Antimicrobial resistance in pediatrics US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Antimicrobial resistance in pediatrics. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Antimicrobial resistance in pediatrics US Medical PG Question 1: Three days after admission to the hospital following a motor vehicle accident, a 45-year-old woman develops a fever. A central venous catheter was placed on the day of admission for treatment of severe hypotension. Her temperature is 39.2°C (102.5°F). Examination shows erythema surrounding the catheter insertion site at the right internal jugular vein. Blood cultures show gram-positive, catalase-positive cocci that have a high minimum inhibitory concentration when exposed to novobiocin. Which of the following is the most appropriate pharmacotherapy?
- A. Clarithromycin
- B. Vancomycin (Correct Answer)
- C. Metronidazole
- D. Penicillin G
- E. Polymyxin B
Antimicrobial resistance in pediatrics Explanation: ***Vancomycin***
- The description of **gram-positive, catalase-positive cocci** that are **novobiocin-resistant** (high MIC) strongly points to **Staphylococcus epidermidis** or other coagulase-negative staphylococci. *S. epidermidis* is the most common cause of **catheter-related bloodstream infections** and is often **methicillin-resistant**, making **vancomycin** the drug of choice.
- The presence of erythema at the catheter site and fever in a patient with a central venous catheter indicates a **central line-associated bloodstream infection (CLABSI)**, for which empiric coverage with vancomycin is standard until sensitivities are known.
- The novobiocin resistance test helps differentiate *S. epidermidis* (resistant) from *S. saprophyticus* (sensitive).
*Clarithromycin*
- **Clarithromycin** is a macrolide antibiotic primarily used for respiratory tract infections and *Mycobacterium avium complex*.
- It is **not effective** against methicillin-resistant staphylococci and would not be appropriate for a suspected CLABSI.
*Metronidazole*
- **Metronidazole** is an antibiotic mainly used for **anaerobic bacterial infections** and certain parasitic infections.
- It has **no activity** against gram-positive cocci like staphylococci.
*Penicillin G*
- **Penicillin G** is a narrow-spectrum penicillin effective against some gram-positive cocci, like **Streptococcus pyogenes**.
- However, virtually all staphylococci, especially those causing hospital-acquired infections, are **resistant to penicillin G** due to beta-lactamase (penicillinase) production.
*Polymyxin B*
- **Polymyxin B** is an antibiotic primarily effective against **gram-negative bacteria**, particularly those with multi-drug resistance such as **Pseudomonas aeruginosa** and **Acinetobacter baumannii**.
- It has **no significant activity** against gram-positive cocci like staphylococci.
Antimicrobial resistance in pediatrics US Medical PG Question 2: A 32-year-old man presents to an outpatient clinic for tuberculosis prophylaxis before leaving for a trip to Asia, where tuberculosis is endemic. The Mantoux test is positive, but the chest X-ray and AFB sputum culture are negative. He was started on isoniazid. What is the most likely mechanism of resistance to isoniazid?
- A. Methylation of the RNA binding site
- B. Plasmid-mediated resistance
- C. Reduction of drug binding to RNA polymerase
- D. Increased efflux from the cell
- E. Mutations in katG (Correct Answer)
Antimicrobial resistance in pediatrics Explanation: ***Mutations in katG***
- The **katG gene** encodes **catalase-peroxidase**, an enzyme essential for activating isoniazid into its active form within *Mycobacterium tuberculosis*.
- Mutations in *katG* prevent the activation of isoniazid, thereby conferring **resistance**.
*Methylation of the RNA binding site*
- This mechanism is primarily associated with **aminoglycoside resistance**, where methylation of ribosomal RNA prevents antibiotic binding.
- It is not a known mechanism for resistance to **isoniazid**.
*Plasmid-mediated resistance*
- While common in many bacteria for antibiotic resistance, **plasmid-mediated resistance** is rare for **first-line anti-tuberculosis drugs** like isoniazid in *Mycobacterium tuberculosis*.
- Most *M. tuberculosis* resistance mechanisms involve **chromosomal mutations**.
*Reduction of drug binding to RNA polymerase*
- This mechanism is typically associated with resistance to **rifamycins** (e.g., rifampin), which target the **bacterial RNA polymerase**.
- Isoniazid's mechanism of action involves **mycolic acid synthesis inhibition**, not RNA polymerase binding.
*Increased efflux from the cell*
- While efflux pumps contribute to antibiotic resistance in many bacteria, they are less commonly the primary mechanism for high-level **isoniazid resistance** in *M. tuberculosis*.
- Resistance is predominantly linked to target modification or enzyme deficits, like those involving **katG**.
Antimicrobial resistance in pediatrics US Medical PG Question 3: A scientist is studying the mechanisms by which bacteria become resistant to antibiotics. She begins by obtaining a culture of vancomycin-resistant Enterococcus faecalis and conducts replicate plating experiments. In these experiments, colonies are inoculated onto a membrane and smeared on 2 separate plates, 1 containing vancomycin and the other with no antibiotics. She finds that all of the bacterial colonies are vancomycin resistant because they grow on both plates. She then maintains the bacteria in liquid culture without vancomycin while she performs her other studies. Fifteen generations of bacteria later, she conducts replicate plating experiments again and finds that 20% of the colonies are now sensitive to vancomycin. Which of the following mechanisms is the most likely explanation for why these colonies have become vancomycin sensitive?
- A. Point mutation
- B. Gain of function mutation
- C. Viral infection
- D. Plasmid loss (Correct Answer)
- E. Loss of function mutation
Antimicrobial resistance in pediatrics Explanation: ***Plasmid loss***
- The initial **vancomycin resistance** in *Enterococcus faecalis* is often mediated by genes located on **plasmids**, which are extrachromosomal DNA.
- In the absence of selective pressure (vancomycin), bacteria that lose the plasmid (and thus the resistance genes) have a **growth advantage** over those that retain the energetically costly plasmid, leading to an increase in sensitive colonies over generations.
*Point mutation*
- A **point mutation** typically involves a change in a single nucleotide and could lead to loss of resistance if it occurred in a gene conferring resistance.
- However, since there was no selective pressure for loss of resistance, it is less likely that 20% of the population would acquire such a specific point mutation to revert resistance.
*Gain of function mutation*
- A **gain of function mutation** would imply that the bacteria acquired a *new* advantageous trait, not the *loss* of resistance.
- This type of mutation would not explain why some colonies became sensitive to vancomycin after the drug was removed.
*Viral infection*
- **Viral infection** (bacteriophages) can transfer genes through transduction or cause bacterial lysis, but it's not the primary mechanism for a widespread reversion of resistance in the absence of antibiotic pressure.
- It would not explain the observed increase in vancomycin-sensitive colonies due to evolutionary pressure.
*Loss of function mutation*
- While a **loss of function mutation** in a gene conferring resistance could lead to sensitivity, it's generally less likely to explain a 20% shift without selective pressure than **plasmid loss**.
- Plasmids are often unstable and are easily lost in the absence of selection, whereas a specific gene mutation causing loss of function would need to arise and become prevalent in the population.
Antimicrobial resistance in pediatrics US Medical PG Question 4: A 3-year-old child is brought to the pediatrician by his mother who states that he has been fussy for the past two days. She says that he has had a runny nose, a cough, a sore throat, and decreased appetite. Vital signs are within normal limits. Physical exam reveals a slightly erythematous oropharynx and clear nasal discharge. The mother states that she is a single mother working at a busy law firm. The mother demands that the child receive antibiotics, as her babysitter refuses to care for the child unless he is treated with antibiotics. You diagnose the child with the common cold and inform the mother that antibiotics are not indicated. She is infuriated and accuses you of refusing to treat her child appropriately. How should you respond?
- A. Prescribe a placebo
- B. Ask the mother to leave immediately
- C. Prescribe antibiotics to the child
- D. Refer the mother to a nearby physician who will prescribe antibiotics
- E. Explain the reasoning as to why antibiotics are not indicated for the common cold (Correct Answer)
Antimicrobial resistance in pediatrics Explanation: ***Explain the reasoning as to why antibiotics are not indicated for the common cold***
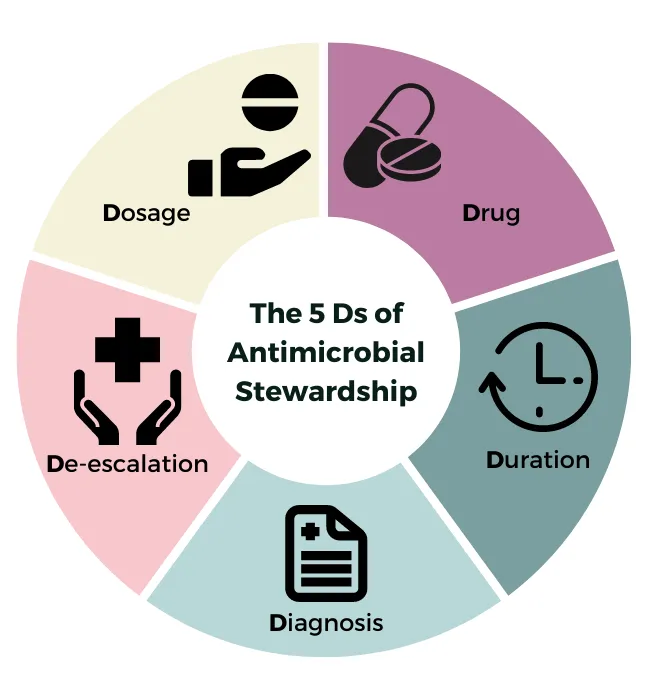
- Maintaining a **professional and ethical stance** involves educating the patient or guardian about the appropriate medical management, especially regarding the judicious use of antibiotics.
- The common cold is **virally mediated**, and antibiotics are ineffective against viruses and contribute to **antibiotic resistance** when used inappropriately.
*Prescribe a placebo*
- Prescribing a placebo without the patient's or guardian's informed consent is **deceptive** and unethical, undermining trust in the physician-patient relationship.
- This practice does not address the underlying issue of the mother's misunderstanding about antibiotic use and avoids proper medical education.
*Ask the mother to leave immediately*
- This response is **unprofessional** and dismissive, failing to address the mother's concerns or provide appropriate patient education.
- It escalates the conflict and breaches the physician's duty to provide compassionate care and education.
*Prescribe antibiotics to the child*
- Prescribing antibiotics for a **viral infection** is inappropriate, contributing to **antibiotic resistance** and potentially exposing the child to unnecessary side effects.
- Yielding to inappropriate demands compromises medical ethics and best practices for patient care.
*Refer the mother to a nearby physician who will prescribe antibiotics*
- Referring the mother to another physician who is known to act unethically by prescribing unnecessary antibiotics would be an **unethical action** by physicians.
- This action promotes **inappropriate medical practices** and does not uphold the standards of care.
Antimicrobial resistance in pediatrics US Medical PG Question 5: You are treating a neonate with meningitis using ampicillin and a second antibiotic, X, that is known to cause ototoxicity. What is the mechanism of antibiotic X?
- A. It binds the 50S ribosomal subunit and inhibits formation of the initiation complex
- B. It binds the 30S ribosomal subunit and inhibits formation of the initiation complex (Correct Answer)
- C. It binds the 30S ribosomal subunit and reversibly inhibits translocation
- D. It binds the 50S ribosomal subunit and inhibits peptidyltransferase
- E. It binds the 50S ribosomal subunit and reversibly inhibits translocation
Antimicrobial resistance in pediatrics Explanation: ***It binds the 30s ribosomal subunit and inhibits formation of the initiation complex***
- The second antibiotic, X, is likely an **aminoglycoside**, such as **gentamicin** or **amikacin**, which are commonly used in combination with ampicillin for neonatal meningitis and are known to cause ototoxicity.
- Aminoglycosides exert their bactericidal effect by **irreversibly binding to the 30S ribosomal subunit**, thereby **inhibiting the formation of the initiation complex** and leading to misreading of mRNA.
*It binds the 50S ribosomal subunit and inhibits formation of the initiation complex*
- This mechanism is characteristic of **linezolid**, which targets the 50S ribosomal subunit to prevent the formation of the initiation complex.
- While linezolid can cause side effects, **ototoxicity** is less commonly associated with it compared to aminoglycosides, and it is not a primary drug for neonatal meningitis alongside ampicillin.
*It binds the 50S ribosomal subunit and inhibits peptidyltransferase*
- This is the mechanism of action for **chloramphenicol**, which inhibits **peptidyltransferase** activity on the 50S ribosomal subunit, preventing peptide bond formation.
- Although chloramphenicol can cause **ototoxicity** and **aplastic anemia**, its use in neonates is limited due to the risk of **Gray Baby Syndrome**.
*It binds the 30s ribosomal subunit and reversibly inhibits translocation*
- This describes the mechanism of action of **tetracyclines**, which reversibly bind to the 30S ribosomal subunit and prevent the attachment of aminoacyl-tRNA, thereby inhibiting protein synthesis.
- Tetracyclines are **contraindicated in neonates** due to their potential to cause **tooth discoloration** and **bone growth inhibition**, and ototoxicity is not their primary adverse effect.
*It binds the 50s ribosomal subunit and reversibly inhibits translocation*
- This mechanism of reversibly inhibiting translocation by binding to the 50S ribosomal subunit is characteristic of **macrolides** (e.g., erythromycin, azithromycin) and **clindamycin**.
- While some macrolides can cause **transient ototoxicity**, they are not typically the second antibiotic of choice for neonatal meningitis in combination with ampicillin, and clindamycin's side effect profile is different.
Antimicrobial resistance in pediatrics US Medical PG Question 6: A 26-year-old patient presents to your office with rhinorrhea that you believe to be viral in origin. He respectfully requests treatment with antibiotics, and he demonstrates an understanding of the risks, benefits, and alternatives to treatment. His mental status is intact, and you believe him to have full decision-making capacity. Which of the following is the best course of action?
- A. Refer the patient to an infectious disease specialist
- B. Prescribe ciprofloxacin
- C. Prescribe amoxicillin
- D. Deny the patient's request (Correct Answer)
- E. Prescribe zidovudine
Antimicrobial resistance in pediatrics Explanation: ***Deny the patient's request***
- As a physician, you have a professional obligation to act in the patient's best interest, which includes avoiding **unnecessary treatments** that could cause harm.
- Prescribing antibiotics for a **viral infection** contributes to **antibiotic resistance**, exposes the patient to potential side effects (e.g., *C. difficile* infection), and contradicts evidence-based medical practice.
*Refer the patient to an infectious disease specialist*
- This is an **unnecessary referral** as the diagnosis is clear (viral rhinorrhea) and does not require specialized infectious disease management.
- Referral would incur **additional healthcare costs** and delays for a condition that does not warrant such specialized consultation.
*Prescribe ciprofloxacin*
- Ciprofloxacin is a **broad-spectrum antibiotic** that is completely ineffective against viral infections and carries a risk of significant side effects, including **tendon rupture** and *C. difficile* infection.
- Misuse of powerful antibiotics like ciprofloxacin promotes **antibiotic resistance**, making future bacterial infections harder to treat.
*Prescribe amoxicillin*
- Amoxicillin is an antibiotic and, like other antibiotics, is **ineffective against viral infections** such as viral rhinorrhea.
- Prescribing it would contribute to **antibiotic resistance** and expose the patient to potential drug side effects (e.g., rash, gastrointestinal upset) without any clinical benefit.
*Prescribe zidovudine*
- Zidovudine is an **antiretroviral medication** specifically used for the treatment of **HIV infection**.
- It has absolutely **no role** in treating common viral rhinorrhea and would be an inappropriate and potentially harmful prescription.
Antimicrobial resistance in pediatrics US Medical PG Question 7: A 27-year-old man presents to the emergency department with weakness and a fever for the past week. The patient is homeless and has a past medical history of alcohol and IV drug abuse. His temperature is 102°F (38.9°C), blood pressure is 107/68 mmHg, pulse is 120/min, respirations are 17/min, and oxygen saturation is 98% on room air. Physical exam is notable for a tremulous patient with antecubital scars and a murmur over the left lower sternal border. Blood cultures are drawn and the patient is started on vancomycin and ceftriaxone and is admitted to the ICU. The patient's fever and symptoms do not improve despite antibiotic therapy for which the initial identified organism is susceptible. Cultures currently reveal MRSA as one of the infective organisms. Which of the following is the best next step in management?
- A. Transesophageal echocardiography (Correct Answer)
- B. Obtain new blood cultures
- C. CT scan of the chest
- D. Nafcillin and piperacillin-tazobactam
- E. Vancomycin and gentamicin
Antimicrobial resistance in pediatrics Explanation: ***Transesophageal echocardiography***
- The patient's history of **IV drug abuse**, **fever**, **new murmur**, and identification of **MRSA** strongly suggest **infective endocarditis**.
- A Transesophageal echocardiography (TEE) is the **most sensitive and specific imaging modality** to detect vegetations, abscesses, or valvular damage, which is crucial for guiding further management.
*Obtain new blood cultures*
- While repeating blood cultures can be useful to confirm eradication or identify new pathogens, the initial blood cultures already revealed MRSA, which is a common cause of **endocarditis in IV drug users**.
- The immediate priority given the lack of improvement and high suspicion of endocarditis is to visualize the heart valves for vegetations.
*CT scan of the chest*
- A CT scan of the chest would be useful to look for complications such as **septic emboli in the lungs** or other pulmonary pathologies.
- However, it would not provide the detailed visualization of heart valves necessary to diagnose or rule out valvular vegetations characteristic of endocarditis.
*Nafcillin and piperacillin-tazobactam*
- **Nafcillin** is active against **methicillin-susceptible Staphylococcus aureus (MSSA)**, but the patient's cultures already identified **MRSA**.
- **Piperacillin-tazobactam** is a broad-spectrum antibiotic but not a first-line treatment for MRSA infections and would not be appropriate given the identified pathogen.
*Vancomycin and gentamicin*
- The patient is already on **Vancomycin**, which is appropriate for MRSA, but adding **gentamicin** without clear indication would not be the best next step.
- While gentamicin is sometimes used as an adjunct in specific endocarditis regimens (e.g., enterococcal), the primary concern here is the lack of clinical improvement despite appropriate MRSA coverage, pointing towards a structural cardiac issue.
Antimicrobial resistance in pediatrics US Medical PG Question 8: A 2-year-old boy is brought to the physician by his mother because of fever and left ear pain for the past 3 days. He has also been frequently rubbing his left ear since he woke up in the morning. He has a history of atopic dermatitis, and his mother is concerned that his symptoms may be caused by him itching at night. She says that he has not been having many flare-ups lately; the latest flare-up subsided in time for his second birthday party, which he celebrated at a swimming pool 1 week ago. Six months ago, he had an episode of urticaria following antibiotic treatment for pharyngitis. He takes no medications. His temperature is 38.5°C (101.3°F), pulse is 110/min, respirations are 25/min, and blood pressure is 90/50 mm Hg. Otoscopy shows an opaque, bulging tympanic membrane. Which of the following is the most appropriate next step in management?
- A. Tympanocentesis
- B. Topical hydrocortisone and gentamicin eardrops
- C. Otic ofloxacin therapy
- D. Oral azithromycin (Correct Answer)
- E. Tympanostomy tube placement
Antimicrobial resistance in pediatrics Explanation: ***Oral azithromycin***
- The patient presents with classic symptoms of **acute otitis media (AOM)**, including fever, ear pain, and an opaque, bulging tympanic membrane. Given his recent history of urticaria following antibiotic treatment for pharyngitis, **azithromycin** is an appropriate choice due to its effectiveness against common AOM pathogens and its use in patients with **penicillin allergies**.
- This patient is generally healthy, above 6 months of age, and not severely ill, making oral antibiotic therapy the standard and most appropriate first-line treatment.
*Tympanocentesis*
- This procedure involves puncturing the tympanic membrane to aspirate middle ear fluid for culture and relief of pressure, and is typically reserved for **severely ill children**, those with **immunocompromise**, or in cases of **treatment failure** on empiric antibiotics, which is not indicated here.
- It is an **invasive procedure** and not a first-line treatment for uncomplicated acute otitis media.
*Topical hydrocortisone and gentamicin eardrops*
- **Topical corticosteroids** are used to reduce inflammation in conditions like **otitis externa**, while **gentamicin** is an aminoglycoside antibiotic primarily used for topical infections.
- These eardrops are inappropriate for **acute otitis media (AOM)** because the infection is in the middle ear, behind an intact tympanic membrane, and thus topical medications cannot reach the site of infection.
*Otic ofloxacin therapy*
- **Otic fluoroquinolone drops** like ofloxacin are primarily used for **otitis externa** or in cases of **perforated tympanic membranes** with otitis media, as they can directly reach the infection in the outer ear canal or middle ear.
- They are not indicated as a primary treatment for acute otitis media with an **intact, bulging tympanic membrane**, as the drops would not be able to reach the middle ear.
*Tympanostomy tube placement*
- This surgical procedure involves placing tubes through the tympanic membrane to **ventilate the middle ear** and prevent recurrent infections or persistent effusions.
- It is typically considered for **recurrent acute otitis media** (e.g., three episodes in 6 months or four in a year with at least one in the preceding 6 months) or **persistent otitis media with effusion** leading to hearing loss, neither of which is the case for this patient's first presentation.
Antimicrobial resistance in pediatrics US Medical PG Question 9: A 7-year-old boy comes to the physician because of a generalized rash for 3 days. Over the past 5 days, he has also had a high fever and a sore throat. His 16-year-old sister was treated for infectious mononucleosis 2 weeks ago. He returned from a summer camp a week ago. His immunizations are up-to-date. Three years ago, he required intubation after an allergic reaction to dicloxacillin. The patient appears ill. His temperature is 38.2°C (100.8°F). Examination shows circumferential oral pallor. Cervical lymphadenopathy is present. There is tonsillar erythema and exudate. A confluent, blanching, punctate erythematous rash with a rough texture is spread over his trunk and extremities. His hemoglobin concentration is 13.3 g/dL, leukocyte count is 12,000/mm3, and erythrocyte sedimentation rate is 43 mm/h. Which of the following is the most appropriate next step in management?
- A. Amoxicillin therapy
- B. Doxycycline therapy
- C. Azithromycin therapy (Correct Answer)
- D. Cephalexin therapy
- E. Acyclovir therapy
Antimicrobial resistance in pediatrics Explanation: ***Azithromycin therapy***
- This patient presents with symptoms highly suggestive of **streptococcal pharyngitis** (sore throat, fever, tonsillar exudates, cervical lymphadenopathy) complicated by **scarlet fever** (confluent, blanching, punctate erythematous rash with a rough texture, circumferential oral pallor).
- Given his **history of severe allergic reaction (intubation) to dicloxacillin**, a penicillin-class antibiotic, azithromycin (a macrolide) is the appropriate choice for treating **Group A Streptococcus** (GAS) infection in a penicillin-allergic patient.
*Amoxicillin therapy*
- **Amoxicillin** is a penicillin-class antibiotic and is **contraindicated** due to the patient's severe allergic reaction (intubation) to dicloxacillin, another penicillin.
- Cross-reactivity between penicillins, especially in severe allergic reactions, is a significant concern, making this an unsafe choice.
*Doxycycline therapy*
- **Doxycycline**, a tetracycline, is not a first-line treatment for **streptococcal pharyngitis** and is primarily used for atypical bacterial infections or in specific cases of penicillin allergy where other agents are not suitable.
- While it has some activity against GAS, macrolides like azithromycin are preferred alternatives for penicillin-allergic patients.
*Cephalexin therapy*
- **Cephalexin** is a first-generation cephalosporin, and while it can be used for GAS, roughly 5-10% of patients with a penicillin allergy may have a **cross-reaction** to cephalosporins, especially with a history of severe reactions.
- Therefore, it is generally avoided in patients with a history of anaphylaxis or other severe reactions to penicillin.
*Acyclovir therapy*
- **Acyclovir** is an antiviral medication used to treat herpes simplex and varicella-zoster virus infections.
- The patient's symptoms (pharyngitis, rash consistent with scarlet fever) are indicative of a **bacterial infection (GAS)**, not a viral infection that would respond to acyclovir.
Antimicrobial resistance in pediatrics US Medical PG Question 10: A 7-year-old boy is brought to the emergency department because of a 3-day history of generalized fatigue, myalgia, and fever. He has sickle cell disease. His current medications include hydroxyurea and folic acid. He appears ill. His temperature is 39.2°C (102.6°F), pulse is 103/min, and respirations are 28/min. Examination shows pale conjunctivae. The lungs are clear to auscultation. The abdomen is soft and nontender. Neurologic examination shows no focal findings, His hemoglobin concentration is 10.3 g/dL and leukocyte count is 14,100/mm3. Intravenous fluid is administered and blood cultures are obtained. Which of the following is the most appropriate next step in treatment?
- A. Clindamycin
- B. Prednisone
- C. Vancomycin
- D. Ceftriaxone (Correct Answer)
- E. Levofloxacin
Antimicrobial resistance in pediatrics Explanation: ***Ceftriaxone***
- This patient presents with **fever** and **sickle cell disease**, placing him at high risk for bacterial infections, especially from **encapsulated organisms** like *Streptococcus pneumoniae* and *Haemophilus influenzae*. **Ceftriaxone** is a broad-spectrum third-generation cephalosporin that provides excellent coverage against these common pathogens.
- Due to the high risk of **sepsis** and rapid progression of infection in sickle cell patients, empiric, prompt administration of **intravenous antibiotics** is crucial, even before culture results are available.
*Clindamycin*
- **Clindamycin** is primarily effective against **anaerobic bacteria** and some gram-positive organisms, including methicillin-sensitive *Staphylococcus aureus* (MSSA).
- It does not provide adequate coverage against the most common and life-threatening pathogens in febrile sickle cell patients, such as encapsulated bacteria.
*Prednisone*
- **Prednisone** is a corticosteroid used for its **anti-inflammatory** and immunosuppressive effects. It is not indicated for the initial management of fever and suspected bacterial infection.
- Administering corticosteroids in a patient with suspected infection without appropriate antibiotic coverage could worsen the infection.
*Vancomycin*
- **Vancomycin** is a powerful antibiotic primarily used to cover **multi-drug resistant gram-positive bacteria**, especially **MRSA** and drug-resistant *S. pneumoniae*.
- While it covers gram-positive organisms well, it does **not cover gram-negative bacteria** such as *H. influenzae* or *Salmonella* species, which are important pathogens in sickle cell patients. **Ceftriaxone** provides broader coverage including both gram-positive and gram-negative encapsulated organisms, making it the preferred empiric choice.
*Levofloxacin*
- **Levofloxacin** is a fluoroquinolone that provides broad-spectrum coverage, including against atypical organisms and some gram-negatives and gram-positives.
- However, **fluoroquinolones** are generally avoided in children due to potential adverse effects on cartilage development, and it is not the first-line empiric choice for severe bacterial infections in this age group, especially when **cephalosporins** are highly effective and safer.
More Antimicrobial resistance in pediatrics US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.