Nutritional assessment tools US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Nutritional assessment tools. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Nutritional assessment tools US Medical PG Question 1: A 21-year-old woman is admitted to the hospital for severe malnutrition with a BMI of 15 kg/m2. Past medical history is significant for chronic anorexia nervosa. During the course of her stay, she is treated with parenteral fluids and nutrition management. On the 4th day, her status changes. Her blood pressure is 110/75 mm Hg, heart rate is 120/min, respiratory rate is 25/min, and temperature is 37.0°C (98.6°F). On physical exam, her heart is tachycardic with a regular rhythm and her lungs are clear to auscultation bilaterally. She appears confused, disoriented, and agitated. Strength in her lower extremities is 4/5. What is the next step in management?
- A. MRI of the brain
- B. Administer insulin
- C. Measure electrolytes (Correct Answer)
- D. Arrange for outpatient counseling
- E. Doppler ultrasound on lower extremities
Nutritional assessment tools Explanation: ***Measure electrolytes***
- The patient's presentation with **confusion, disorientation, agitation**, and **lower extremity weakness** after refeeding for severe **malnutrition** is highly suggestive of **refeeding syndrome**. This syndrome is characterized by severe electrolyte shifts, particularly **hypophosphatemia**, **hypokalemia**, and **hypomagnesemia**.
- Measuring electrolytes immediately is crucial to diagnose and then correct these imbalances, which can lead to life-threatening complications like **cardiac arrhythmias**, **respiratory failure**, and **seizures**.
*MRI of the brain*
- While neurological symptoms are present, a brain MRI is not the immediate first step given the context of refeeding in a severely malnourished patient.
- The symptoms are more consistent with **metabolic derangements** associated with **refeeding syndrome** than an acute primary neurological event.
*Administer insulin*
- Administering insulin without knowing the patient's glucose or electrolyte status could be dangerous, especially given the increased risk of **hypokalemia** and **hypophosphatemia** in refeeding syndrome, which insulin can exacerbate.
- Refeeding syndrome typically involves glucose shifts, but **hypoglycemia** is not the primary immediate concern, and hyperinsulinemia in this context can cause cellular uptake of electrolytes leading to further depletion.
*Arrange for outpatient counseling*
- The patient is acutely ill and experiencing a potentially life-threatening complication requiring immediate medical intervention.
- **Outpatient counseling** is not appropriate for an acute hospital admission with severe, rapidly changing symptoms.
*Doppler ultrasound on lower extremities*
- While immobility can increase the risk of deep vein thrombosis (DVT), the patient's symptoms of **confusion, agitation, tachycardia, tachypnea**, and **weakness** are not primary indicators of DVT.
- The clinical picture points strongly towards **metabolic complications** of refeeding.
Nutritional assessment tools US Medical PG Question 2: During the selection of subjects for a study on infantile vitamin deficiencies, a child is examined by the lead investigator. She is at the 75th percentile for head circumference and the 80th percentile for length and weight. She can lift her chest and shoulders up when in a prone position, but cannot roll over from a prone position. Her eyes follow objects past the midline. She coos and makes gurgling sounds. When the investigator strokes the sole of her foot, her big toe curls upward and there is fanning of her other toes. She makes a stepping motion when she is held upright and her feet are in contact with the examination table. Which of the following additional skills or behaviors would be expected in a healthy patient of this developmental age?
- A. Cries when separated from her mother
- B. Smiles at her mother (Correct Answer)
- C. Rolls over from her back
- D. Responds to calling of own name
- E. Reaches out for objects
Nutritional assessment tools Explanation: ***Smiles at her mother***
- The child exhibits developmental milestones consistent with a **2-month-old infant**, such as lifting her chest in a prone position, following objects past the midline, cooing, and gurgling. Social smiling typically emerges around **2 months of age**.
- Primitive reflexes like the **Babinski reflex** (big toe curling upward and fanning of other toes) and **stepping reflex** are normally present at this age, supporting the approximate age of 2 months.
*Cries when separated from her mother*
- This behavior suggests **separation anxiety**, which typically develops much later, usually around **8-9 months of age**.
- A 2-month-old infant does not yet have the cognitive understanding or object permanence needed to exhibit true separation anxiety.
*Rolls over from her back*
- Rolling over from the back to the stomach is usually achieved between **4 and 6 months of age**.
- The child in the vignette cannot even roll over from a prone position, indicating she is not yet at the age for rolling from her back.
*Responds to calling of own name*
- Responding to one's own name is a more advanced auditory and cognitive milestone, generally developing between **6 and 9 months of age**.
- At 2 months, infants respond to voices and sounds but do not associate specific words with themselves.
*Reaches out for objects*
- Purposeful reaching and grasping for objects (palmar grasp) typically develops around **4 to 6 months of age**.
- A 2-month-old infant may swat at objects reflexively but does not exhibit coordinated, intentional reaching.
Nutritional assessment tools US Medical PG Question 3: A concerned mother presents to clinic stating that her 14-year-old son has not gone through his growth spurt. She states that, although shorter, he had been growing at the same rate as his peers until the past year. There is no evidence of delayed puberty in the mother, but the father's history is unknown. The patient has no complaints. On physical exam, the patient is a healthy-appearing 14-year-old boy whose height is below the third percentile and whose weight is at the 50th percentile. His bone age is determined to be 11 years. A laboratory workup, including thyroid stimulating hormone (TSH), is unremarkable. What is the most likely diagnosis?
- A. Hypothyroidism
- B. Familial short stature
- C. Constitutional growth delay (Correct Answer)
- D. Growth hormone deficiency
- E. Celiac disease
Nutritional assessment tools Explanation: ***Constitutional growth delay***
- This condition is characterized by **delayed bone age**, normal growth velocity initially followed by a deceleration, and an eventual **catch-up growth spurt** leading to normal adult height. The patient's history of being shorter than peers but growing at the same rate, followed by a recent slow down, and a bone age of 11 years (compared to his chronological age of 14) strongly indicates this.
- The absence of other symptoms, **unremarkable lab workup** (including TSH), and the fact that he was previously growing at the same rate as peers further supports constitutional growth delay, which is often linked to a family history of delayed puberty, even if the mother's history is negative and the father's is unknown.
*Hypothyroidism*
- **Hypothyroidism** would typically present with symptoms such as fatigue, weight gain, constipation, and cold intolerance, none of which are mentioned in the patient's history.
- The **unremarkable TSH** level rules out hypothyroidism as the cause of growth delay in this case.
*Familial short stature*
- In **familial short stature**, children typically grow along a short but otherwise normal percentile curve, and their bone age would typically match their chronological age.
- The patient's growth deceleration and significantly **delayed bone age** are inconsistent with familial short stature.
*Growth hormone deficiency*
- **Growth hormone deficiency** often presents with a significant deceleration of growth velocity and very short stature for age, but usually the bone age delay is more pronounced or proportional to the chronological age.
- While low height is present, the **otherwise healthy appearance** and absence of other metabolic or health issues make constitutional growth delay more likely, especially with the provided bone age and normal lab results.
*Celiac disease*
- **Celiac disease** can cause growth delay, but it would typically be accompanied by gastrointestinal symptoms such as abdominal pain, diarrhea, or malabsorption-related issues like weight loss or anemia.
- This patient is **asymptomatic** and has a normal weight for his height percentiles, which makes celiac disease an unlikely diagnosis.
Nutritional assessment tools US Medical PG Question 4: A 4-day-old male newborn is brought to the physician for a well-child examination. His mother is concerned that he is losing weight. He was born at 40 weeks' gestation and weighed 2980g (6-lb 9-oz); he currently weighs 2830g (6-lb 4-oz). Pregnancy was uncomplicated. He passed stool and urine 8 and 10 hours after delivery. He has been exclusively breast fed since birth and feeds 11–12 times daily. His mother says she changes 5–6 heavy diapers daily. Examination shows an open and firm anterior fontanelle. Mucous membranes are moist. Capillary refill time is less than 2 seconds. Cardiopulmonary examination shows no abnormalities. Which of the following is the most appropriate next best step in management?
- A. Continue breastfeeding (Correct Answer)
- B. Add rice based cereal
- C. Add cow milk based formula
- D. Serum creatinine and urea nitrogen
- E. Switch to soy-based formula
Nutritional assessment tools Explanation: ***Continue breastfeeding***
- A 4-day-old newborn losing less than 7% of birth weight, with good feeding frequency, adequate wet diapers, and normal physical examination findings, is considered typical for **physiological weight loss** in breastfed infants.
- The infant's current weight of 2830g is within the expected range, as healthy full-term newborns may lose up to 7-10% of their birth weight in the first few days, and his weight loss is only about 5%.
*Add rice based cereal*
- **Solid foods**, including rice cereal, should not be introduced before 4-6 months of age due to the immaturity of the infant's digestive system and potential for choking.
- Introducing solids too early can interfere with nutrient absorption from breast milk and increase the risk of allergies.
*Add cow milk based formula*
- Supplementing with formula is unnecessary in a healthy, breastfed infant exhibiting normal physiological weight loss and adequate feeding cues.
- Early introduction of formula can interfere with **successful breastfeeding establishment** and alter the infant's gut microbiome.
*Serum creatinine and urea nitrogen*
- These tests are used to assess **renal function** and are not indicated here, as the infant shows no signs of renal impairment (e.g., adequate urine output, moist mucous membranes).
- The physical examination findings and feeding pattern suggest a healthy newborn, not one requiring investigation for kidney issues.
*Switch to soy-based formula*
- Switching to any formula is unwarranted given the normal weight loss and breastfeeding progress, and specifically, soy-based formula is not routinely recommended for healthy infants.
- Soy formula is often reserved for infants with **cow's milk protein allergy** or **galactosemia**, neither of which is suggested by this clinical picture.
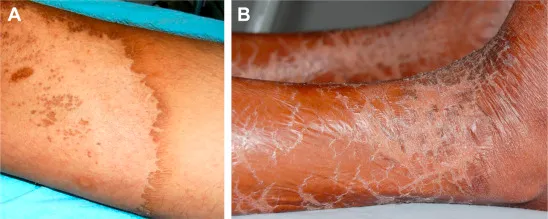
Nutritional assessment tools US Medical PG Question 5: A homeless woman presents with shortness of breath on exertion and pedal edema. Cardiac workup performed shows evidence of dilated cardiomyopathy and increased cardiac output. She also has decreased sensation over both extremities bilaterally. Which vitamin deficiency most likely caused these symptoms?
- A. Vitamin B6
- B. Vitamin C
- C. Vitamin B1 (Correct Answer)
- D. Vitamin B3
- E. Vitamin A
Nutritional assessment tools Explanation: ***Vitamin B1***
- The combination of **dilated cardiomyopathy**, **high-output heart failure** (manifesting as shortness of breath and pedal edema), and **peripheral neuropathy** (decreased sensation) is classic for **wet beriberi**, caused by thiamine (Vitamin B1) deficiency.
- **Homelessness** is a significant risk factor for nutritional deficiencies, including thiamine deficiency, due to inadequate diet.
*Vitamin B6*
- Deficiency can cause **peripheral neuropathy**, but it does not typically lead to **dilated cardiomyopathy** or **high-output heart failure**.
- Other manifestations of B6 deficiency include **sideroblastic anemia** and **seizures**.
*Vitamin C*
- Deficiency causes **scurvy**, characterized by **gingivitis**, **poor wound healing**, **petechiae**, and joint pain.
- It does not present with **cardiomyopathy** or **neuropathy** as described.
*Vitamin B3*
- Deficiency causes **pellagra**, characterized by the "3 Ds": **dermatitis**, **diarrhea**, and **dementia**.
- While it can affect the nervous system (dementia), it does not typically cause **dilated cardiomyopathy** or **peripheral neuropathy**.
*Vitamin A*
- Deficiency primarily affects **vision** (e.g., **night blindness**, **xerophthalmia**) and immune function.
- It is not associated with **cardiac** or **neurological symptoms** like those described in the patient.
Nutritional assessment tools US Medical PG Question 6: A 1-minute-old newborn is being examined by the pediatric nurse. The nurse auscultates the heart and determines that the heart rate is 89/min. The respirations are spontaneous and regular. The chest and abdomen are both pink while the tips of the fingers and toes are blue. When the newborn’s foot is slapped the face grimaces and he cries loud and strong. When the arms are extended by the nurse they flex back quickly. What is this patient’s Apgar score?
- A. 5
- B. 10
- C. 8 (Correct Answer)
- D. 6
- E. 9
Nutritional assessment tools Explanation: ***8***
- The Apgar score is calculated by assigning 0, 1, or 2 points to five criteria: **Appearance**, **Pulse**, **Grimace (reflex irritability)**, **Activity (muscle tone)**, and **Respiration**.
- This newborn scores 1 point for **Appearance** (pink body, blue extremities/acrocyanosis), 1 point for **Pulse** (89/min, which is below 100), 2 points for **Grimace** (cries loud and strong), 2 points for **Activity** (arms flex back quickly), and 2 points for **Respiration** (spontaneous and regular), totaling **8**.
*5*
- An Apgar score of 5 would indicate a more compromised state, with lower scores in multiple categories.
- This newborn demonstrates strong respiratory effort, vigorous cry, and active muscle tone, all inconsistent with a score of 5.
*10*
- A perfect score of 10 is rare and would require the newborn to have a **pink appearance throughout** (including extremities), a heart rate over 100 bpm, strong cry, active movement, and vigorous breathing.
- This newborn has two findings preventing a score of 10: **acrocyanosis** (blue extremities) and **heart rate of 89/min** (below 100).
*6*
- An Apgar score of 6 would imply more significant compromise, such as weak respiratory effort, minimal response to stimulation, or poor muscle tone.
- This newborn's strong cry, vigorous grimace response, and quick flexion indicate better performance than a score of 6.
*9*
- A score of 9 would mean only one parameter scores 1 point, with all others scoring 2 points.
- This newborn has **two parameters scoring 1 point**: **Appearance** (acrocyanosis) and **Pulse** (89/min, below 100), making the maximum possible score 8, not 9.
Nutritional assessment tools US Medical PG Question 7: A 21-year-old Syrian refugee, who arrived in the US 2 weeks ago after living in refugee camps in Jordan and Turkey for 2 years, presents with decreased night vision, severe dry eyes unresponsive to eye drops, and a corneal ulcer. She reports limiting her food intake to ensure her 3-year-old son's nutrition. Her BMI is 18.1 kg/m2. Examination reveals lethargy, dry mucous membranes, decreased skin turgor, and dry, thickened conjunctiva. This patient's symptoms are most consistent with a deficiency in a vitamin that contributes to which of the following processes?
- A. Clotting factor synthesis
- B. Cystathionine synthesis
- C. Methylation reactions
- D. Collagen synthesis
- E. T-cell differentiation (Correct Answer)
Nutritional assessment tools Explanation: ***T-cell differentiation***
- The patient's symptoms (night blindness, dry eyes, corneal ulcer, dry conjunctiva) are classic for **vitamin A deficiency**, which is crucial for **immune function** including T-cell differentiation.
- **Vitamin A** (retinoids) plays a vital role in the proper development and function of the immune system, influencing the differentiation of various immune cells, including T cells.
*Clotting factor synthesis*
- **Vitamin K** is essential for the synthesis of **blood clotting factors**, not vitamin A.
- Deficiency would manifest as bleeding tendencies, which are not described in this patient.
*Cystathionine synthesis*
- This process is dependent on **vitamin B6 (pyridoxine)**, which is involved in amino acid metabolism.
- Deficiency would lead to symptoms like **neuropathy** or **anemia**, not ophthalmic issues.
*Methylation reactions*
- **Folate (vitamin B9)** and **vitamin B12** are key cofactors in methylation reactions.
- Deficiencies typically lead to **megaloblastic anemia** and neurological symptoms.
*Collagen synthesis*
- **Vitamin C** is a crucial cofactor for **collagen synthesis** and hydroxylation.
- Deficiency results in **scurvy**, characterized by bleeding gums, poor wound healing, and petechiae.
Nutritional assessment tools US Medical PG Question 8: An 18-month-old boy is brought to the physician by his mother because of concern that he has not yet begun to walk. He was born at term and exclusively breastfed until 15 months of age. His mother says he has been well, apart from an episode of high fever and seizure 4 months ago for which she did not seek medical attention. He has an older brother who is currently receiving medical treatment for failure to thrive. His parents have no history of serious illness; they are of normal height. His last vaccine was at the age of 4 months. He is at the 20th percentile for length, 10th percentile for weight, and 50th percentile for head circumference. Physical examination shows dry mucous membranes and erosion of the enamel on the lingual surface of the incisors and carious molars. He has frontal bossing. His wrists are widened, his legs seem bent, and there is beading of the ribs. Which of the following is the most likely underlying cause of this patient's delay in walking?
- A. Deficiency of osteoclasts to reabsorb bone
- B. Osteoid proliferation in the subperiosteal bone
- C. Defect in type I collagen
- D. Mutation of fibroblast growth factor receptor 3
- E. Defective growth plate mineralization (Correct Answer)
Nutritional assessment tools Explanation: ***Defective growth plate mineralization***
- The patient's symptoms, including **delayed walking**, **frontal bossing**, **widened wrists**, **bowed legs** (bent legs), and **rachitic rosary** (beading of the ribs), are classic signs of **rickets**.
- **Rickets** is caused by a deficiency of vitamin D, leading to impaired mineralization of the cartilage and newly formed bone at the growth plates, resulting in soft and weak bones. The prolonged **exclusive breastfeeding** in this case, without vitamin D supplementation, increases the risk.
*Deficiency of osteoclasts to reabsorb bone*
- This describes conditions like **osteopetrosis** (Albers-Schonberg disease), which typically presents with **dense, brittle bones**, prone to fractures, and often associated with **bone marrow failure**.
- While osteopetrosis can cause skeletal deformities and delayed milestones, the specific findings of widened wrists, bowed legs, and rachitic rosary are not characteristic of osteopetrosis, which involves increased bone density.
*Osteoid proliferation in the subperiosteal bone*
- This is a feature of conditions like **secondary hyperparathyroidism** or some bone tumors, which do not typically present with the widespread skeletal deformities and growth plate abnormalities seen in rickets.
- While it can lead to bone pain and fragility, it does not explain the characteristic signs of rickets, such as widened growth plates and bone softening.
*Defect in type I collagen*
- A defect in type I collagen is characteristic of **osteogenesis imperfecta**, a genetic disorder leading to **brittle bones** that are prone to frequent fractures.
- Patients with osteogenesis imperfecta often have **blue sclerae** and **dentinogenesis imperfecta** (which can cause dental issues, but not specifically enamel erosion and caries in the manner described), but not the specific rickets-like skeletal deformities.
*Mutation of fibroblast growth factor receptor 3*
- A mutation in **fibroblast growth factor receptor 3 (FGFR3)** causes **achondroplasia**, the most common form of dwarfism.
- Achondroplasia is characterized by **short limbs**, a **normal trunk size**, and a **large head with frontal bossing**, but it does not cause the specific skeletal findings of widely spaced growth plates, bowed legs, and rachitic rosary associated with defective mineralization.
Nutritional assessment tools US Medical PG Question 9: A laborer's younger child is brought to the OPD with a swollen belly and dull face. He has been fed rice water (rice milk) in his diet mostly. On investigations, the child is found to have low serum protein and low albumin. What is the probable diagnosis?
- A. Kwashiorkor (Correct Answer)
- B. Kawasaki disease
- C. Marasmus
- D. Indian childhood cirrhosis
- E. Nephrotic syndrome
Nutritional assessment tools Explanation: ***Kwashiorkor***
- The symptoms of a **swollen belly** (due to **edema** from low albumin), **dull face**, and a diet primarily of **rice water** (low in protein) are classic signs of Kwashiorkor.
- Kwashiorkor is a form of severe protein-energy malnutrition characterized by **protein deficiency** that is greater than the calorie deficit, leading to **hypoalbuminemia** and fluid retention.
- The **dietary history** of rice water (carbohydrate-rich but protein-poor) is the key distinguishing feature.
*Kawasaki disease*
- This is an **acute vasculitis** primarily affecting young children, presenting with fever, rash, conjunctivitis, mouth changes, and lymphadenopathy.
- It does not involve a swollen belly or dull face as primary symptoms, nor is it linked to dietary protein deficiency.
*Marasmus*
- Marasmus is a form of severe malnutrition characterized by an **overall deficiency of calories** and nutrients, resulting in severe **wasting** of muscle and fat.
- While it involves low weight and energy deficit, the prominent **edema** (swollen belly) seen in this case points away from marasmus.
*Indian childhood cirrhosis*
- This is a rare, **fatal liver disease** in young children, often characterized by jaundice, hepatosplenomegaly, and liver failure.
- It is not primarily caused by protein deficiency and its symptoms are distinct from the presentation described.
*Nephrotic syndrome*
- While nephrotic syndrome also presents with **hypoalbuminemia and edema**, it would show **proteinuria** (>3.5 g/day), hyperlipidemia, and lipiduria on urinalysis.
- The **dietary history** and absence of urinary findings distinguish kwashiorkor from nephrotic syndrome.
Nutritional assessment tools US Medical PG Question 10: A 12-year-old boy presents with symptoms of headaches, visual disturbances, and growth retardation. An MRI scan is performed, and the image provided shows a cystic mass with both solid and calcified components in the suprasellar region, extending into the third ventricle. Based on the clinical presentation and MRI findings, what is the most likely diagnosis?
- A. Craniopharyngioma (Correct Answer)
- B. Germinoma
- C. Meningioma
- D. Pituitary adenoma
- E. Optic glioma
Nutritional assessment tools Explanation: ***Craniopharyngioma***
- This tumor is classically described as having **cystic** and **solid components** with **calcification**, which is evident in the provided MRI image. Its location in the **suprasellar region** and extension into the **third ventricle** are also typical.
- The clinical presentation of **headaches**, **visual disturbances** (due to compression of the optic chiasm), and **growth retardation** (due to hypothalamic-pituitary axis dysfunction) in a 12-year-old boy is highly suggestive of a craniopharyngioma, which commonly affects children and young adults.
*Germinoma*
- While germinomas can occur in the suprasellar region and cause similar endocrine and visual symptoms, they typically appear as **solid, homogeneously enhancing masses** on MRI and are less commonly cystic and calcified.
- They are more common in adolescence and are highly sensitive to radiation therapy, but their imaging characteristics differ from the described lesion.
*Meningioma*
- Meningiomas typically arise from the **arachnoid mater** and are usually **solid, extra-axial masses** that often have a **dural tail sign** on MRI.
- They are less common in children, and while they can calcify, their characteristic imaging features (extra-axial, dural attachment) are not consistent with the described suprasellar, intra-axial cystic mass.
*Pituitary adenoma*
- Pituitary adenomas originate from the **pituitary gland** and are usually located within the sella turcica, extending superiorly. While they can be cystic, **calcification is rare**, and they are more commonly solid and homogeneously enhancing.
- Although they can cause visual disturbances and hormonal imbalances, the prominent cystic-solid appearance with calcification and clear suprasellar origin extending into the third ventricle makes craniopharyngioma a more likely diagnosis in this age group and imaging.
*Optic glioma*
- Optic gliomas (pilocytic astrocytomas) are common **suprasellar tumors in children**, especially those with neurofibromatosis type 1, and can cause visual disturbances and endocrine dysfunction.
- However, they typically appear as **solid, fusiform masses** involving the optic nerve or chiasm with **homogeneous enhancement** and rarely show the characteristic cystic-solid architecture with prominent calcification seen in craniopharyngiomas.
More Nutritional assessment tools US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.