Obesity in children US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Obesity in children. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Obesity in children US Medical PG Question 1: A 14-year-old girl is brought to the physician because she frequently experiences cramping and pain in her legs during school sports. She is at the 10th percentile for height. Her blood pressure is 155/90 mm Hg. Examination shows a high-arched palate with maloccluded teeth and a low posterior hairline. The patient has a broad chest with widely spaced nipples. Pelvic examination shows normal external female genitalia with scant pubic hair. Without appropriate treatment, this patient is at the greatest risk of developing which of the following complications?
- A. Alzheimer disease
- B. Hyperphagia
- C. Pulmonary stenosis
- D. Osteoporosis (Correct Answer)
- E. Severe acne
Obesity in children Explanation: ***Osteoporosis***
- This patient's presentation with **short stature**, high blood pressure, **webbed neck** (implied by low posterior hairline), and **wide-spaced nipples** is highly suggestive of **Turner syndrome (45,X0)**.
- Turner syndrome is characterized by **gonadal dysgenesis**, leading to **estrogen deficiency**, which is a major risk factor for developing **osteoporosis**.
- Without estrogen replacement therapy, patients with Turner syndrome have significantly increased risk of **low bone mineral density** and **fractures**.
*Pulmonary stenosis*
- While Turner syndrome is associated with **cardiac anomalies** such as **bicuspid aortic valve** and **coarctation of the aorta**, these are typically **congenital defects** present from birth rather than complications that develop over time.
- **Pulmonary stenosis** itself is not a primary cardiac finding in Turner syndrome.
- The question asks about complications that develop without treatment, making **osteoporosis** more appropriate as it progressively worsens due to chronic **estrogen deficiency**.
*Alzheimer disease*
- **Alzheimer disease** is a neurodegenerative disorder primarily associated with aging and genetics, not typically a direct complication of Turner syndrome.
- While cognitive profiles in Turner syndrome can differ (particularly with visuospatial skills), there is no established increased risk of Alzheimer disease.
*Hyperphagia*
- **Hyperphagia** (excessive eating) is characteristically associated with **Prader-Willi syndrome** due to hypothalamic dysfunction.
- It is not a feature or complication of **Turner syndrome**.
*Severe acne*
- **Severe acne** is often related to increased androgen levels or hormonal fluctuations during puberty.
- In Turner syndrome, there is typically **hypogonadism** and **estrogen deficiency**, which would not predispose to severe acne.
Obesity in children US Medical PG Question 2: A 7-day-old male infant presents to the pediatrician for weight loss. There is no history of excessive crying, irritability, lethargy, or feeding difficulty. The parents deny any history of fast breathing, bluish discoloration of lips/nails, fever, vomiting, diarrhea, or seizures. He was born at full term by vaginal delivery without any perinatal complications and his birth weight was 3.6 kg (8 lb). Since birth he has been exclusively breastfed and passes urine six to eight times a day. His physical examination, including vital signs, is completely normal. His weight is 3.3 kg (7.3 lb); length and head circumference are normal for his age and sex. Which of the following is the next best step in the management of the infant?
- A. Reassurance of parents (Correct Answer)
- B. Evaluation of the mother for malnutrition
- C. Admission of the infant in the NICU to treat with empiric intravenous antibiotics
- D. Emphasize the need to clothe the infant warmly to prevent hypothermia
- E. Supplementation of breastfeeding with an appropriate infant formula
Obesity in children Explanation: ***Reassurance of parents***
- A **weight loss of 8.3%** (300g from 3.6kg) is within the expected range for a 7-day-old exclusively breastfed infant, which can be up to 7-10% in the first week.
- The infant's normal physical exam, good urine output, and lack of other symptoms suggest **adequate feeding** and overall well-being.
*Evaluation of the mother for malnutrition*
- The mother's nutritional status is not directly indicative of the infant's weight loss within the normal physiological range in this scenario.
- There is no information to suggest the mother is malnourished or that it would directly impact the quality or quantity of breast milk to cause pathological weight loss.
*Admission of the infant in the NICU to treat with empiric intravenous antibiotics*
- This is an overly aggressive intervention as there are **no signs or symptoms of infection** (e.g., fever, lethargy, poor feeding) and the infant appears well.
- Empiric antibiotics are not warranted in an otherwise healthy, full-term infant with normal physiological weight loss.
*Emphasize the need to clothe the infant warmly to prevent hypothermia*
- The infant's **vital signs are normal**, indicating no hypothermia, and there is no clinical evidence to support this as a primary concern.
- While maintaining warmth is important, it is not the next best step for addressing this specific presentation of physiological weight loss.
*Supplementation of breastfeeding with an appropriate infant formula*
- Supplementation is typically not needed for physiological weight loss in an otherwise healthy, exclusively breastfed infant with **adequate urine output** and no signs of dehydration.
- Encouraging continued exclusive breastfeeding and providing support for proper latch and feeding techniques would be more appropriate if there were concerns about inadequate milk intake.
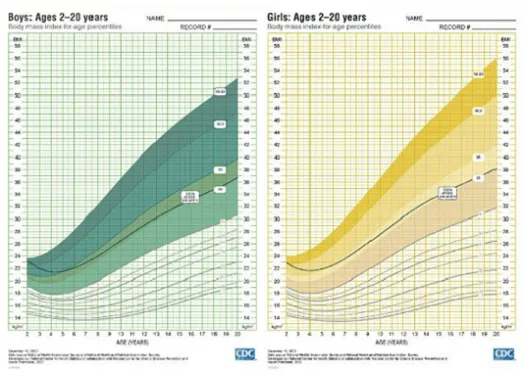
Obesity in children US Medical PG Question 3: A 5-year-old boy is brought to the physician because of behavioral problems. His mother says that he has frequent angry outbursts and gets into fights with his classmates. He constantly complains of feeling hungry, even after eating a full meal. He has no siblings, and both of his parents are healthy. He is at the 25th percentile for height and is above the 95th percentile for weight. Physical examination shows central obesity, undescended testes, almond-shaped eyes, and a thin upper lip. Which of the following genetic changes is most likely associated with this patient's condition?
- A. Mitotic nondisjunction of chromosome 21
- B. Mutation of FBN-1 gene on chromosome 15
- C. Microdeletion of long arm of chromosome 7
- D. Loss of paternal gene expression on chromosome 15 (Correct Answer)
- E. Deletion of Phe508 on chromosome 7
Obesity in children Explanation: ***Loss of paternal gene expression on chromosome 15***
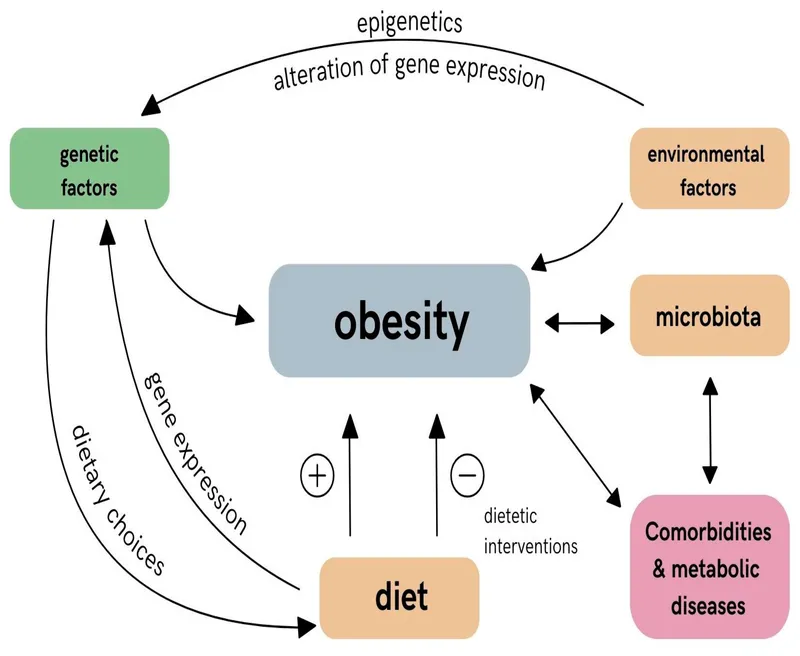
- The patient's symptoms, including **hyperphagia**, **obesity**, behavioral issues, short stature, and **hypogonadism** (undescended testes), are characteristic of **Prader-Willi syndrome**.
- Prader-Willi syndrome is most commonly caused by the **loss of paternal gene expression** from the **q11-q13 region of chromosome 15**, either due to a paternal deletion, maternal uniparental disomy, or a defect in the imprinting center.
*Microdeletion of long arm of chromosome 7*
- A microdeletion on the long arm of chromosome 7 (7q11.23) is associated with **Williams syndrome**, characterized by an **elfin facial appearance**, supravalvular aortic stenosis, and intellectual disability.
- This does not match the patient's symptoms of obesity, hyperphagia, or hypogonadism.
*Deletion of Phe508 on chromosome 7*
- A deletion of phenylalanine at position 508 (**ΔF508**) on chromosome 7 is the most common mutation in the **cystic fibrosis transmembrane conductance regulator (CFTR)** gene, causing **cystic fibrosis**.
- Cystic fibrosis is an **autosomal recessive disorder** requiring mutations in both alleles (inherited from both parents), and primarily affects the exocrine glands, leading to lung disease, pancreatic insufficiency, and infertility, which are unrelated to the patient's presentation.
*Mutation of FBN-1 gene on chromosome 15*
- A mutation in the **FBN1 gene** on chromosome 15 (15q21.1) causes **Marfan syndrome**, which is a connective tissue disorder.
- Marfan syndrome presents with tall stature, long limbs (**arachnodactyly**), lens dislocation, and aortic root dilation, none of which are described in this patient.
*Mitotic nondisjunction of chromosome 21*
- Mitotic nondisjunction of chromosome 21 can lead to **mosaic Down syndrome**, but **trisomy 21** (due to meiotic nondisjunction) is the most common cause of Down syndrome.
- Down syndrome is associated with characteristic facial features, intellectual disability, and congenital heart defects, which are distinct from the symptoms presented.
Obesity in children US Medical PG Question 4: A 5-year-old boy presents to the pediatrician for a well child visit. He is meeting his developmental milestones and is in the 15th percentile for height and 70th percentile for weight. His parents report that he complains of fatiguing easily and having trouble participating in sports. They are concerned he is not getting enough sleep and state that sometimes they hear him snore. The patient has a past medical history of a supracondylar fracture of the humerus, which was appropriately treated. He is doing well in school but is sometimes bullied for being small. The patient eats a balanced diet of milk, fruit, and some vegetables. His parents have been trying to get him to drink more milk so he can grow taller. His temperature is 99.5°F (37.5°C), blood pressure is 90/48 mmHg, pulse is 100/min, respirations are 19/min, and oxygen saturation is 98% on room air. On physical exam, the patient appears well. HEENT exam is notable for conjunctival pallor and a unilateral clear middle ear effusion. Cardiac exam reveals a benign flow murmur. Pulmonary exam is clear to auscultation bilaterally. The patient's gait is stable and he is able to jump up and down. A full set of labs are ordered as requested by the parents including a serum vitamin D level, B12 level, and IGF level. A selection of these lab values are seen below.
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 4.3 mEq/L
HCO3-: 25 mEq/L
BUN: 20 mg/dL
Glucose: 99 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 9.9 mg/dL
AST: 12 U/L
ALT: 10 U/L
Which of the following would you expect to find in this patient?
- A. Decreased IGF levels
- B. Increased RDW and TIBC (Correct Answer)
- C. Decreased oxygen saturation when the patient sleeps
- D. Increased MCV
- E. Decreased vitamin D level
Obesity in children Explanation: ***Increased RDW and TIBC***
- The patient presents with **conjunctival pallor**, fatigue, and snoring, falling in the 15th percentile for height and 70th for weight, suggesting **iron deficiency anemia**. Anemia would cause an **increased red cell distribution width (RDW)** as red blood cells vary in size, and **increased total iron-binding capacity (TIBC)** as the body tries to maximize iron absorption.
- While other signs of mild anemia like glossitis or pica are not explicitly mentioned, the combination of symptoms and the common prevalence of **iron-deficiency anemia** in children due to inadequate dietary intake or rapid growth phases supports this finding. Prolonged milk intake can inhibit iron absorption.
*Decreased IGF levels*
- **Insulin-like growth factor (IGF) levels** are primarily associated with growth hormone deficiency or severe malnutrition, which is not strongly indicated here. The patient's height is at the 15th percentile, which is *small*, but within the normal range, and his weight is at the 70th percentile, indicating he is not severely malnourished.
- While fatigue and small stature can be associated with growth disorders, the overall presentation with pallor points more distinctly towards an alternative diagnosis like **anemia** rather than growth hormone axis dysfunction.
*Decreased oxygen saturation when the patient sleeps*
- The patient's snoring could suggest **sleep-disordered breathing** or **sleep apnea**, leading to decreased oxygen saturation during sleep.
- However, based on the *conjunctival pallor*, fatigue, and growth concerns, **iron deficiency anemia** is a more prominent diagnosis, and while sleep apnea is possible, direct evidence of desaturation is not provided.
*Increased MCV*
- An **increased MCV (macrocytic anemia)** is characteristic of deficiencies in **vitamin B12** or **folate**.
- The patient's symptoms, particularly conjunctival pallor and fatigue, are more consistent with a **microcytic anemia** (decreased MCV), often caused by **iron deficiency**, rather than a macrocytic one.
*Decreased vitamin D level*
- While **fatigue** can be a symptom of **vitamin D deficiency**, the more prominent findings of **conjunctival pallor** and height/weight percentiles are less directly indicative of this specific deficiency as the primary diagnosis.
- The patient's diet
includes milk and fruit, which are typically fortified or contain vitamin D, making a severe deficiency less likely to be the primary cause of his symptoms, though a mild deficiency cannot be ruled out without specific lab results.
Obesity in children US Medical PG Question 5: A 17-year-old girl is brought into the physician's office with complaints of nausea, vomiting, headache, and blurry vision. In preparation for final exams the patient's mother started her on an array of supplements and herbal preparations given the "viral illness" that is prevalent at her school. Despite these remedies, the girl has been feeling perpetually worse, and yesterday during cheerleading practice had to sit out after vomiting and feeling dizzy. The patient admits to falling during one of the exercises and hitting her head on another girl's shin due to her dizziness. When asked to clarify her dizziness, the patient states that she feels rather lightheaded at times. The patient's BMI is 19 kg/m^2. She endorses diarrhea of recent onset, and some non-specific, diffuse pruritus of her skin which she attributes to stress from her finals. The patient has a past medical history of anxiety, depression, and excessive exercise habits. On physical exam the patient is alert and oriented to place, person, and time, and answers questions appropriately. She denies any decreased ability to participate in school or to focus. Her skin is dry and peeling with a minor yellow discoloration. Her memory is intact at 1 minute and 5 minutes for 3 objects. The patient's pupils are equal and reactive to light and there are no abnormalities upon examination of cranial nerve III, IV or VI.
Which of the following is the most likely cause of this patient's symptoms?
- A. Idiopathic intracranial hypertension
- B. Migraine headache with aura
- C. Bulimia nervosa
- D. Head trauma
- E. Supplement use (Correct Answer)
Obesity in children Explanation: ***Supplement use***
- The patient's history of being started on "an array of supplements and herbal preparations" for a "viral illness," combined with **nausea, vomiting, headache, blurry vision, dizziness, diarrhea, and pruritus,** strongly suggests an adverse reaction or toxicity from these supplements.
- The **dry, peeling skin with minor yellow discoloration** could indicate vitamin A toxicity, as many "viral illness" supplements contain high doses of vitamin A, and this symptom set is highly consistent with hypervitaminosis A.
*Idiopathic intracranial hypertension*
- While idiopathic intracranial hypertension (IIH) can present with **headache, nausea, vomiting, and blurry vision**, it typically involves **papilledema** on fundoscopic exam, which is not mentioned and generally causes more severe visual disturbances than described.
- IIH is more common in **obese young women**, and this patient has a BMI of 19 kg/m^2, making it less likely.
*Migraine headache with aura*
- Migraines can cause **headache, nausea, vomiting, and aura** (e.g., blurry vision, dizziness), but the **diarrhea, pruritus, diffuse dry skin with yellow discoloration**, and the onset coinciding with supplement use are not typical features of a migraine.
- The symptoms are described as progressively worsening over time, which is less consistent with a typical migraine attack.
*Bulimia nervosa*
- The patient has a history of anxiety, depression, and excessive exercise, which can be associated with bulimia, but there is no mention of **binge-eating** or **purging behaviors** (like self-induced vomiting).
- The combination of **dry skin, yellow discoloration, diarrhea, and widespread pruritus** is not classic for bulimia nervosa, which often presents with **dental erosions, parotid gland enlargement, and electrolyte imbalances**.
*Head trauma*
- While the patient admits to falling and hitting her head, her symptoms of **nausea, vomiting, headache, blurry vision, and dizziness** predated the fall and worsened irrespective of it.
- She is **alert, oriented, answers questions appropriately, and has intact memory** with no focal neurological deficits or abnormal cranial nerve findings (III, IV, VI), making a significant head injury less likely to be the primary cause of her widespread symptoms.
Obesity in children US Medical PG Question 6: A 42-year-old woman comes to the physician for a routine health maintenance examination. She has generalized fatigue and has had difficulties doing her household duties for the past 3 months. She has eczema and gastroesophageal reflux disease. She has a history of using intravenous methamphetamine in her youth but has not used illicit drugs in 23 years. Her medications include topical clobetasol and pantoprazole. She is 160 cm (5 ft 3 in) tall and weighs 105 kg (231 lb); BMI is 42 kg/m2. Her temperature is 37°C (98.6°F), pulse is 95/min, and blood pressure is 145/90 mm Hg. The lungs are clear to auscultation. Cardiac examination shows no abnormalities. Pelvic examination shows a normal vagina and cervix. Laboratory studies show:
Hemoglobin 13.1 g/dL
Leukocyte count 7,800/mm3
Platelet count 312,000/mm3
Serum
Na+ 141 mEq/L
K+ 4.6 mEq/L
Cl- 98 mEq/L
Urea nitrogen 12 mg/dL
Fasting glucose 110 mg/dL
Creatinine 0.8 mg/dL
Total cholesterol 269 mg/dL
HDL-cholesterol 55 mg/dL
LDL-cholesterol 160 mg/dL
Triglycerides 320 mg/dL
Urinalysis is within normal limits. An x-ray of the chest shows no abnormalities. She has not lost any weight over the past year despite following supervised weight loss programs, including various diets and exercise regimens. Which of the following is the most appropriate next step in management of this patient?
- A. Phentermine and topiramate therapy and follow-up in 3 months
- B. Bariatric surgery (Correct Answer)
- C. Liposuction
- D. Behavioral therapy
- E. Metformin and statin therapy and follow-up in 3 months
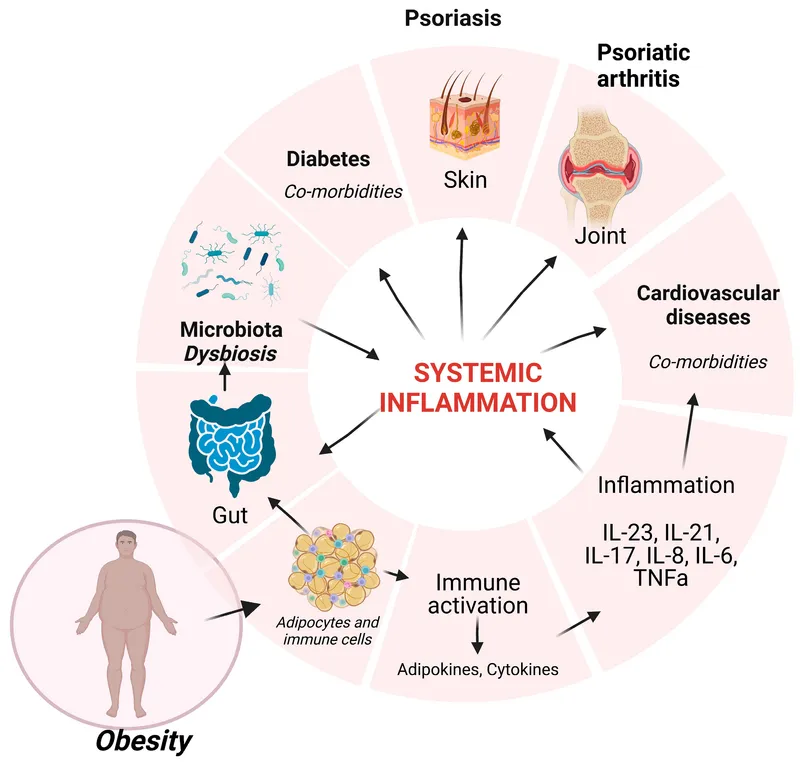
Obesity in children Explanation: ***Bariatric surgery***
- This patient has **severe obesity** (BMI of 42 kg/m²) with obesity-related comorbidities including **hypertension** (BP 145/90 mm Hg), **dyslipidemia** (elevated cholesterol and triglycerides), and **pre-diabetes** (fasting glucose 110 mg/dL), and has failed multiple supervised weight loss programs. **Bariatric surgery** is indicated for patients with BMI ≥ 40 kg/m² or BMI ≥ 35 kg/m² with obesity-related comorbidities who have failed at least 6 months of supervised weight loss.
- It is the most effective treatment for sustained weight loss in patients with **severe obesity**, leading to significant improvement or resolution of comorbidities.
*Phentermine and topiramate therapy and follow-up in 3 months*
- While medication can aid weight loss, this patient's **BMI of 42 kg/m²** signifies severe obesity, where medication alone is often insufficient for sustained and significant weight reduction.
- **Pharmacotherapy** is typically considered for BMI ≥ 30 kg/m² or BMI ≥ 27 kg/m² with comorbidities, but for class III obesity (BMI ≥ 40 kg/m²), bariatric surgery generally provides superior and more lasting outcomes.
*Liposuction*
- **Liposuction** is primarily a cosmetic procedure for localized fat removal and is not an effective treatment for generalized severe obesity or weight loss, nor does it address the metabolic complications of obesity.
- It does not lead to sustained weight loss or improvement in obesity-related comorbidities like **hypertension** and **dyslipidemia**.
*Behavioral therapy*
- The patient has already attempted multiple supervised weight loss programs, including various diets and exercise regimens, suggesting that **behavioral therapy** alone has not been effective for sustained weight loss in her case.
- While beneficial as part of a comprehensive approach, it is unlikely to achieve the significant and sustained weight loss required for a patient with **severe obesity** that has failed prior conventional methods.
*Metformin and statin therapy and follow-up in 3 months*
- **Metformin** and **statin therapy** target specific comorbidities (pre-diabetes/insulin resistance and dyslipidemia, respectively) but do not address the underlying **severe obesity**.
- While these medications are important for managing aspects of her metabolic syndrome, they are not a primary treatment for weight loss and will not lead to significant weight reduction in a patient with a **BMI of 42 kg/m²**.
Obesity in children US Medical PG Question 7: A 52-year-old Caucasian man with hypertension comes to the physician because of frequent urination and increased thirst. He drinks 4 oz of alcohol daily and has smoked 1 pack of cigarettes daily for the past 30 years. He is 180 cm (5 ft 10 in) tall and weighs 106 kg (233 lb); BMI is 33 kg/m2. His blood pressure is 130/80 mm Hg. Laboratory studies show a hemoglobin A1c of 8.5%. Which of the following is the most likely predisposing factor for this patient's condition?
- A. High calorie diet (Correct Answer)
- B. Alcohol consumption
- C. Smoking history
- D. Caucasian ethnicity
- E. HLA-DR4 status
Obesity in children Explanation: ***High calorie diet***
- This patient presents with **Type 2 Diabetes Mellitus**, evidenced by **polyuria**, **polydipsia**, and **HbA1c of 8.5%** (diagnostic threshold >6.5%).
- **Obesity** (BMI 33 kg/m²) resulting from chronic high-calorie intake is the **most significant predisposing factor** for Type 2 DM, as it leads to **insulin resistance** through adipose tissue accumulation and inflammatory cytokine release.
- Among all the listed risk factors, obesity from dietary excess is the **strongest and most direct modifiable risk factor** for developing Type 2 DM.
*Alcohol consumption*
- Moderate alcohol intake (4 oz daily) is not a primary predisposing factor for Type 2 DM.
- Excessive chronic alcohol consumption can affect glucose metabolism and contribute to pancreatitis-related diabetes, but this patient's moderate intake is not the primary driver of his condition.
*Smoking history*
- Smoking increases risk of **cardiovascular complications** and worsens diabetes outcomes, but it is not the primary predisposing factor for **developing** Type 2 DM.
- The strongest association with DM onset is obesity and insulin resistance, not smoking.
*Caucasian ethnicity*
- Caucasian ethnicity confers **lower risk** for Type 2 DM compared to African American, Hispanic, Native American, and Asian populations.
- While genetic factors play a role, Caucasian ethnicity is not a specific predisposing factor in this case.
*HLA-DR4 status*
- **HLA-DR4** is strongly associated with **Type 1 Diabetes Mellitus**, an autoimmune condition typically presenting in younger patients with absolute insulin deficiency.
- This patient's age, obesity, and clinical presentation are classic for **Type 2 DM**, which has no association with HLA-DR4.
Obesity in children US Medical PG Question 8: A six-year-old male presents to the pediatrician for a well child visit. The patient’s parents report that they are struggling to manage his temper tantrums, which happen as frequently as several times per day. They usually occur in the morning before school and during mealtimes, when his parents try to limit how much he eats. The patient often returns for second or third helpings at meals and snacks throughout the day. The patient’s parents have begun limiting the patient’s food intake because he has been gaining weight. They also report that the patient recently began first grade but still struggles with counting objects and naming letters consistently. The patient sat without support at 11 months of age and walked at 17 months of age. He is in the 99th percentile for weight and 5th percentile for height. On physical exam, he has almond-shaped eyes and a downturned mouth. He has poor muscle tone.
Which of the following additional findings would most likely be seen in this patient?
- A. Webbed neck
- B. Macroorchidism
- C. Ataxia
- D. Hemihyperplasia
- E. Hypogonadism (Correct Answer)
Obesity in children Explanation: ***Hypogonadism***
- The patient's presentation, including **hyperphagia**, **obesity**, developmental delay, and distinctive facial features (almond-shaped eyes, downturned mouth, poor muscle tone), is highly suggestive of **Prader-Willi Syndrome**.
- **Hypogonadism** (undescended testes in males, delayed puberty) is a classic feature of **Prader-Willi Syndrome** due to hypothalamic dysfunction, which also causes the voracious appetite.
*Webbed neck*
- A **webbed neck** is characteristic of **Turner Syndrome** (45, XO), which affects females and is associated with short stature, but not typically with the hyperphagia and obesity seen here.
- The patient is a male, making Turner Syndrome an unlikely diagnosis.
*Macroorchidism*
- **Macroorchidism** (enlarged testes) is a hallmark feature of **Fragile X Syndrome**, which is associated with intellectual disability and developmental delays.
- While fragile X syndrome involves developmental delay, it does not typically present with the extreme hyperphagia, obesity, and specific facial features described in the patient.
*Ataxia*
- **Ataxia** (lack of voluntary coordination of muscle movements) in conjunction with developmental delays can be seen in various neurological disorders such as **Friedreich's ataxia** or **cerebral palsy**.
- This symptom is not a primary or characteristic finding in Prader-Willi Syndrome, and the other described features point away from ataxia as the most likely additional finding.
*Hemihyperplasia*
- **Hemihyperplasia** (overgrowth of one side of the body) is associated with conditions like **Beckwith-Wiedemann Syndrome**, which also involves macroglossia and an increased risk of tumors.
- This finding is not typically associated with the constellation of symptoms (hyperphagia, obesity, intellectual disability, hypotonia) seen in Prader-Willi Syndrome.
Obesity in children US Medical PG Question 9: A 3-year-old boy is brought to the emergency department by his mother because of a cough and mild shortness of breath for the past 12 hours. He has not had fever. He has been to the emergency department 4 times during the past 6 months for treatment of asthma exacerbations. His 9-month-old sister was treated for bronchiolitis a week ago. His father has allergic rhinitis. Current medications include an albuterol inhaler and a formoterol-fluticasone inhaler. He appears in mild distress. His temperature is 37.5°C (99.5°F), pulse is 101/min, respirations are 28/min, and blood pressure is 86/60 mm Hg. Examination shows mild intercostal and subcostal retractions. Pulmonary examination shows decreased breath sounds and mild expiratory wheezing throughout the right lung field. Cardiac examination shows no abnormalities. An x-ray of the chest shows hyperlucency of the right lung field with decreased pulmonary markings. Which of the following is the next best step in management?
- A. Azithromycin therapy
- B. Racemic epinephrine
- C. Albuterol nebulization
- D. CT of the lung
- E. Bronchoscopy (Correct Answer)
Obesity in children Explanation: ***Bronchoscopy***
- The patient's history of recurrent respiratory symptoms, unilateral wheezing and decreased breath sounds, and radiological findings of **unilateral hyperlucency** and **decreased pulmonary markings** strongly suggest a **foreign body aspiration**.
- **Bronchoscopy** is both diagnostic and therapeutic in this situation, allowing for direct visualization and removal of the foreign body.
*Azithromycin therapy*
- This is an **antibiotic** and would be used for bacterial infections, which are not indicated here given the clinical picture of a suspected foreign body.
- Antibiotics are not effective for mechanical obstruction of the airway.
*Racemic epinephrine*
- Racemic epinephrine is used for conditions like **croup** to reduce airway edema.
- It would not address an inhaled **foreign body**, which is a mechanical obstruction.
*Albuterol nebulization*
- While albuterol is used for bronchospasm, the unilateral nature of the findings and the history of recurrent issues point away from simple asthma exacerbation.
- Albuterol would likely not relieve the obstruction caused by a **foreign body**.
*CT of the lung*
- While CT could help identify a foreign body, it exposes the child to **radiation** and is not the definitive treatment.
- Bronchoscopy offers both diagnosis and immediate treatment, making it superior to CT as the *next best step*.
Obesity in children US Medical PG Question 10: An 8-year-old girl is brought to the emergency department by her parents with severe difficulty in breathing for an hour. She is struggling to breathe. She was playing outside with her friends, when she suddenly fell to the ground, out of breath. She was diagnosed with asthma one year before and has since been on treatment for it. At present, she is sitting leaning forward with severe retractions of the intercostal muscles. She is unable to lie down. Her parents mentioned that she has already taken several puffs of her inhaler since this episode began but without response. On physical examination, her lungs are hyperresonant to percussion and there is decreased air entry in both of her lungs. Her vital signs show: blood pressure 110/60 mm Hg, pulse 110/min, respirations 22/min, and a peak expiratory flow rate (PEFR) of 50%. She is having difficulty in communicating with the physician. Her blood is sent for evaluation and a chest X-ray is ordered. Her arterial blood gas reports are as follows:
PaO2 50 mm Hg
pH 7.38
PaCO2 47 mm Hg
HCO3 27 mEq/L
Which of the following is the most appropriate next step in management?
- A. Intravenous corticosteroid (Correct Answer)
- B. Inhaled corticosteroid
- C. Mechanical ventilation
- D. Methacholine challenge test
- E. Inhaled β-agonist
Obesity in children Explanation: ***Intravenous corticosteroid***
- The patient exhibits severe asthma exacerbation with **poor response to inhaled β-agonists**, marked respiratory distress, and an alarming **PEFR of 50%**.
- **Intravenous corticosteroids** are crucial in this scenario to reduce airway inflammation and prevent progression to respiratory failure.
*Inhaled corticosteroid*
- While essential for **long-term asthma control**, inhaled corticosteroids are **not effective enough for acute, severe exacerbations** due to their slower onset of action.
- The patient's inability to effectively inhale deeply due to distress also limits the utility of inhaled delivery in this emergency.
*Mechanical ventilation*
- Mechanical ventilation is a **last-resort intervention** for impending respiratory failure, indicated by signs like declining consciousness, hypercapnia, or respiratory arrest.
- While concerning, the patient's current ABG with a **near-normal pH (7.38)** despite hypercapnia suggests she is not yet in full respiratory failure, and less invasive measures should be initiated first.
*Methacholine challenge test*
- The methacholine challenge test is used to **diagnose asthma in stable patients** with normal spirometry, by assessing airway hyperresponsiveness.
- It is **absolutely contraindicated** in an acute, severe asthma exacerbation as it could worsen bronchoconstriction and respiratory distress.
*Inhaled β-agonist*
- The patient has **already taken several puffs of her inhaler** (likely a β-agonist) without response, indicating **refractory bronchospasm**.
- While initially appropriate, repeated administration when ineffective suggests the need for other therapeutic interventions to address the underlying inflammation.
More Obesity in children US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.