcal serology (e.g., elevated ASO titer or anti-DNase B) is a mandatory component for diagnosing **acute rheumatic fever** (ARF) when using the updated Jones criteria, as it confirms a preceding Group A Streptococcal infection.
- Given the history of a recent **sore throat** and clinical manifestations suggestive of ARF (migratory polyarthritis, fever, erythema marginatum), confirmation of a preceding streptococcal infection is crucial.
*Elevated erythrocyte sedimentation rate (ESR)*
- An elevated **ESR** is one of the **minor criteria** for ARF and indicates general inflammation, but it is not sufficient on its own to confirm the diagnosis.
- While supportive of an inflammatory process, it does not confirm the specific etiology of ARF, which requires evidence of a recent **streptococcal infection**.
*Elevated leukocyte count*
- An elevated **leukocyte count** (leukocytosis) is a non-specific indicator of inflammation or infection and is also considered a **minor criterion** for ARF.
- It does not definitively point to ARF or a preceding streptococcal infection and thus cannot solely establish the diagnosis.
*No other criterion is needed to establish the diagnosis of acute rheumatic fever*
- This statement is incorrect because the diagnosis of ARF requires fulfilling specific Jones criteria, which include evidence of a preceding **Group A Streptococcal infection** along with major and/or minor clinical manifestations.
- While the patient exhibits several major criteria (migratory polyarthritis, erythema marginatum), the diagnosis is incomplete without confirming the **streptococcal trigger**.
*Prolonged PR interval*
- A **prolonged PR interval** on an ECG is a sign of **carditis**, which is a **major criterion** for ARF.
- Although carditis can be a significant manifestation, it is not always present in every case and does not replace the requirement for evidence of a preceding **streptococcal infection** for diagnosis.
Post-infectious immune complications US Medical PG Question 8: A 54-year-old man is brought to the emergency department because of progressive tingling and weakness in both of his legs for the past two days. The patient reports that his symptoms interfere with his ability to walk. Two weeks ago, he had an upper respiratory tract infection, which resolved spontaneously. His vital signs are within normal limits. Examination shows weakness in the lower extremities with absent deep tendon reflexes. Reflexes are 1+ in the upper extremities. Sensation to pinprick and light touch is intact. Romberg's test is negative. Laboratory studies show a leukocyte count of 12,000/mm3. Cerebrospinal fluid analysis results show:
Opening pressure normal
Protein 200 mg/dL
Glucose 70 mg/dL
White blood cells 4/mm3
This patient is at increased risk for which of the following conditions?
- A. Respiratory failure (Correct Answer)
- B. Dementia
- C. Hypertrophic cardiomyopathy
- D. Thymoma
- E. Urinary incontinence
Post-infectious immune complications Explanation: ***Respiratory failure***
- The patient's presentation is consistent with **Guillain-Barré Syndrome (GBS)**, characterized by **ascending paralysis**, areflexia, and a history of preceding infection.
- As the paralysis ascends, it can affect the **respiratory muscles** (diaphragm and intercostal muscles), leading to life-threatening respiratory failure requiring mechanical ventilation.
*Dementia*
- **Dementia** is a chronic neurodegenerative condition characterized by progressive cognitive decline, memory impairment, and functional deficits.
- It does not present with acute, rapidly progressing **motor weakness** and **areflexia** as seen in this patient.
*Hypertrophic cardiomyopathy*
- **Hypertrophic cardiomyopathy** is a genetic heart condition causing thickening of the heart muscle, leading to impaired diastolic filling and potential arrhythmias.
- It does not explain the patient's neurological symptoms of **progressive weakness**, **areflexia**, or the characteristic CSF findings.
*Thymoma*
- A **thymoma** is a tumor of the thymus gland, most commonly associated with **myasthenia gravis**, an autoimmune disorder causing fluctuating muscle weakness that worsens with activity.
- The patient's symptoms of progressive, ascending paralysis with absent reflexes are **inconsistent with myasthenia gravis**.
*Urinary incontinence*
- While urinary symptoms can be seen in some neurological conditions, **urinary incontinence** is not a primary or hallmark feature of **Guillain-Barré Syndrome** in its acute phase unless severe autonomic dysfunction or profound flaccid paralysis affecting the bladder occurs.
- The most immediate and life-threatening complication in GBS is respiratory compromise due to ascending paralysis.
Post-infectious immune complications US Medical PG Question 9: A 24-year-old man presents to the emergency department with sudden onset of fever for the past few hours as well as pain and swelling in his right knee and left ankle. He denies any recent history of trauma or injury. The patient is otherwise a healthy, active young man. He recently recovered from a case of gastroenteritis which caused significant abdominal pain and bloody stool 4 weeks ago. He believes the infection was related to eating undercooked chicken while camping. His blood pressure is 124/76 mm Hg, his heart rate is 76/min, and his temperature is 36.9 ℃ (98.4 ℉). Physical examination reveals tenderness to palpation of his right knee and left ankle as well as erythematous conjunctiva. Which of the following features would be least likely to develop in patients with this condition?
- A. Circinate balanitis
- B. Genital ulcers
- C. DIP joint swelling (Correct Answer)
- D. Urethritis
- E. Skin rash
Post-infectious immune complications Explanation: ***DIP joint swelling***
- **Reactive arthritis** typically involves the **large joints** of the lower extremities in an asymmetric pattern, such as the knees and ankles, but spares the **distal interphalangeal (DIP) joints**.
- The patient's history of recent gastroenteritis, subsequent arthritis, and conjunctivitis are classic features of reactive arthritis (formerly Reiter's syndrome), which is a form of **seronegative spondyloarthropathy**.
*Circinate balanitis*
- **Circinate balanitis** is a painless, shallow ulceration of the glans penis that is a characteristic **mucocutaneous manifestation** of reactive arthritis.
- This condition occurs in a significant number of male patients with **HLA-B27 positive** reactive arthritis.
*Genital ulcers*
- **Genital ulcers** are possible cutaneous manifestations of reactive arthritis.
- These can present along with other skin findings such as **keratoderma blennorrhagicum** (pustular psoriasis-like lesions) and circinate balanitis.
*Urethritis*
- **Urethritis** is a common component of the classic triad of symptoms in reactive arthritis ("can't pee, can't see, can't climb a tree").
- It manifests as **dysuria, urinary frequency**, or penile discharge, often following a gastrointestinal or genitourinary infection.
*Skin rash*
- A skin rash, particularly **keratoderma blennorrhagicum**, which resembles pustular psoriasis, is a known *cutaneous manifestation* of reactive arthritis.
- Lesions typically appear on the **palms and soles**, but can also affect the trunk and scalp.
Post-infectious immune complications US Medical PG Question 10: A 14-year-old girl is brought to the physician because of a 1-week history of fever, malaise, and chest pain. She describes the pain as 6 out of 10 in intensity and that it is more severe if she takes a deep breath. The pain is centrally located in the chest and does not radiate. Three weeks ago, she had a sore throat that resolved without treatment. She has no personal history of serious illness. She appears ill. Her temperature is 38.7°C (101.7°F). Examination shows several subcutaneous nodules on the elbows and wrist bilaterally. Breath sounds are normal. A soft early systolic murmur is heard best at the apex in the left lateral position. Abdominal examination is unremarkable. Laboratory studies show:
Hemoglobin 12.6 g/dL
Leukocyte count 12,300/mm3
Platelet count 230,000/mm3
Erythrocyte sedimentation rate 40 mm/hr
Serum
Antistreptolysin O titer 327 U/mL (N < 200 U/mL)
She is treated with aspirin and penicillin and her symptoms resolve. An echocardiography of the heart done 14 days later shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Intramuscular benzathine penicillin every 4 weeks until the age of 21
- B. Intramuscular benzathine penicillin every 4 weeks for 5 years
- C. Intramuscular benzathine penicillin every 4 weeks for 10 years (Correct Answer)
- D. Intramuscular benzathine penicillin every 4 weeks until the age of 40
- E. Low-dose prednisone therapy for a month
Post-infectious immune complications Explanation: ***Intramuscular benzathine penicillin every 4 weeks for 10 years***
- This patient likely has **acute rheumatic fever (ARF)** given the recent **strep infection**, carditis (murmur), polyarthritis (chest pain, malaise), fever, elevated ESR, and subcutaneous nodules, satisfying the **modified Jones criteria**. Although the echocardiogram was normal, the presence of **carditis** (murmur) signifies cardiac involvement during the acute phase.
- Secondary prophylaxis with **intramuscular benzathine penicillin every 4 weeks for 10 years** or until age 21 (whichever is longer) is indicated for patients with ARF and carditis but **no residual heart disease** (as suggested by the follow-up echocardiogram).
*Intramuscular benzathine penicillin every 4 weeks until the age of 21*
- This duration of prophylaxis (until age 21) would only be appropriate if the patient had **ARF without carditis**, which is not the case here.
- The presence of a **soft early systolic murmur** and the subsequent resolution of symptoms with treatment point to carditis during the acute phase, even if residual damage was not found on echocardiogram.
*Intramuscular benzathine penicillin every 4 weeks for 5 years*
- This duration of prophylaxis is typically recommended for patients with **ARF without carditis**.
- Since this patient had clinical evidence of **carditis** during the acute illness (new murmur), a longer duration of prophylaxis is required to prevent recurrent attacks and progressive cardiac damage.
*Intramuscular benzathine penicillin every 4 weeks until the age of 40*
- This duration of prophylaxis is indicated for patients with **ARF and persistent valvular disease (e.g., moderate to severe rheumatic heart disease)**.
- The follow-up echocardiogram showing **no abnormalities** indicates that there is no residual valvular damage at this point, so this duration is unnecessarily long.
*Low-dose prednisone therapy for a month*
- **Corticosteroids (e.g., prednisone)** are used to treat **severe carditis** or **arthritis** in the acute phase of rheumatic fever.
- Since the patient's symptoms have already resolved with aspirin and penicillin, and the question asks for the "next step in management" after the acute phase, long-term prophylaxis for prevention of recurrence is the primary concern, not further acute symptom management.
More Post-infectious immune complications US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.