Central nervous system infections US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Central nervous system infections. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Central nervous system infections US Medical PG Question 1: A 6-year-old boy and his parents present to the emergency department with high-grade fever, headache, and projectile vomiting. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all developmental milestones. Past medical history is noncontributory. He has had no sick contacts at school or at home. The family has not traveled out of the area recently. He likes school and playing videogames with his younger brother. Today, his blood pressure is 115/76 mm Hg, heart rate is 110/min, respiratory rate is 22/min, and temperature is 38.4°C (101.2°F). On physical exam, the child is disoriented. Kernig’s sign is positive. A head CT was performed followed by a lumbar puncture. Several aliquots of CSF were distributed throughout the lab. Cytology showed high counts of polymorphs, biochemistry showed low glucose and elevated protein levels, and a gram smear shows gram-positive lanceolate-shaped cocci alone and in pairs. A smear is prepared on blood agar in an aerobic environment and grows mucoid colonies with clearly defined edges and alpha hemolysis. On later evaluation they develop a ‘draughtsman’ appearance. Which one of the following is the most likely pathogen?
- A. Streptococcus pneumoniae (Correct Answer)
- B. Staphylococcus aureus
- C. Neisseria meningitidis
- D. Staphylococcus epidermidis
- E. Streptococcus agalactiae
Central nervous system infections Explanation: ***Streptococcus pneumoniae***
- The CSF findings of **high polymorphs**, **low glucose**, and **elevated protein** are classic for bacterial meningitis. The Gram stain showing **Gram-positive, lanceolate-shaped cocci in pairs** is highly characteristic of *Streptococcus pneumoniae*.
- The growth of **mucoid colonies** with **alpha hemolysis** on blood agar in an aerobic environment, which later develop a **'draughtsman' appearance**, are further confirmatory characteristics of *S. pneumoniae*.
*Staphylococcus aureus*
- *Staphylococcus aureus* is a Gram-positive coccus but typically presents in **clusters** on Gram stain, not lanceolate pairs.
- While it can cause meningitis, it usually exhibits **beta-hemolysis** and is catalase-positive, unlike *S. pneumoniae*.
*Neisseria meningitidis*
- *Neisseria meningitidis* is a **Gram-negative diplococcus**, which would appear distinctly different on Gram stain compared to the described Gram-positive lanceolate cocci.
- Although it is a common cause of bacterial meningitis, its colonial morphology and Gram stain characteristics do not match the case.
*Staphylococcus epidermidis*
- *Staphylococcus epidermidis* is a **Gram-positive coccus in clusters**, similar to *S. aureus*, and is commonly a **skin commensal** or found in infections related to indwelling devices.
- It typically exhibits **gamma-hemolysis** (non-hemolytic) and is usually **coagulase-negative**, differentiating it from the alpha-hemolytic, 'draughtsman' appearing colonies described.
*Streptococcus agalactiae*
- *Streptococcus agalactiae* (**Group B Streptococcus**) is a Gram-positive coccus that typically grows in **chains** and causes **beta-hemolysis**, particularly in neonates.
- While it can cause meningitis, its characteristic hemolytic pattern and arrangement on Gram stain differ from the alpha-hemolytic, lanceolate-shaped cocci in pairs described.
Central nervous system infections US Medical PG Question 2: A 7-year-old boy is brought to the emergency department because of high-grade fever and lethargy for 4 days. He has had a severe headache for 3 days and 2 episodes of non-bilious vomiting. He has sickle cell disease. His only medication is hydroxyurea. His mother has refused vaccinations and antibiotics in the past because of their possible side effects. He appears ill. His temperature is 40.1°C (104.2°F), pulse is 131/min, and blood pressure is 92/50 mm Hg. Examination shows nuchal rigidity. Kernig and Brudzinski signs are present. A lumbar puncture is performed. Analysis of the cerebrospinal fluid (CSF) shows a decreased glucose concentration, increased protein concentration, and numerous segmented neutrophils. A Gram stain of the CSF shows gram-negative coccobacilli. This patient is at greatest risk for which of the following complications?
- A. Adrenal insufficiency
- B. Cerebral palsy
- C. Hearing loss (Correct Answer)
- D. Communicating hydrocephalus
- E. Brain abscess
Central nervous system infections Explanation: ***Hearing loss***
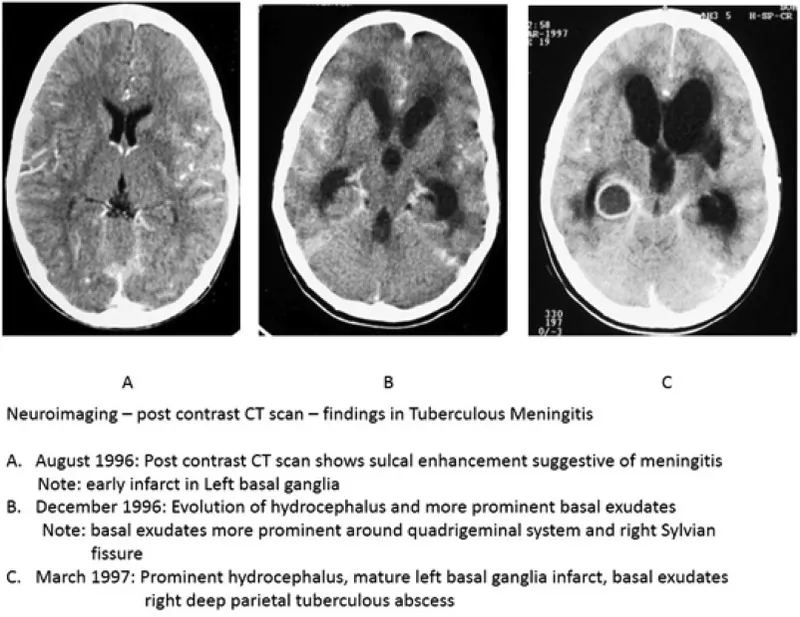
- The patient has bacterial meningitis, likely caused by *Haemophilus influenzae* type b given the **gram-negative coccobacilli** and his unvaccinated status.
- **Sensorineural hearing loss is the MOST COMMON long-term neurological sequela of bacterial meningitis**, occurring in 10-30% of survivors, making this the greatest risk for this patient.
- It results from inflammation of the **cochlea and eighth cranial nerve**, which can occur even with appropriate treatment.
- Children with *H. influenzae* meningitis are at particularly high risk for this complication.
*Adrenal insufficiency*
- While adrenal hemorrhage and crisis can occur with overwhelming sepsis (Waterhouse-Friderichsen syndrome), this is **classically associated with meningococcemia**, not *H. influenzae*.
- It is an acute complication of septic shock rather than a common sequela of meningitis itself.
*Cerebral palsy*
- Cerebral palsy requires significant hypoxic-ischemic injury or extensive brain damage during the acute illness.
- While possible with severe meningitis, it is a **much less common** complication compared to hearing loss.
*Communicating hydrocephalus*
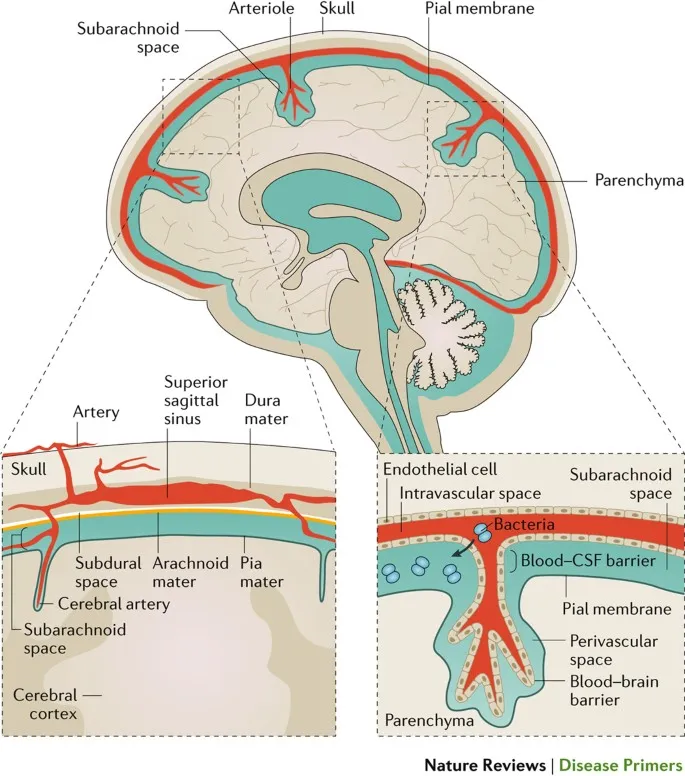
- Can occur due to impaired CSF reabsorption at the arachnoid granulations following meningeal inflammation.
- This is a recognized complication but occurs in **fewer than 5-10%** of cases, making it less common than hearing loss.
*Brain abscess*
- Brain abscess represents a focal parenchymal infection and is a **rare complication** of bacterial meningitis.
- It typically occurs when infection spreads from contiguous sites or when meningitis is inadequately treated.
Central nervous system infections US Medical PG Question 3: A 65-year-old patient presents with rapidly progressive dementia, myoclonus, and ataxia over 3 months. Laboratory studies, including serum vitamin B12 (cyanocobalamin), thyroxine (T4), and thyroid-stimulating hormone concentrations, are within normal limits. A lumbar puncture is performed. Cerebrospinal fluid (CSF) analysis is most likely to show which of the following?
- A. Increased 14-3-3 protein concentration (Correct Answer)
- B. Antiganglioside GM1 antibodies
- C. Anti-glutamic acid decarboxylase antibodies
- D. Increased α-synuclein protein concentration
- E. Oligoclonal bands
Central nervous system infections Explanation: ***Increased 14-3-3 protein concentration***
- The constellation of **rapidly progressive dementia**, **myoclonus**, and **ataxia** over 3 months with normal routine labs is highly suggestive of **Creutzfeldt-Jakob disease (CJD)**.
- An **elevated 14-3-3 protein concentration** in the CSF is a **classic diagnostic marker** for CJD, reflecting rapid neuronal destruction and included in the **WHO diagnostic criteria**.
- This is the most characteristic CSF finding in CJD, with high sensitivity and specificity.
*Oligoclonal bands*
- **Oligoclonal bands** are indicative of intrathecal antibody production and are characteristic of **inflammatory or demyelinating conditions** such as **multiple sclerosis** and **CNS infections**.
- They are **NOT typically found in prion diseases** like CJD, which involve protein misfolding rather than immune-mediated inflammation.
*Increased α-synuclein protein concentration*
- **Alpha-synuclein accumulation** is characteristic of **synucleinopathies** such as Parkinson's disease, Lewy body dementia, and multiple system atrophy.
- While these can involve dementia and motor symptoms, they typically have a **slower progression** and different symptom profile than the rapid course seen in CJD.
*Antiganglioside GM1 antibodies*
- **Anti-ganglioside GM1 antibodies** are primarily associated with autoimmune **motor neuropathies**, particularly **multifocal motor neuropathy** and some forms of Guillain-Barré syndrome.
- They are not typically associated with rapidly progressive dementia or CJD.
*Anti-glutamic acid decarboxylase antibodies*
- **Anti-glutamic acid decarboxylase (GAD) antibodies** are primarily associated with **stiff-person syndrome** and certain types of **autoimmune encephalitis**.
- While these conditions can present with neurological symptoms, the clinical picture of rapidly progressive dementia with myoclonus and ataxia is not typical for GAD antibody-mediated disorders.
Central nervous system infections US Medical PG Question 4: A 3-day-old boy is brought to the physician by his mother because of irritability and feeding intolerance for 1 day. His temperature is 39.2°C (102.6°F). Physical examination shows a bulging anterior fontanelle. A photomicrograph of a Gram stain of the cerebrospinal fluid is shown. Further evaluation shows that the organism expresses the K1 capsular polysaccharide. Which of the following is the most likely causal pathogen?
- A. Streptococcus agalactiae
- B. Salmonella typhi
- C. Listeria monocytogenes
- D. Pseudomonas aeruginosa
- E. Escherichia coli (Correct Answer)
Central nervous system infections Explanation: ***Escherichia coli***
- The combination of **bacterial meningitis** in a neonate (3-day-old irritable and feeding-intolerant boy with fever and bulging fontanelle) and the presence of **K1 capsular polysaccharide** on the gram-negative rod in cerebrospinal fluid (CSF) strongly indicates *E. coli*.
- **K1 capsular polysaccharide** is a major virulence factor for *E. coli* strains causing neonatal meningitis, allowing them to invade the central nervous system.
*Streptococcus agalactiae*
- This is a common cause of **early-onset neonatal sepsis and meningitis**, but it is a **Gram-positive coccus** and expresses **Group B Streptococcus (GBS) antigens**, not K1 capsular polysaccharide.
- The Gram stain would show chains of cocci, which contradicts the description of the photomicrograph (implying Gram-negative rods).
*Salmonella typhi*
- While *S. typhi* is a **Gram-negative rod**, it typically causes **typhoid fever** with systemic symptoms and is an uncommon cause of neonatal meningitis.
- It does not express the **K1 capsular polysaccharide** associated with neonatal *E. coli* meningitis.
*Listeria monocytogenes*
- This is a significant cause of **neonatal meningitis**, but it is a **Gram-positive rod** that can mimic Gram-negative rods on initial Gram stain interpretation but is not characterized by K1 capsular polysaccharide.
- *Listeria* infections are often acquired transplacentally or during delivery and show characteristic tumbling motility.
*Pseudomonas aeruginosa*
- *P. aeruginosa* is a **Gram-negative rod** but is a rare cause of **neonatal meningitis**, typically seen in preterm infants or those with indwelling catheters or compromised immune systems.
- It does not express the K1 capsular polysaccharide and is more commonly associated with nosocomial infections.
Central nervous system infections US Medical PG Question 5: A 6-month old child is brought to the ER by parents for one day of fever, decreased feeding, and lethargy. They report that neither she nor her siblings are immunized due to their concerns about vaccinations. On exam, the infant is toxic-appearing. Antibiotics are started and lumbar puncture reveals bacterial meningitis caused by a gram-negative, encapsulated organism that requires chocolate agar and the two factors shown in Image A for growth. Which organism does this best describe?
- A. Group B Streptococcus
- B. Haemophilus influenzae (Correct Answer)
- C. Moraxella catarrhalis
- D. Streptococcus pneumoniae
- E. Listeria monocytogenes
Central nervous system infections Explanation: **Haemophilus influenzae**
- This organism is a **gram-negative, encapsulated coccobacillus** that requires **chocolate agar** and **factors X (hemin) and V (NAD+)** for growth, which perfectly matches the description.
- In unvaccinated children, *H. influenzae* type b (Hib) is a significant cause of **bacterial meningitis**, epiglottitis, and other invasive infections, especially considering the family's anti-vaccination stance.
*Group B Streptococcus*
- **Group B Streptococcus (GBS)** is a **gram-positive coccus** and a common cause of early-onset neonatal sepsis and meningitis, typically in infants less than 3 months old.
- It does not require chocolate agar or specific growth factors X and V, and is **gram-positive**, not gram-negative.
*Moraxella catarrhalis*
- *Moraxella catarrhalis* is a **gram-negative diplococcus** and a common cause of otitis media, sinusitis, and bronchitis, but it is a rare cause of meningitis.
- While it is a gram-negative organism, it does not typically require chocolate agar or specific growth factors X and V for isolation, usually growing on standard blood agar.
*Streptococcus pneumoniae*
- *Streptococcus pneumoniae* is a **gram-positive coccus** that is a leading cause of bacterial meningitis in children and adults.
- It is **gram-positive**, not gram-negative, and grows on blood agar, not specifically requiring chocolate agar or factors X and V.
*Listeria monocytogenes*
- *Listeria monocytogenes* is a **gram-positive rod** and a cause of meningitis in neonates, immunocompromised individuals, and the elderly.
- It is a **gram-positive rod**, contrary to the gram-negative, encapsulated organism described, and does not require chocolate agar or factors X and V for growth.
Central nervous system infections US Medical PG Question 6: A 9-year-old girl is admitted to the hospital with a one-day history of acute abdominal pain and vomiting. She also has a two-day history of fever, headache, and neck pain. Her immunizations are up-to-date. She is confused and oriented only to place and person. Her temperature is 39.7°C (103.5°F), pulse is 148/min, blood pressure is 90/50 mm Hg, and respiratory rate is 28/min. Cervical range of motion is limited by pain. The remainder of the neurologic examination shows no abnormalities. Laboratory studies show:
Hemoglobin 10.9 g/dL
Leukocyte count 44,000/mm3
Serum
pH 7.33
Na+ 130 mEq/L
Cl- 108 mEq/L
K+ 6.1 mEq/L
HCO3- 20 mEq/L
Urea nitrogen 34 mg/dL
Glucose 180 mg/dL
Creatinine 2.4 mg/dL
Urine ketones negative
A CT scan of the head shows enhancement of the arachnoid and pia mater. Cerebrospinal fluid analysis shows a leukocyte count of 3,400/μL (90% neutrophils), a glucose concentration of 50 mg/dL, protein concentration of 81 mg/dL, and no erythrocytes. Gram stain of the CSF shows gram-negative diplococci. This patient is at increased risk for which of the following complications?
- A. Vesicular skin eruptions
- B. Adrenal hemorrhage (Correct Answer)
- C. Pancreatitis
- D. Temporal lobe inflammation
- E. Deep neck abscess
Central nervous system infections Explanation: **Adrenal hemorrhage**
- The clinical picture of **fever, acute abdominal pain, confusion, hypotension, and a high WBC count (44,000/mm³)**, along with **Gram-negative diplococci in CSF**, indicates **meningococcal meningitis with sepsis**. This rapidly progressive infection by *Neisseria meningitidis* can lead to **Waterhouse-Friderichsen syndrome**, characterized by **adrenal hemorrhage** and profound shock.
- The **elevated potassium (6.1 mEq/L)** and **hyponatremia (130 mEq/L)** are consistent with **adrenal insufficiency** resulting from adrenal hemorrhage.
*Vesicular skin eruptions*
- **Vesicular skin eruptions** are characteristic of viral infections such as **herpes simplex virus (HSV)** or **varicella-zoster virus**, which would present differently (e.g., HSV encephalitis often causes temporal lobe involvement).
- While various infections can cause skin rashes, this specific presentation with extensive meningeal inflammation and septic shock points away from typical vesicular eruptions.
*Pancreatitis*
- **Pancreatitis** is characterized by severe epigastric pain radiating to the back, often with nausea and vomiting, and elevated lipase/amylase. While **abdominal pain** is present, other symptoms like **neck stiffness, confusion, and CSF findings of bacterial meningitis** are not typical for pancreatitis.
- There is no specific evidence, such as imaging findings or elevated pancreatic enzymes, to suggest pancreatitis in this case.
*Temporal lobe inflammation*
- **Temporal lobe inflammation** is a hallmark of **HSV encephalitis**, which often presents with seizures, bizarre behavior, and specific MRI findings in the temporal lobes. While a CT scan showed arachnoid and pia mater enhancement, this indicates **meningeal inflammation**, not specifically temporal lobe parenchymal inflammation (encephalitis).
- The presence of **Gram-negative diplococci in the CSF** strongly indicates bacterial meningitis, not viral encephalitis, making temporal lobe inflammation less likely.
*Deep neck abscess*
- A **deep neck abscess** would typically cause localized neck pain, swelling, dysphagia, and stridor, potentially with fever, but would not explain the widespread CNS symptoms (confusion, meningeal signs, CSF findings) or systemic signs of shock and coagulopathy seen here.
- While the patient has neck pain, it is due to **meningismus**, not a localized abscess, and there is no mention of local swelling or airway compromise.
Central nervous system infections US Medical PG Question 7: A 3-year-old girl is brought to the emergency room because of a 5-day history of high fever and fatigue. During this time she has been crying more than usual and eating less. Her mother says that the child has also complained about pain in her arms and legs for the past 3 days. She was born at term and has been otherwise healthy. She appears ill. Her temperature is 39.5°C (103.1°F), pulse is 128/min, and blood pressure is 96/52 mm Hg. The lungs are clear to auscultation. A grade 3/6 systolic murmur is heard at the apex. There is mild tenderness to palpation of the left upper quadrant with no guarding or rebound. The spleen is palpated 3 cm below the left costal margin. There is no redness or swelling of the joints. Laboratory studies show:
Hemoglobin 11.8 g/dL
Leukocyte count 16,300/mm3
Platelet count 220,000/mm3
Erythrocyte sedimentation rate 50 mm/h
Serum
Glucose 96 mg/dL
Creatinine 1.7 mg/dL
Total bilirubin 0.4 mg/dL
AST 18 U/L
ALT 20 U/L
Urine
Protein 2+
RBC casts rare
RBC 10/hpf
WBC 1–2/hpf
Which of the following is the most appropriate next step in management?
- A. Obtain a transesophageal echocardiography
- B. Administer intravenous vancomycin
- C. Obtain a renal biopsy
- D. Measure rheumatoid factors
- E. Obtain 3 sets of blood cultures (Correct Answer)
Central nervous system infections Explanation: ***Obtain 3 sets of blood cultures***
- The patient presents with **fever, new murmur**, and **splenomegaly**, in addition to elevated ESR and proteinuria. These findings are highly suggestive of **infective endocarditis**, which requires urgent diagnosis via blood cultures.
- Blood cultures are essential to identify the causative organism for targeted antibiotic therapy and confirm the diagnosis of endocarditis.
*Obtain a transesophageal echocardiography*
- While echocardiography is crucial for diagnosing endocarditis, **blood cultures should be obtained first** to identify the pathogen before initiating empiric antibiotics.
- Transesophageal echocardiography (TEE) provides superior visualization of vegetations compared to transthoracic echo (TTE) but is usually performed after positive blood cultures or if TTE is inconclusive.
*Administer intravenous vancomycin*
- Administering antibiotics prior to obtaining blood cultures can **sterilize the blood**, making it difficult to identify the causative organism and select effective definitive treatment.
- Empiric antibiotic therapy, such as vancomycin, is typically initiated after blood cultures are drawn, especially if the patient is severely ill and infective endocarditis is highly suspected.
*Obtain a renal biopsy*
- The patient has elevated creatinine and proteinuria with RBC casts, suggesting **glomerulonephritis**, which can be a complication of infective endocarditis or other systemic diseases.
- However, a renal biopsy is an invasive procedure and generally not the initial step in management for a sick child with suspected endocarditis, as the primary concern is the cardiac infection.
*Measure rheumatoid factors*
- Rheumatoid factors are associated with **rheumatoid arthritis** and other autoimmune conditions, which do not fully explain the constellation of symptoms (fever, new murmur, splenomegaly, elevated ESR, renal involvement) seen in this patient.
- While some autoimmune conditions can cause similar symptoms, the acute presentation with fever and a new murmur points more strongly towards an infectious etiology like endocarditis.
Central nervous system infections US Medical PG Question 8: A 32-year-old woman presents with a 3-month history of intermittent blurred vision and problems walking. The patient states that she often feels “pins and needles” in her legs that cause her problems when she’s walking. The patient is afebrile, and her vital signs are within normal limits. An autoimmune disorder is suspected. Which of the following findings would most likely be present in this patient?
- A. Damaged myelin sheath and myelin-producing cells (Correct Answer)
- B. Absence of interneurons
- C. Destruction of blood-brain barrier
- D. Degeneration of anterior horn cells
- E. Decreased cerebrospinal fluid due to destruction of cells
Central nervous system infections Explanation: ***Damaged myelin sheath and myelin-producing cells***
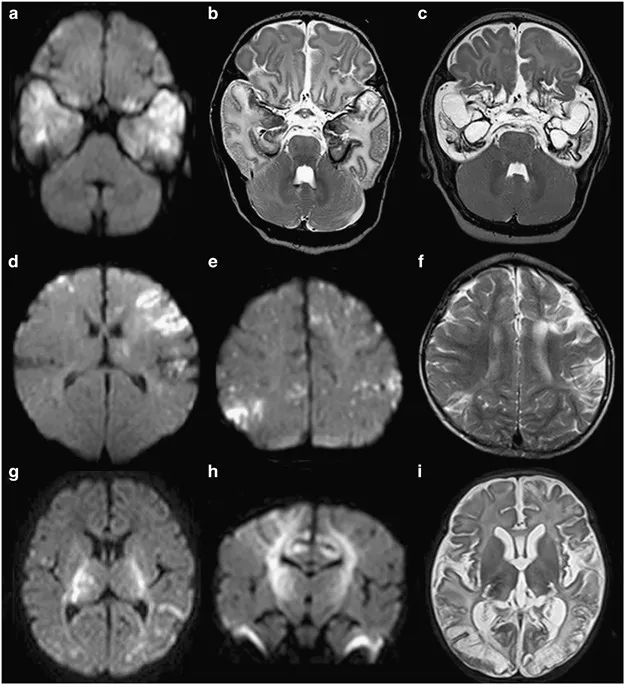
- The patient's symptoms of intermittent **blurred vision** (optic neuritis), **problems walking** (ataxia, spasticity), and **paresthesias** ("pins and needles") are classical presentations of Multiple Sclerosis (MS).
- MS is characterized by multifocal areas of inflammation and **demyelination** in the central nervous system, where the **myelin sheath** surrounding axons is damaged, and the **oligodendrocytes** (myelin-producing cells) are attacked.
- This demyelination disrupts saltatory conduction, leading to the varied and intermittent neurological symptoms.
*Absence of interneurons*
- The absence of **interneurons** is typically associated with conditions like **spinal muscular atrophy** or certain **neuropathies**, which present with different clinical features (e.g., muscle weakness, atrophy) than those described.
- While interneurons are crucial for neuronal communication, their absence doesn't explain the *intermittent* and multifocal symptoms seen in this case.
*Destruction of blood-brain barrier*
- While **blood-brain barrier (BBB) breakdown** does occur in MS, it is a *consequence* of the inflammatory process rather than the primary *pathological finding* that directly explains the neurological symptoms.
- BBB destruction allows inflammatory cells to enter the CNS, contributing to demyelination, but the core issue remains the myelin damage itself.
*Degeneration of anterior horn cells*
- **Anterior horn cell degeneration** is the hallmark of **amyotrophic lateral sclerosis (ALS)** and **spinal muscular atrophy**, presenting with progressive muscle weakness, atrophy, and fasciculations.
- These conditions lack the sensory symptoms (paresthesias) and visual disturbances seen in this patient, and typically show a progressive rather than intermittent course.
*Decreased cerebrospinal fluid due to destruction of cells*
- **Decreased CSF volume** is not a characteristic feature of MS; in fact, CSF analysis often shows increased protein and **oligoclonal bands**.
- The destruction of cells in MS primarily affects myelin and oligodendrocytes, not cells responsible for CSF production or volume regulation.
Central nervous system infections US Medical PG Question 9: A 21-year-old G3P2 woman presents to her obstetrician at 6 weeks gestation for routine prenatal care. Her past medical history includes obesity and gestational diabetes. She has had two spontaneous vaginal deliveries at term. One infant was macrosomic with hypoglycemia, but otherwise, she has had no complications. Her physician informs her that she must start taking a multivitamin with folic acid daily. The defect that folic acid supplementation protects against arises in tissue that is derived from which germ cell layer?
- A. Mesoderm
- B. Notochord
- C. Endoderm
- D. Mesenchyme
- E. Ectoderm (Correct Answer)
Central nervous system infections Explanation: ***Ectoderm***
- Folic acid supplementation primarily prevents **neural tube defects**, such as **spina bifida** and **anencephaly**.
- The **neural tube**, which forms the brain and spinal cord, is derived from the **ectoderm**.
*Mesoderm*
- The **mesoderm** gives rise to structures like muscle, bone, connective tissue, and the cardiovascular system.
- Defects in mesodermal development are not primarily prevented by folic acid supplementation.
*Notochord*
- The **notochord** is a transient embryonic structure that induces the formation of the neural plate from the ectoderm.
- While critical for nervous system development, it is not a germ cell layer itself, and defects in its development are not directly prevented by folic acid.
*Endoderm*
- The **endoderm** forms the lining of the gastrointestinal and respiratory tracts, as well as glands like the thyroid and pancreas.
- Anomalies of these internal organs are not the primary target of folic acid supplementation.
*Mesenchyme*
- **Mesenchyme** is embryonic connective tissue, largely derived from the mesoderm, but can also come from neural crest (ectoderm).
- It differentiates into connective tissues, blood, and lymphatic vessels; neural tube defects are not considered mesenchymal in origin.
Central nervous system infections US Medical PG Question 10: A 3-year-old boy is brought to the physician for the evaluation of recurrent skin lesions. The episodes of lesions started at the age of 3 months. He has also had several episodes of respiratory tract infections, enlarged lymph nodes, and recurrent fevers since birth. The boy attends daycare. The patient's immunizations are up-to-date. He is at the 5th percentile for length and 10th percentile for weight. He appears ill. Temperature is 38°C (100.4°F). Examination shows several raised, erythematous lesions of different sizes over the face, neck, groin, and extremities; some are purulent. Bilateral cervical and axillary lymphadenopathy are present. What is the most likely underlying mechanism of this patient's symptoms?
- A. Defective cytoplasmic tyrosine kinase
- B. NADPH oxidase deficiency (Correct Answer)
- C. Impaired signaling to actin cytoskeleton reorganization
- D. Defective neutrophil chemotaxis
- E. Impaired repair of double-strand DNA breaks
Central nervous system infections Explanation: ***NADPH oxidase deficiency***
- The recurrent skin abscesses (purulent lesions), respiratory tract infections, lymphadenopathy, and fevers point to chronic granulomatous disease (CGD), which is caused by a deficiency in **NADPH oxidase**.
- **NADPH oxidase** is essential for the production of reactive oxygen species (ROS) in phagocytes, which are critical for killing catalase-positive bacteria and fungi.
*Defective cytoplasmic tyrosine kinase*
- This mechanism is associated with **X-linked agammaglobulinemia (Bruton's agammaglobulinemia)**, which primarily causes recurrent bacterial infections due to a lack of B cells and antibodies.
- While recurrent infections occur, the typical presentation involves encapsulated bacteria and lacks the widespread purulent skin lesions and lymphadenopathy seen in CGD.
*Impaired signaling to actin cytoskeleton reorganization*
- This defect is characteristic of **Wiskott-Aldrich syndrome**, leading to thrombocytopenia, eczema, and recurrent infections, particularly by encapsulated bacteria.
- The clinical picture of recurrent widespread skin abscesses and granuloma formation is not typical for Wiskott-Aldrich syndrome.
*Defective neutrophil chemotaxis*
- This can be seen in conditions like **leukocyte adhesion deficiency (LAD)** or **Chédiak-Higashi syndrome**.
- LAD presents with recurrent bacterial infections, impaired wound healing, and delayed umbilical cord separation, while Chédiak-Higashi involves partial oculocutaneous albinism and recurrent pyogenic infections, distinct from this patient's symptoms.
*Impaired repair of double-strand DNA breaks*
- This defect is associated with conditions like **ataxia-telangiectasia**, which involves cerebellar ataxia, telangiectasias, and immunodeficiency (T-cell and IgA deficiency).
- The patient's symptoms of recurrent purulent skin lesions and infections are not characteristic of the DNA repair defects seen in ataxia-telangiectasia.
More Central nervous system infections US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.