Pediatric respiratory infections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pediatric respiratory infections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pediatric respiratory infections US Medical PG Question 1: A 6-year-old boy and his parents present to the emergency department with high-grade fever, headache, and projectile vomiting. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. Past medical history is noncontributory. He has had no sick contacts at school or at home. The family has not traveled out of the area recently. He likes school and playing videogames with his younger brother. Today, his blood pressure is 115/76 mm Hg, heart rate is 110/min, respiratory rate is 22/min, and temperature is 38.4°C (101.2°F). On physical exam, the child is disoriented. Kernig’s sign is positive. A head CT was performed followed by a lumbar puncture. Several aliquots of CSF were distributed throughout the lab. Cytology showed high counts of polymorphs, biochemistry showed low glucose and elevated protein levels, and a gram smear shows gram-positive lanceolate-shaped cocci alone and in pairs. A smear is prepared on blood agar in an aerobic environment and grows mucoid colonies with clearly defined edges and alpha hemolysis. On later evaluation they develop a ‘draughtsman’ appearance. Which one of the following is the most likely pathogen?
- A. Streptococcus pneumoniae (Correct Answer)
- B. Staphylococcus aureus
- C. Neisseria meningitidis
- D. Staphylococcus epidermidis
- E. Streptococcus agalactiae
Pediatric respiratory infections Explanation: ***Streptococcus pneumoniae***
- The CSF findings of **high polymorphs**, **low glucose**, and **elevated protein** are classic for bacterial meningitis. The Gram stain showing **Gram-positive, lanceolate-shaped cocci in pairs** is highly characteristic of *Streptococcus pneumoniae*.
- The growth of **mucoid colonies** with **alpha hemolysis** on blood agar in an aerobic environment, which later develop a **'draughtsman' appearance**, are further confirmatory characteristics of *S. pneumoniae*.
*Staphylococcus aureus*
- *Staphylococcus aureus* is a Gram-positive coccus but typically presents in **clusters** on Gram stain, not lanceolate pairs.
- While it can cause meningitis, it usually exhibits **beta-hemolysis** and is catalase-positive, unlike *S. pneumoniae*.
*Neisseria meningitidis*
- *Neisseria meningitidis* is a **Gram-negative diplococcus**, which would appear distinctly different on Gram stain compared to the described Gram-positive lanceolate cocci.
- Although it is a common cause of bacterial meningitis, its colonial morphology and Gram stain characteristics do not match the case.
*Staphylococcus epidermidis*
- *Staphylococcus epidermidis* is a **Gram-positive coccus in clusters**, similar to *S. aureus*, and is commonly a **skin commensal** or found in infections related to indwelling devices.
- It typically exhibits **gamma-hemolysis** (non-hemolytic) and is usually **coagulase-negative**, differentiating it from the alpha-hemolytic, 'draughtsman' appearing colonies described.
*Streptococcus agalactiae*
- *Streptococcus agalactiae* (**Group B Streptococcus**) is a Gram-positive coccus that typically grows in **chains** and causes **beta-hemolysis**, particularly in neonates.
- While it can cause meningitis, its characteristic hemolytic pattern and arrangement on Gram stain differ from the alpha-hemolytic, lanceolate-shaped cocci in pairs described.
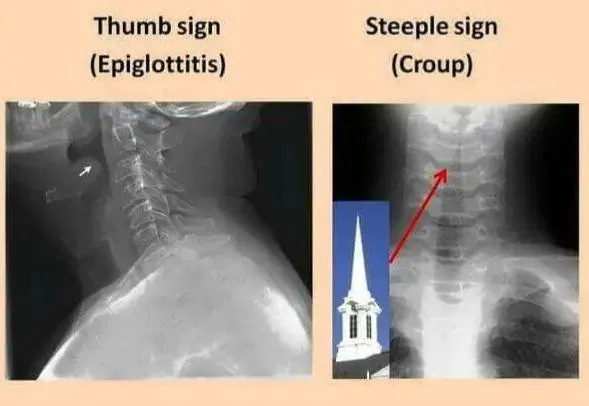
Pediatric respiratory infections US Medical PG Question 2: A 3-year-old girl is brought to the physician by her parents because of a barking cough, a raspy voice, and noisy breathing for the last 3 days. Five days ago, she had a low-grade fever and runny nose. She attends daycare. Her immunizations are up-to-date. Her temperature is 37.8°C (100°F) and respirations are 33/min. Physical examination shows supraclavicular retractions. There is a high-pitched sound present on inspiration. Examination of the throat shows erythema without exudates. Which of the following is the most likely location of the anatomic narrowing causing this patient's symptoms?
- A. Bronchioles
- B. Pharynx
- C. Subglottic larynx (Correct Answer)
- D. Distal trachea
- E. Epiglottis
Pediatric respiratory infections Explanation: ***Subglottic larynx***
- The patient's symptoms of **barking cough**, **raspy voice**, **stridor** (high-pitched inspiratory sound), and **supraclavicular retractions** are classic for **croup** (laryngotracheobronchitis), which is caused by inflammation and narrowing of the subglottic region of the larynx.
- The preceding low-grade fever and runny nose are typical of a viral upper respiratory infection, which commonly precedes croup.
*Bronchioles*
- Narrowing in the bronchioles typically causes **wheezing** (a high-pitched whistling sound on expiration) and **respiratory distress**, often seen in conditions like **bronchiolitis** or **asthma**.
- A barking cough and raspy voice are not characteristic symptoms of bronchiolar obstruction.
*Pharynx*
- Inflammation and narrowing of the pharynx primarily cause **sore throat**, **difficulty swallowing** (dysphagia), and sometimes **muffled voice**.
- It would not typically lead to a barking cough, stridor, or severe inspiratory distress.
*Distal trachea*
- While tracheal narrowing can cause stridor, the classic **barking cough** and **hoarseness** (raspy voice) are more specifically localized to the laryngeal area.
- Obstruction in the distal trachea would be less likely to affect voice quality as significantly as subglottic narrowing.
*Epiglottis*
- **Epiglottitis** presents as a rapidly progressive, life-threatening condition with **high fever**, **dysphagia**, **drooling**, and a **muffled "hot potato" voice**.
- The patient would typically appear toxic and prefer to sit in the **tripod position**, which is not described in this case, and her symptoms are less acute.
Pediatric respiratory infections US Medical PG Question 3: A 2-year-old boy is brought to the physician by his parents for the evaluation of an unusual cough, a raspy voice, and noisy breathing for the last 2 days. During this time, the symptoms have always occurred in the late evening. The parents also report that prior to the onset of these symptoms, their son had a low-grade fever and a runny nose for 2 days. He attends daycare. His immunizations are up-to-date. His temperature is 37.8°C (100°F) and respirations are 33/min. Physical examination shows supraclavicular retractions. There is a high-pitched breath sound on inspiration. Which of the following is the most likely location of the abnormality?
- A. Epiglottis
- B. Subglottic larynx (Correct Answer)
- C. Supraglottic larynx
- D. Bronchioles
- E. Bronchi
Pediatric respiratory infections Explanation: ***Subglottic larynx***
- The symptoms of **barking cough**, **raspy voice**, and **inspiratory stridor** (high-pitched breath sound on inspiration) are classic for **croup (laryngotracheobronchitis)**.
- Croup is characterized by **inflammation and edema of the subglottic larynx**, which is the narrowest part of the pediatric airway, leading to obstruction.
*Epiglottis*
- **Epiglottitis** typically presents with a sudden onset of **high fever**, **dysphagia**, drooling, and a muffled voice, often without a preceding viral prodrome.
- Patients with epiglottitis usually appear severely ill and may adopt a **tripod position** to maximize airway opening, which is not described here.
*Supraglottic larynx*
- While inflammation can occur here, severe **supraglottic edema** leading to the described symptoms (especially the barking cough) is uncommon in typical croup.
- Conditions affecting the supraglottic area, such as **supraglottitis**, often cause a muffled voice and severe dysphagia, rather than a raspy voice and classic croupy cough.
*Bronchioles*
- Inflammation of the bronchioles typically causes **bronchiolitis**, characterized by **wheezing**, tachypnea, and increased work of breathing due to small airway obstruction.
- This condition does not typically present with a **barking cough** or **stridor**, which are indicative of upper airway obstruction.
*Bronchi*
- Inflammation of the bronchi (**bronchitis**) primarily causes a **cough** (often productive) and sometimes wheezing or rhonchi.
- It does not typically result in **stridor** or a **raspy voice**, as these symptoms arise from laryngeal or tracheal involvement.
Pediatric respiratory infections US Medical PG Question 4: A 6-month-old male presents for a routine visit to his pediatrician. Two months ago, the patient was seen for tachypnea and wheezing, and diagnosed with severe respiratory syncytial virus (RSV) bronchiolitis. After admission to the hospital and supportive care, the patient recovered and currently is not experiencing any trouble breathing. Regarding the possibility of future reactive airway disease, which of the following statements is most accurate?
- A. “There is no clear relationship between RSV and the development of asthma.”
- B. “Your child has a greater than 20% chance of developing asthma” (Correct Answer)
- C. “Your child’s risk of asthma is less than the general population.”
- D. “Your child has a less than 5% chance of developing asthma”
- E. “Your child’s risk of asthma is the same as the general population.”
Pediatric respiratory infections Explanation: ***“Your child has a greater than 20% chance of developing asthma”***
- Severe **RSV bronchiolitis** in infancy is a significant risk factor for the development of **recurrent wheezing** and **childhood asthma**.
- Studies estimate that a substantial proportion, often greater than 20%, of infants with severe RSV bronchiolitis will go on to develop **asthma** later in childhood.
*“There is no clear relationship between RSV and the development of asthma.”*
- This statement is incorrect as there is a **well-established link** between severe RSV infection in early life and an increased risk of developing **asthma**.
- Numerous epidemiological and longitudinal studies have documented this association.
*“Your child’s risk of asthma is less than the general population.”*
- This is incorrect, as severe RSV infection **increases** the risk of asthma, not decreases it.
- Children with a history of severe RSV have a **higher incidence** of asthma compared to the general pediatric population.
*“Your child has a less than 5% chance of developing asthma”*
- This percentage is **too low** given the known association between severe RSV bronchiolitis and subsequent asthma.
- The actual risk is considerably higher, typically falling into the range of 20-50% for those with severe RSV.
*“Your child’s risk of asthma is the same as the general population.”*
- This statement is inaccurate because severe RSV infection in infancy is a recognized independent **risk factor** for **asthma development**.
- Therefore, the child's risk is elevated above that of the general population.
Pediatric respiratory infections US Medical PG Question 5: A patient is hospitalized for pneumonia. Gram-positive cocci in clusters are seen on sputum gram stain. Which of the following clinical scenarios is most commonly associated with this form of pneumonia?
- A. Elderly patient who has trouble swallowing and poor dentition
- B. An alcoholic with evidence of empyema and "currant jelly sputum"
- C. An otherwise healthy young adult with a week of mild fatigue, chills, and cough
- D. Hospitalized adult with development of pneumonia symptoms 2 weeks following a viral illness (Correct Answer)
- E. HIV positive adult with a CD4 count less than 150 and an impaired diffusion capacity
Pediatric respiratory infections Explanation: ***Hospitalized adult with development of pneumonia symptoms 2 weeks following a viral illness***
- Gram-positive cocci in clusters suggests **Staphylococcus aureus**, which is a common cause of secondary bacterial pneumonia, often following **viral illnesses** (e.g., influenza).
- This scenario represents a classic presentation of **secondary bacterial pneumonia**, where the initial viral infection compromises the respiratory defenses, allowing bacterial superinfection.
*Elderly patient who has trouble swallowing and poor dentition*
- This scenario points towards **aspiration pneumonia**, often caused by a **polymicrobial infection** that includes oral anaerobes, not typically dominated by Gram-positive cocci in clusters.
- While *S. aureus* can cause aspiration pneumonia, the primary concern in this context would be **anaerobic bacteria**, given the aspiration risk factors.
*An alcoholic with evidence of empyema and \"currant jelly sputum\"*
- This description is highly suggestive of **Klebsiella pneumoniae** infection, which typically presents with thick, gelatinous, and often **blood-tinged sputum**.
- **Klebsiella** is a Gram-negative rod, not Gram-positive cocci in clusters.
*An otherwise healthy young adult with a week of mild fatigue, chills, and cough*
- This presentation is more consistent with **atypical pneumonia** caused by organisms like **Mycoplasma pneumoniae** or **Chlamydophila pneumoniae**, which would not show Gram-positive cocci in clusters on sputum stain.
- **Streptococcus pneumoniae** (Gram-positive cocci in chains) can also cause community-acquired pneumonia in otherwise healthy individuals, but the "clusters" indicate **Staphylococcus aureus**.
*HIV positive adult with a CD4 count less than 150 and an impaired diffusion capacity*
- This clinical picture strongly suggests **Pneumocystis jirovecii pneumonia (PJP)**, which is common in severely immunocompromised HIV patients.
- *P. jirovecii* is a fungus and would not be seen as Gram-positive cocci in clusters on a routine Gram stain.
Pediatric respiratory infections US Medical PG Question 6: A 9-year-old girl presents with a 3-week history of cough. Her mother reports that initially, she had a runny nose and was tired, with a slight cough, but as the runny nose resolved, the cough seemed to get worse. She further states that the cough is dry sounding and occurs during the day and night. She describes having coughing spasms that occasionally end in vomiting, but between episodes of coughing she is fine. She reports that during a coughing spasm, her daughter will gasp for air and sometimes make a “whooping” noise. A nasopharyngeal swab confirms a diagnosis of Bordetella pertussis. Which of the following statements apply to this patient?
- A. She should be started on azithromycin for more rapid resolution of cough.
- B. Her classmates should be treated with clarithromycin as prophylaxis.
- C. She will have lifelong natural immunity against Bordetella pertussis.
- D. Her 3-month-old brother should be treated with azithromycin as prophylaxis. (Correct Answer)
- E. Her classmates should receive a Tdap booster regardless of their vaccination status.
Pediatric respiratory infections Explanation: ***Her 3-month-old brother should be treated with azithromycin as prophylaxis.***
- The patient's 3-month-old brother is at a very high risk of severe pertussis due to his age and direct exposure, making **post-exposure prophylaxis (PEP)** crucial.
- **Azithromycin** is the recommended antibiotic for PEP in infants due to its efficacy and safety profile.
*She should be started on azithromycin for more rapid resolution of cough.*
- While **azithromycin** is the recommended treatment for pertussis, it is primarily effective in reducing the transmission of *Bordetella pertussis* if started early in the **catarrhal stage**.
- Once the patient is in the **paroxysmal (whooping cough) stage**, as described by the 3-week cough and "whooping" noises, antibiotics **do not significantly shorten the duration or severity of the cough**.
*Her classmates should be treated with clarithromycin as prophylaxis.*
- **Classmates** are generally considered at lower risk for severe disease compared to household contacts, and routine prophylaxis for an entire classroom is not typically recommended unless there is a specific outbreak investigation or direct close contact.
- If prophylaxis were considered for close contacts, **azithromycin** is generally preferred over clarithromycin in children due to fewer drug interactions and a more convenient dosing schedule.
*She will have lifelong natural immunity against Bordetella pertussis.*
- **Natural immunity** following a pertussis infection is not lifelong; it wanes over time, typically within a few years.
- This is why **booster vaccinations (Tdap)** are recommended for adolescents and adults to maintain protection.
*Her classmates should receive a Tdap booster regardless of their vaccination status.*
- **Tdap boosters** are recommended for adolescents and adults, but giving a booster *regardless of vaccination status* to all classmates is not the standard immediate public health response for isolated pertussis cases.
- Public health guidance often focuses on identifying and vaccinating **unvaccinated** or **under-vaccinated close contacts**, rather than providing universal boosters for an entire class.
Pediatric respiratory infections US Medical PG Question 7: A 3-month-old boy is brought to the emergency room by his mother for 2 days of difficulty breathing. He was born at 35 weeks gestation but has otherwise been healthy. She noticed a cough and some trouble breathing in the setting of a runny nose. His temperature is 100°F (37.8°C), blood pressure is 64/34 mmHg, pulse is 140/min, respirations are 39/min, and oxygen saturation is 93% on room air. Pulmonary exam is notable for expiratory wheezing and crackles throughout and intercostal retractions. Oral mucosa is noted to be dry. Which of the following is the most appropriate diagnostic test?
- A. Chest radiograph
- B. Sputum culture
- C. Viral culture
- D. Polymerase chain reaction
- E. No further testing needed (Correct Answer)
Pediatric respiratory infections Explanation: ***No further testing needed***
- This patient presents with classic signs and symptoms of **bronchiolitis**, including a **preterm infant** (risk factor), **URI symptoms** followed by **respiratory distress** (cough, difficulty breathing), **expiratory wheezing**, and **crackles**.
- Bronchiolitis is a clinical diagnosis, and **routine testing** like chest X-rays or viral studies is generally **not recommended** for uncomplicated cases as it rarely changes management unless there are atypical features or concerns for other diagnoses.
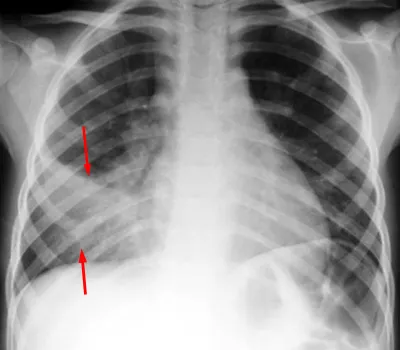
*Chest radiograph*
- A chest X-ray is generally **not indicated** for typical bronchiolitis presentations. It may show hyperinflation or peribronchial thickening but these findings often do not alter management.
- It should only be considered if there are atypical signs, such as a localized finding on exam or concern for **pneumonia** or **atelectasis**, which are not strongly suggested here.
*Sputum culture*
- **Infants** typically **do not produce sputum** for culture.
- Bronchiolitis is primarily a **viral infection**, making bacterial sputum cultures **irrelevant** for initial diagnosis and management unless secondary bacterial infection is strongly suspected, for which there is no evidence here.
*Viral culture*
- While bronchiolitis is caused by viruses, typically **RSV**, **routine viral culture** or rapid antigen testing for RSV is usually **not necessary** for diagnosis in typical cases.
- Identification of the specific virus does not change the clinical management, which is primarily **supportive care**.
*Polymerase chain reaction*
- **PCR testing** can identify viral pathogens but is generally **not recommended** for uncomplicated bronchiolitis cases as it does not change the management plan, which focuses on supportive care.
- It might be considered in severe cases, for **infection control** purposes in a hospital setting, or if there is a specific need for **epidemiological surveillance**, none of which are described as immediate priorities for this patient.
Pediatric respiratory infections US Medical PG Question 8: A 6-month old child is brought to the ER by parents for one day of fever, decreased feeding, and lethargy. They report that neither she nor her siblings are immunized due to their concerns about vaccinations. On exam, the infant is toxic-appearing. Antibiotics are started and lumbar puncture reveals bacterial meningitis caused by a gram-negative, encapsulated organism that requires chocolate agar and the two factors shown in Image A for growth. Which organism does this best describe?
- A. Group B Streptococcus
- B. Haemophilus influenzae (Correct Answer)
- C. Moraxella catarrhalis
- D. Streptococcus pneumoniae
- E. Listeria monocytogenes
Pediatric respiratory infections Explanation: **Haemophilus influenzae**
- This organism is a **gram-negative, encapsulated coccobacillus** that requires **chocolate agar** and **factors X (hemin) and V (NAD+)** for growth, which perfectly matches the description.
- In unvaccinated children, *H. influenzae* type b (Hib) is a significant cause of **bacterial meningitis**, epiglottitis, and other invasive infections, especially considering the family's anti-vaccination stance.
*Group B Streptococcus*
- **Group B Streptococcus (GBS)** is a **gram-positive coccus** and a common cause of early-onset neonatal sepsis and meningitis, typically in infants less than 3 months old.
- It does not require chocolate agar or specific growth factors X and V, and is **gram-positive**, not gram-negative.
*Moraxella catarrhalis*
- *Moraxella catarrhalis* is a **gram-negative diplococcus** and a common cause of otitis media, sinusitis, and bronchitis, but it is a rare cause of meningitis.
- While it is a gram-negative organism, it does not typically require chocolate agar or specific growth factors X and V for isolation, usually growing on standard blood agar.
*Streptococcus pneumoniae*
- *Streptococcus pneumoniae* is a **gram-positive coccus** that is a leading cause of bacterial meningitis in children and adults.
- It is **gram-positive**, not gram-negative, and grows on blood agar, not specifically requiring chocolate agar or factors X and V.
*Listeria monocytogenes*
- *Listeria monocytogenes* is a **gram-positive rod** and a cause of meningitis in neonates, immunocompromised individuals, and the elderly.
- It is a **gram-positive rod**, contrary to the gram-negative, encapsulated organism described, and does not require chocolate agar or factors X and V for growth.
Pediatric respiratory infections US Medical PG Question 9: An 8-year-old boy presents to his pediatrician accompanied by his father with a complaint of chronic cough. For the past 2 months he has been coughing up yellow, foul-smelling sputum. He has been treated at a local urgent care center for multiple episodes of otitis media, sinusitis, and bronchitis since 2 years of age. His family history is unremarkable. At the pediatrician's office, his temperature is 99.2°F (37.3°C), blood pressure is 110/84 mmHg, pulse is 95/min, and respirations are 20/min. Inspection shows a young boy who coughs occasionally during examination. Pulmonary exam demonstrates diffuse wheezing and crackles bilaterally. Mild clubbing is present on the fingers. The father has brought an electrocardiogram (ECG) from the patient’s last urgent care visit that shows pronounced right axis deviation. Which of the following is the most likely etiology of this patient’s condition?
- A. Failure of neural crest cell migration
- B. Maldevelopment of pharyngeal pouches
- C. Transient bronchoconstriction
- D. Defective maturation of B-lymphocytes
- E. Decreased motility of cilia (Correct Answer)
Pediatric respiratory infections Explanation: ***Decreased motility of cilia***
- The recurrent respiratory infections (**otitis media, sinusitis, bronchitis**), chronic productive cough with **foul-smelling sputum**, and **bronchiectasis** (implied by chronic cough, wheezing, crackles) are highly suggestive of **primary ciliary dyskinesia (PCD)**.
- **Clubbing** and **right axis deviation** (suggesting right ventricular hypertrophy from pulmonary hypertension) are complications of chronic lung disease such as severe bronchiectasis, which is characteristic of PCD.
*Failure of neural crest cell migration*
- This is associated with conditions like **DiGeorge syndrome** or **Hirschsprung disease**, which present with different clinical features (e.g., cardiac defects, hypocalcemia, intestinal obstruction).
- It does not directly explain the recurrent respiratory tract infections and bronchiectasis seen in this patient.
*Maldevelopment of pharyngeal pouches*
- Similar to neural crest cell defects, issues with pharyngeal pouch development (e.g., **DiGeorge syndrome**) affect the immune system and cardiac structures.
- While it can lead to recurrent infections, it typically involves **T-cell deficiencies** and specific cardiac anomalies, rather than chronic suppurative respiratory disease and bronchiectasis as the primary presentation.
*Transient bronchoconstriction*
- This describes conditions like **asthma**, which causes reversible airway narrowing and wheezing.
- However, asthma does not explain the chronic **foul-smelling sputum**, **clubbing**, persistent recurrent infections like otitis media and sinusitis, or the development of bronchiectasis.
*Defective maturation of B-lymphocytes*
- This leads to **immunodeficiencies** primarily affecting **antibody production**, such as **X-linked agammaglobulinemia**.
- While patients would experience recurrent bacterial infections, the specific pattern of chronic sinusitis, otitis, and bronchiectasis with **foul-smelling sputum** (suggesting chronic bacterial colonization and impaired clearance) points more towards a structural or ciliary defect than a purely humoral immune deficiency.
Pediatric respiratory infections US Medical PG Question 10: A 10-year-old girl is admitted to the medical floor for a respiratory infection. The patient lives in a foster home and has been admitted many times. Since birth, the patient has had repeated episodes of pain/pressure over her frontal sinuses and a chronic cough that produces mucus. She was recently treated with amoxicillin for an infection. The patient is in the 25th percentile for height and weight which has been constant since birth. Her guardians state that the patient has normal bowel movements and has been gaining weight appropriately. The patient has a history of tricuspid stenosis. She also recently had magnetic resonance imaging (MRI) of her chest which demonstrated dilation of her airways. Her temperature is 99.5°F (37.5°C), blood pressure is 90/58 mmHg, pulse is 120/min, respirations are 18/min, and oxygen saturation is 94% on room air. Physical exam is notable for bruises along the patient's shins which the guardians state are from playing soccer. The rest of the exam is deferred because the patient starts crying. Which of the following findings is associated with this patient's most likely underlying diagnosis?
- A. Social withdrawal and avoidance of eye contact
- B. Hypocalcemia
- C. Repeat sinus infections secondary to seasonal allergies
- D. Diastolic murmur best heard along the right lower sternal border
- E. Increased chloride in the patient's sweat (Correct Answer)
Pediatric respiratory infections Explanation: ***Increased chloride in the patient's sweat***
- The patient's history of recurrent respiratory infections, chronic productive cough, frontal sinus pain, and **bronchiectasis** (dilated airways on MRI) are highly suggestive of **cystic fibrosis**.
- **Elevated sweat chloride** is the hallmark diagnostic test for cystic fibrosis, reflecting defective chloride transport in exocrine glands.
*Social withdrawal and avoidance of eye contact*
- These are features associated with **autism spectrum disorder**, which is unrelated to the patient's respiratory and sinus symptoms.
- While possible as a co-occurring condition, it is not directly linked to the most likely **underlying diagnosis** described.
*Hypocalcemia*
- **Hypocalcemia** is typically associated with conditions like **hypoparathyroidism** or severe **vitamin D deficiency**.
- It is not a characteristic feature or direct complication of cystic fibrosis.
*Repeat sinus infections secondary to seasonal allergies*
- While seasonal allergies can cause sinus issues, the patient's history of **chronic, productive cough**, and **bronchiectasis** points to a more severe underlying condition like cystic fibrosis, not just allergies.
- Cystic fibrosis patients often have chronic sinusitis due to thick, inspissated mucus, not primarily due to allergens.
*Diastolic murmur best heard along the right lower sternal border*
- A diastolic murmur at the right lower sternal border might suggest **aortic regurgitation** or a specific type of **pulmonary regurgitation**, but it is not characteristic of the patient's known tricuspid stenosis.
- The patient has **tricuspid stenosis**, which typically causes a mid-diastolic murmur best heard at the left lower sternal border, often increasing with inspiration. This finding is unrelated to cystic fibrosis.
More Pediatric respiratory infections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.