Tall stature evaluation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Tall stature evaluation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Tall stature evaluation US Medical PG Question 1: A 15-year-old girl comes to the physician with her father for evaluation of her tall stature. She is concerned because she is taller than all of her friends. Her birth weight and height were within normal limits. Her father is 174 cm (5 ft 7 in) tall; her mother is 162 cm (5 ft 3 in) tall. She is at the 98th percentile for height and 90th percentile for BMI. She has not had her menstrual period yet. Her mother has Graves disease. Vital signs are within normal limits. Examination shows a tall stature with broad hands and feet. There is frontal bossing and protrusion of the mandible. Finger perimetry is normal. The remainder of the examinations shows no abnormalities. Serum studies show a fasting serum glucose of 144 mg/dL. An x-ray of the left hand and wrist shows a bone age of 15 years. Which of the following is the most appropriate definitive treatment for this patient's condition?
- A. Caloric restriction
- B. Letrozole therapy
- C. Methimazole therapy
- D. Transsphenoidal adenomectomy (Correct Answer)
- E. Leuprolide therapy
Tall stature evaluation Explanation: ***Transsphenoidal adenomectomy***
- The patient's clinical presentation, including **tall stature with broad hands and feet**, frontal bossing, mandibular prognathism, primary amenorrhea, and elevated fasting glucose, is highly suggestive of **gigantism** (growth hormone excess before epiphyseal closure) due to a **GH-secreting pituitary adenoma**.
- **Transsphenoidal adenomectomy** is the **definitive treatment** to surgically remove the GH-secreting tumor, thereby normalizing GH levels and preventing further progression of gigantism.
- This is the most appropriate treatment to address the **underlying cause** and halt disease progression.
*Caloric restriction*
- While caloric restriction might impact overall growth, it is not a treatment for a hormonally driven condition like **gigantism** caused by a pituitary adenoma.
- It would not address the underlying **excess growth hormone production** or prevent the associated physical changes and metabolic complications.
*Letrozole therapy*
- **Letrozole** is an **aromatase inhibitor** used primarily in the treatment of estrogen-dependent breast cancer and sometimes to induce ovulation or delay puberty in tall stature from other causes.
- It does not directly target or reduce **growth hormone secretion** from a pituitary adenoma and is not appropriate for treating gigantism.
*Methimazole therapy*
- **Methimazole** is an **antithyroid medication** used to treat hyperthyroidism by reducing thyroid hormone production.
- While the patient's mother has Graves' disease, this patient's symptoms are not indicative of thyroid dysfunction, and methimazole would not treat **GH excess** from a pituitary adenoma.
*Leuprolide therapy*
- **Leuprolide** is a **GnRH agonist** used to suppress puberty (e.g., in central precocious puberty) or for hormone-sensitive cancers.
- It primarily affects the **hypothalamic-pituitary-gonadal axis** and has no direct role in treating **growth hormone excess** from a pituitary adenoma.
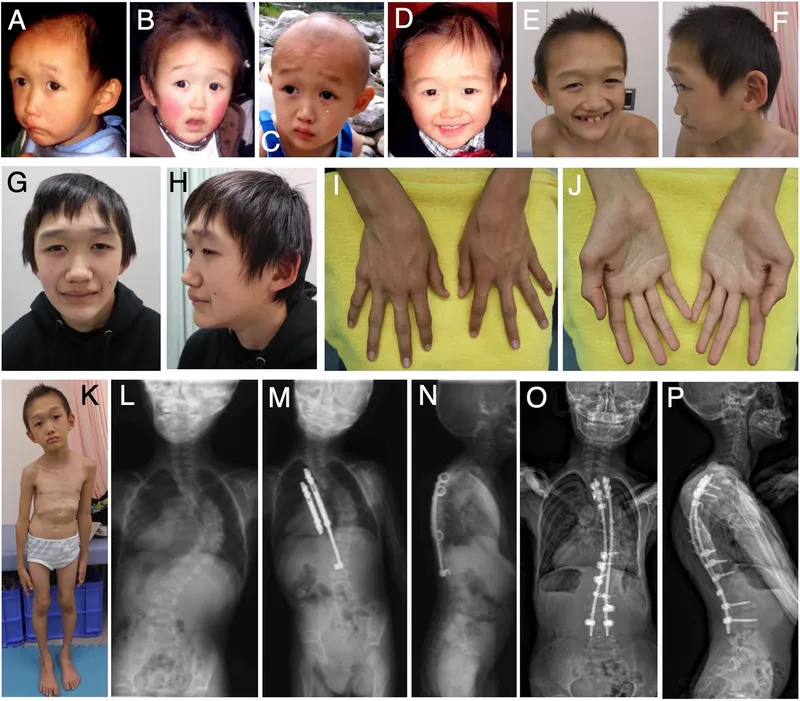
Tall stature evaluation US Medical PG Question 2: A 3-year-old male presents with his parents to a pediatrician for a new patient visit. The child was recently adopted and little is known about his prior medical or family history. The parents report that the child seems to be doing well, but they are concerned because the patient is much larger than any of the other 3-year-olds in his preschool class. They report that he eats a varied diet at home, and that they limit juice and snack foods. On physical exam, the patient is in the 73rd percentile for weight, 99th percentile for height, and 86th percentile for head circumference. He appears mildly developmentally delayed. He has a fair complexion and tall stature with a prominent sternum. The patient also has joint hypermobility and hyperelastic skin. He appears to have poor visual acuity and is referred to an ophthalmologist, who diagnoses upward lens subluxation of the right eye.
This child is most likely to develop which of the following complications?
- A. Osteoarthritis
- B. Wilms tumor
- C. Medullary thyroid cancer
- D. Aortic dissection (Correct Answer)
- E. Thromboembolic stroke
Tall stature evaluation Explanation: ***Aortic dissection***
- The constellation of **tall stature**, **prominent sternum**, **joint hypermobility**, **hyperelastic skin**, and **upward lens subluxation (ectopia lentis)** in a young child strongly suggests **Marfan syndrome**.
- **Aortic root dilation** and subsequent **aortic dissection** are the most serious cardiovascular complications in Marfan syndrome due to weakened connective tissue in the aortic wall caused by **fibrillin-1 deficiency**.
- This is the **leading cause of mortality** in untreated Marfan syndrome.
*Osteoarthritis*
- While joint hypermobility can contribute to **joint instability** and accelerate degenerative changes, typical **osteoarthritis** is less common as a primary, severe complication in childhood Marfan syndrome.
- Early-onset, severe osteoarthritis is not the major life-threatening complication associated with Marfan syndrome at this age.
*Wilms tumor*
- **Wilms tumor** is a type of kidney cancer typically associated with syndromes like **WAGR (Wilms tumor, Aniridia, Genitourinary anomalies, intellectual disability)** or **Beckwith-Wiedemann syndrome**, none of which fit the patient's presentation.
- There is no known direct association between Wilms tumor and Marfan syndrome.
*Medullary thyroid cancer*
- **Medullary thyroid cancer** is a feature of **Multiple Endocrine Neoplasia type 2 (MEN 2) syndromes**, which also present with pheochromocytomas and parathyroid hyperplasia.
- The clinical features described in the patient are not consistent with MEN 2.
*Thromboembolic stroke*
- While Marfan syndrome can lead to cardiovascular issues, a **thromboembolic stroke** is not a primary or characteristic complication, especially in comparison to the high risk of aortic dissection.
- The main vascular pathology in Marfan is related to connective tissue weakness, not primarily hypercoagulability or mural thrombi leading to stroke.
- Thromboembolic complications are more characteristic of **homocystinuria**, which presents with **downward** lens subluxation.
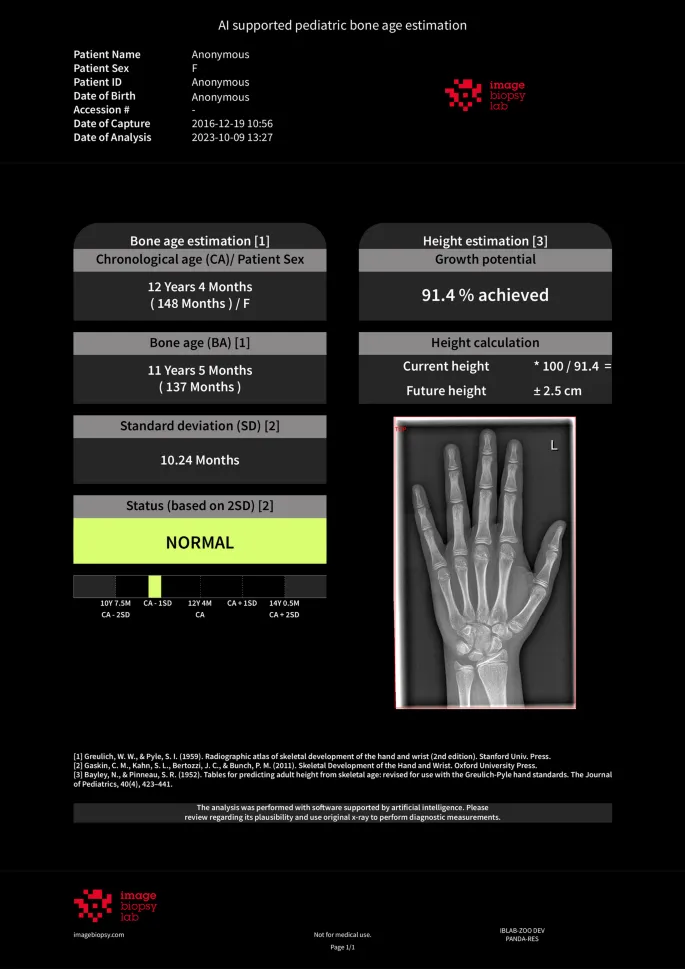
Tall stature evaluation US Medical PG Question 3: A 15-year-old girl comes to the physician with her father for evaluation of short stature. She feels well overall but is concerned because all of her friends are taller than her. Her birth weight was normal. Menarche has not yet occurred. Her father says he also had short stature and late puberty. The girl is at the 5th percentile for height and 35th percentile for weight. Breast development is Tanner stage 2. Pubic and axillary hair is absent. An x-ray of the left hand and wrist shows a bone age of 12 years. Further evaluation of this patient is most likely to show which of the following sets of laboratory findings?
- A. High FSH, High LH, Normal Estradiol, Normal Prolactin
- B. Normal FSH, Normal LH, Normal Estradiol, Normal Prolactin
- C. Normal FSH, Normal LH, Low Estradiol, Normal Prolactin
- D. Low-normal FSH, Low-normal LH, Low Estradiol, Normal Prolactin (Correct Answer)
- E. Low FSH, Low LH, Low Estradiol, Normal Prolactin
Tall stature evaluation Explanation: ***Low-normal FSH, Low-normal LH, Low Estradiol, Normal Prolactin***
- This pattern is characteristic of **constitutional delay of growth and puberty (CDGP)**, where the hypothalamic-pituitary-gonadal (HPG) axis has not yet fully matured, resulting in low-normal gonadotropins and low estradiol.
- The key clinical features supporting CDGP include: **delayed bone age** (12 years vs chronologic age 15), **positive family history** of late puberty, normal growth velocity, and absence of pathological findings.
- In CDGP, gonadotropins are in the **low-normal or prepubertal range** but will eventually rise spontaneously as the HPG axis matures, distinguishing this from permanent hypogonadotropic hypogonadism.
- GnRH stimulation testing would show a pubertal (not prepubertal) response, confirming the functional delay rather than a pathologic deficiency.
*Low FSH, Low LH, Low Estradiol, Normal Prolactin*
- This pattern suggests **hypogonadotropic hypogonadism**, such as Kallmann syndrome or functional hypothalamic amenorrhea, where gonadotropins are frankly low (not just low-normal).
- While this also presents with low estradiol and delayed puberty, patients with hypogonadotropic hypogonadism typically lack the **positive family history** and would not show delayed bone age suggesting growth potential.
- The distinction is that in permanent hypogonadotropic hypogonadism, the HPG axis is deficient and will not mature spontaneously without hormonal treatment.
*High FSH, High LH, Normal Estradiol, Normal Prolactin*
- This combination is inconsistent with delayed puberty, as high gonadotropins indicate **hypergonadotropic hypogonadism** (primary ovarian failure such as Turner syndrome).
- Hypergonadotropic hypogonadism presents with **high FSH/LH and low estradiol** (not normal), as the pituitary attempts to stimulate non-responsive ovaries.
- This patient's delayed bone age and family history make a physiologic delay (CDGP) much more likely than ovarian failure.
*Normal FSH, Normal LH, Normal Estradiol, Normal Prolactin*
- **Normal estradiol** at age 15 would indicate that puberty is progressing appropriately, which contradicts this patient's clinical presentation.
- The patient has delayed menarche, absent pubic/axillary hair, only Tanner stage 2 breast development, and bone age of 12 years - all indicating **low estradiol** and delayed pubertal progression.
- If all hormones were normal, we would expect more advanced pubertal development at this age.
*Normal FSH, Normal LH, Low Estradiol, Normal Prolactin*
- While low estradiol correctly reflects delayed puberty, describing FSH and LH as fully "normal" is imprecise for CDGP.
- In CDGP, gonadotropins are characteristically in the **low-normal or prepubertal range**, not at robust normal adult levels, reflecting the immature but eventually functional HPG axis.
- The distinction between "normal" and "low-normal" gonadotropins is clinically important for differentiating constitutional delay from other causes of delayed puberty.
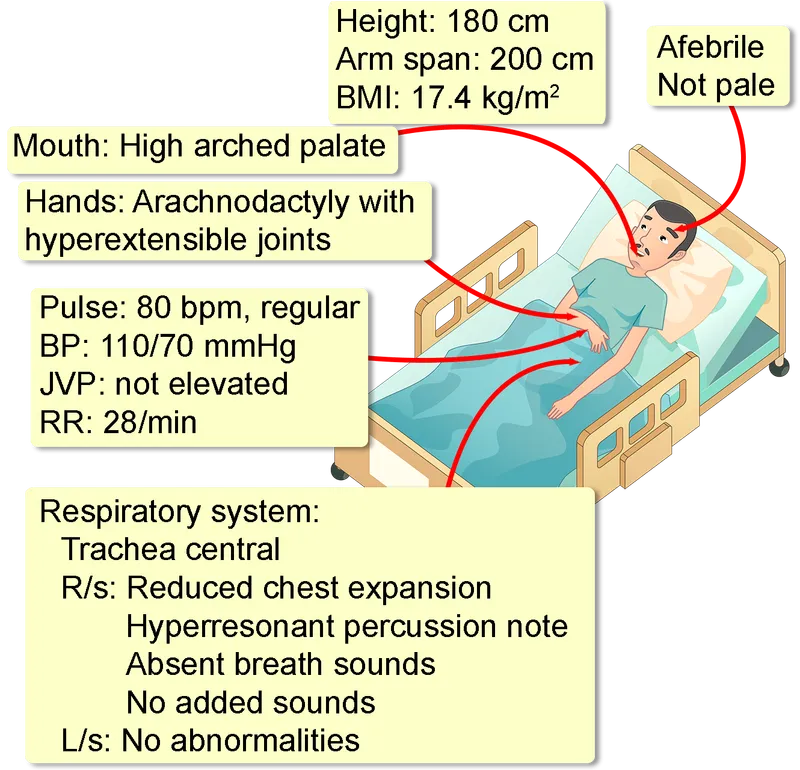
Tall stature evaluation US Medical PG Question 4: A 14-year-old boy is brought to the physician because of blurry vision. He is at the 97th percentile for height and 25th percentile for weight. He has long, slender fingers and toes that are hyperflexible. Examination of the oropharynx shows a high-arched palate. Slit lamp examination shows bilateral lens subluxation in the superotemporal direction. The patient's older sister is also tall and has hyperflexible joints. However, she does not have lens subluxation or an arched palate. Which of the following genetic principles accounts for the phenotypical differences seen in this pair of siblings?
- A. Incomplete penetrance
- B. Frameshift mutation
- C. Compound heterozygosity
- D. Variable expressivity (Correct Answer)
- E. Chromosomal instability
Tall stature evaluation Explanation: ***Variable expressivity***
- This principle accounts for the **range of phenotypes** observed among individuals who carry the same genetic mutation, as seen in the siblings with Marfan syndrome.
- Both siblings likely have the same genetic defect (e.g., in the *FBN1* gene), but express different combinations and severity of symptoms.
*Incomplete penetrance*
- This occurs when individuals with a specific genotype **do not always express** the associated phenotype.
- In this case, both siblings *do* express some features of Marfan syndrome, indicating that the gene is penetrant in both.
*Frameshift mutation*
- A frameshift mutation is a type of **gene mutation** caused by indels (insertions or deletions) of a number of nucleotides not divisible by three.
- While a frameshift mutation could be the underlying cause of Marfan syndrome, it does not explain the *phenotypical differences* between two individuals with the same underlying genetic defect.
*Compound heterozygosity*
- This describes a situation where an individual has **two different mutant alleles** at the same gene locus, one on each chromosome.
- While relevant to some genetic disorders, it does not explain the phenotypic variability between two siblings who inherited the same underlying genetic susceptibility.
*Chromosomal instability*
- This refers to a high rate of **chromosome rearrangements** or aneuploidy (abnormal chromosome number) within cells.
- While it can lead to various medical conditions, it is not the mechanism primarily responsible for the varying phenotypes of a single-gene disorder like Marfan syndrome in different individuals.
Tall stature evaluation US Medical PG Question 5: A 14-year-old boy is brought to the physician by his parents for a well-child visit. The patient was born at 38 weeks' gestation via vaginal delivery and has been healthy. He attends a junior high school and is having difficulties keeping up with his classmates in many classes. He is at the 97th percentile for height and 50th percentile for weight. Vital signs are within normal limits. Cardiac examination shows a high-frequency midsystolic click that is best heard at the left fifth intercostal space. The patient has long extremities along with excess breast tissue bilaterally. He has no axillary hair. Genital examination shows reduced scrotal size and a normal sized penis. Which of the following tests is the most likely to diagnose the patient's underlying disorder?
- A. Urinalysis
- B. Southern blot
- C. Slit-lamp examination
- D. Karyotyping (Correct Answer)
- E. Serum IGF-1 measurement
Tall stature evaluation Explanation: ***Karyotyping***
- The patient's presentation with **tall stature**, **long extremities**, **gynecomastia**, **small testes**, and **learning difficulties** is highly suggestive of **Klinefelter syndrome (47,XXY)**.
- **Karyotyping** is the definitive diagnostic test for Klinefelter syndrome as it identifies the presence of an extra X chromosome.
*Urinalysis*
- This test is used to detect various kidney and urinary tract conditions and would not identify a **chromosomal abnormality**.
- While it can reveal issues like **proteinuria** or **hematuria**, these are not consistent with the primary presenting symptoms.
*Southern blot*
- This technique detects specific **DNA sequences** and is used for conditions like **fragile X syndrome** or **gene deletions**, but it is not the primary diagnostic tool for **aneuploidies** like Klinefelter syndrome.
- Karyotyping provides a broader overview of the entire **chromosome set**, which is necessary to identify an extra chromosome.
*Slit-lamp examination*
- This examination is used to visualize the eyes and is relevant for conditions like **Marfan syndrome** (**ectopia lentis**) or other ocular abnormalities, which are not the primary concern here.
- There are no symptoms presented that would suggest the need for a **slit-lamp examination**.
*Serum IGF-1 measurement*
- **Insulin-like growth factor 1 (IGF-1)** is measured to assess **growth hormone levels** and diagnose conditions like **acromegaly** or **dwarfism**.
- While the patient is tall, his other features (gynecomastia, small testes, learning difficulties) point strongly to a **chromosomal disorder** rather than a primary growth hormone abnormality.
Tall stature evaluation US Medical PG Question 6: A 15-year-old boy is brought to the physician by his mother for a well-child examination. He recently stopped attending his swim classes. The patient is at the 97th percentile for height and the 50th percentile for weight. Examination shows decreased facial hair, bilateral breast enlargement, and long extremities. Genital examination shows scant pubic hair, small testes, and a normal-sized penis. Further evaluation is most likely to show which of the following karyotypes?
- A. 45,XO/46,XX
- B. 45,XO
- C. 47,XYY
- D. 46,XX/46,XY
- E. 47,XXY (Correct Answer)
Tall stature evaluation Explanation: ***47,XXY***
- The patient's presentation with **tall stature**, **gynecomastia**, **small testes**, and **scant pubic hair** is characteristic of **Klinefelter syndrome**, which is caused by a **47,XXY karyotype**.
- **Hypogonadism** in Klinefelter syndrome leads to **decreased testosterone production**, explaining the lack of facial hair and undeveloped secondary sexual characteristics.
*45,XO/46,XX*
- This mosaic karyotype is associated with **Turner syndrome**, which primarily affects females and presents with features like **short stature**, **gonadal dysgenesis**, and **webbed neck**.
- Males with this karyotype are rare and would not exhibit the typical features described, such as **gynecomastia** and eunuchoid body habitus.
*45,XO*
- This is the classic karyotype for **Turner syndrome**, which is exclusively found in phenotypic females.
- Individuals with 45,XO present with **short stature**, **streak gonads**, and a lack of secondary sexual characteristics, none of which align with the male patient's symptoms.
*47,XYY*
- Individuals with **XYY syndrome** (Jacob syndrome) are typically **tall** but usually have **normal sexual development** and **fertility**.
- This karyotype does not explain the **gynecomastia**, **small testes**, or **decreased facial hair** seen in the patient.
*46,XX/46,XY*
- This karyotype indicates **gonadal mosaicism**, also known as **ovotesticular disorder of sex development (DSD)** or **chimerism**, where an individual has both ovarian and testicular tissue.
- While it can present with ambiguous genitalia and mixed secondary sexual characteristics, the specific constellation of **tall stature**, **gynecomastia**, and **small testes** is more indicative of Klinefelter syndrome.
Tall stature evaluation US Medical PG Question 7: A 15-year-old boy is brought to the clinic by his father for difficulty in school. He reports that his son has been suspended several times over his high school career for instigating fights. Per the patient, he has always had trouble controlling his anger and would feel especially frustrated at school since he has difficulty “keeping up.” His past medical history is unremarkable and he is up-to-date on all his vaccinations. A physical examination demonstrates a 6-foot tall teenage boy with severe acne vulgaris throughout his face and back. He is later worked up to have a chromosomal abnormality. What is the most likely explanation for this patient’s presentation?
- A. Klinefelter syndrome
- B. Down syndrome
- C. Fragile X syndrome
- D. Conduct disorder
- E. XYY syndrome (Correct Answer)
Tall stature evaluation Explanation: ***XYY syndrome***
- The patient's presentation of **tall stature**, severe **acne vulgaris**, learning difficulties, and behavioral problems like aggression and anger issues are characteristic features of **XYY syndrome**.
- This syndrome is due to the presence of an **extra Y chromosome**, often leading to increased testosterone levels and associated physical and behavioral phenotypes.
*Klinefelter syndrome*
- Characterized by **XXY karyotype**, leading to features like **tall stature**, small testes, **gynecomastia**, and often learning difficulties, but typically not severe acne or markedly aggressive behavior as the primary concern.
- Individuals with Klinefelter syndrome often have reduced fertility and hormonal imbalances that differ from those seen in XYY syndrome.
*Down syndrome*
- Caused by **trisomy 21** and presents with distinct facial features (**epicanthic folds**, flat nasal bridge), intellectual disability, and congenital heart defects, which are not described in this patient.
- Patients with Down syndrome are not typically known for excessive height or severe acne.
*Fragile X syndrome*
- This is an **X-linked genetic disorder** causing intellectual disability, characteristic long face, large ears, and macroorchidism, which are not mentioned in this patient's presentation.
- While behavioral issues can occur, the combination of tall stature and severe acne is not typical of Fragile X syndrome.
*Conduct disorder*
- This is a **behavioral disorder** characterized by a persistent pattern of violating the rights of others or major age-appropriate societal norms, fitting the description of instigating fights and difficulty in school.
- However, conduct disorder is a **diagnosis of exclusion** and does not account for the physical findings of tall stature, severe acne, or the underlying chromosomal abnormality that was later identified.
Tall stature evaluation US Medical PG Question 8: A 6-year-old girl is brought to the pediatrician by her father for an annual physical examination. The father reports that the patient is a happy and healthy child, but he sometimes worries about her weight. He says that she is a “picky” eater and only wants chicken nuggets and French fries. He also notes some mild acne on her cheeks and forehead but thinks it’s because she “doesn’t like baths.” The father says she has met all her pediatric milestones. She has recently started kindergarten, can tell time, and is beginning to read. Her teacher says she gets along with her classmates well. The patient was born at 38 weeks gestation. She has no chronic medical conditions and takes only a multivitamin. Height and weight are above the 95th percentile. Physical examination reveals scattered comedones on the patient’s forehead and bilateral cheeks. There is palpable breast tissue bilaterally with raised and enlarged areolae. Scant axillary hair and coarse pubic hair are also noted. A radiograph of the left hand shows a bone age of 9 years. Serum follicular stimulating hormone (FSH) level is 9.6 mU/mL (normal range 0.7-5.3 mU/mL) and luteinizing hormone (LH) level is 6.4 mU/mL (normal range < 0.26 mU/mL). Which of the following is the most appropriate diagnostic test?
- A. Pelvic ultrasound
- B. Estrogen levels
- C. 17-hydroxyprogesterone levels
- D. Dehydroepiandrosterone sulfate levels
- E. Brain magnetic resonance imaging (MRI) (Correct Answer)
Tall stature evaluation Explanation: ***Brain magnetic resonance imaging (MRI)***
- The constellation of **precocious puberty** (breast development, pubic and axillary hair, advanced bone age) and **elevated FSH and LH levels** in a 6-year-old girl indicates central precocious puberty, which is often caused by a CNS lesion.
- **Brain MRI is the gold standard imaging** to rule out **hypothalamic hamartomas**, **gliomas**, **craniopharyngiomas**, or other structural abnormalities of the **hypothalamic-pituitary axis**.
- MRI provides superior soft tissue resolution without radiation exposure, making it the preferred modality in children.
*Pelvic ultrasound*
- A pelvic ultrasound is primarily used to evaluate **gonadal tumors** or cysts in cases of **peripheral precocious puberty**, where FSH and LH levels would be suppressed.
- Given the elevated FSH and LH, the puberty is central (gonadotropin-dependent), making CNS imaging more appropriate than ovarian imaging.
*Estrogen levels*
- While estrogen levels would certainly be elevated in this patient, measuring them would confirm sexual precocity but would not differentiate between **central** and **peripheral precocious puberty**.
- The **elevated FSH and LH levels** already indicate active gonadal stimulation, making direct estrogen measurement less informative for pinpointing the etiology.
*17-hydroxyprogesterone levels*
- Elevated 17-hydroxyprogesterone levels are indicative of **congenital adrenal hyperplasia (CAH)**, particularly the 21-hydroxylase deficiency.
- CAH typically causes signs of **virilization** (e.g., clitoromegaly) but not breast development, and would not cause elevated FSH and LH levels.
*Dehydroepiandrosterone sulfate levels*
- Elevated DHEAS levels suggest an **adrenal source of androgens**, which could contribute to **pubic and axillary hair growth** (adrenarche).
- However, DHEAS elevation alone would not explain the **breast development** and **elevated gonadotropins**, which point towards central precocious puberty.
Tall stature evaluation US Medical PG Question 9: A 7-year-old boy is brought to the physician because his parents are concerned about his early sexual development. He has no history of serious illness and takes no medications. His brother was diagnosed with testicular cancer 5 years ago and underwent a radical orchiectomy. The patient is at the 85th percentile for height and 70th percentile for weight. Examination shows greasy facial skin. There is coarse axillary hair. Pubic hair development is at Tanner stage 3 and testicular development is at Tanner stage 2. The remainder of the examination shows no abnormalities. An x-ray of the wrist shows a bone age of 10 years. Basal serum luteinizing hormone and follicle-stimulating hormone are elevated. An MRI of the brain shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Leuprolide therapy (Correct Answer)
- B. Testicular ultrasound
- C. Cortisol supplementation
- D. Radiation therapy
- E. Observation
Tall stature evaluation Explanation: ***Leuprolide therapy***
- This patient presents with **central precocious puberty** (CPP), indicated by elevated **basal LH and FSH levels** in the context of advanced bone age, Tanner stage 3 pubic hair, and Tanner stage 2 testicular development at a young age.
- **Leuprolide** is a GnRH analog that, when given continuously, downregulates the pituitary's GnRH receptors, suppressing gonadotropin release and halting pubertal progression. This is the appropriate treatment for CPP.
*Testicular ultrasound*
- While useful for evaluating testicular size and consistency, it is typically performed when there is suspicion of **peripheral precocious puberty** (e.g., Leydig cell tumor) with low LH/FSH or significant testicular asymmetry, which is not the primary presentation here.
- The elevated basal LH and FSH values indicate a **central origin** of puberty, making a testicular ultrasound less immediately relevant as a *next step* compared to directly addressing the central hormonal drive.
*Cortisol supplementation*
- This would be indicated for conditions causing **adrenal insufficiency**, such as **congenital adrenal hyperplasia (CAH)** with salt-wasting or Addison's disease.
- CAH typically presents with virilization and advanced bone age but would show **low LH/FSH** (due to peripheral androgen excess) and elevated adrenal androgens (e.g., DHEA-S, 17-hydroxyprogesterone), which are not described.
*Radiation therapy*
- This is a treatment for **malignant tumors**, often used in cases of brain tumors.
- The MRI of the brain showed **no abnormalities**, ruling out a pituitary or hypothalamic tumor as the cause of CPP in this case, thus making radiation therapy inappropriate.
*Observation*
- **Observation** alone is inappropriate given the significant **advancement of bone age** (10 years in a 7-year-old) and clear signs of central precocious puberty.
- Untreated CPP can lead to **compromised adult height potential** due to premature epiphyseal fusion and psychosocial issues, necessitating intervention.
Tall stature evaluation US Medical PG Question 10: A 7-year-old girl is brought to the physician because of vaginal bleeding for 2 days. There is no personal or family history of serious illness. She is at the 95th percentile for height and at the 90th percentile for weight. Examination shows enlarged breasts, and the areola and papilla have formed a secondary mound. There is coarse pubic hair that does not extend to the inner thigh. The remainder of the examination show no abnormalities. An x-ray of the left hand and wrist shows a bone age of 11 years. Her serum luteinizing hormone concentration is 0.1 mIU/mL (N < 0.2 mIU/mL). Which of the following is the most appropriate next step in management?
- A. Serum dehydroepiandrosterone level
- B. Reassurance and follow-up
- C. Ultrasound of the pelvis
- D. GnRH stimulation test (Correct Answer)
- E. MRI of the brain
Tall stature evaluation Explanation: ***GnRH stimulation test***
- This patient presents with signs of **precocious puberty** (vaginal bleeding, enlarged breasts, pubic hair, advanced bone age) but a **low basal LH level**. A **GnRH stimulation test** is crucial to differentiate between **central (gonadotropin-dependent)** and **peripheral (gonadotropin-independent)** precocious puberty.
- A significant rise in LH after GnRH administration indicates **central precocious puberty**, while a lack of significant response suggests **peripheral precocious puberty**.
*Serum dehydroepiandrosterone level*
- **DHEA** is a precursor to androgens and its elevation might indicate **adrenal causes** of precocious puberty (e.g., congenital adrenal hyperplasia, adrenal tumor).
- However, the prominent signs of **breast development** and **vaginal bleeding** point more towards estrogen production, making a GnRH stimulation test a more direct and comprehensive initial step to evaluate the source of puberty.
*Reassurance and follow-up*
- Reassurance is inappropriate given the presence of **vaginal bleeding** and signs of **accelerated skeletal maturation** (bone age of 11 years at chronological age 7).
- These findings warrant further investigation to determine the underlying cause and initiate appropriate management to prevent complications like **compromised adult height**.
*Ultrasound of the pelvis*
- A **pelvic ultrasound** would be useful to evaluate for ovarian cysts or tumors, which can cause **peripheral precocious puberty**.
- However, the GnRH stimulation test is a **more critical first step** to determine whether the puberty is central or peripheral before focusing on specific peripheral etiologies.
*MRI of the brain*
- An **MRI of the brain** is indicated if **central precocious puberty** is confirmed by the GnRH stimulation test, especially in a young child, to rule out **hypothalamic or pituitary tumors** or other CNS lesions.
- Doing an MRI of the brain before establishing the type of precocious puberty (central vs. peripheral) is **premature** as it is only indicated for central causes.
More Tall stature evaluation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.