Infectious Disease

On this page
🦠 The Infectious Disease Command Center: Pediatric Pathogen Mastery
Infectious diseases remain the leading reason children seek medical care, yet distinguishing viral from bacterial illness, recognizing early sepsis, and choosing appropriate antimicrobials demands systematic clinical reasoning under pressure. You'll master pathogen recognition patterns, build diagnostic frameworks that integrate history with physical findings and laboratory data, and develop treatment algorithms that balance antimicrobial stewardship with patient safety. By connecting infectious principles across organ systems-from febrile neonate protocols to post-splenectomy prophylaxis-you'll transform pattern recognition into confident, evidence-based action when every decision counts.
The Infectious Disease Spectrum: Age-Dependent Vulnerability Patterns
Pediatric infectious susceptibility follows distinct age-related patterns driven by immune system maturation and environmental exposure:
-
Neonatal Period (0-28 days)
- Group B Streptococcus: 60% of early-onset sepsis cases
- E. coli: 25% of late-onset meningitis
- Maternal antibody protection: IgG transfer at 32+ weeks
- Preterm infants: ↓85% protective antibodies
- Term infants: Full maternal IgG by birth
- Antibody half-life: 21-28 days postnatal
-
Infant Period (1-12 months)
- RSV bronchiolitis: Peak incidence 2-6 months
- Pertussis vulnerability: 90% of deaths occur <6 months
- Vaccine-preventable diseases: Maximum risk 2-4 months
- Maternal antibody waning: 50% reduction by 3 months
- Primary immunization incomplete until 6 months
-
Toddler Period (1-3 years)
- Viral exanthems: Peak incidence 12-36 months
- Febrile seizures: 85% occur between 6 months-5 years
- Daycare exposure: ↑300% respiratory infection rate
📌 Remember: NITS for age-specific infectious priorities - Neonatal sepsis, Infant RSV/pertussis, Toddler viral exanthems, School-age atypical pneumonia
⭐ Clinical Pearl: Fever >38.5°C in infants <3 months requires immediate sepsis workup with blood culture, urine culture, and lumbar puncture - bacteremia risk 12-15% in this age group
| Age Group | Primary Pathogens | Key Clinical Features | Diagnostic Priority | Mortality Risk |
|---|---|---|---|---|
| 0-28 days | GBS, E.coli, Listeria | Poor feeding, lethargy | Blood/CSF culture | 15-20% |
| 1-3 months | S.pneumoniae, N.meningitidis | Fever, irritability | Full sepsis workup | 8-12% |
| 3-24 months | Viral (RSV, influenza) | Respiratory distress | Rapid antigen tests | 2-5% |
| 2-5 years | Streptococcus, viral exanthems | Fever, rash patterns | Clinical diagnosis | <1% |
| 5+ years | Mycoplasma, viral URI | Atypical pneumonia | Chest imaging | <0.5% |
Pediatric immune competence develops through predictable stages that directly influence infection susceptibility and clinical presentation:
-
Innate Immunity Maturation
- Neutrophil function: Reaches adult levels by 2 years
- Complement system: C3/C4 levels adult values by 6-12 months
- Natural killer cells: Full cytotoxicity by 12 months
-
Adaptive Immunity Development
- T-cell responses: Mature Th1 responses by 2-3 years
- B-cell function: IgG subclass maturation by 4-6 years
- Memory formation: Durable responses established by 5-7 years
💡 Master This: Young children show ↑atypical presentations of serious infections due to immature inflammatory responses - absence of fever in 15-20% of neonatal sepsis cases and delayed meningeal signs in 40% of infant meningitis
The foundation of pediatric infectious disease mastery lies in understanding these age-dependent vulnerability patterns and immune maturation timelines. Connect this developmental framework through pathogen-specific recognition patterns to build comprehensive diagnostic expertise.
🦠 The Infectious Disease Command Center: Pediatric Pathogen Mastery
🎯 Pathogen Recognition Arsenal: The Clinical Detective's Toolkit
Bacterial Pathogen Signatures: The High-Stakes Players
Bacterial infections in children present with distinct clinical fingerprints that enable rapid recognition and targeted intervention:
-
Streptococcus pneumoniae
- Clinical signature: Abrupt fever >39.5°C, rigors, focal consolidation
- Laboratory markers: WBC >15,000 with >80% neutrophils
- Complications: Bacteremia 15-25%, meningitis 1-2%
- Pneumococcal pneumonia: Lobar consolidation in 70%
- Empyema development: 8-12% of hospitalized cases
- Treatment response: Defervescence within 48-72 hours
-
Haemophilus influenzae type b
- Clinical signature: Epiglottitis, cellulitis, septic arthritis
- Age predilection: Peak 6 months-4 years (pre-vaccine era)
- Current incidence: ↓99% post-Hib vaccination
- Epiglottitis: Drooling, stridor, tripod positioning
- Cellulitis: Violaceous, well-demarcated facial involvement
- Bacteremia rate: >90% with invasive disease
-
Neisseria meningitidis
- Clinical signature: Petechial rash + meningeal signs
- Progression timeline: Shock within 6-12 hours
- Mortality rates: Meningitis 5-10%, Sepsis 20-40%
- Rash evolution: Petechiae → purpura → ecchymoses
- Adrenal involvement: Waterhouse-Friderichsen syndrome
- Close contact prophylaxis: Rifampin within 24 hours
📌 Remember: SPINE for serious bacterial infections - Streptococcus (pneumonia), Pneumococcus (meningitis), Invasive Hib, Neisseria (sepsis), Enterococcus (UTI)
⭐ Clinical Pearl: Petechial rash below the nipple line in a febrile child has 85% positive predictive value for meningococcal disease - immediate blood culture and empiric antibiotics indicated
Viral Pathogen Patterns: The Great Mimickers
Viral infections dominate pediatric infectious disease presentations, requiring systematic differentiation from bacterial causes:
-
Respiratory Syncytial Virus (RSV)
- Seasonal pattern: October-March in temperate climates
- Age impact: Hospitalization rate 1-3% in first year
- Clinical progression: Rhinorrhea → cough → wheeze → apnea
- Bronchiolitis criteria: Age <2 years + first wheeze episode
- Severe disease markers: RR >70, O2 sat <92%, poor feeding
- Apnea risk: ↑20-fold in infants <6 weeks
-
Influenza A/B
- Clinical signature: Abrupt fever + myalgia + headache
- Complications: Secondary bacterial pneumonia 5-15%
- Antiviral efficacy: ↓symptom duration 1-2 days if started <48 hours
- Oseltamivir dosing: 3mg/kg BID for children >1 year
- Pneumonia risk factors: Age <2 years, chronic conditions
- Rapid testing: Sensitivity 50-70%, specificity >95%
-
Human Metapneumovirus (hMPV)
- Clinical overlap: Indistinguishable from RSV clinically
- Seasonal timing: Late winter/early spring
- Diagnostic approach: PCR panel for differentiation
- Hospitalization rate: Similar to RSV in young infants
- Treatment: Supportive care identical to RSV
- Prevention: No vaccine available
💡 Master This: Viral vs bacterial pneumonia differentiation - gradual onset, bilateral infiltrates, and WBC <15,000 suggest viral etiology with 80% accuracy, while abrupt fever, lobar consolidation, and neutrophilia indicate bacterial cause
| Pathogen | Incubation | Key Clinical Features | Diagnostic Test | Treatment Response |
|---|---|---|---|---|
| S. pneumoniae | 1-3 days | Abrupt fever, rigors | Blood culture | 48-72h defervescence |
| N. meningitidis | 2-10 days | Petechial rash, shock | Blood culture | 24-48h improvement |
| RSV | 4-6 days | Gradual wheeze, apnea | PCR/antigen | 7-10d resolution |
| Influenza | 1-4 days | Abrupt myalgia, fever | Rapid antigen | 3-5d with antivirals |
| hMPV | 5-8 days | RSV-like syndrome | PCR panel | 7-14d supportive |
🎯 Pathogen Recognition Arsenal: The Clinical Detective's Toolkit
🔬 Diagnostic Precision Matrix: Evidence-Based Clinical Decision Making
Laboratory Markers: The Inflammatory Cascade Indicators
Systematic interpretation of inflammatory markers enables differentiation between bacterial and viral infections with high clinical accuracy:
-
Complete Blood Count Patterns
- Bacterial infections: WBC >15,000 with >80% neutrophils
- Viral infections: WBC 5,000-12,000 with >50% lymphocytes
- Left shift significance: >10% bands suggests bacterial etiology
- Neutrophil count: >10,000 indicates bacterial infection (85% sensitivity)
- Lymphocyte predominance: >60% suggests viral cause (80% specificity)
- Thrombocytopenia: <100,000 in 25% of viral infections
-
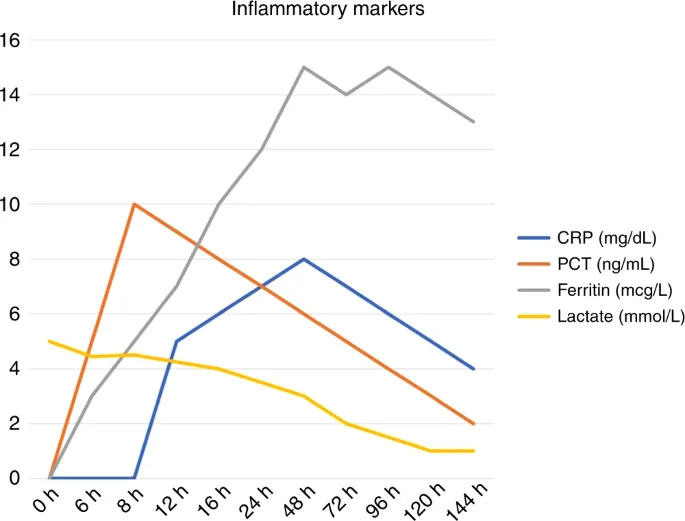
Acute Phase Reactants
- C-Reactive Protein (CRP): >40 mg/L suggests bacterial infection
- Procalcitonin (PCT): >0.5 ng/mL indicates bacterial sepsis
- Erythrocyte Sedimentation Rate: >30 mm/hr in inflammatory conditions
- CRP kinetics: Peaks 24-48 hours, normalizes 3-7 days
- PCT specificity: 90% for bacterial vs viral differentiation
- Combined markers: CRP + PCT achieves 95% diagnostic accuracy
-
Age-Specific Reference Ranges
- Neonatal WBC: 9,000-30,000 (normal range wider)
- Infant neutrophils: Adult ratios achieved by 2 years
- CRP production: Limited in neonates <7 days old
- Neonatal sepsis: Normal WBC in 30% of cases
- Immature:Total neutrophil ratio: >0.2 suggests sepsis
- Platelet count: <100,000 in 40% of neonatal sepsis
📌 Remember: CRISP for inflammatory markers - CRP >40, Rising PCT, Increased neutrophils, Shift to left, Platelet changes
⭐ Clinical Pearl: Procalcitonin <0.25 ng/mL has 95% negative predictive value for bacterial infection, enabling safe antibiotic discontinuation in clinically stable patients
Culture Techniques: The Gold Standard Approaches
Optimal culture collection and interpretation remain fundamental to infectious disease diagnosis and antimicrobial stewardship:
-
Blood Culture Optimization
- Volume requirements: 1-3 mL per bottle in children
- Collection timing: Before antibiotics when possible
- Yield optimization: 2 sets from different sites
- Contamination rates: <3% with proper technique
- Time to positivity: Median 12-24 hours for common pathogens
- Sensitivity: >95% for bacteremia detection
-
Cerebrospinal Fluid Analysis
- Normal parameters: <5 WBC/μL, glucose >40 mg/dL
- Bacterial meningitis: >1000 WBC/μL, glucose <40 mg/dL
- Viral meningitis: 10-500 WBC/μL, normal glucose
- Opening pressure: >300 mmH2O suggests bacterial etiology
- Protein elevation: >100 mg/dL in bacterial cases
- PCR sensitivity: >95% for viral pathogens
-
Respiratory Specimen Collection
- Nasopharyngeal swab: Optimal for viral PCR
- Sputum culture: Limited utility in young children
- Bronchoalveolar lavage: Reserved for severe cases
- Viral PCR panels: Detect 15-20 pathogens simultaneously
- Turnaround time: 2-4 hours for rapid results
- Cost-effectiveness: Reduces antibiotic use 20-30%
Rapid Diagnostic Technologies: Point-of-Care Precision
Modern rapid diagnostics enable immediate clinical decision-making with high accuracy and improved patient outcomes:
-
Multiplex PCR Panels
- Respiratory panels: 15-20 pathogens in 2-4 hours
- Gastrointestinal panels: 20+ enteric pathogens simultaneously
- Meningitis panels: Bacterial, viral, fungal detection
- Sensitivity: >95% for included pathogens
- Specificity: >98% with minimal cross-reactivity
- Clinical impact: ↓antibiotic use 25%, ↓length of stay 1-2 days
-
Biomarker-Based Testing
- Procalcitonin: Results in 20 minutes
- CRP: Point-of-care testing available
- Lactate: Sepsis severity assessment
- PCT-guided therapy: ↓antibiotic duration 2-3 days
- CRP monitoring: Treatment response assessment
- Combined approach: Optimal diagnostic accuracy
💡 Master This: Diagnostic stewardship principles - use narrow-spectrum testing for specific clinical questions, broad panels for undifferentiated illness, and biomarkers for treatment decisions to optimize accuracy while controlling costs
| Test Category | Turnaround Time | Sensitivity | Specificity | Clinical Application |
|---|---|---|---|---|
| Blood Culture | 24-48 hours | >95% | >98% | Bacteremia detection |
| PCR Panels | 2-4 hours | >95% | >98% | Viral identification |
| Rapid Antigen | 15-30 minutes | 50-80% | >95% | Point-of-care screening |
| Procalcitonin | 20 minutes | 85% | 90% | Bacterial vs viral |
| CRP | 10 minutes | 80% | 75% | Inflammatory response |
🔬 Diagnostic Precision Matrix: Evidence-Based Clinical Decision Making
⚖️ Treatment Algorithm Mastery: Evidence-Based Therapeutic Precision
Antibiotic Selection Matrix: Pathogen-Directed Precision
Optimal antibiotic selection requires systematic matching of pathogen susceptibility patterns with patient-specific factors and local resistance data:
-
First-Line Empiric Choices
- Community-acquired pneumonia: Amoxicillin 90 mg/kg/day
- Skin/soft tissue: Clindamycin 30-40 mg/kg/day
- Urinary tract infection: Cephalexin 50-100 mg/kg/day
- Amoxicillin resistance: S. pneumoniae 15-25% in most regions
- High-dose strategy: Overcomes intermediate resistance
- Duration optimization: 5-7 days for uncomplicated infections
-
Severe Infection Protocols
- Suspected meningitis: Ceftriaxone 100 mg/kg/day + Vancomycin
- Sepsis syndrome: Ceftriaxone + Clindamycin for toxin suppression
- Necrotizing infections: Clindamycin + Penicillin G
- Vancomycin indications: MRSA risk >10% in community
- Clindamycin benefit: Toxin production inhibition
- Combination rationale: Synergistic bacterial killing
-
Resistance-Guided Modifications
- MRSA coverage: Vancomycin or Linezolid based on MIC
- ESBL producers: Meropenem for serious infections
- Pseudomonas risk: Cefepime or Piperacillin-tazobactam
- Local antibiograms: Guide empiric choices
- De-escalation strategy: Narrow spectrum after culture results
- Duration limits: Shortest effective course
📌 Remember: SMART antibiotic prescribing - Specific pathogen targeting, Minimal effective duration, Antibiogram-guided selection, Resistance prevention, Toxicity monitoring
⭐ Clinical Pearl: High-dose amoxicillin (90 mg/kg/day) achieves >90% cure rates for pneumococcal pneumonia, including intermediate-resistant strains with MIC ≤2 μg/mL
Dosing Optimization: Pharmacokinetic Precision
Pediatric antibiotic dosing requires age-specific adjustments based on developmental pharmacokinetics and infection severity:
-
Age-Based Dosing Adjustments
- Neonates (0-28 days): ↓clearance, extended intervals
- Infants (1-12 months): ↑clearance per kg, higher doses
- Children (1-12 years): Adult-equivalent mg/kg dosing
- Renal maturation: Adult GFR achieved by 2 years
- Hepatic metabolism: Adult capacity by 6-12 months
- Protein binding: Adult levels by 12 months
-
Severity-Adjusted Dosing
- Meningitis doses: 2-3x higher for CNS penetration
- Severe pneumonia: Maximum recommended doses
- Sepsis syndrome: Loading doses for rapid levels
- CNS penetration: 10-20% of serum levels for most antibiotics
- Tissue distribution: Higher doses needed for deep infections
- Therapeutic monitoring: Vancomycin levels, aminoglycoside levels
-
Renal Function Considerations
- Creatinine clearance: Adjust nephrotoxic drugs
- Fluid status: Affects distribution volume
- Concurrent medications: Drug interactions
- Nephrotoxic combinations: Avoid when possible
- Dose adjustments: Based on calculated clearance
- Monitoring frequency: Daily in severe illness
💡 Master This: Therapeutic drug monitoring is essential for vancomycin (target trough 10-15 μg/mL), aminoglycosides (peak 5-10 μg/mL), and linezolid in prolonged therapy to optimize efficacy while minimizing toxicity
| Antibiotic | Standard Dose | Severe Infection | Meningitis Dose | Monitoring Required |
|---|---|---|---|---|
| Amoxicillin | 45 mg/kg/day | 90 mg/kg/day | Not recommended | Clinical response |
| Ceftriaxone | 50 mg/kg/day | 100 mg/kg/day | 100 mg/kg/day | Clinical response |
| Vancomycin | 40 mg/kg/day | 60 mg/kg/day | 60 mg/kg/day | Trough levels |
| Clindamycin | 30 mg/kg/day | 40 mg/kg/day | 40 mg/kg/day | Liver function |
| Meropenem | 60 mg/kg/day | 120 mg/kg/day | 120 mg/kg/day | Renal function |
Optimal treatment duration balances clinical cure with resistance prevention and adverse effect minimization:
-
Uncomplicated Infections
- Pneumonia: 5-7 days for typical pathogens
- Skin infections: 5-7 days for cellulitis
- UTI: 7-10 days for first episode
- Shorter courses: Equal efficacy with ↓resistance
- Clinical stability: 48-72 hours before step-down
- Biomarker guidance: CRP normalization supports discontinuation
-
Complicated Infections
- Bacteremia: 7-10 days after blood culture clearance
- Meningitis: 10-14 days for bacterial causes
- Osteomyelitis: 4-6 weeks total therapy
- Source control: Essential for cure
- Clinical markers: Fever resolution, improved appetite
- Laboratory trends: Normalizing inflammatory markers
-
Biomarker-Guided Duration
- Procalcitonin: <0.25 ng/mL supports discontinuation
- CRP: <20 mg/L indicates treatment response
- Clinical stability: 24-48 hours before stopping
- PCT-guided therapy: ↓duration 2-3 days safely
- Combined approach: Clinical + biomarker assessment
- Safety monitoring: 48-72 hours post-discontinuation
Evidence-based treatment algorithms optimize clinical outcomes while minimizing resistance development and adverse effects. Connect these therapeutic principles through systematic monitoring approaches to achieve comprehensive infectious disease mastery.
⚖️ Treatment Algorithm Mastery: Evidence-Based Therapeutic Precision
🔗 Multi-System Integration Hub: Infectious Disease Interconnections
Cardiovascular-Infectious Interface: The Hemodynamic Cascade
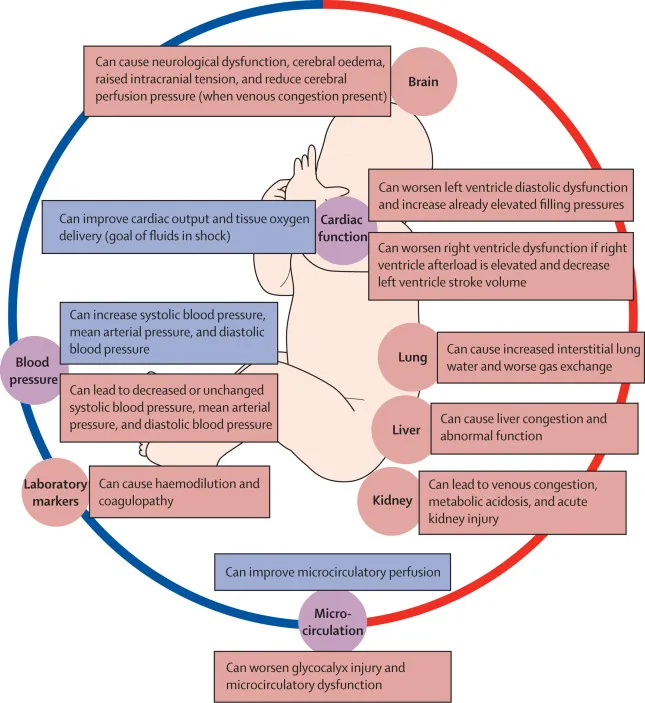
Infectious diseases profoundly impact cardiovascular function through direct pathogen effects and inflammatory mediator release:
-
Sepsis-Induced Cardiomyopathy
- Incidence: 40-50% of pediatric septic shock cases
- Mechanism: Cytokine-mediated myocardial depression
- Recovery timeline: 7-10 days with supportive care
- Ejection fraction: ↓30-50% during acute phase
- Troponin elevation: Present in 85% of severe cases
- Inotropic support: Required in 60% of shock patients
-
Endocarditis Complications
- Vegetation formation: S. aureus most aggressive
- Embolic events: 20-30% of cases
- Heart failure: Acute valve destruction
- Echocardiography: Sensitivity >95% for vegetations
- Blood culture: 3 sets before antibiotic therapy
- Surgical intervention: Required in 25-30% of cases
-
Pericarditis Syndromes
- Viral etiology: 80-90% of pediatric cases
- Bacterial causes: S. pneumoniae, S. aureus
- Constrictive risk: <5% in viral pericarditis
- ECG changes: Diffuse ST elevation in acute phase
- Pericardial friction rub: Present in 60% of cases
- Effusion development: Requires serial monitoring
📌 Remember: SHOCK for sepsis cardiovascular effects - Systemic vasodilation, Heart failure, Organ hypoperfusion, Capillary leak, Kinetic circulation changes
⭐ Clinical Pearl: Pediatric septic shock requires fluid resuscitation 20 mL/kg within first hour, followed by inotropic support if perfusion remains inadequate - mortality increases 40% with each hour of delay
Neurologic-Infectious Convergence: The CNS Vulnerability Matrix
Central nervous system infections represent medical emergencies requiring immediate recognition and intervention:
-
Bacterial Meningitis Pathophysiology
- Blood-brain barrier disruption: Inflammatory cascade
- Cerebral edema: Cytotoxic and vasogenic components
- Intracranial pressure: ↑ICP in 60% of cases
- Mortality rates: 5-10% with optimal treatment
- Neurologic sequelae: 15-25% of survivors
- Hearing loss: Most common long-term complication
-
Encephalitis Syndromes
- Viral causes: HSV, EBV, influenza predominate
- Autoimmune: Anti-NMDA receptor encephalitis
- Diagnostic approach: CSF PCR and MRI imaging
- HSV encephalitis: Temporal lobe predilection
- Treatment window: Acyclovir within 24 hours
- Outcome correlation: Early treatment improves prognosis
-
Post-Infectious Complications
- Acute disseminated encephalomyelitis: Demyelinating process
- Guillain-Barré syndrome: Ascending paralysis
- PANDAS: Streptococcal-associated neuropsychiatric symptoms
- ADEM incidence: 1:1000 viral infections
- GBS recovery: 80-90% complete recovery
- PANDAS criteria: Temporal association with strep infection
Immunologic-Infectious Dynamics: The Host Response Spectrum
Understanding immune system responses to infection enables prediction of disease severity and therapeutic intervention:
-
Cytokine Storm Syndrome
- Pathophysiology: Uncontrolled inflammatory response
- Clinical markers: Ferritin >500, IL-6 elevation
- Mortality risk: 20-30% without intervention
- Hemophagocytic lymphohistiocytosis: Secondary HLH
- Treatment approach: Immunosuppression with steroids
- Monitoring parameters: Ferritin, LDH, triglycerides
-
Immunodeficiency Considerations
- Primary immunodeficiency: Recurrent severe infections
- Secondary causes: Malnutrition, medications
- Opportunistic pathogens: Unusual organisms
- Warning signs: >8 infections per year
- Severity markers: Hospitalization required
- Family history: Early deaths, consanguinity
-
Vaccine-Preventable Disease Resurgence
- Measles outbreaks: Vaccination gaps
- Pertussis cycles: Waning immunity
- Pneumococcal disease: Serotype replacement
- Herd immunity thresholds: >95% for measles
- Vaccine effectiveness: >90% for most vaccines
- Breakthrough infections: Milder disease in vaccinated
💡 Master This: Multi-system organ failure in pediatric sepsis follows predictable patterns - respiratory failure (first 24 hours), cardiovascular shock (24-48 hours), renal dysfunction (48-72 hours), neurologic changes (72+ hours) - early recognition enables proactive intervention
| System | Early Changes (0-24h) | Progressive Changes (24-72h) | Late Changes (>72h) | Intervention Window |
|---|---|---|---|---|
| Cardiovascular | Tachycardia, ↓BP | Shock, ↓cardiac output | Cardiomyopathy | First 6 hours |
| Respiratory | Tachypnea, ↓O2 sat | ARDS, ventilator need | Pulmonary fibrosis | First 12 hours |
| Neurologic | Altered mental status | Seizures, coma | Cerebral edema | First 24 hours |
| Renal | ↓urine output | Acute kidney injury | Dialysis requirement | First 48 hours |
| Hematologic | Thrombocytopenia | DIC, bleeding | Bone marrow failure | First 72 hours |
🔗 Multi-System Integration Hub: Infectious Disease Interconnections
🎯 Clinical Mastery Command Center: Rapid Decision Frameworks
The Essential Arsenal: Critical Numbers and Thresholds
Master these quantitative benchmarks for immediate clinical application:
-
Fever Thresholds by Age
- Neonates (0-28 days): >38.0°C requires full sepsis workup
- Infants (29-90 days): >38.5°C with risk stratification
- Children (>3 months): >39.0°C suggests bacterial infection
- Serious bacterial infection risk: 15% in neonates with fever
- Bacteremia probability: 3-5% in well-appearing febrile children
- Meningitis incidence: 0.2-0.4% in febrile children >3 months
-
Laboratory Decision Points
- WBC >15,000 or <5,000: Bacterial infection likely
- ANC >10,000: 85% sensitivity for bacterial cause
- CRP >40 mg/L: 80% specificity for bacterial infection
- Procalcitonin >0.5 ng/mL: 90% specificity for sepsis
- Combined markers: CRP + PCT achieves 95% accuracy
- Negative predictive value: PCT <0.25 rules out bacterial infection
- Trending values: More reliable than single measurements
-
Clinical Severity Indicators
- Respiratory rate: >60 (infants), >40 (children) suggests pneumonia
- Heart rate: >180 (infants), >140 (children) indicates distress
- Blood pressure: <70 + (2×age) defines hypotension
- Oxygen saturation: <92% requires immediate intervention
- Capillary refill: >3 seconds suggests poor perfusion
- Mental status: Altered consciousness indicates severe illness
📌 Remember: FEVER for rapid assessment - Focal signs, Elevated WBC, Vital sign abnormalities, Elevated inflammatory markers, Risk factors present
⭐ Clinical Pearl: Rochester Criteria identify low-risk febrile infants 29-90 days: well-appearing, WBC 5,000-15,000, <1,500 bands, normal urinalysis, no focal infection - negative predictive value >98%
Pattern Recognition Drill Framework
Systematic pattern recognition enables rapid diagnosis and appropriate intervention:
-
The "Sick vs Not Sick" Assessment
- Appearance: Alert, interactive vs lethargic, irritable
- Perfusion: Normal color vs mottled, pale
- Respiratory effort: Comfortable vs increased work
- Yale Observation Scale: Score >16 predicts serious illness
- Pediatric Assessment Triangle: Appearance, breathing, circulation
- Clinical gestalt: Experienced clinician assessment highly accurate
-
Pathogen-Specific Recognition Patterns
- "See petechiae, think meningococcus": Immediate blood culture
- "See barking cough, think croup": Dexamethasone indicated
- "See drooling + fever, think epiglottitis": Avoid throat examination
- Pattern reliability: >90% accuracy for classic presentations
- Atypical presentations: 15-20% of serious infections
- Age modifications: Patterns vary by developmental stage
-
Complication Prediction Models
- Pneumonia severity: CURB-65 modified for children
- Sepsis progression: qSOFA criteria adapted for pediatrics
- Meningitis outcomes: Glasgow Coma Scale on presentation
- Risk stratification: Guides disposition and monitoring intensity
- Early warning systems: Prevent clinical deterioration
- Resource allocation: ICU vs ward placement decisions
💡 Master This: The 6-Hour Rule - most serious bacterial infections declare themselves within 6 hours of presentation through vital sign changes, laboratory abnormalities, or clinical deterioration - systematic reassessment prevents missed diagnoses
| Clinical Scenario | Key Recognition Pattern | Immediate Action | Time-Sensitive Intervention |
|---|---|---|---|
| Febrile neonate | Poor feeding + lethargy | Full sepsis workup | Antibiotics within 1 hour |
| Petechial rash | Non-blanching + fever | Blood culture | Antibiotics within 30 minutes |
| Respiratory distress | Retractions + hypoxia | Oxygen support | Bronchodilators if wheeze |
| Altered mental status | Fever + neck stiffness | Lumbar puncture | Antibiotics + dexamethasone |
| Shock presentation | Tachycardia + poor perfusion | IV access | Fluid bolus 20 mL/kg |
These evidence-based principles guide optimal infectious disease management:
-
"Never delay antibiotics in suspected sepsis" - Each hour of delay increases mortality 7-10%
-
"Always obtain cultures before antibiotics" - When clinically feasible without compromising patient safety
-
"Narrow antibiotics based on culture results" - De-escalation within 48-72 hours prevents resistance
-
"Monitor treatment response systematically" - Clinical improvement expected within 48-72 hours
-
"Consider immunodeficiency in recurrent infections" - >8 infections per year warrants evaluation
⭐ Clinical Pearl: The Golden Hour principle applies to pediatric sepsis - recognition, resuscitation, and antibiotics within 60 minutes of presentation achieves optimal survival rates and minimal long-term sequelae
These rapid decision frameworks transform clinical uncertainty into systematic excellence, enabling optimal patient outcomes through evidence-based precision and timely intervention.
🎯 Clinical Mastery Command Center: Rapid Decision Frameworks
Practice Questions: Infectious Disease
Test your understanding with these related questions
An 18-month-old boy presents to the emergency department for malaise. The boy’s parents report worsening fatigue for 3 days with associated irritability and anorexia. The patient’s newborn screening revealed a point mutation in the beta-globin gene but the patient has otherwise been healthy since birth. On physical exam, his temperature is 102.4°F (39.1°C), blood pressure is 78/42 mmHg, pulse is 124/min, and respirations are 32/min. The child is tired-appearing and difficult to soothe. Laboratory testing is performed and reveals the following: Serum: Na+: 137 mEq/L Cl-: 100 mEq/L K+: 4.4 mEq/L HCO3-: 24 mEq/L Urea nitrogen: 16 mg/dL Creatinine: 0.9 mg/dL Glucose: 96 mg/dL Leukocyte count: 19,300/mm^3 with normal differential Hemoglobin: 7.8 g/dL Hematocrit: 21% Mean corpuscular volume: 82 um^3 Platelet count: 324,000/mm^3 Reticulocyte index: 3.6% Which of the following is the most likely causative organism for this patient's presentation?












