Short stature workup US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Short stature workup. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Short stature workup US Medical PG Question 1: A 10-year-old boy is brought to the physician by his parents for a follow-up examination. He has had a short stature since birth and underwent diagnostic testing. Genetic analyses showed a gain of function mutation in the fibroblast growth factor receptor 3 (FGFR3) gene. He has met all developmental milestones. He is at the 10th percentile for height and 90th percentile for weight. Which of the following additional findings is most likely on physical examination?
- A. Frontal bossing (Correct Answer)
- B. Absent collar bones
- C. Long extremities
- D. Blue sclerae
- E. Small genitalia
Short stature workup Explanation: ***Frontal bossing***
- A gain of function mutation in the **FGFR3 gene** is characteristic of **achondroplasia**, which is a common cause of short stature.
- **Frontal bossing** (prominent forehead) and midface hypoplasia are classical craniofacial features seen in individuals with achondroplasia.
*Absent collar bones*
- **Absent or hypoplastic clavicles** (collar bones) are a hallmark feature of **cleidocranial dysostosis**, a genetic disorder caused by mutations in the *RUNX2* gene, not typically associated with FGFR3 mutations.
- This condition also presents with delayed closure of fontanelles and dental anomalies, which are not suggested by the patient's presentation.
*Long extremities*
- Patients with achondroplasia characteristically have **rhizomelic short stature**, meaning the **proximal limbs** (femur and humerus) are disproportionately shorter than the trunk, leading to short extremities overall, not long ones.
- Long extremities are characteristic of conditions like **Marfan syndrome**, which has distinct genetic and clinical features.
*Blue sclerae*
- **Blue sclerae** are a common finding in **osteogenesis imperfecta**, a genetic disorder characterized by bone fragility due to defects in type I collagen synthesis.
- This condition is not caused by FGFR3 mutations and typically presents with recurrent fractures and other connective tissue abnormalities.
*Small genitalia*
- **Micropenis** (small genitalia) can be associated with various endocrine disorders, such as **hypogonadism** or congenital adrenal hyperplasia, or certain genetic syndromes.
- It is not a characteristic feature of achondroplasia or FGFR3-related skeletal dysplasias.
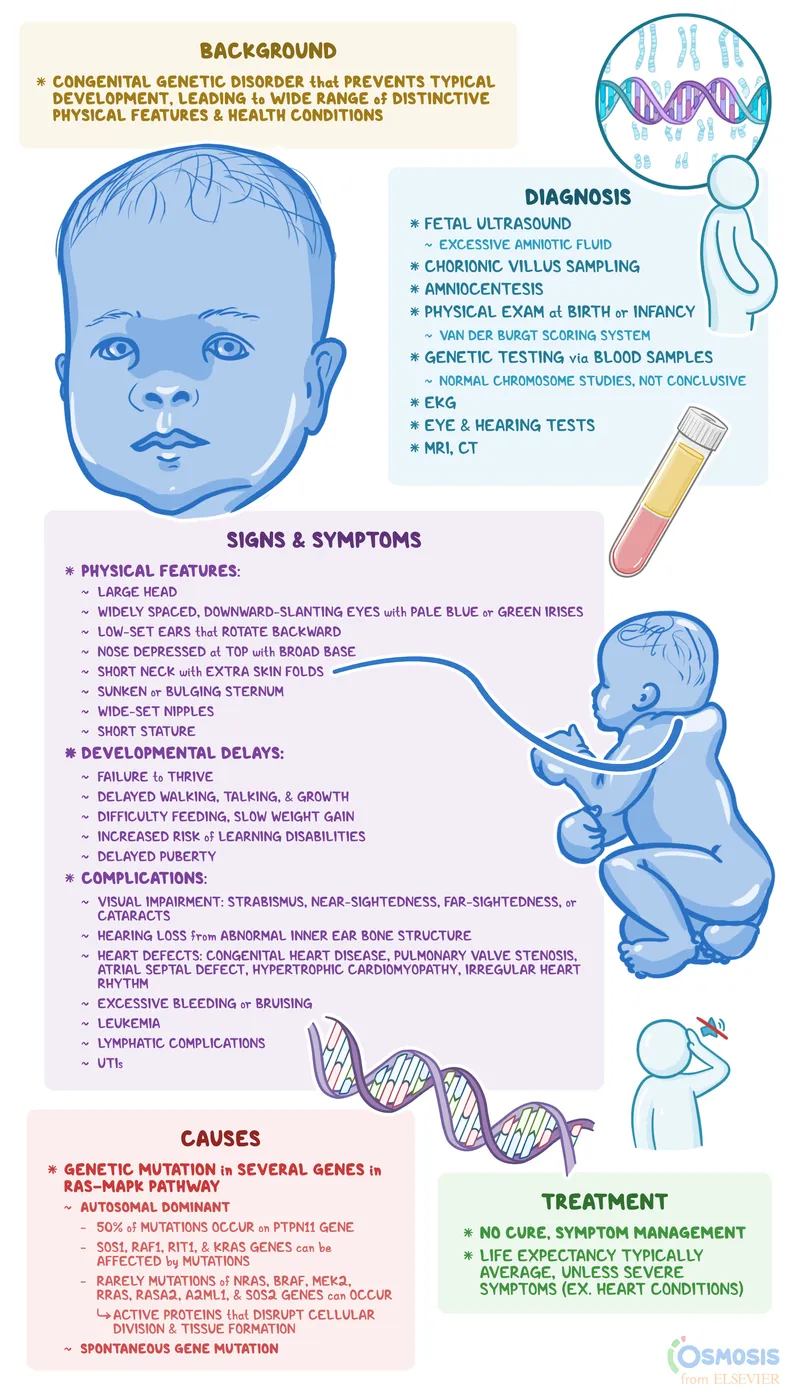
Short stature workup US Medical PG Question 2: A 6-year-old girl is brought to the physician by her parents because of concern that she is the shortest in her class. She has always been short for her age, but she is upset now that her classmates have begun teasing her for her height. She has no history of serious illness and takes no medications. She is 109 cm (3 ft 7 in) tall (10th percentile) and weighs 20 kg (45 lb) (50th percentile). Her blood pressure is 140/80 mm Hg. Vital signs are otherwise within normal limits. Physical examination shows a low-set hairline and a high-arched palate. Breast development is Tanner stage 1 and the nipples are widely spaced. Extremities are well perfused with strong peripheral pulses. Her hands are moderately edematous. This patient is at increased risk of developing which of the following complications?
- A. Precocious puberty
- B. Acute lymphoblastic leukemia
- C. Ectopia lentis
- D. Renal cell carcinoma
- E. Aortic insufficiency (Correct Answer)
Short stature workup Explanation: ***Aortic insufficiency***
- The patient's features, including **short stature**, **low-set hairline**, **widely spaced nipples**, **high-arched palate**, and **hand edema**, are classic for **Turner syndrome (45,XO)**.
- Individuals with Turner syndrome are at significantly increased risk of **cardiovascular anomalies**, particularly **bicuspid aortic valve** and **coarctation of the aorta**, which can both lead to **aortic insufficiency** and hypertension.
*Precocious puberty*
- **Precocious puberty** involves the premature onset of puberty, which is not suggested by the patient's **Tanner stage 1 breast development**, indicating **absent breast development**.
- Girls with Turner syndrome typically experience **delayed or absent puberty** due to gonadal dysgenesis and **ovarian failure**.
*Acute lymphoblastic leukemia*
- While chromosomal abnormalities can increase cancer risk, there is no strong, direct association between **Turner syndrome** and an increased risk of **acute lymphoblastic leukemia (ALL)** specifically.
- The presenting symptoms do not point towards hematological malignancy, which would involve signs like **fatigue**, **bruising**, or **recurrent infections**.
*Ectopia lentis*
- **Ectopia lentis**, or displaced lens, is a hallmark feature of conditions like **Marfan syndrome** and **homocystinuria**, not typically associated with Turner syndrome.
- There are no other features of connective tissue disorders presented in the patient's clinical picture.
*Renal cell carcinoma*
- While individuals with Turner syndrome can have a higher incidence of **renal anomalies**, such as **horseshoe kidney** or **duplex collecting systems**, there is no specific increased risk of **renal cell carcinoma** directly linked to the syndrome.
- The high blood pressure in this patient is more attributable to **cardiovascular defects** like coarctation of the aorta.
Short stature workup US Medical PG Question 3: A 19-year-old woman presents to her gynecologist’s office stating that she has never had a period. She is slightly alarmed because most of her friends in college have been menstruating for years. She is also concerned about her short stature. When she previously visited her family physician during early puberty, she was told that she will gain the appropriate height during her final teenage years. However, over the past few years, she has gained only a couple of inches. On examination, she has a wide chest and short neck. Her breast development is at Tanner stage 1. Her external genitalia is normal with sparse hair distribution over the mons pubis. Her gynecologist suspects a genetic condition and sends her for genetic counseling. Based on her clinical findings, which of the following diseases is she most likely to develop?
- A. Cystic medial necrosis
- B. Coarctation of aorta (Correct Answer)
- C. Supravalvular aortic stenosis
- D. Intellectual disability
- E. Endocardial cushion defects
Short stature workup Explanation: ***Coarctation of aorta***
- The patient's presentation with **primary amenorrhea**, **short stature**, a **wide chest**, and **short neck** are classic signs of **Turner syndrome (45, XO)**.
- **Coarctation of the aorta** is a common cardiovascular anomaly associated with Turner syndrome, occurring in approximately 10-20% of affected individuals.
*Cystic medial necrosis*
- This condition is associated with conditions like **Marfan syndrome** or **Ehlers-Danlos syndrome**, which present with different physical features, such as tall stature and joint hypermobility.
- While it can lead to aortic dissection, it is not a characteristic cardiovascular anomaly of Turner syndrome.
*Supravalvular aortic stenosis*
- This is a feature more commonly associated with **Williams syndrome**, which involves distinct facial features, intellectual disability, and a cheerful personality, none of which are described in this patient.
- It involves narrowing of the ascending aorta above the aortic valve, but is not typically linked to Turner syndrome.
*Intelligence disability*
- Patients with **Turner syndrome typically have normal intelligence**, although they may experience specific learning difficulties, particularly in visuospatial tasks.
- Significant intellectual disability is not a characteristic feature of this syndrome.
*Endocardial cushion defects*
- These defects, particularly **atrioventricular septal defects**, are classically associated with **Down syndrome (Trisomy 21)**.
- They are not a common cardiovascular defect seen in Turner syndrome.
Short stature workup US Medical PG Question 4: A 16-year-old teenager presents to the pediatrician with his mother. After she leaves the room he tells the physician that he is worried about puberty. All of his friends have had growth spurts, started building muscle mass, and their voices have changed while he still feels underdeveloped. The physician takes a complete history and performs a thorough physical examination. He goes through the patient’s past medical records and growth charts and notes physical findings documented over the last five years, concluding that the patient has delayed puberty. Which of the following findings supports his conclusion?
- A. The absence of testicular enlargement by age of 14 years (Correct Answer)
- B. The absence of an adult type of pubic hair distribution by age of 16 years
- C. The absence of linear growth acceleration by age of 13 years
- D. Presence of gynecomastia at age of 15 years
- E. The absence of penile enlargement by age of 12 years
Short stature workup Explanation: ***The absence of testicular enlargement by age of 14 years***
- The first reliable sign of male puberty is an increase in **testicular volume**, typically occurring by age 14.
- Absence of this by age 14 years indicates **delayed puberty** in males.
*The absence of an adult type of pubic hair distribution by age of 16 years*
- While pubic hair development is a sign of puberty, **adult-type distribution** (Tanner stage 5) by age 16 is normal for many.
- The definition of delayed puberty in males is typically based on the **absence of any secondary sexual characteristics** by age 14, or more specifically, testicular enlargement.
*The absence of linear growth acceleration by age of 13 years*
- The pubertal **growth spurt** typically occurs later in puberty, often around 13-14 years in males, following testicular enlargement.
- Its absence by age 13 might suggest early delay, but **testicular enlargement** is the primary diagnostic criterion.
*Presence of gynecomastia at age of 15 years*
- **Gynecomastia** can be a normal, transient finding during puberty due to temporary estrogen-androgen imbalance, not necessarily indicative of delayed puberty.
- Its presence doesn't rule out delayed puberty but isn't a direct sign of delay itself.
*The absence of penile enlargement by age of 12 years*
- **Penile enlargement** typically occurs after testicular enlargement.
- The absence of this by age 12 is less specific than **testicular enlargement by age 14** for defining delayed puberty.
Short stature workup US Medical PG Question 5: A 14-year-old boy is brought to the physician by his parents for a well-child visit. The patient was born at 38 weeks' gestation via vaginal delivery and has been healthy. He attends a junior high school and is having difficulties keeping up with his classmates in many classes. He is at the 97th percentile for height and 50th percentile for weight. Vital signs are within normal limits. Cardiac examination shows a high-frequency midsystolic click that is best heard at the left fifth intercostal space. The patient has long extremities along with excess breast tissue bilaterally. He has no axillary hair. Genital examination shows reduced scrotal size and a normal sized penis. Which of the following tests is the most likely to diagnose the patient's underlying disorder?
- A. Urinalysis
- B. Southern blot
- C. Slit-lamp examination
- D. Karyotyping (Correct Answer)
- E. Serum IGF-1 measurement
Short stature workup Explanation: ***Karyotyping***
- The patient's presentation with **tall stature**, **long extremities**, **gynecomastia**, **small testes**, and **learning difficulties** is highly suggestive of **Klinefelter syndrome (47,XXY)**.
- **Karyotyping** is the definitive diagnostic test for Klinefelter syndrome as it identifies the presence of an extra X chromosome.
*Urinalysis*
- This test is used to detect various kidney and urinary tract conditions and would not identify a **chromosomal abnormality**.
- While it can reveal issues like **proteinuria** or **hematuria**, these are not consistent with the primary presenting symptoms.
*Southern blot*
- This technique detects specific **DNA sequences** and is used for conditions like **fragile X syndrome** or **gene deletions**, but it is not the primary diagnostic tool for **aneuploidies** like Klinefelter syndrome.
- Karyotyping provides a broader overview of the entire **chromosome set**, which is necessary to identify an extra chromosome.
*Slit-lamp examination*
- This examination is used to visualize the eyes and is relevant for conditions like **Marfan syndrome** (**ectopia lentis**) or other ocular abnormalities, which are not the primary concern here.
- There are no symptoms presented that would suggest the need for a **slit-lamp examination**.
*Serum IGF-1 measurement*
- **Insulin-like growth factor 1 (IGF-1)** is measured to assess **growth hormone levels** and diagnose conditions like **acromegaly** or **dwarfism**.
- While the patient is tall, his other features (gynecomastia, small testes, learning difficulties) point strongly to a **chromosomal disorder** rather than a primary growth hormone abnormality.
Short stature workup US Medical PG Question 6: A 12-month-old boy is brought to the physician for a well-child examination. He was born at 38 weeks' gestation and was 48 cm (19 in) in length and weighed 3061 g (6 lb 12 oz); he is currently 60 cm (24 in) in length and weighs 7,910 g (17 lb 7 oz). He can walk with one hand held and can throw a small ball. He can pick up an object between his thumb and index finger. He can wave 'bye-bye'. He can say 'mama', 'dada' and 'uh-oh'. He cries if left to play with a stranger alone. Physical examination shows no abnormalities. Which of the following is most likely delayed in this child?
- A. Fine motor skills
- B. Language skills
- C. Growth (Correct Answer)
- D. Gross motor skills
- E. Social skills
Short stature workup Explanation: ***Growth***
- At 1 year of age, a child's **birth weight should triple**, and their **birth length should increase by 50%**.
- This child's birth weight was 3061 g (6 lb 12 oz), meaning his expected weight at 1 year should be around **9183 g (20 lb 4 oz)**, but he only weighs **7910 g (17 lb 7 oz)**, indicating **inadequate weight gain** (~1273 g below expected).
- This child's birth length was 48 cm (19 in), meaning his expected length at 1 year should be around **72 cm (28 in)**, but he is only **60 cm (24 in)**, indicating **poor linear growth** (12 cm below expected).
- Both **weight-for-age and length-for-age are delayed**, making growth the most likely delayed parameter.
*Fine motor skills*
- The child can **pick up an object between his thumb and index finger**, demonstrating a **pincer grasp**, which is an appropriate fine motor skill for a 12-month-old.
- He can also **throw a small ball**, further indicating age-appropriate fine motor development.
*Language skills*
- The child can say **'mama', 'dada'**, and **'uh-oh'**, which are appropriate first words for a 12-month-old.
- He also **waves 'bye-bye'**, showing appropriate receptive and expressive communication.
*Gross motor skills*
- The child can **walk with one hand held**, which is an expected gross motor milestone for a 12-month-old.
- Many 12-month-olds are just beginning to cruise or take their first independent steps.
*Social skills*
- The child **waves 'bye-bye'** and **cries if left with a stranger alone**, which are age-appropriate demonstrations of **social interaction** and **stranger anxiety**, respectively, for a 12-month-old.
- These behaviors indicate typical social and emotional development.
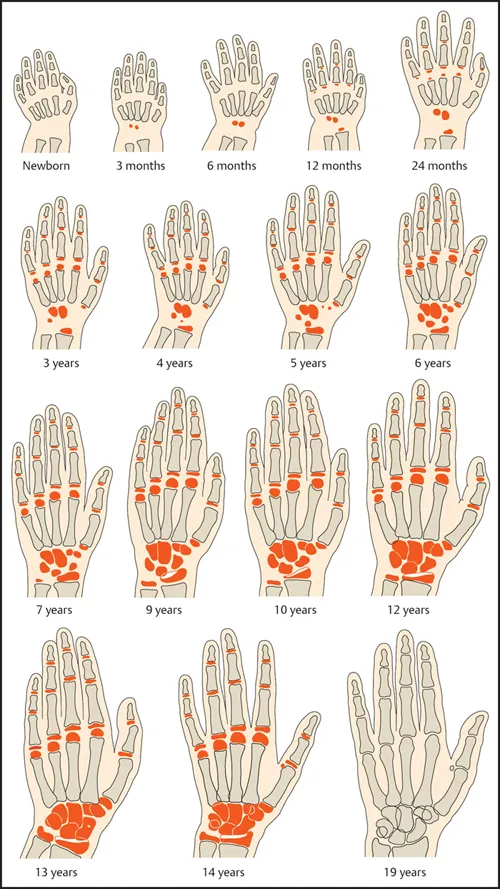
Short stature workup US Medical PG Question 7: A concerned mother presents to clinic stating that her 14-year-old son has not gone through his growth spurt. She states that, although shorter, he had been growing at the same rate as his peers until the past year. There is no evidence of delayed puberty in the mother, but the father's history is unknown. The patient has no complaints. On physical exam, the patient is a healthy-appearing 14-year-old boy whose height is below the third percentile and whose weight is at the 50th percentile. His bone age is determined to be 11 years. A laboratory workup, including thyroid stimulating hormone (TSH), is unremarkable. What is the most likely diagnosis?
- A. Hypothyroidism
- B. Familial short stature
- C. Constitutional growth delay (Correct Answer)
- D. Growth hormone deficiency
- E. Celiac disease
Short stature workup Explanation: ***Constitutional growth delay***
- This condition is characterized by **delayed bone age**, normal growth velocity initially followed by a deceleration, and an eventual **catch-up growth spurt** leading to normal adult height. The patient's history of being shorter than peers but growing at the same rate, followed by a recent slow down, and a bone age of 11 years (compared to his chronological age of 14) strongly indicates this.
- The absence of other symptoms, **unremarkable lab workup** (including TSH), and the fact that he was previously growing at the same rate as peers further supports constitutional growth delay, which is often linked to a family history of delayed puberty, even if the mother's history is negative and the father's is unknown.
*Hypothyroidism*
- **Hypothyroidism** would typically present with symptoms such as fatigue, weight gain, constipation, and cold intolerance, none of which are mentioned in the patient's history.
- The **unremarkable TSH** level rules out hypothyroidism as the cause of growth delay in this case.
*Familial short stature*
- In **familial short stature**, children typically grow along a short but otherwise normal percentile curve, and their bone age would typically match their chronological age.
- The patient's growth deceleration and significantly **delayed bone age** are inconsistent with familial short stature.
*Growth hormone deficiency*
- **Growth hormone deficiency** often presents with a significant deceleration of growth velocity and very short stature for age, but usually the bone age delay is more pronounced or proportional to the chronological age.
- While low height is present, the **otherwise healthy appearance** and absence of other metabolic or health issues make constitutional growth delay more likely, especially with the provided bone age and normal lab results.
*Celiac disease*
- **Celiac disease** can cause growth delay, but it would typically be accompanied by gastrointestinal symptoms such as abdominal pain, diarrhea, or malabsorption-related issues like weight loss or anemia.
- This patient is **asymptomatic** and has a normal weight for his height percentiles, which makes celiac disease an unlikely diagnosis.
Short stature workup US Medical PG Question 8: A 5-year-old girl presents to the physician with increased muscle cramping in her lower extremities after walking extended distances. The young girl is in the 10th percentile for height. Her past medical history is notable only for a cystic hygroma detected shortly after birth. Which of the following findings is most likely in this patient?
- A. Inferior erosion of the ribs
- B. Barr bodies on buccal smear
- C. Apparent hypertrophy of the calves
- D. Endocardial cushion defect
- E. Differential blood pressures between upper and lower extremities (Correct Answer)
Short stature workup Explanation: ***Differential blood pressures between upper and lower extremities***
- This patient's presentation of **muscle cramping** in the lower extremities after exertion (claudication), being in the **10th percentile for height**, and history of **cystic hygroma** is highly suggestive of **Turner syndrome** (45,XO).
- A common cardiovascular anomaly associated with Turner syndrome is **coarctation of the aorta**, which causes **higher blood pressure in the upper extremities** compared to the lower extremities due to narrowing of the aorta, typically distal to the left subclavian artery.
- This finding is the **classic clinical sign** on physical examination and would be present at any age when coarctation exists, making it the most likely finding in this **5-year-old patient**.
- The reduced blood flow to the lower extremities explains the muscle cramping with exertion (intermittent claudication).
*Inferior erosion of the ribs*
- **Rib notching** (inferior erosion) is indeed associated with **coarctation of the aorta** due to collateral circulation through dilated intercostal arteries.
- However, this is a **chronic radiological finding** that typically develops over many years and is more commonly seen in **older children and adults** with long-standing coarctation.
- In a **5-year-old child**, rib notching is **unlikely to have developed yet**, making differential blood pressures a more likely finding at this age.
*Apparent hypertrophy of the calves*
- **Calf pseudohypertrophy** is characteristic of **Duchenne muscular dystrophy**, a progressive X-linked recessive disorder typically affecting boys by age 3-5, caused by dystrophin deficiency leading to fatty and fibrous tissue replacement of muscle.
- While both conditions can present in childhood, this patient's **female sex**, history of **cystic hygroma**, and **short stature** point toward Turner syndrome rather than Duchenne muscular dystrophy.
*Endocardial cushion defect*
- **Endocardial cushion defects** (including atrioventricular septal defects) are classically associated with **Down syndrome** (Trisomy 21).
- While congenital heart defects are common in Turner syndrome (occurring in 30-50% of patients), **bicuspid aortic valve** and **coarctation of the aorta** are the most characteristic cardiac anomalies, not endocardial cushion defects.
*Barr bodies on buccal smear*
- **Barr bodies** represent an **inactivated X chromosome** and are visible in cells with at least two X chromosomes (e.g., normal XX females).
- **Turner syndrome** is characterized by **monosomy X** (45,XO), meaning there is only one X chromosome and thus **no Barr bodies** would be found on buccal smear.
Short stature workup US Medical PG Question 9: A 9-year-old boy is brought to the physician for evaluation of short stature. He is at the 5th percentile for height, 65th percentile for weight, and 95th percentile for head circumference. Examination shows midface retrusion, a bulging forehead, and flattening of the nose. The extremities are disproportionately short. He was adopted and does not know his biological parents. The patient’s condition is an example of which of the following genetic phenomena?
- A. Variable expressivity
- B. Anticipation
- C. Codominance
- D. Imprinting
- E. Complete penetrance (Correct Answer)
Short stature workup Explanation: ***Complete penetrance***
- Complete penetrance means that **all individuals who inherit the disease-causing allele will express the phenotype** associated with that allele
- This patient presents with classic features of **achondroplasia**: short stature at 5th percentile, midface retrusion, bulging forehead, flattened nose, and disproportionately short extremities
- Achondroplasia is caused by a mutation in the **FGFR3 gene** (autosomal dominant) and demonstrates **nearly 100% penetrance** - virtually all individuals with the mutation manifest the characteristic skeletal abnormalities
- This is a textbook example of complete penetrance where genotype reliably predicts phenotype
*Incorrect: Variable expressivity*
- Variable expressivity refers to differences in the **severity or clinical manifestations** among individuals with the same genetic mutation
- While achondroplasia may show some variation in severity, the question describes typical features without emphasizing variability in expression
- This patient shows the classic, expected phenotype rather than unusual expressivity
*Incorrect: Anticipation*
- Anticipation occurs when a genetic disorder becomes **more severe or presents at an earlier age in successive generations**
- This is characteristic of **trinucleotide repeat disorders** (e.g., Huntington disease, myotonic dystrophy, fragile X syndrome)
- Achondroplasia does not demonstrate anticipation; most cases arise from **de novo mutations** rather than inherited mutations
*Incorrect: Codominance*
- Codominance occurs when **both alleles are fully expressed** in the heterozygous state, with neither being dominant or recessive
- Classic examples include **ABO blood groups** and **HbS in sickle cell trait**
- Achondroplasia is an **autosomal dominant** condition, not codominant
*Incorrect: Imprinting*
- Genomic imprinting refers to **parent-of-origin effects** where gene expression depends on whether the allele was inherited from mother or father
- Examples include **Prader-Willi syndrome** (paternal deletion) and **Angelman syndrome** (maternal deletion)
- Achondroplasia shows no parent-of-origin effects
Short stature workup US Medical PG Question 10: A 4-year-old boy is brought to the pediatrician by his mother for a routine medical examination. His medical history is relevant for delayed gross motor milestones. The mother is concerned about a growth delay because both of his brothers were twice his size at this age. Physical examination reveals a well-groomed and healthy boy with a prominent forehead and short stature, in addition to shortened upper and lower extremities with a normal vertebral column. The patient’s vitals reveal: temperature 36.5°C (97.6°F); pulse 60/min; and respiratory rate 17/min and a normal intelligence quotient (IQ). A mutation in which of the following genes is the most likely cause underlying the patient’s condition?
- A. Runt-related transcription factor 2
- B. Alpha-1 type I collagen
- C. Fibroblast growth factor receptor 3 (Correct Answer)
- D. Insulin-like growth factor 1 receptor
- E. Fibrillin-1
Short stature workup Explanation: ***Fibroblast growth factor receptor 3***
- The constellation of **short stature**, prominent forehead, and **shortened upper and lower extremities** with a normal vertebral column in a child with normal intelligence is characteristic of **achondroplasia**.
- Achondroplasia is caused by a gain-of-function mutation in the **fibroblast growth factor receptor 3 (FGFR3)** gene, which inhibits chondrocyte proliferation and differentiation, leading to impaired endochondral ossification.
*Runt-related transcription factor 2*
- Mutations in **Runt-related transcription factor 2 (RUNX2)** are associated with **cleidocranial dysplasia**, a condition characterized by absent or hypoplastic clavicles, delayed closure of fontanelles, and dental abnormalities, which are not described in this patient.
- While it affects bone development, the specific features of achondroplasia, such as rhizomelic dwarfism and a prominent forehead, are not typical of RUNX2 mutations.
*Alpha-1 type I collagen*
- Mutations in **collagen genes**, particularly type I collagen (COL1A1, COL1A2), are linked to **osteogenesis imperfecta**, characterized by **fragile bones**, blue sclera, and hearing loss.
- The patient's presentation does not include these features, and the primary issue is disproportionate short stature due to impaired cartilage growth, not bone fragility.
*Insulin-like growth factor 1 receptor*
- Mutations in the **insulin-like growth factor 1 receptor (IGF1R)** can lead to **pre- and postnatal growth retardation** and microcephaly, often associated with developmental delay and feeding difficulties.
- While IGF1R mutations cause short stature, the specific skeletal dysmorphology (e.g., prominent forehead, shortened limbs) and normal intelligence are much more suggestive of achondroplasia.
*Fibrillin-1*
- Mutations in **fibrillin-1** are responsible for **Marfan syndrome**, which typically presents with **tall stature**, long limbs (dolichostenomelia), joint hypermobility, and cardiovascular abnormalities such as aortic root dilation.
- The patient's short stature and shortened limbs directly contradict the clinical picture of Marfan syndrome.
More Short stature workup US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.