Pediatric tuberculosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pediatric tuberculosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pediatric tuberculosis US Medical PG Question 1: A 34-year-old female medical professional who works for a non-governmental organization visits her primary care provider for a routine health check-up. She made a recent trip to Sub-Saharan Africa where she participated in a humanitarian medical project. Her medical history and physical examination are unremarkable. A chest radiograph and a tuberculin skin test (PPD) are ordered. The chest radiograph is performed at the side and the PPD reaction measures 12 mm after 72 hours. Which of the following mechanisms is involved in the skin test reaction?
- A. Complement activation
- B. Formation of immune complexes
- C. Th1-mediated delayed-type hypersensitivity (Correct Answer)
- D. IgE cross-linking
Pediatric tuberculosis Explanation: ***Th1-mediated delayed-type hypersensitivity***
- The **tuberculin skin test (PPD)** is a classic example of a **Type IV hypersensitivity reaction**, which is mediated by **T-helper 1 (Th1) cells** [3].
- Upon re-exposure to mycobacterial antigens (tuberculin), previously sensitized Th1 cells release **cytokines** that recruit and activate **macrophages**, leading to the characteristic induration and erythema [3].
*Complement activation*
- This mechanism is primarily involved in host defense against microbial infections and in **Type II** and **Type III hypersensitivity reactions**, not Delayed-Type Hypersensitivity [2].
- Activation of the complement system leads to cell lysis, opsonization, and inflammation, but it does not directly drive the PPD skin test response [2].
*Formation of immune complexes*
- This describes a **Type III hypersensitivity reaction**, where **antigen-antibody complexes** deposit in tissues, leading to inflammation and tissue damage [1].
- Examples include serum sickness and Arthus reaction, which are distinct from the cell-mediated PPD response [1].
*IgE cross-linking*
- This mechanism is characteristic of **Type I (immediate) hypersensitivity reactions**, commonly known as allergies [4].
- **IgE antibodies** bind to mast cells and basophils; subsequent cross-linking by antigens triggers the release of mediators like histamine, leading to rapid allergic symptoms [4].
Pediatric tuberculosis US Medical PG Question 2: A 13-month-old boy is referred to an immunologist with recurrent otitis media, bacterial sinus infections, and pneumonia, which began several months earlier. He is healthy now, but the recurrent nature of these infections are troubling to his parents and they are hoping to find a definitive cause. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. The patient has five older siblings, but none of them had similar recurrent illnesses. Clinical pathology results suggest very low levels of serum immunoglobulin. As you discuss options for diagnosis with the patient’s family, which of the following tests should be performed next?
- A. CSF gram staining
- B. Urine protein screening
- C. Stool cultures
- D. Flow cytometry (Correct Answer)
- E. Genetic analysis
Pediatric tuberculosis Explanation: ***Flow cytometry***
- Flow cytometry is essential for evaluating **lymphocyte subsets** (B cells, T cells, NK cells) and their maturation, which is crucial for diagnosing **primary immunodeficiencies** like X-linked agammaglobulinemia (XLA).
- Given the history of recurrent bacterial infections and **very low serum immunoglobulin levels**, assessing B cell numbers and T cell populations would directly help identify defects in humoral immunity.
*CSF gram staining*
- **CSF gram staining** is used to diagnose **bacterial meningitis** at the time of an active infection.
- The patient is currently healthy, and the test would not identify the underlying cause of recurrent infections or low immunoglobulin levels.
*Urine protein screening*
- **Urine protein screening** is used to detect **kidney disease** or other conditions causing proteinuria.
- It is not relevant to investigating recurrent bacterial infections or low serum immunoglobulin levels, which point towards an immune system defect.
*Stool cultures*
- **Stool cultures** are performed to identify **gastrointestinal infections** (e.g., bacterial, parasitic).
- While infections can occur in immunodeficient patients, this test is not a primary diagnostic tool for the underlying **immunodeficiency** causing recurrent otitis media, sinus infections, and pneumonia.
*Genetic analysis*
- **Genetic analysis** can confirm certain **primary immunodeficiency diagnoses** once specific defects are suspected (e.g., mutations in *BTK* for XLA).
- However, flow cytometry is typically the next step to broadly characterize the immune cell populations and narrowed down differential diagnoses before proceeding with targeted genetic testing.
Pediatric tuberculosis US Medical PG Question 3: You are seeing a patient in clinic who recently started treatment for active tuberculosis. The patient is currently being treated with rifampin, isoniazid, pyrazinamide, and ethambutol. The patient is not used to taking medicines and is very concerned about side effects. Specifically regarding the carbohydrate polymerization inhibiting medication, which of the following is a known side effect?
- A. Vision loss (Correct Answer)
- B. Paresthesias of the hands and feet
- C. Cutaneous flushing
- D. Arthralgias
- E. Elevated liver enzymes
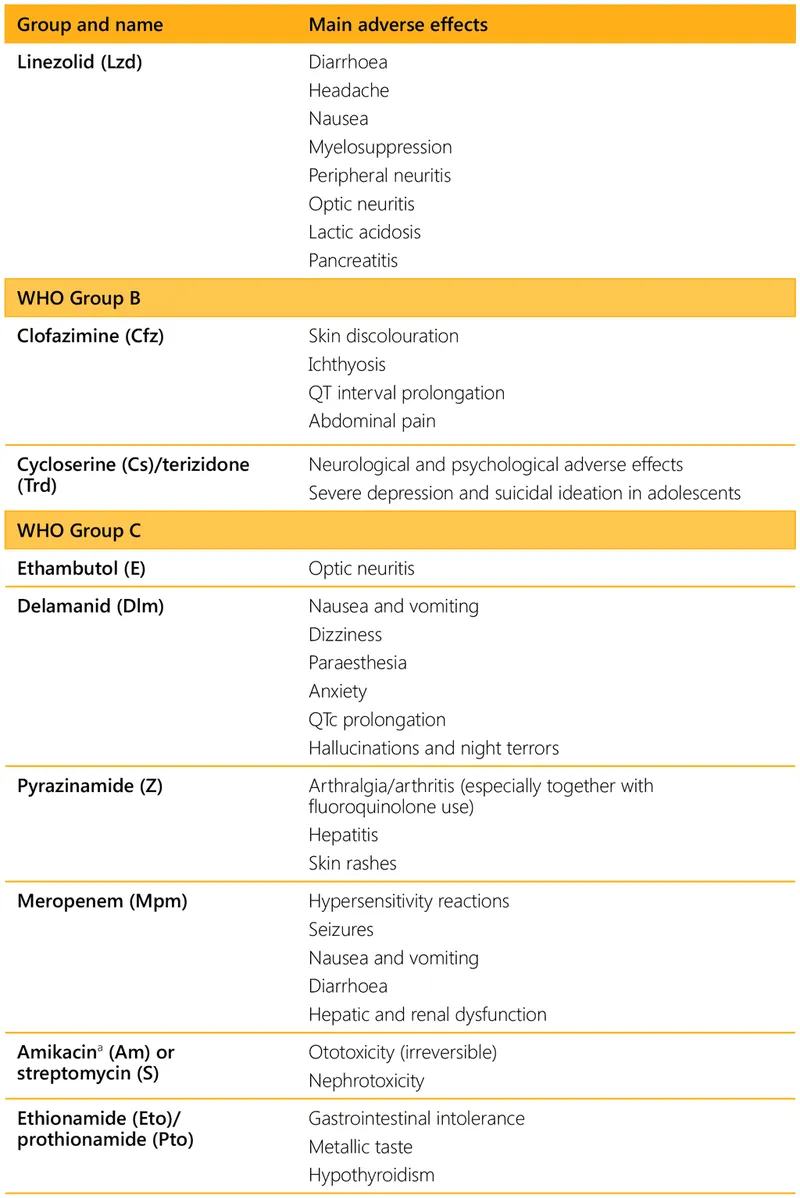
Pediatric tuberculosis Explanation: ***Vision loss***
- The "carbohydrate polymerization inhibiting medication" refers to **ethambutol**, which inhibits **arabinosyl transferase** (involved in mycobacterial cell wall arabinogalactan synthesis)
- **Ethambutol** causes **optic neuritis**, leading to **decreased visual acuity**, **red-green color blindness**, and potentially **irreversible vision loss**
- **Regular ophthalmologic monitoring** is essential during ethambutol therapy
*Paresthesias of the hands and feet*
- This describes **peripheral neuropathy** caused by **isoniazid**
- Isoniazid interferes with **pyridoxine (vitamin B6) metabolism**, leading to neurotoxicity
- Risk factors include malnutrition, diabetes, alcoholism, and pregnancy
- Prevented by **pyridoxine supplementation**
*Cutaneous flushing*
- Not a characteristic side effect of first-line anti-tuberculosis medications
- More commonly associated with niacin or certain allergic/vasodilatory reactions
*Arthralgias*
- Classic side effect of **pyrazinamide**, often affecting small joints
- Caused by **pyrazinamide-induced hyperuricemia** (inhibits renal uric acid excretion)
- May require dose adjustment or discontinuation if severe
*Elevated liver enzymes*
- **Hepatotoxicity** can occur with **rifampin**, **isoniazid**, and **pyrazinamide**
- Requires regular monitoring of liver function tests during TB treatment
- Most common serious adverse effect of combination TB therapy
Pediatric tuberculosis US Medical PG Question 4: A 35-year-old man from Thailand presents with low-grade fever, chronic cough, and night sweats for 3 months. He describes the cough as productive and producing white sputum that is sometimes streaked with blood. He also says he has lost 10 lb in the last 3 months. Past medical history is unremarkable. The patient denies any smoking history, alcohol, or recreational drug use. The vital signs include blood pressure 115/75 mm Hg, heart rate 120/min, respiratory rate 20/min, and temperature 36.6℃ (97.8℉). On physical examination, the patient is ill-looking and thin with no pallor or jaundice. Cardiopulmonary auscultation reveals some fine crackles in the right upper lobe. A chest radiograph reveals a right upper lobe homogeneous density. Which of the following tests would be most helpful in making a definitive diagnosis of active infection in this patient?
- A. PPD test
- B. Silver stain
- C. Ziehl-Neelsen stain (Correct Answer)
- D. Gram stain
- E. Interferon-gamma assay
Pediatric tuberculosis Explanation: ***Ziehl-Neelsen stain***
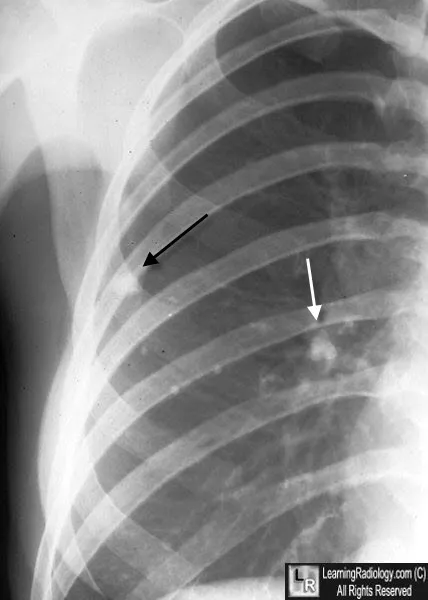
- The patient's symptoms (low-grade fever, chronic cough with white/bloody sputum, night sweats, weight loss) and chest X-ray findings (right upper lobe homogeneous density) are highly suggestive of **active tuberculosis (TB)**, especially given his origin from Thailand (a country with a high TB burden).
- The **Ziehl-Neelsen stain** (acid-fast stain) directly visualizes **acid-fast bacilli** (AFB) like *Mycobacterium tuberculosis* in sputum, providing a rapid and definitive diagnosis of active infection.
*PPD test*
- A **PPD test** (tuberculin skin test) indicates exposure to *Mycobacterium tuberculosis* but cannot differentiate between **latent TB infection** and **active disease**.
- A positive PPD can occur in individuals previously exposed or vaccinated with BCG, offering no direct evidence of current active infection.
*Silver stain*
- **Silver stain** (e.g., Gomori methenamine silver) is used to identify fungal organisms like *Pneumocystis jirovecii* or certain bacteria, such as *Legionella pneumophila*.
- It is not the primary stain for diagnosing tuberculosis, which requires detection of acid-fast bacilli.
*Gram stain*
- **Gram stain** is used to classify bacteria based on their cell wall properties (Gram-positive or Gram-negative).
- *Mycobacterium tuberculosis* has a unique **mycolic acid-rich cell wall** that makes it resistant to Gram staining and requires acid-fast staining for visualization.
*Interferon-gamma assay*
- An **interferon-gamma release assay (IGRA)**, like the Quantiferon-TB Gold test, detects exposure to *Mycobacterium tuberculosis* and is used to diagnose **latent TB infection**.
- Similar to the PPD test, it cannot distinguish between latent infection and **active disease**, and a positive result requires further investigation for active TB.
Pediatric tuberculosis US Medical PG Question 5: A 7-month-old girl is brought to the pediatrician by her parents with a mild, persistent fever for the past week. The patient’s mother also states she is feeding poorly and has become somewhat lethargic. The patient was born at term and the delivery was uncomplicated. The child’s birth weight was 3.5 kg (7.7 lb) and at 6 months was 7.0 kg (15.4 lb). She is fully immunized. The patient’s father recently returned from a business trip to India with a mild cough and was diagnosed with tuberculosis. The patient’s mother tests negative for tuberculosis The patient’s temperature is 38.1℃ (100.5℉). Today, she weighs 7.0 kg (15.4 lb). Cardiopulmonary auscultation reveals diminished breath sounds in the upper lobes. A chest radiograph demonstrates hilar lymphadenopathy and infiltrates in the upper lobes. Gastric aspirates are positive for acid-fast bacilli, however, cultures are still pending. Father and daughter are both started on standard antitubercular therapy. Which of the following is the appropriate management for the patient’s mother?
- A. Isoniazid and rifampicin
- B. Isoniazid alone (Correct Answer)
- C. No medication is required
- D. Isoniazid, rifampicin, and pyrazinamide
- E. Isoniazid, rifampicin, pyrazinamide, and ethambutol
Pediatric tuberculosis Explanation: ***Isoniazid alone***
- The mother is a **close household contact** to TWO active tuberculosis cases (her husband and daughter), placing her at extremely high risk for TB infection.
- Although her TB test is currently **negative**, she may be in the **window period** (8-10 weeks post-exposure before test conversion) or at ongoing risk of infection.
- **Preventive therapy with isoniazid** (daily for 9 months or twice-weekly for 9 months) is recommended by CDC guidelines for high-risk contacts, even with negative initial testing, to prevent development of active TB.
- She should undergo **repeat TB testing in 8-10 weeks** to detect delayed conversion.
*Isoniazid and rifampicin*
- This combination (3-4 months duration) is an **alternative regimen for LTBI treatment**, shorter than isoniazid monotherapy.
- However, for contacts with **negative testing**, single-drug prophylaxis with isoniazid is the standard first-line recommendation.
- This regimen would be appropriate if she had **documented LTBI** (positive test) and needed a shorter course.
*No medication is required*
- This would be **inappropriate** given her extremely high-risk exposure to two household members with active TB.
- Even with negative testing, household contacts warrant preventive therapy due to the risk of recent infection in the window period and ongoing exposure.
- Failure to provide prophylaxis could result in progression to active TB.
*Isoniazid, rifampicin, and pyrazinamide*
- This three-drug regimen is used for the **intensive phase of active TB treatment**, not for preventive therapy in contacts.
- The mother has **no evidence of active disease** (negative test, asymptomatic), so this would be overtreatment with unnecessary toxicity risk.
*Isoniazid, rifampicin, pyrazinamide, and ethambutol*
- This four-drug regimen is the standard for treating **active tuberculosis** or when drug resistance is suspected.
- This represents significant **overtreatment** for a contact with negative testing and no clinical evidence of disease.
- Would expose her to unnecessary adverse effects including hepatotoxicity and optic neuritis.
Pediatric tuberculosis US Medical PG Question 6: A 55-year-old homeless man is presented to the emergency department by a group of volunteers after they found him coughing up blood during 1 of the beneficiary dinners they offer every week. His medical history is unknown as he recently immigrated from Bangladesh. He says that he has been coughing constantly for the past 3 months with occasional blood in his sputum. He also sweats a lot at nights and for the past 2 days, he has been thirsty with increased frequency of urination and feeling hungrier than usual. The respiratory rate is 30/min and the temperature is 38.6°C (101.5°F). He looks emaciated and has a fruity smell to his breath. The breath sounds are reduced over the apex of the right lung. The remainder of the physical exam is unremarkable. Biochemical tests are ordered, including a hemoglobin A1c (HbA1c) (8.5%) and chest radiography reveals cavitations in the apical region of the right lung. Which of the following immune cells is most critical in orchestrating the formation and maintenance of the granulomatous structure that led to these cavitations?
- A. B lymphocytes
- B. Treg lymphocytes
- C. Epithelioid cells
- D. Th1 lymphocytes (Correct Answer)
- E. Th2 lymphocytes
Pediatric tuberculosis Explanation: ***Th1 lymphocytes***
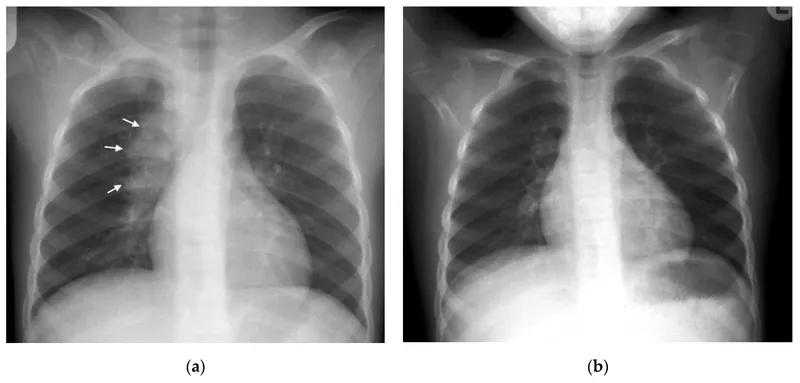
- The clinical picture strongly suggests **reactivation of tuberculosis** due to the cavitary lung lesions, constitutional symptoms, and likely immunocompromise from undiagnosed diabetes (HbA1c 8.5%).
- **Th1 lymphocytes** are crucial for the cell-mediated immune response against **intracellular pathogens** like *Mycobacterium tuberculosis*, producing **interferon-gamma** which activates macrophages to form granulomas and contain the infection, thus preventing dissemination and contributing to cavitation.
*B lymphocytes*
- **B lymphocytes** primarily mediate **humoral immunity** by producing antibodies, which are less critical for controlling intracellular bacterial infections like tuberculosis.
- While antibodies can play a role in modulating inflammation, they are not the primary cells involved in the **granuloma formation** and containment of *M. tuberculosis* within the lungs.
*Treg lymphocytes*
- **Treg lymphocytes** (regulatory T cells) primarily function to **suppress immune responses** to prevent autoimmunity and limit tissue damage.
- While they can modulate the immune response in tuberculosis, their main role is not in the initial formation of **cavities** or primary defense against the pathogen, but rather in regulating the overall inflammatory process.
*Epithelioid cells*
- **Epithelioid cells** are **activated macrophages** that form the core of granulomas, but they are not lymphocytes; they are derived from monocytes.
- They are a crucial component of the **granulomatous structure** itself, but their differentiation and activation are largely driven by cytokines produced by **Th1 lymphocytes**.
*Th2 lymphocytes*
- **Th2 lymphocytes** are primarily involved in immunity against **extracellular parasites** and in allergic reactions, mediating humoral responses through cytokines like **IL-4, IL-5, and IL-13**.
- An effective immune response against *Mycobacterium tuberculosis* is dominated by a **Th1 cellular response**, and a prominent Th2 response is generally considered detrimental or insufficient in controlling the infection.
Pediatric tuberculosis US Medical PG Question 7: A 12-year-old boy is brought in by his mother to the emergency department. He has had abdominal pain, fever, nausea, vomiting, and loss of appetite since yesterday. At first, the mother believed it was just a "stomach flu," but she is growing concerned about his progressive decline. Vitals include: T 102.3 F, HR 110 bpm, BP 120/89 mmHg, RR 16, O2 Sat 100%. Abdominal exam is notable for pain over the right lower quadrant. What is the next best step in management in addition to IV hydration and analgesia?
- A. Upright and supine abdominal radiographs
- B. Abdominal MRI with gadolinium contrast
- C. Abdominal CT scan with IV contrast
- D. Right lower quadrant ultrasound (Correct Answer)
- E. Abdominal CT scan with IV and PO contrast
Pediatric tuberculosis Explanation: ***Right lower quadrant ultrasound***
- In a 12-year-old boy with suspected **appendicitis**, **ultrasound** is the preferred initial imaging modality due to its **lack of radiation** and high diagnostic accuracy in this population.
- It effectively identifies an inflamed **appendix**, periappendiceal fluid, and other relevant findings while avoiding radiation exposure, which is particularly important in children.
*Upright and supine abdominal radiographs*
- **Plain abdominal X-rays** are generally not useful for diagnosing appendicitis as they often do not visualize the appendix directly.
- While they can rule out other causes of abdominal pain like **bowel obstruction** or **perforation** (free air), they lack the sensitivity and specificity for appendicitis.
*Abdominal MRI with gadolinium contrast*
- **MRI** is an excellent alternative to CT, especially in pregnant patients, but it is **less readily available** and consumes more time than ultrasound in an emergent setting for a pediatric patient.
- Though it provides good soft tissue detail without radiation, its **cost and accessibility** make it less practical as a first-line imaging test for suspected appendicitis in children.
*Abdominal CT scan with IV contrast*
- An **abdominal CT scan with IV contrast** is highly accurate for diagnosing appendicitis, but it involves significant **ionizing radiation**, which should be minimized in pediatric patients.
- It is typically reserved for cases where ultrasound findings are equivocal or other diagnoses are strongly suspected, or when the patient is older or body habitus limits ultrasound utility.
*Abdominal CT scan with IV and PO contrast*
- Adding **oral contrast** to a CT scan significantly increases the time before imaging can be performed, which is not ideal in an acute emergency like suspected appendicitis.
- While it can help delineate bowel loops, the additional contrast and associated delay are usually **unnecessary** for diagnosing appendicitis and further expose the child to radiation.
Pediatric tuberculosis US Medical PG Question 8: A 16-year-old boy comes to the emergency department because of painful urination and urethral discharge for 3 days. He has multiple sexual partners and only occasionally uses condoms. His vital signs are within normal limits. The result of nucleic acid amplification testing for Neisseria gonorrhoeae is positive. The patient requests that his parents not be informed of the diagnosis. Which of the following initial actions by the physician is most appropriate?
- A. Order urinary PCR testing in two weeks
- B. Request parental consent prior to prescribing antibiotics
- C. Administer intramuscular and oral antibiotics (Correct Answer)
- D. Perform urethral swab culture for antibiotic sensitivities
- E. Discuss results with patient's primary care physician
Pediatric tuberculosis Explanation: ***Administer intramuscular and oral antibiotics***
- As a minor, this patient falls under the principle of **mature minor doctrine** and state laws allowing minors to consent to their own STI treatment without parental approval. Treating the infection promptly is crucial to prevent complications and further spread.
- The positive **nucleic acid amplification test (NAAT)** for *Neisseria gonorrhoeae* confirms the diagnosis, necessitating immediate treatment with appropriate antibiotics (e.g., ceftriaxone 500 mg intramuscularly, with consideration for azithromycin 1g orally if chlamydia co-infection is suspected).
*Order urinary PCR testing in two weeks*
- This action is premature as the patient requires immediate treatment for a confirmed infection; **waiting two weeks** could lead to disease progression and transmission.
- **Repeat testing** is typically indicated 3 months after treatment to confirm eradication and screen for re-infection, not 2 weeks.
*Request parental consent prior to prescribing antibiotics*
- The **mature minor doctrine** and specific state laws allow minors to consent to treatment for sexually transmitted infections (STIs) without parental notification or consent in most US jurisdictions.
- Delaying treatment to seek parental consent could lead to worsening infection, increased infectivity, and does not respect the minor's **confidentiality rights** in this context.
*Perform urethral swab culture for antibiotic sensitivities*
- While helpful for management of resistant cases, a **urethral swab culture for sensitivities** is not the initial most appropriate action when a NAAT is already positive for *Neisseria gonorrhoeae*.
- **Empiric treatment** based on current CDC guidelines for uncomplicated gonorrhea is the standard and most appropriate first step due to the urgency of treatment and high cure rates with recommended regimens.
*Discuss results with patient's primary care physician*
- While the patient's primary care physician (PCP) should ultimately be informed for continuity of care, the **immediate priority** is to treat the acute infection and protect the patient's confidentiality.
- This discussion should only occur with the patient's consent, especially concerning sensitive information like STI diagnoses for a **minor**.
Pediatric tuberculosis US Medical PG Question 9: A 3-year-old girl is brought to the emergency department by her parents with sudden onset shortness of breath. They tell the emergency physician that their daughter was lying on the bed watching television when she suddenly began gasping for air. They observed a bowl of peanuts lying next to her when they grabbed her up and brought her to the emergency department. Her respirations are 25/min, the pulse is 100/min and the blood pressure is 90/65 mm Hg. The physical findings as of now are apparently normal. She is started on oxygen and is sent in for a chest X-ray. Based on her history and physical exam findings, the cause of her current symptoms would be seen on the X-ray at which of the following sites?
- A. The superior segment of the right lower lobe
- B. The posterior segment of the right lower lobe (Correct Answer)
- C. The lingula of the left upper lobe
- D. The apical segment of the right upper lobe
- E. The apical segment of the left upper lobe
Pediatric tuberculosis Explanation: ***The posterior segment of the right lower lobe***
- This is the **most common site for foreign body aspiration in a supine or lying down position** due to gravity and anatomical orientation.
- The history explicitly states the child was **"lying on the bed watching television"** when aspiration occurred, making the **posterior segment of the right lower lobe** the most gravity-dependent and therefore most likely location.
- The **right main bronchus** is wider, shorter, and more vertical than the left, making the right lung the predominant site for aspiration, and in supine position, the posterior segment is most dependent [1, 2].
*The superior segment of the right lower lobe*
- The **superior segment of the right lower lobe** is the most common site for aspiration in **upright, standing, or semi-upright positions**, not in a supine position.
- Since the child was lying down (supine), gravity would direct the aspirated peanut to the **posterior segment** rather than the superior segment.
- This would be correct if the child had aspirated while sitting upright.
*The lingula of the left upper lobe*
- The **lingula** is an uncommon site for aspiration because the **left main bronchus** has a sharper angle and smaller diameter compared to the right bronchus [2].
- The anatomical differences make aspiration into the right lung significantly more common than the left lung [2].
- The lingula is not a gravity-dependent area in the supine position.
*The apical segment of the right upper lobe*
- The **apical segment of the right upper lobe** is associated with aspiration when the patient is in **Trendelenburg position** (head lower than feet) or in extreme head-down positions.
- The described scenario of lying flat on the bed does not favor aspiration into apical segments, which are non-gravity-dependent in supine position.
- This location would be contra-gravity in the supine position.
*The apical segment of the left upper lobe*
- Aspiration into the **left upper lobe** is less frequent than the right lung due to the sharper angle of the left main bronchus [2].
- The **apical segment** would require head-down positioning (Trendelenburg) that is not described in this clinical scenario.
- This is the least likely location given both the supine position and left-sided anatomy.
Pediatric tuberculosis US Medical PG Question 10: A 10-year-old girl with a rash is brought to the clinic by her mother. The patient’s mother says that the onset of the rash occurred 2 days ago. The rash was itchy, red, and initially localized to the cheeks with circumoral pallor, and it gradually spread to the arms and trunk. The patient’s mother also says her daughter had been reporting a high fever of 39.4°C (102.9°F), headaches, myalgia, and flu-like symptoms about a week ago, which resolved in 2 days with acetaminophen. The patient has no significant past medical history. Her vital signs include: temperature 37.0°C (98.6°F), pulse 90/min, blood pressure 125/85 mm Hg, respiratory rate 20/min. Physical examination shows a symmetric erythematous maculopapular rash on both cheeks with circumoral pallor, which extends to the patient’s trunk, arms, and buttocks. The remainder of the exam is unremarkable. Laboratory findings are significant for a leukocyte count of 7,100/mm3 and platelet count of 325,000/mm3. Which of the following is the next best step in the management of this patient?
- A. Administer intravenous immunoglobulin (IVIG)
- B. Discharge home, saying that the patient may return to school after the disappearance of the rash
- C. Transfuse with whole blood
- D. Discharge home with instructions for strict isolation from pregnant women until disappearance of the rash
- E. Discharge home, saying that the patient may immediately return to school (Correct Answer)
Pediatric tuberculosis Explanation: ***Discharge home, saying that the patient may immediately return to school***
- This patient likely has **Fifth Disease (Erythema Infectiosum)**, caused by **Parvovirus B19**, characterized by a **"slapped cheek" rash** and a **lacy, reticular rash** on the trunk and extremities.
- Patients with Fifth Disease are **contagious before the rash appears** and are generally **no longer contagious once the rash develops**, making immediate return to school safe.
*Administer intravenous immunoglobulin (IVIG)*
- **IVIG** is typically reserved for **severe cases of Parvovirus B19 infection** in immunocompromised individuals or those with chronic hemolytic anemias who develop **aplastic crisis**.
- The patient's symptoms are mild and self-limiting, without evidence of severe complications like aplastic anemia (normal leukocyte and platelet counts).
*Discharge home, saying that the patient may return to school after the disappearance of the rash*
- This advice is incorrect because the patient is **no longer contagious once the rash erupts**.
- Requiring isolation until the rash disappears would be unnecessarily disruptive and is not medically indicated for Fifth Disease.
*Transfuse with whole blood*
- **Whole blood transfusion** is not indicated for uncomplicated Fifth Disease, as it can cause significant complications.
- Transfusions are considered only in cases of **severe aplastic crisis** with significant anemia, which is not present in this patient (normal complete blood count).
*Discharge home with instructions for strict isolation from pregnant women until disappearance of the rash*
- While exposure to **Parvovirus B19 in pregnant women** can lead to significant fetal complications (e.g., hydrops fetalis), the patient is **no longer infectious once the rash appears**.
- Therefore, strict isolation from pregnant women **after rash onset** is not necessary, as the risk of transmission has passed.
More Pediatric tuberculosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.