Puberty stages (Tanner stages) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Puberty stages (Tanner stages). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Puberty stages (Tanner stages) US Medical PG Question 1: A 15-year-old girl is brought in by her parents to her pediatrician with concerns that their daughter still has not had her first menstrual cycle. The parents report that the patient has had no developmental issues in the past. She was born full term by vaginal delivery and has met all other milestones growing up. Based on chart review, the patient demonstrated breast bud development at 10 years of age. The patient is not self conscious of her appearance but is concerned that something may be wrong since she has not yet had her first period. The patient’s temperature is 97.9°F (36.6°C), blood pressure is 116/70 mmHg, pulse is 66/min, and respirations are 12/min. On exam, the patient appears her stated age and is of normal stature. She has Tanner 5 breast development but Tanner 2 pubic hair. On gynecologic exam, external genitalia appears normal, but the vagina ends in a blind pouch. Lab studies demonstrate that the patient has elevated levels of testosterone, estrogen, and luteinizing hormone. Which of the following is the most likely karyotype for this patient?
- A. 46, XX
- B. 47, XXY
- C. 45, XO
- D. 46, XY (Correct Answer)
- E. 47, XYY
Puberty stages (Tanner stages) Explanation: ***46, XY***
- This karyotype, coupled with the presentation, is classic for **Androgen Insensitivity Syndrome (AIS)**. Individuals with complete AIS are genetically male (**46, XY**) but have a female external phenotype due to a non-functional androgen receptor.
- The patient's **Tanner 5 breast development** (due to peripheral conversion of testosterone to estrogen) and **blind-ending vagina** are characteristic features of AIS, consistent with the lack of a uterus and fallopian tubes. Elevated testosterone, estrogen, and LH are also typical findings.
*46, XX*
- This karyotype represents a genotypically female individual. Failure of menstruation (primary amenorrhea) in this setting would suggest conditions like **Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome** (vaginal and uterine agenesis in a female karyotype), but this patient's hormonal profile (elevated testosterone) and blind-ending vagina in the presence of breast development without pubic hair are not typical for MRKH.
- In 46, XX individuals with primary amenorrhea, often there are issues with ovarian function, outflow tract obstruction, or hypothalamic-pituitary axis dysfunction, which do not fully align with the described hormonal and physical findings.
*47, XXY*
- This karyotype describes **Klinefelter syndrome**, which affects males. Individuals with Klinefelter syndrome typically present with a male phenotype, often with **hypogonadism, gynecomastia, and infertility**.
- This karyotype would not explain the patient's female external appearance and lack of menstruation; it's a condition affecting males.
*45, XO*
- This karyotype describes **Turner syndrome**, which affects females. Patients with Turner syndrome typically present with **gonadal dysgenesis**, leading to primary amenorrhea and a lack of secondary sexual characteristics (e.g., absent breast development).
- While patients with Turner syndrome can have a blind-ending vagina (if associated with Müllerian agenesis), the presence of **normal stature, Tanner 5 breast development**, and elevated testosterone levels are inconsistent with Turner syndrome.
*47, XYY*
- This karyotype describes **XYY syndrome**, which affects males. Individuals with XYY syndrome are typically phenotypically male and often present with increased height, but generally have normal fertility and sexual development.
- This karyotype would not be associated with a female external phenotype, breast development, or primary amenorrhea.
Puberty stages (Tanner stages) US Medical PG Question 2: A 16-year-old girl is brought to the physician because she has not attained menarche. There is no personal or family history of serious illness. She is 165 cm (5 ft 5 in) tall and weighs 60 kg (132 lb); BMI is 22 kg/m2. Breast development is Tanner stage 4, and pubic hair development is Tanner stage 1. Pelvic examination shows a blind vaginal pouch. This patient is most likely to have which of the following karyotypes?
- A. 47,XYY
- B. 46,XY (Correct Answer)
- C. 47,XXY
- D. 46,XX
- E. 45,XO
Puberty stages (Tanner stages) Explanation: ***46,XY***
- This karyotype, in the presence of **androgen insensitivity syndrome (AIS)**, explains the presentation: a genetic male (XY) who phenotypically appears female due to **androgen receptor defects**, leading to lack of masculinization and female external genitalia.
- The **blind vaginal pouch** and **absent uterus/cervix** (implied by lack of menarche despite breast development) are characteristic of AIS, as is the normal range of height and weight, and presence of breast development due to peripheral aromatization of androgens.
*47,XYY*
- This karyotype is associated with **XYY syndrome**, typically affecting males and not causing primary amenorrhea or female phenotypic development.
- Individuals with XYY syndrome are usually tall and may experience learning difficulties or behavioral issues, but they have normal male sexual development.
*47,XXY*
- This karyotype is characteristic of **Klinefelter syndrome**, affecting males and typically presenting with **hypogonadism**, small testes, gynecomastia, and often infertility.
- It does not cause a female phenotype, primary amenorrhea, or a blind vaginal pouch.
*46,XX*
- This is the normal female karyotype; if this patient had 46,XX, the most likely cause of primary amenorrhea would be **Müllerian agenesis (Mayer-Rokitansky-Küster-Hauser syndrome)**.
- However, in Müllerian agenesis, despite underdeveloped or absent vagina, uterus, and cervix, **normal ovarian function** would lead to typical pubic hair development (Tanner stage 4-5) and secondary sexual characteristics congruent with age, which contrasts with the Tanner stage 1 pubic hair here.
*45,XO*
- This karyotype denotes **Turner syndrome**, which presents with primary amenorrhea, but also with characteristic features such as **short stature**, streak gonads, and often specific dysmorphic features (e.g., webbed neck, shield chest).
- The patient's normal height and significant breast development (Tanner stage 4) make Turner syndrome unlikely, as ovarian failure in Turner syndrome typically prevents substantial breast development without hormone therapy.
Puberty stages (Tanner stages) US Medical PG Question 3: A 3-year-old girl is brought to the physician by her parents for complaints of breast development and pubic hair growth for the past 6 months. She has no significant birth or medical history. The temperature is 37.0°C (98.6°F), the pulse is 88/min, and the respirations are 20/min. Physical examination shows enlarged breasts at Tanner stage 3 and pubic hair at stage 2. Height and weight are in the normal range. On GnRH stimulation testing, a luteinizing hormone (LH) response of < 5 IU/L is detected. What is the most appropriate next step in diagnosis?
- A. Perform leuprolide stimulation test to measure testosterone
- B. Measure baseline estradiol levels and perform pelvic ultrasound (Correct Answer)
- C. Measure FSH levels to evaluate pituitary function
- D. Calculate LH:FSH ratio from previous GnRH test
- E. Repeat GnRH stimulation test to confirm LH response
Puberty stages (Tanner stages) Explanation: ***Measure baseline estradiol levels and perform pelvic ultrasound***
- This patient presents with **precocious puberty** (breast development and pubic hair at age 3). The **low LH response** (<5 IU/L) to GnRH stimulation confirms **peripheral (gonadotropin-independent) precocious puberty**.
- In peripheral precocious puberty, sex hormones are produced **autonomously** (independent of pituitary control), which **suppresses** the hypothalamic-pituitary-gonadal axis through negative feedback.
- The next step is to **identify the source** of autonomous sex hormone production. **Measuring estradiol levels** confirms elevated estrogen, and **pelvic ultrasound** evaluates for ovarian causes such as **ovarian cysts** or **tumors** (e.g., granulosa cell tumor), which are common causes of peripheral precocious puberty in girls.
- Other causes to consider include **McCune-Albright syndrome** (café-au-lait spots, polyostotic fibrous dysplasia) or exogenous estrogen exposure.
*Measure FSH levels to evaluate pituitary function*
- Measuring FSH is **not helpful** in this clinical context because the low LH response to GnRH stimulation **already indicates** that the pituitary is suppressed.
- In peripheral precocious puberty, both LH and FSH are **suppressed** due to negative feedback from peripherally produced sex hormones. Measuring FSH would simply confirm what we already know - that the pituitary axis is not activated.
- The priority is to find the **source** of the sex hormones, not to further characterize pituitary suppression.
*Perform leuprolide stimulation test to measure testosterone*
- Leuprolide is a **GnRH agonist** used to evaluate **central precocious puberty**, where the HPG axis is prematurely activated.
- This test is **not indicated** for peripheral precocious puberty, which has already been confirmed by the low LH response.
- Additionally, measuring testosterone would not be useful in a female patient presenting with estrogenic signs (breast development).
*Calculate LH:FSH ratio from previous GnRH test*
- The **LH:FSH ratio** is useful in diagnosing **central precocious puberty**, where an LH-predominant response (LH:FSH ratio >0.6-1.0) is characteristic.
- Since the LH response is already **low** (<5 IU/L), confirming peripheral precocious puberty, this ratio would not provide diagnostic value.
- The focus should be on investigating the **peripheral source** of sex hormones.
*Repeat GnRH stimulation test to confirm LH response*
- Repeating the GnRH stimulation test is **unnecessary** when the initial test provides clear results.
- The low LH response (<5 IU/L) definitively indicates peripheral precocious puberty, and repeating the test would only delay appropriate diagnostic workup for the underlying cause.
Puberty stages (Tanner stages) US Medical PG Question 4: A 16-year-old girl comes to the physician because of a 3-week history of nausea, increased urinary frequency, and breast tenderness. She has never had a menstrual period. She is actively involved in her school's track and field team. She is 173 cm (5 ft 8 in) tall and weighs 54 kg (120 lb); BMI is 18 kg/m2. Her breast and pubic hair development are at Tanner stage 5. Which of the following serum assays is the most appropriate next step in the diagnosis of this patient's condition?
- A. Thyrotropin
- B. Human chorionic gonadotropin (Correct Answer)
- C. Estriol
- D. Prolactin
- E. Luteinizing hormone
Puberty stages (Tanner stages) Explanation: **Human chorionic gonadotropin**
- The patient's symptoms (nausea, increased urinary frequency, breast tenderness) are classic signs of **pregnancy**, especially given her primary amenorrhea.
- A **human chorionic gonadotropin (hCG)** assay is the definitive test to confirm or rule out pregnancy.
*Thyrotropin*
- **Thyroid disorders** can cause menstrual irregularities, but the acute onset of nausea, increased urinary frequency, and breast tenderness points away from primary thyroid dysfunction as the initial primary diagnosis.
- While thyroid function may be assessed later if pregnancy is ruled out, it's not the most immediate next step for these specific symptoms.
*Estriol*
- **Estriol** is primarily useful in assessing **fetal well-being** later in pregnancy and in diagnosing estrogen deficiencies; it is not the initial test for suspected pregnancy.
- While part of the estrogen family, measuring estriol directly is not the first-line diagnostic for the patient's presenting symptoms.
*Prolactin*
- Elevated **prolactin** can cause **amenorrhea** and **galactorrhea** (breast discharge), but it doesn't typically cause nausea or increased urinary frequency.
- While hyperprolactinemia could be a cause for primary amenorrhea, the combination of symptoms strongly suggests pregnancy over hyperprolactinemia.
*Luteinizing hormone*
- **Luteinizing hormone (LH)** levels are used to assess ovulation and other causes of menstrual dysfunction, but they do not directly indicate pregnancy.
- While relevant to reproductive health, an LH assay isn't the most appropriate first step given the strong suspicious for pregnancy based on symptoms.
Puberty stages (Tanner stages) US Medical PG Question 5: A concerned mother presents to clinic stating that her 14-year-old son has not gone through his growth spurt. She states that, although shorter, he had been growing at the same rate as his peers until the past year. There is no evidence of delayed puberty in the mother, but the father's history is unknown. The patient has no complaints. On physical exam, the patient is a healthy-appearing 14-year-old boy whose height is below the third percentile and whose weight is at the 50th percentile. His bone age is determined to be 11 years. A laboratory workup, including thyroid stimulating hormone (TSH), is unremarkable. What is the most likely diagnosis?
- A. Hypothyroidism
- B. Familial short stature
- C. Constitutional growth delay (Correct Answer)
- D. Growth hormone deficiency
- E. Celiac disease
Puberty stages (Tanner stages) Explanation: ***Constitutional growth delay***
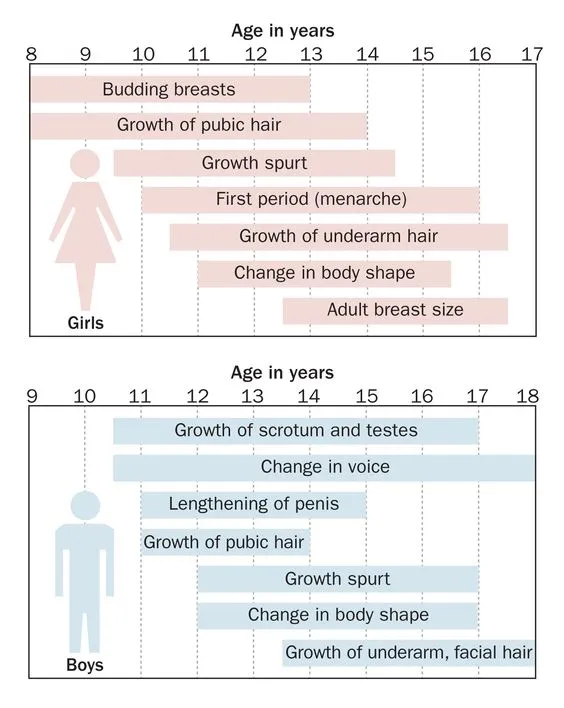
- This condition is characterized by **delayed bone age**, normal growth velocity initially followed by a deceleration, and an eventual **catch-up growth spurt** leading to normal adult height. The patient's history of being shorter than peers but growing at the same rate, followed by a recent slow down, and a bone age of 11 years (compared to his chronological age of 14) strongly indicates this.
- The absence of other symptoms, **unremarkable lab workup** (including TSH), and the fact that he was previously growing at the same rate as peers further supports constitutional growth delay, which is often linked to a family history of delayed puberty, even if the mother's history is negative and the father's is unknown.
*Hypothyroidism*
- **Hypothyroidism** would typically present with symptoms such as fatigue, weight gain, constipation, and cold intolerance, none of which are mentioned in the patient's history.
- The **unremarkable TSH** level rules out hypothyroidism as the cause of growth delay in this case.
*Familial short stature*
- In **familial short stature**, children typically grow along a short but otherwise normal percentile curve, and their bone age would typically match their chronological age.
- The patient's growth deceleration and significantly **delayed bone age** are inconsistent with familial short stature.
*Growth hormone deficiency*
- **Growth hormone deficiency** often presents with a significant deceleration of growth velocity and very short stature for age, but usually the bone age delay is more pronounced or proportional to the chronological age.
- While low height is present, the **otherwise healthy appearance** and absence of other metabolic or health issues make constitutional growth delay more likely, especially with the provided bone age and normal lab results.
*Celiac disease*
- **Celiac disease** can cause growth delay, but it would typically be accompanied by gastrointestinal symptoms such as abdominal pain, diarrhea, or malabsorption-related issues like weight loss or anemia.
- This patient is **asymptomatic** and has a normal weight for his height percentiles, which makes celiac disease an unlikely diagnosis.
Puberty stages (Tanner stages) US Medical PG Question 6: A previously healthy 6-year-old boy is brought to the physician because he has increased facial and axillary hair. There is no family history of serious illness. He is at 95th percentile for height and weight. Examination shows coarse pubic and axillary hair. The penis and left testicle are enlarged. Serum concentrations of human chorionic gonadotropin and alpha-fetoprotein are within the reference range. Which of the following is the most likely cause of these findings?
- A. Sertoli cell tumor
- B. Seminoma
- C. Leydig cell tumor (Correct Answer)
- D. Lymphoma
- E. Choriocarcinoma
Puberty stages (Tanner stages) Explanation: ***Leydig cell tumor***
- The boy's **precocious puberty** symptoms, including increased facial/axillary hair and an enlarged penis and testicle, are consistent with excessive **androgen production**.
- **Leydig cells** are the primary source of testosterone in the testes, and a tumor can cause autonomous androgen secretion, leading to virilization.
*Sertoli cell tumor*
- While Sertoli cell tumors can occur in children, they more commonly present with **feminization** due to estrogen production, such as gynecomastia, or with a palpable mass.
- They are less likely to cause precocious virilization; this patient's enlarged testicle and penis with marked virilization are more characteristic of testosterone-secreting tumors.
*Seminoma*
- **Seminomas** are malignant germ cell tumors that typically affect adult males aged 30-50 and are rare in young children.
- They are unlikely to cause precocious puberty symptoms as directly as a Leydig cell tumor; they often present as a painless testicular mass and may produce **hCG** or **AFP** in some cases.
*Lymphoma*
- Testicular lymphoma is a rare form of non-Hodgkin lymphoma, primarily affecting older men, and is exceedingly rare in children.
- It does not typically cause **endocrine symptoms** like precocious puberty; it would present as a rapidly growing testicular mass.
*Choriocarcinoma*
- **Choriocarcinomas** are aggressive germ cell tumors that produce high levels of **human chorionic gonadotropin (hCG)**.
- While hCG can stimulate Leydig cells to produce testosterone and cause precocious puberty, the serum hCG concentration in this patient is within the reference range, making choriocarcinoma unlikely.
Puberty stages (Tanner stages) US Medical PG Question 7: An otherwise healthy 13-year-old boy is brought to the physician for the evaluation of severe acne for the last 3 years. Topical retinoic acid and oral tetracycline did not improve his symptoms. He shaves his chin and mustache area every few days. His parents report that he grew 5 cm (2 in) during the last year. The onset of pubic hair growth was at age 8. He is at the 95th percentile for height and weight. Vital signs are within normal limits. Examination shows several pimples and pustules along the skin of the cheeks, chin, and neck. Genitals are Tanner stage 4 and pubic hair is Tanner stage 5. Early morning serum laboratory studies drawn 30 minutes after administration of ACTH show:
Sodium 137 mEq/L
Potassium 3.8 mEq/L
Cortisol (0800 h) 4 μg/dL
Aldosterone 10 ng/dL (N = 7–30)
17OH-Progesterone 230 ng/dL (N = 3–90)
Deoxycorticosterone 2.7 ng/dL (N = 3.5–11.5)
Androstenedione 350 ng/dL (N = 80–240)
Dehydroepiandrosterone sulfate (DHEAS) 420 μg/dL (N = 29–412)
Which of the following is the most likely underlying cause of this patient's symptoms?
- A. Constitutive activation of adenylyl cyclase
- B. Leydig-cell tumor production of androgens
- C. Exposure to exogenous steroids
- D. 17α-hydroxylase deficiency
- E. 21-hydroxylase deficiency (Correct Answer)
Puberty stages (Tanner stages) Explanation: ***21-hydroxylase deficiency***
- The very high **17-OH progesterone** (230 ng/dL) is characteristic of **21-hydroxylase deficiency**, as the enzyme block causes a buildup of precursors proximal to the block.
- This leads to increased shunting towards **androgen production** (**androstenedione** and **DHEAS** are elevated), explaining the severe acne, early puberty, and advanced physical development, while **cortisol** and **aldosterone** are low or normal leading to mineralocorticoid deficiency, though it's not a salt-wasting crisis in this non-classical presentation.
*Constitutive activation of adenylyl cyclase*
- This condition, in the context of adrenal hyperplasia, would lead to **ACTH-independent cortisol production**, not the low cortisol observed here after ACTH administration, nor the specific steroid precursor elevations.
- It is associated with conditions like **primary pigmented nodular adrenocortical disease** (PPNAD) or McCune-Albright syndrome, which presents differently, primarily with Cushing features.
*Leydig-cell tumor production of androgens*
- While a Leydig-cell tumor would cause **precocious puberty** and elevated androgens, it would typically **suppress LH and FSH** and would not explain the specific pattern of elevated adrenal precursors like **17-OH progesterone**.
- **Adrenal steroid levels** (like 17-OH progesterone, DHEA-S) would not be elevated from a testicular Leydig cell tumor.
*Exposure to exogenous steroids*
- Exogenous androgen exposure would lead to **suppression of endogenous androgen production** and would likely cause **adrenal suppression**, resulting in low cortisol levels, but not the elevated **17-OH progesterone** and other adrenal androgen precursors seen in this patient.
- Long-term exogenous corticosteroid use causes **Cushingoid features** and adrenal suppression, not directly increased androgen production.
*17α-hydroxylase deficiency*
- This deficiency would lead to **low cortisol and androgens** but markedly **elevated mineralocorticoids** like deoxycorticosterone and corticosterone.
- The patient's **deoxycorticosterone** is below the normal range, and **aldosterone** is normal, ruling out 17α-hydroxylase deficiency.
Puberty stages (Tanner stages) US Medical PG Question 8: An 11-year-old girl presents to the pediatrician with her mother, who is concerned about her sexual development. She mentions that she herself experienced the onset of menses at the age of 10.5 years, while her daughter has still not had a menstrual period. However, she is otherwise a healthy girl with no significant medical problems since birth. On physical examination, her vital signs are stable. Evaluation of breast and pubic hair are Tanner stage 2. The pediatrician reassures the mother that her daughter's sexual development is within the normal range for girls and there is nothing to worry about at present. Which is a sign of Tanner stage 2?
- A. Pubarche
- B. Adrenarche
- C. Menarche
- D. Thelarche (Correct Answer)
- E. Coarse pubic hair
Puberty stages (Tanner stages) Explanation: ***Thelarche***
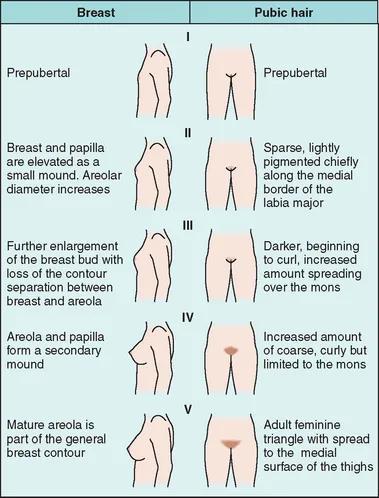
- **Thelarche** refers to the initial development of breast buds, which is the defining characteristic of **Tanner stage 2** breast development.
- This stage indicates the beginning of puberty, marked by a slight elevation of the breast and papilla, forming a small mound.
*Pubarche*
- **Pubarche** refers to the appearance of **pubic hair**, which is typically seen in **Tanner stage 2** for pubic hair development, but not breast development.
- While girls often experience pubarche around the same time as thelarche, the term specifically describes pubic hair growth, not breast development.
*Adrenarche*
- **Adrenarche** is the maturation of the adrenal cortex, leading to increased production of adrenal androgens and typically precedes the physical changes of puberty.
- It refers to the biochemical process of adrenal androgen secretion, not a specific physical sign of **Tanner stage 2** development.
*Menarche*
- **Menarche** is the first menstrual period, which occurs much later in puberty, typically after a significant progression through **Tanner stages 2-4**.
- This event signifies reproductive maturity and is not present at the initial stage of breast budding.
*Coarse pubic hair*
- The presence of **coarse pubic hair** indicates a more advanced stage of pubic hair development, typically **Tanner stage 3 or 4**, as hair becomes darker and coarser.
- **Tanner stage 2** pubic hair is usually sparse, long, straight, and lightly pigmented.
Puberty stages (Tanner stages) US Medical PG Question 9: A 7-year-old boy is brought to the physician because his parents are concerned about his early sexual development. He has no history of serious illness and takes no medications. His brother was diagnosed with testicular cancer 5 years ago and underwent a radical orchiectomy. The patient is at the 85th percentile for height and 70th percentile for weight. Examination shows greasy facial skin. There is coarse axillary hair. Pubic hair development is at Tanner stage 3 and testicular development is at Tanner stage 2. The remainder of the examination shows no abnormalities. An x-ray of the wrist shows a bone age of 10 years. Basal serum luteinizing hormone and follicle-stimulating hormone are elevated. An MRI of the brain shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Leuprolide therapy (Correct Answer)
- B. Testicular ultrasound
- C. Cortisol supplementation
- D. Radiation therapy
- E. Observation
Puberty stages (Tanner stages) Explanation: ***Leuprolide therapy***
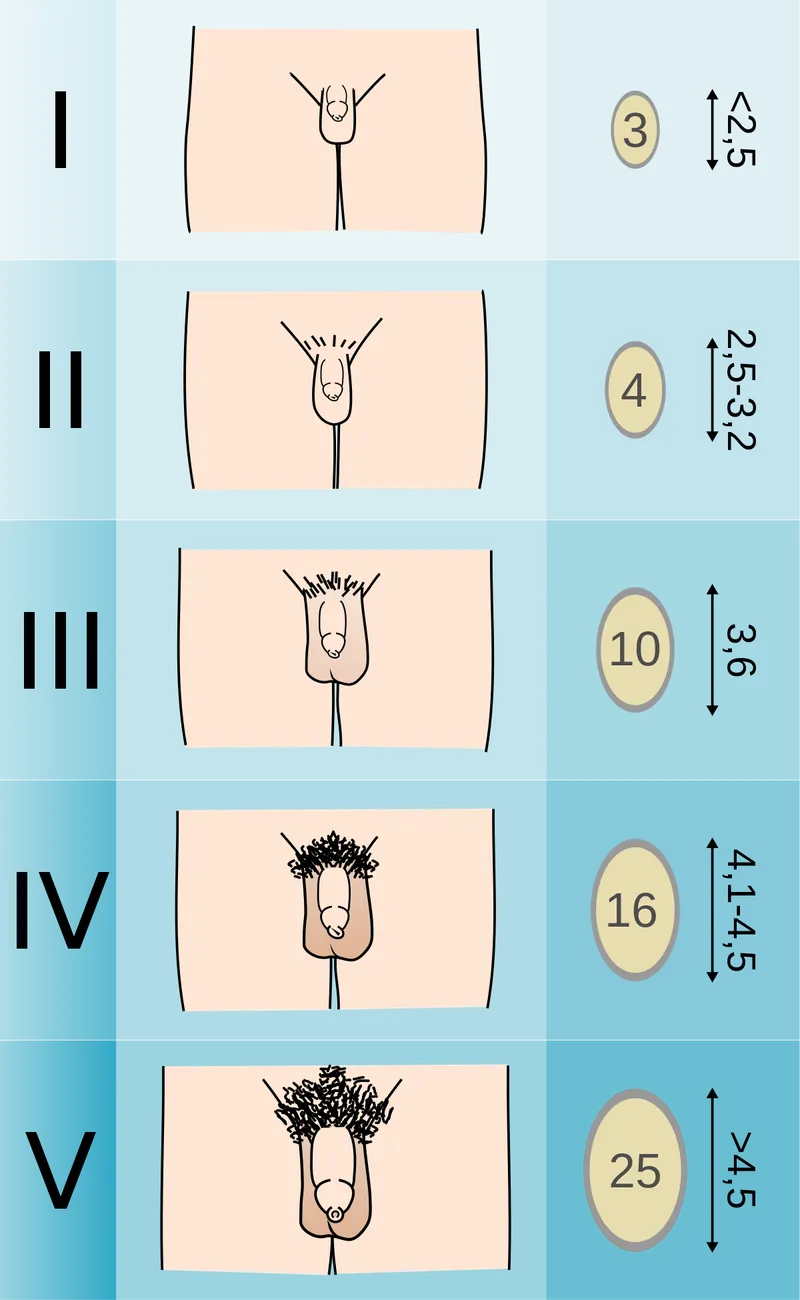
- This patient presents with **central precocious puberty** (CPP), indicated by elevated **basal LH and FSH levels** in the context of advanced bone age, Tanner stage 3 pubic hair, and Tanner stage 2 testicular development at a young age.
- **Leuprolide** is a GnRH analog that, when given continuously, downregulates the pituitary's GnRH receptors, suppressing gonadotropin release and halting pubertal progression. This is the appropriate treatment for CPP.
*Testicular ultrasound*
- While useful for evaluating testicular size and consistency, it is typically performed when there is suspicion of **peripheral precocious puberty** (e.g., Leydig cell tumor) with low LH/FSH or significant testicular asymmetry, which is not the primary presentation here.
- The elevated basal LH and FSH values indicate a **central origin** of puberty, making a testicular ultrasound less immediately relevant as a *next step* compared to directly addressing the central hormonal drive.
*Cortisol supplementation*
- This would be indicated for conditions causing **adrenal insufficiency**, such as **congenital adrenal hyperplasia (CAH)** with salt-wasting or Addison's disease.
- CAH typically presents with virilization and advanced bone age but would show **low LH/FSH** (due to peripheral androgen excess) and elevated adrenal androgens (e.g., DHEA-S, 17-hydroxyprogesterone), which are not described.
*Radiation therapy*
- This is a treatment for **malignant tumors**, often used in cases of brain tumors.
- The MRI of the brain showed **no abnormalities**, ruling out a pituitary or hypothalamic tumor as the cause of CPP in this case, thus making radiation therapy inappropriate.
*Observation*
- **Observation** alone is inappropriate given the significant **advancement of bone age** (10 years in a 7-year-old) and clear signs of central precocious puberty.
- Untreated CPP can lead to **compromised adult height potential** due to premature epiphyseal fusion and psychosocial issues, necessitating intervention.
Puberty stages (Tanner stages) US Medical PG Question 10: A 3-year-old girl is brought to the physician by her mother two days after the sudden onset of a rash. The mother says that the rash developed an hour after she bathed the child in hot water. Two weeks ago, the patient was diagnosed with a skin infection and was treated with penicillin V. She has been otherwise healthy but has missed several well-child examinations. She lives with her single mother, who recently lost her job and is now dependent on social assistance. The patient's mother has major depressive disorder and her maternal aunt has systemic lupus erythematosus. The girl's temperature is 36.8°C (98.2°F), pulse is 112/min, and blood pressure is 108/62 mm Hg. She has poor eye contact. Physical examination shows sharply delineated erythema on the lower extremities up to the umbilicus with sparing of the knees and flexor surfaces. Further evaluation is most likely to reveal which of the following?
- A. Dermatographism
- B. Multiple injuries in different stages of healing (Correct Answer)
- C. Ulcers of the oral mucosa
- D. Malar rash with sparing of the nasolabial folds
- E. Positive Nikolsky's sign
Puberty stages (Tanner stages) Explanation: ***Multiple injuries in different stages of healing***
- This scenario strongly suggests **child abuse**. The "rash" described is suspicious; it is a **sharply delineated erythema** on the lower extremities up to the umbilicus with sparing of the knees and flexor surfaces, appearing after a hot bath. This pattern is classic for a **scald injury**, which would be considered abuse if inflicted by hot water.
- The mother's claim of a sudden rash occurring an hour after a hot bath makes a thermal injury more likely, especially given her recent job loss, dependence on social assistance, and major depressive disorder, all of which are **risk factors for child abuse**. The child's poor eye contact also raises concerns.
*Dermatographism*
- **Dermatographism** is a form of urticaria where strokes or pressure on the skin cause raised, red lines.
- This condition presents as transient wheals and would not align with the described **sharply delineated erythema** in a specific distribution, nor would it be triggered only by a hot bath in this manner.
*Ulcers of the oral mucosa*
- **Oral ulcers** are common in various systemic conditions (e.g., aphthous stomatitis, viral infections, lupus) but are not directly suggested by a sudden onset of skin erythema after a hot bath.
- While some forms of abuse might involve oral injury, the described skin rash is not a typical presentation or associated finding that would lead one to specifically look for oral ulcers.
*Malar rash with sparing of the nasolabial folds*
- A **malar rash** (butterfly rash) is characteristic of **systemic lupus erythematosus (SLE)**, which the patient's maternal aunt has. However, this rash typically affects the cheeks and bridge of the nose.
- The patient's rash is described as **sharply delineated erythema** on the lower extremities up to the umbilicus, with sparing of specific areas, which is inconsistent with the distribution and appearance of a malar rash.
*Positive Nikolsky's sign*
- **Nikolsky's sign** involves the epidermal detachment upon light friction, indicative of blistering disorders like **pemphigus vulgaris** or **staphylococcal scalded skin syndrome (SSSS)**.
- While SSSS can cause widespread erythema and skin peeling, the description of **sharply delineated erythema** on specific body parts after a hot bath is more consistent with a thermal injury than the diffuse blistering and epidermal sloughing seen in SSSS.
More Puberty stages (Tanner stages) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.