Emerging infectious diseases in children US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Emerging infectious diseases in children. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Emerging infectious diseases in children US Medical PG Question 1: A previously healthy 6-year-old boy is brought to the physician because of a 3-day history of progressive rash. The rash started on his face and now involves the entire body. For the past week, he has had a cough and a runny nose. He is visiting from the Philippines with his family. He is in first grade and spends his afternoons at an after-school child care program. Immunization records are not available. His temperature is 39.5°C (103°F), pulse is 115/min, and blood pressure is 105/66 mm Hg. Examination shows generalized lymphadenopathy. There is an erythematous maculopapular, blanching, and partially confluent exanthem on his entire body. The remainder of the examination shows no abnormalities. Which of the following is most likely to confirm the diagnosis?
- A. Monospot test
- B. Measles-specific IgM antibodies (Correct Answer)
- C. Tzanck smear
- D. Rapid antigen detection testing
- E. Rapid plasma reagin
Emerging infectious diseases in children Explanation: ***Measles-specific IgM antibodies***
- The clinical presentation with **fever**, **cough**, **coryza** (runny nose), and a **maculopapular rash** spreading from the face downward in an unvaccinated child from an endemic area (Philippines) is classic for **measles (rubeola)**.
- The **3 C's** (cough, coryza, conjunctivitis) along with high fever precede the rash by 2-4 days. **Koplik spots** (white spots on buccal mucosa) may appear before the rash but are often transient.
- Detecting **measles-specific IgM antibodies** in serum is the **gold standard** for confirming acute measles infection, with IgM appearing within days of rash onset and persisting for weeks.
- Generalized lymphadenopathy is also consistent with measles.
*Monospot test*
- The Monospot test detects **heterophile antibodies** associated with **infectious mononucleosis** caused by **Epstein-Barr virus (EBV)**.
- EBV typically presents with **fatigue**, **pharyngitis**, **posterior cervical lymphadenopathy**, and **splenomegaly**; the rash (if present) usually occurs after ampicillin administration.
- The cephalocaudal spread of rash and prominent **respiratory prodrome** are more characteristic of measles.
*Tzanck smear*
- A Tzanck smear identifies **multinucleated giant cells** characteristic of **herpes simplex virus (HSV)** or **varicella-zoster virus (VZV)** infections.
- These conditions present with **vesicular or blistering lesions**, not the **maculopapular, blanching rash** described in this patient.
- Varicella (chickenpox) has a vesicular rash in different stages, not confluent maculopapular lesions.
*Rapid antigen detection testing*
- Rapid antigen tests are typically used for diagnosing **streptococcal pharyngitis** or **influenza**.
- While respiratory symptoms are present, the **prominent maculopapular exanthem** with cephalocaudal spread and **generalized lymphadenopathy** are not consistent with these diagnoses.
- Measles rapid antigen tests exist but are not standard first-line confirmatory tests; **serology (IgM)** is preferred.
*Rapid plasma reagin*
- Rapid Plasma Reagin (RPR) is a non-treponemal test used to screen for **syphilis**.
- Congenital syphilis can present with rash, but this patient's **age (6 years)**, **acute febrile illness with respiratory prodrome**, and **classic rash progression** make measles far more likely.
- Secondary syphilis (which causes rash) requires sexual transmission, making it highly unlikely in a 6-year-old child.
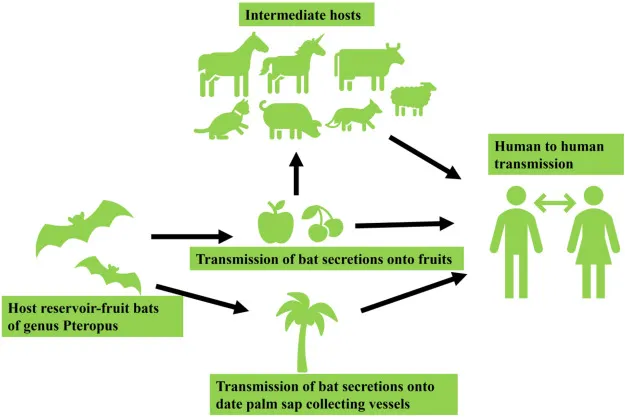
Emerging infectious diseases in children US Medical PG Question 2: A 45-year-old woman presents to the emergency department with a headache, fevers with chills, rigors, and generalized joint pain for the past week. She also complains of a progressive rash on her left arm. She says that a few days ago she noticed a small, slightly raised lesion resembling an insect bite mark, which had a burning sensation. The medical and surgical histories are unremarkable. She recalls walking in the woods 2 weeks prior to the onset of symptoms, but does not recall finding a tick on her body. On examination, the temperature is 40.2°C (104.4°F). A circular red rash measuring 10 cm x 5 cm in diameter is noted on the left arm, as shown in the accompanying image. The remainder of her physical examination is unremarkable. The tick causing her disease is also responsible for the transmission of which of the following pathogens?
- A. Rickettsia rickettsii
- B. Babesia microti (Correct Answer)
- C. Rickettsia typhi
- D. Ehrlichia
- E. Plasmodium vivax
Emerging infectious diseases in children Explanation: ***Babesia microti***
- The clinical picture of **headache**, **fever with chills**, **rigors**, **generalized joint pain**, and an **expanding erythematous rash (erythema migrans)** after a woodland exposure points to **Lyme disease**, caused by *Borrelia burgdorferi*.
- **Both *Borrelia burgdorferi*** and ***Babesia microti*** are transmitted by the **deer tick** (*Ixodes scapularis*), making co-infection common in endemic areas.
*Rickettsia rickettsii*
- This pathogen causes **Rocky Mountain spotted fever**, which typically presents with a **maculopapular rash** that often becomes petechial and involves the palms and soles.
- The rash in this vignette is an **expanding erythematous lesion (erythema migrans)**, characteristic of Lyme disease, not RMSF.
*Rickettsia typhi*
- This bacterium causes **endemic (murine) typhus**, typically transmitted by the **infected flea** (*Xenopsylla cheopis*).
- Symptoms include fever, headache, and a **truncal maculopapular rash**, but it is not associated with a tick bite or erythema migrans.
*Ehrlichia*
- *Ehrlichia chaffeensis* causes **human monocytic ehrlichiosis**, transmitted by the **lone star tick** (*Amblyomma americanum*).
- While it can cause fever, headache, and myalgia, it does not typically present with the classic **erythema migrans rash** seen in Lyme disease.
*Plasmodium vivax*
- This protozoan causes **malaria**, transmitted by the **Anopheles mosquito**.
- Symptoms include cyclical fevers, chills, and headache but do not involve a tick bite or the characteristic **erythema migrans rash**.
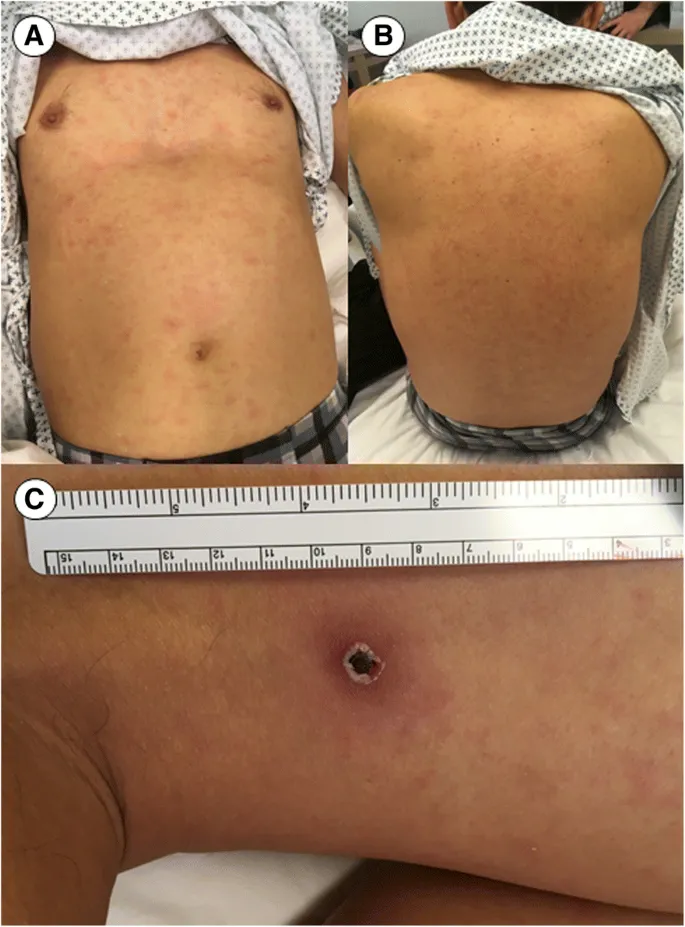
Emerging infectious diseases in children US Medical PG Question 3: A 4-year-old boy is brought to the clinic by his mother with fever and a rash. The patient’s mother says his symptoms started 1 week ago with the acute onset of fever and a runny nose, which resolved over the next 3 days. Then, 4 days later, she noted a rash on his face, which, after a day, spread to his neck, torso, and extremities. The patient denies any pruritus or pain associated with the rash. No recent history of sore throat, chills, or upper respiratory infection. The patient has no significant past medical history and takes no medications. The vital signs include: temperature 37.2°C (99.9°F) and pulse 88/min. On physical examination, there is a maculopapular rash on his face, torso, and extremities, which spares the palms and soles. The appearance of the rash is shown in the exhibit (see image below). Which of the following would most likely confirm the diagnosis in this patient?
- A. Assay for IgM and IgG against measles virus
- B. Serology for human herpesvirus-6 IgM antibodies
- C. Throat culture
- D. ELISA for parvovirus B-19 IgM and IgG antibodies (Correct Answer)
- E. ELISA for IgM antibodies against Rubella virus
Emerging infectious diseases in children Explanation: ***ELISA for parvovirus B-19 IgM and IgG antibodies***
- The presentation of a child with a prodrome of fever and runny nose followed a few days later by a **maculopapular rash** that started on the face and spread to the torso and extremities, sparing the palms and soles, is highly suggestive of **Erythema Infectiosum** (Fifth Disease) caused by **Parvovirus B19**.
- An **ELISA for parvovirus B-19 IgM antibodies**, indicating a recent infection, would confirm the diagnosis, with IgG antibodies suggesting past exposure and immunity.
*Assay for IgM and IgG against measles virus*
- Measles (Rubeola) typically presents with a prodrome of **cough, coryza, conjunctivitis, and Koplik spots** before the rash appears, which are not described in this patient.
- The rash of measles is usually **more confluent** and starts behind the ears, spreading downwards, and is often accompanied by a higher fever.
*Serology for human herpesvirus-6 IgM antibodies*
- Human herpesvirus-6 (HHV-6) causes **Roseola Infantum** (Sixth Disease), which is characterized by a **high fever** for 3-5 days that resolves abruptly, followed by the appearance of a **rose-colored maculopapular rash** on the trunk that spreads to the extremities.
- Though there is a rash after fever, the rash in this patient started on the face and the fever was mild, which is atypical for Roseola.
*ELISA for IgG antibodies against Rubella virus*
- A positive IgM antibody test would suggest an acute infection with Rubella (German Measles), which presents with a rash that often starts on the face and spreads downwards, similar to this case.
- However, Rubella is typically associated with **posterior auricular and suboccipital lymphadenopathy**, which is not mentioned in the patient's history or physical exam.
*Throat culture*
- A throat culture is primarily used to diagnose **bacterial infections** like Streptococcus pyogenes (strep throat), which can cause a rash such as scarlet fever.
- The rash of scarlet fever characteristically feels like sandpaper and is associated with a "strawberry tongue" and perioral pallor, which are not seen here.
Emerging infectious diseases in children US Medical PG Question 4: A 3-year-old boy presents with his mother to the family medicine clinic for an itchy rash on the face that started 3 days ago. The mother states that her son had a fever with a runny nose a little more than a week ago. There has been no sore throat or cough according to the mother. No significant medical conditions are noted. No medications are on record. The boy is up-to-date on all immunizations. His heart rate is 102/min, respiratory rate is 24/min, temperature is 36.5°C (97.7°F), and blood pressure is 92/65 mm Hg. The boy appears well-nourished and alert. Auscultation of the heart is without murmurs. Lungs are clear to auscultation bilaterally. An erythematous malar rash extending from the left lateral nasal region to the left medial zygomatic region is present. There is no lymphadenopathy present. A full skin examination reveals an erythematous, reticulated rash on the lower extremities (see image). Which of the following etiologic agents is responsible for the patient's signs and symptoms?
- A. Parvovirus B19 (Correct Answer)
- B. Adenovirus
- C. Streptococcus pyogenes
- D. Rubella virus
- E. Human herpesvirus 6 (HHV-6)
Emerging infectious diseases in children Explanation: ***Parvovirus B19***
- The presentation of a **malar rash** ("slapped cheek" appearance) followed by a **reticulated rash** on the extremities after a prodromal febrile illness is classic for **erythema infectiosum**, also known as fifth disease, caused by Parvovirus B19.
- The rash typically starts on the face and spreads to the body, often with a lacy or reticulated pattern, and the child is generally well-appearing.
*Adenovirus*
- Adenovirus can cause a variety of symptoms including **respiratory illness**, **conjunctivitis**, and sometimes a rash, but it typically does not present with the characteristic "slapped cheek" and reticulated rash described.
- The fever and runny nose are common initial symptoms but are not specific enough to point towards adenovirus without other differentiating features like conjunctivitis or pharyngitis.
*Streptococcus pyogenes*
- *Streptococcus pyogenes* causes conditions like **scarlet fever**, which presents with a rash (scarlatiniform rash) often described as sandpaper-like, and a **sore throat**, which is explicitly stated as absent in this case.
- The rash of scarlet fever usually affects the trunk and extremities but typically spares the face, differentiating it from the described facial rash.
*Rubella virus*
- **Rubella (German measles)** typically presents with a fine, pink, macular rash that starts on the face and spreads downwards, often with associated **postauricular and occipital lymphadenopathy**, which is absent in this patient.
- While there is a febrile prodrome, the characteristic "slapped cheek" followed by a reticulated rash is not typical of rubella.
*Human herpesvirus 6 (HHV-6)*
- HHV-6 causes **roseola infantum (exanthem subitum)**, characterized by a **high fever** that resolves abruptly followed by the appearance of a **rose-pink maculopapular rash** on the trunk and neck, sparing the face.
- The rash pattern and the initial symptoms (high fever followed by rash after fever breaks) are distinct from the patient's presentation.
Emerging infectious diseases in children US Medical PG Question 5: A 45-year-old male presents to the emergency room complaining of severe nausea and vomiting. He returned from a business trip to Nigeria five days ago. Since then, he has developed progressively worsening fevers, headache, nausea, and vomiting. He has lost his appetite and cannot hold down food or water. He did not receive any vaccinations before traveling. His medical history is notable for alcohol abuse and peptic ulcer disease for which he takes omeprazole regularly. His temperature is 103.0°F (39.4°C), blood pressure is 100/70 mmHg, pulse is 128/min, and respirations are 22/min. Physical examination reveals scleral icterus, hepatomegaly, and tenderness to palpation in the right and left upper quadrants. While in the examination room, he vomits up dark vomitus. The patient is admitted and started on multiple anti-protozoal and anti-bacterial medications. Serology studies are pending; however, the patient dies soon after admission. The virus that likely gave rise to this patient’s condition is part of which of the following families?
- A. Togavirus
- B. Flavivirus (Correct Answer)
- C. Calicivirus
- D. Hepevirus
- E. Bunyavirus
Emerging infectious diseases in children Explanation: ***Flavivirus***
- The clinical presentation, including acute onset of **high fever**, headache, nausea, vomiting (**dark vomitus**), **scleral icterus**, and **hepatomegaly** following travel to Nigeria, is highly suggestive of **yellow fever**.
- Yellow fever is caused by the **yellow fever virus**, which is a **flavivirus** transmitted by mosquitoes, primarily *Aedes aegypti*.
*Togavirus*
- The Togavirus family includes viruses like **rubella virus** and **alphaviruses** (e.g., Eastern equine encephalitis virus).
- While some alphaviruses can cause fever and encephalitis, they typically do not present with the characteristic **hemorrhagic fever** and severe liver involvement seen in this case.
*Calicivirus*
- The Calicivirus family includes **Norovirus**, which is a common cause of **gastroenteritis** with vomiting and diarrhea.
- Norovirus infections are typically self-limiting and do not usually lead to the severe systemic symptoms, **jaundice**, or fatal outcome described here.
*Hepevirus*
- The Hepevirus family includes the **hepatitis E virus (HEV)**.
- HEV causes **acute viral hepatitis**, characterized by jaundice, nausea, and vomiting, but it rarely progresses to the rapid, severe, and fatal hemorrhagic form seen in this patient.
*Bunyavirus*
- The Bunyavirus family (now split into several families) includes viruses like Hantavirus and Rift Valley fever virus, which can cause **hemorrhagic fevers**.
- While some bunyaviruses are found in Africa, the specific constellation of symptoms, particularly the prominent **scleral icterus** and rapid progression to severe liver failure and death, is most consistent with **yellow fever**, a flavivirus.
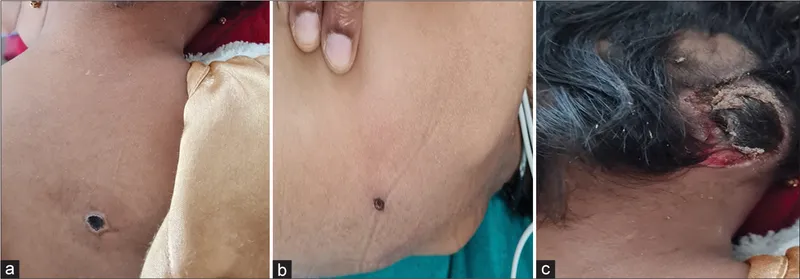
Emerging infectious diseases in children US Medical PG Question 6: A 7-year-old boy is brought to his pediatrician by his parents because of a new rash. The family immigrated from Laos one year ago and recently obtained health insurance. A week ago, the boy stated that he was “not feeling well” and asked to stay home from school. At the time, he starting having cough, nasal congestion, and irritated eyes – symptoms that persisted and intensified. His parents recall that at the time they noticed small whitish-blue papules over the red buccal mucosa opposite his molars. Five days ago, his parents noticed a red rash around his face that quickly spread downward to cover most of his arms, trunk, and then legs. His temperature is 102.5°F (39.2°C), blood pressure is 110/85 mmHg, pulse is 102/min, and respirations 25/min. On physical exam, he has intermittent cough, cervical lymphadenopathy, and nonpurulent conjunctivitis accompanied by a confluent, dark red rash over his body. This patient is at risk for which of the following complications later in life?
- A. CNS degeneration (Correct Answer)
- B. Nonreactive pupils
- C. Monoarticular arthritis
- D. Valvular heart disease
- E. B cell neoplasm
Emerging infectious diseases in children Explanation: ***CNS degeneration***
- The patient's symptoms are highly suggestive of **measles (rubeola)**, characterized by **Koplik spots**, **coryza**, **conjunctivitis**, and a **descending maculopapular rash**.
- A rare but devastating late complication of measles is **subacute sclerosing panencephalitis (SSPE)**, a progressive **CNS degenerative disease** that occurs years after the initial infection.
*Nonreactive pupils*
- **Nonreactive pupils**, or Argyll Robertson pupils, are a classic sign of **neurosyphilis** and are not associated with measles infection.
- This symptom points to damage to specific pathways in the brain affecting pupillary reflexes.
*Monoarticular arthritis*
- **Monoarticular arthritis** is typically seen in conditions like **juvenile idiopathic arthritis**, **septic arthritis**, or **Lyme disease**, not as a direct complication of measles.
- While arthritis can occur in measles, it is usually polyarticular and transient, not a chronic monoarticular condition.
*Valvular heart disease*
- **Valvular heart disease**, particularly **rheumatic heart disease**, is a long-term complication of **streptococcal infections (rheumatic fever)** and is not associated with measles.
- **Kawasaki disease** can also cause coronary artery aneurysms, but the clinical presentation here is classic for measles.
*B cell neoplasm*
- **B-cell neoplasms** (e.g., lymphomas, leukemias) are not directly linked to measles infection.
- While measles can cause temporary immunosuppression, it does not typically lead to long-term hematological malignancies.
Emerging infectious diseases in children US Medical PG Question 7: A 24-year-old man presents to the emergency department with sudden onset of fever for the past few hours as well as pain and swelling in his right knee and left ankle. He denies any recent history of trauma or injury. The patient is otherwise a healthy, active young man. He recently recovered from a case of gastroenteritis which caused significant abdominal pain and bloody stool 4 weeks ago. He believes the infection was related to eating undercooked chicken while camping. His blood pressure is 124/76 mm Hg, his heart rate is 76/min, and his temperature is 36.9 ℃ (98.4 ℉). Physical examination reveals tenderness to palpation of his right knee and left ankle as well as erythematous conjunctiva. Which of the following features would be least likely to develop in patients with this condition?
- A. Circinate balanitis
- B. Genital ulcers
- C. DIP joint swelling (Correct Answer)
- D. Urethritis
- E. Skin rash
Emerging infectious diseases in children Explanation: ***DIP joint swelling***
- **Reactive arthritis** typically involves the **large joints** of the lower extremities in an asymmetric pattern, such as the knees and ankles, but spares the **distal interphalangeal (DIP) joints**.
- The patient's history of recent gastroenteritis, subsequent arthritis, and conjunctivitis are classic features of reactive arthritis (formerly Reiter's syndrome), which is a form of **seronegative spondyloarthropathy**.
*Circinate balanitis*
- **Circinate balanitis** is a painless, shallow ulceration of the glans penis that is a characteristic **mucocutaneous manifestation** of reactive arthritis.
- This condition occurs in a significant number of male patients with **HLA-B27 positive** reactive arthritis.
*Genital ulcers*
- **Genital ulcers** are possible cutaneous manifestations of reactive arthritis.
- These can present along with other skin findings such as **keratoderma blennorrhagicum** (pustular psoriasis-like lesions) and circinate balanitis.
*Urethritis*
- **Urethritis** is a common component of the classic triad of symptoms in reactive arthritis ("can't pee, can't see, can't climb a tree").
- It manifests as **dysuria, urinary frequency**, or penile discharge, often following a gastrointestinal or genitourinary infection.
*Skin rash*
- A skin rash, particularly **keratoderma blennorrhagicum**, which resembles pustular psoriasis, is a known *cutaneous manifestation* of reactive arthritis.
- Lesions typically appear on the **palms and soles**, but can also affect the trunk and scalp.
Emerging infectious diseases in children US Medical PG Question 8: A 15-year-old Caucasian male is brought to his pediatrician by his parents, who note the development of a tremor in their child. Urine and serum analysis reveal elevated levels of copper. Which of the following clinical manifestations would the physician most expect to see in this patient?
- A. Kaiser-Fleischer rings (Correct Answer)
- B. Diabetes mellitus
- C. Hepatocytes that stain with Prussian blue
- D. Panacinar emphysema
- E. Increased serum ceruloplasmin
Emerging infectious diseases in children Explanation: ***Kaiser-Fleischer rings***
- Elevated copper levels, tremor, and young age are classic signs of **Wilson's disease**, an autosomal recessive disorder leading to copper accumulation.
- **Kaiser-Fleischer rings** are greenish-brown deposits of copper in the cornea, a hallmark ocular manifestation of Wilson's disease.
*Diabetes mellitus*
- While copper dysregulation can affect various organs, **diabetes mellitus** is not a typical clinical manifestation of Wilson's disease.
- Pancreatic involvement leading to diabetes is more commonly associated with conditions like **hemochromatosis** (iron overload) or chronic pancreatitis.
*Hepatocytes that stain with Prussian blue*
- **Prussian blue stain** is used to detect **iron deposits**, not copper.
- In Wilson's disease, copper accumulates in hepatocytes, which would not stain positive with Prussian blue.
*Panacinar emphysema*
- **Panacinar emphysema** is primarily associated with **alpha-1 antitrypsin deficiency**, a genetic disorder affecting elastic tissue in the lungs.
- It has no direct association with copper metabolism or Wilson's disease.
*Increased serum ceruloplasmin*
- **Ceruloplasmin** is a copper-carrying protein, and in Wilson's disease, the **serum ceruloplasmin level is typically reduced**, not increased.
- This reduction is due to impaired copper incorporation into ceruloplasmin by the dysfunctional ATP7B protein.
Emerging infectious diseases in children US Medical PG Question 9: A 72-year-old man is brought to your office by his daughter due to concern over recent behavioral changes. Over the last several months he has had increasing difficulty with remembering recent events. She mentions that he is embarrassed due to a new inability to control urination. His medical history is significant for hypertension and insomnia. His medications include alprazolam and hydrochlorothiazide. On physical exam, he is oriented to time and place and thinks his daughter is exaggerating; however, when asked to recall 3 items, the patient refuses to continue the mental status exam. He has 5/5 strength bilaterally. He walks in short strides by sliding his feet across the floor. Which of the following would you expect to see in this patient?
- A. Depigmentation of the substantia nigra pars compacta
- B. Convex hemorrhage that does not cross suture lines
- C. Atrophy of the caudate and putamen
- D. Distortion of corona radiata fibers (Correct Answer)
- E. Atrophy of the subthalamic nucleus
Emerging infectious diseases in children Explanation: ***Distortion of corona radiata fibers***
- The patient's symptoms of **memory decline**, **urinary incontinence**, and **gait disturbance** (magnetic gait) form the classic triad of **normal pressure hydrocephalus (NPH)**.
- In NPH, the enlarged ventricles cause **stretching and distortion of the periventricular white matter tracts**, including the ascending and descending fibers of the **corona radiata**, which leads to the characteristic neurological symptoms.
*Depigmentation of the substantia nigra pars compacta*
- This is a hallmark pathological finding in **Parkinson's disease**, characterized by the loss of **dopaminergic neurons** in the substantia nigra.
- While gait disturbance (shuffling gait) can occur in Parkinson's, the presenting symptoms of **urinary incontinence** and prominent memory decline are not typical primary features, and the gait description is more suggestive of NPH.
*Convex hemorrhage that does not cross suture lines*
- This describes an **epidural hematoma**, typically resulting from **head trauma** and often associated with rupture of the **middle meningeal artery**.
- The clinical presentation is usually acute with signs of increased intracranial pressure, rather than the chronic, progressive symptoms described in the patient.
*Atrophy of the caudate and putamen*
- This is a characteristic finding in **Huntington's disease**, a neurodegenerative disorder.
- Huntington's typically presents with **chorea** (involuntary movements), psychiatric disturbances, and cognitive decline, which do not align with the patient's primary symptoms of gait disturbance and incontinence.
*Atrophy of the subthalamic nucleus*
- Atrophy of the subthalamic nucleus is not a distinct primary disorder associated with the patient's constellation of symptoms.
- The subthalamic nucleus plays a role in motor control, and damage to it can cause **hemiballismus**, which is not described here.
Emerging infectious diseases in children US Medical PG Question 10: A 62-year-old woman comes to the physician because of worsening mental status over the past month. Her husband reports that she was initially experiencing lapses in memory but has recently started having difficulties performing activities of daily living. She appears withdrawn and avoids eye contact. Examination shows diffuse involuntary muscle jerking that can be provoked by loud noises. A cerebrospinal fluid analysis shows elevated concentration of 14-3-3 protein. Four months later, the patient dies. Pathologic examination of the brain on autopsy is most likely to show which of the following findings?
- A. Degeneration of the substantia nigra pars compacta
- B. Spongiform vacuolation of the cortex (Correct Answer)
- C. Focal inflammatory demyelination and gliosis
- D. Deposits of amyloid beta peptides
- E. Marked atrophy of caudate and putamen
Emerging infectious diseases in children Explanation: ***Spongiform vacuolation of the cortex***
- The constellation of **rapidly progressive dementia**, **myoclonus** (involuntary muscle jerking provoked by loud noises), and **elevated 14-3-3 protein in CSF** is highly indicative of **Creutzfeldt-Jakob disease (CJD)**.
- CJD is a **prion disease** characterized pathologically by **spongiform changes** (vacuolation) in the gray matter of the cerebral cortex, cerebellum, and deep nuclei, as well as neuronal loss and astrogliosis.
*Degeneration of the substantia nigra pars compacta*
- This finding is characteristic of **Parkinson's disease**, which typically presents with a **slowly progressive movement disorder** (tremor, rigidity, bradykinesia) rather than rapid dementia and myoclonus.
- While Parkinson's can later involve cognitive decline, the rapid progression and specific neurological signs point away from it as the primary diagnosis.
*Focal inflammatory demyelination and gliosis*
- These findings are typical of **multiple sclerosis** or other **inflammatory demyelinating diseases**.
- While these can cause neurological symptoms, they rarely present with the aggressive, rapidly fatal course and myoclonus seen in this patient, and the CSF 14-3-3 protein is not a specific marker for them.
*Deposits of amyloid beta peptides*
- This is the hallmark pathological feature of **Alzheimer's disease**, which presents as a **gradual, progressive memory impairment** and cognitive decline, typically over many years, without the prominent myoclonus or rapid progression to death seen here.
- The presence of 14-3-3 protein in CSF is not characteristic of Alzheimer's disease.
*Marked atrophy of caudate and putamen*
- This is the classic pathological finding in **Huntington's disease**, which is an inherited neurodegenerative disorder characterized by **chorea**, psychiatric disturbances, and dementia.
- While Huntington's can cause dementia, its typical presentation is earlier onset, often with prominent chorea, and a slower progression than described, without the myoclonus or 14-3-3 CSF findings.
More Emerging infectious diseases in children US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.