Impact of chronic disease on growth US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Impact of chronic disease on growth. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Impact of chronic disease on growth US Medical PG Question 1: A previously healthy 8-year-old boy is brought to the physician by his mother because of 6 months of progressive fatigue and weight loss. His mother reports that during this time, he has had decreased energy and has become a “picky eater.” He often has loose stools and complains of occasional abdominal pain and nausea. His family moved to a different house 7 months ago. He is at the 50th percentile for height and 25th percentile for weight. His temperature is 36.7°C (98°F), pulse is 116/min, and blood pressure is 85/46 mm Hg. Physical examination shows tanned skin and bluish-black gums. The abdomen is soft, nondistended, and nontender. Serum studies show:
Na+ 134 mEq/L
K+ 5.4 mEq/L
Cl- 104 mEq/L
Bicarbonate 21 mEq/L
Urea nitrogen 16 mg/dL
Creatinine 0.9 mg/dL
Glucose 70 mg/dL
Intravenous fluid resuscitation is begun. Which of the following is the most appropriate initial step in treatment?
- A. Fluoxetine
- B. Glucocorticoids (Correct Answer)
- C. Levothyroxine
- D. Deferoxamine
- E. Hyperbaric oxygen
Impact of chronic disease on growth Explanation: ***Glucocorticoids***
- This patient presents with symptoms highly suggestive of **adrenal insufficiency** (Addison's disease), including **fatigue**, weight loss, **hyperpigmentation** (tanned skin, bluish-black gums), **hypotension**, and electrolyte abnormalities like **hyponatremia** and **hyperkalemia**.
- **Glucocorticoid replacement** (e.g., hydrocortisone) is the cornerstone of treatment for adrenal insufficiency and is immediately required, especially given the signs of adrenal crisis (hypotension, fatigue).
*Fluoxetine*
- **Fluoxetine** is a selective serotonin reuptake inhibitor (SSRI) used to treat **depression** and **anxiety disorders**.
- While the patient has fatigue and "picky eating," these are symptoms of a systemic illness, not primary depression, and treating depression will not address the underlying adrenal pathology.
*Levothyroxine*
- **Levothyroxine** is a synthetic thyroid hormone used to treat **hypothyroidism**.
- Symptoms of hypothyroidism (e.g., fatigue, weight gain, constipation) overlap somewhat with adrenal insufficiency, but the **hyperpigmentation** and electrolyte derangements (hyperkalemia, hyponatremia) are not characteristic of hypothyroidism.
*Deferoxamine*
- **Deferoxamine** is a **chelating agent** used to treat **iron toxicity** or iron overload, such as in hemochromatosis.
- There are no clinical signs or laboratory findings in this patient to suggest iron overload or toxicity (e.g., no history of transfusions, no elevated ferritin).
*Hyperbaric oxygen*
- **Hyperbaric oxygen therapy** is used to treat conditions like **carbon monoxide poisoning**, decompression sickness, or refractory wounds.
- None of these conditions are suggested by the patient's presentation; there is no indication for hyperbaric oxygen therapy.
Impact of chronic disease on growth US Medical PG Question 2: A 42-year-old man who is employed as a construction worker presents to his primary care physician with complaints of moderate headaches and profuse sweating. He reports the need to carry up to 3 additional shirt changes to work because they drench quickly even with tasks of low physical exertion. His coworkers have commented about his changing glove and boot sizes, which have increased at least 4 times since he joined the company 10 years ago. Physical examination is unremarkable except for blood pressure of 160/95 mm Hg, hyperhidrosis, noticeably large pores, hypertrichosis, widely spaced teeth, and prognathism. Which of the following best explains the patient’s clinical manifestations?
- A. Increased serum cortisol
- B. Increased thyroid-stimulating hormone
- C. Increased serum metanephrines
- D. Increased serum insulin-like growth factor 1 (IGF-1) (Correct Answer)
- E. Increased serum testosterone
Impact of chronic disease on growth Explanation: ***Increased serum insulin-like growth factor 1 (IGF-1)***
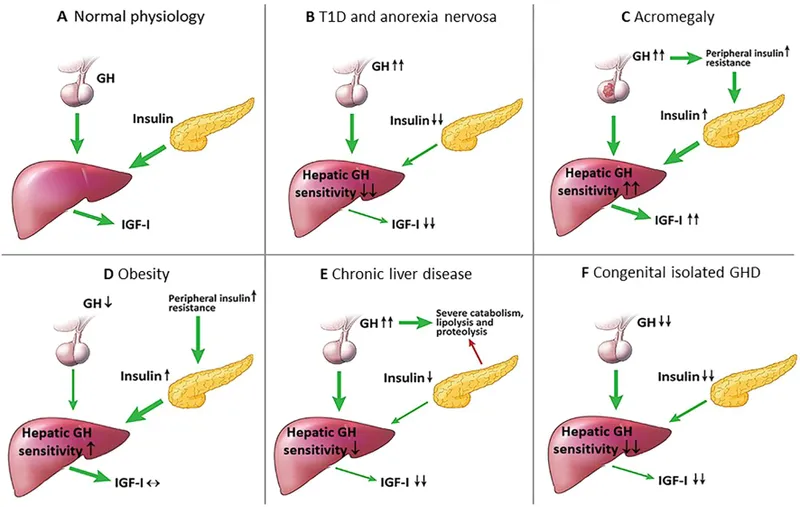
- Elevated **IGF-1** levels are indicative of **acromegaly**, a condition caused by excess growth hormone (GH) secretion, which explains the gradual changes in glove and boot sizes, prognathism, widely spaced teeth, and large pores.
- The symptoms of **profuse sweating**, **hypertrichosis**, **headaches**, and **hypertension** are common clinical manifestations of acromegaly due to the systemic effects of chronic GH excess.
*Increased serum cortisol*
- **Increased cortisol** (Cushing's syndrome) would present with central obesity, moon facies, buffalo hump, and striae, which are not described in the patient.
- While hypertension and hyperhidrosis can occur in Cushing's, the characteristic physical changes related to growth are absent.
*Increased thyroid-stimulating hormone*
- Elevated **TSH** suggests **hypothyroidism**, which would typically cause fatigue, weight gain, cold intolerance, and bradycardia, rather than profuse sweating and hypertension.
- **Hyperthyroidism** (low TSH, high thyroid hormones) can cause sweating and hypertension, but it would not explain the gradual increase in body and appendage size.
*Increased serum metanephrines*
- Elevated **metanephrines** are a hallmark of **pheochromocytoma**, which typically presents with paroxysmal episodes of hypertension, palpitations, and sweating.
- While sweating and hypertension are present, the absence of episodic symptoms and the long-term changes in body size make pheochromocytoma less likely.
*Increased serum testosterone*
- **Increased testosterone** in a male would typically lead to increased muscle mass, acne, and potentially male-pattern baldness, but not the specific skeletal and soft tissue growth patterns observed, such as increased shoe and glove size or prognathism.
- While some skin changes might occur, **hyperhidrosis** and the dramatic facial and extremity changes are not characteristic features of testosterone excess.
Impact of chronic disease on growth US Medical PG Question 3: A 5-year-old boy presents to the pediatrician for a well child visit. He is meeting his developmental milestones and is in the 15th percentile for height and 70th percentile for weight. His parents report that he complains of fatiguing easily and having trouble participating in sports. They are concerned he is not getting enough sleep and state that sometimes they hear him snore. The patient has a past medical history of a supracondylar fracture of the humerus, which was appropriately treated. He is doing well in school but is sometimes bullied for being small. The patient eats a balanced diet of milk, fruit, and some vegetables. His parents have been trying to get him to drink more milk so he can grow taller. His temperature is 99.5°F (37.5°C), blood pressure is 90/48 mmHg, pulse is 100/min, respirations are 19/min, and oxygen saturation is 98% on room air. On physical exam, the patient appears well. HEENT exam is notable for conjunctival pallor and a unilateral clear middle ear effusion. Cardiac exam reveals a benign flow murmur. Pulmonary exam is clear to auscultation bilaterally. The patient's gait is stable and he is able to jump up and down. A full set of labs are ordered as requested by the parents including a serum vitamin D level, B12 level, and IGF level. A selection of these lab values are seen below.
Serum:
Na+: 139 mEq/L
Cl-: 100 mEq/L
K+: 4.3 mEq/L
HCO3-: 25 mEq/L
BUN: 20 mg/dL
Glucose: 99 mg/dL
Creatinine: 1.1 mg/dL
Ca2+: 9.9 mg/dL
AST: 12 U/L
ALT: 10 U/L
Which of the following would you expect to find in this patient?
- A. Decreased IGF levels
- B. Increased RDW and TIBC (Correct Answer)
- C. Decreased oxygen saturation when the patient sleeps
- D. Increased MCV
- E. Decreased vitamin D level
Impact of chronic disease on growth Explanation: ***Increased RDW and TIBC***
- The patient presents with **conjunctival pallor**, fatigue, and snoring, falling in the 15th percentile for height and 70th for weight, suggesting **iron deficiency anemia**. Anemia would cause an **increased red cell distribution width (RDW)** as red blood cells vary in size, and **increased total iron-binding capacity (TIBC)** as the body tries to maximize iron absorption.
- While other signs of mild anemia like glossitis or pica are not explicitly mentioned, the combination of symptoms and the common prevalence of **iron-deficiency anemia** in children due to inadequate dietary intake or rapid growth phases supports this finding. Prolonged milk intake can inhibit iron absorption.
*Decreased IGF levels*
- **Insulin-like growth factor (IGF) levels** are primarily associated with growth hormone deficiency or severe malnutrition, which is not strongly indicated here. The patient's height is at the 15th percentile, which is *small*, but within the normal range, and his weight is at the 70th percentile, indicating he is not severely malnourished.
- While fatigue and small stature can be associated with growth disorders, the overall presentation with pallor points more distinctly towards an alternative diagnosis like **anemia** rather than growth hormone axis dysfunction.
*Decreased oxygen saturation when the patient sleeps*
- The patient's snoring could suggest **sleep-disordered breathing** or **sleep apnea**, leading to decreased oxygen saturation during sleep.
- However, based on the *conjunctival pallor*, fatigue, and growth concerns, **iron deficiency anemia** is a more prominent diagnosis, and while sleep apnea is possible, direct evidence of desaturation is not provided.
*Increased MCV*
- An **increased MCV (macrocytic anemia)** is characteristic of deficiencies in **vitamin B12** or **folate**.
- The patient's symptoms, particularly conjunctival pallor and fatigue, are more consistent with a **microcytic anemia** (decreased MCV), often caused by **iron deficiency**, rather than a macrocytic one.
*Decreased vitamin D level*
- While **fatigue** can be a symptom of **vitamin D deficiency**, the more prominent findings of **conjunctival pallor** and height/weight percentiles are less directly indicative of this specific deficiency as the primary diagnosis.
- The patient's diet
includes milk and fruit, which are typically fortified or contain vitamin D, making a severe deficiency less likely to be the primary cause of his symptoms, though a mild deficiency cannot be ruled out without specific lab results.
Impact of chronic disease on growth US Medical PG Question 4: An 8-month-old child presents with a history of poor growth and a chronic cough. He was born to a 21-year-old woman at 41 weeks of gestation. Soon after birth, he developed respiratory distress and was admitted to the neonatal intensive care unit where he was mechanically ventilated for 24 hours. He was initially breastfed, but due to frequent vomiting and loose bowel movements, he was formula fed thereafter. Despite this change, he continued to have loose, large, greasy, foul-smelling stools and failure to thrive. When physically examined, his temperature is 37.0°C (98.6°F), heart rate is 120/min, and blood pressure is 80/60 mm Hg. Oxygen saturation is 97% on room air and the baby's weight is 6.7 kg (14.8 lb, < 5th percentile). HEENT examination is significant for bilateral otitis media and mild nasal congestion. Normal breath sounds with mild wheezing and rales are heard. Which condition best explains this patient's clinical presentation?
- A. Celiac disease
- B. Shwachman-Diamond syndrome
- C. Cow's milk protein allergy
- D. Giardiasis
- E. Cystic fibrosis (Correct Answer)
Impact of chronic disease on growth Explanation: ***Cystic fibrosis***
- The constellation of **poor growth**, **chronic cough**, **respiratory distress** in the neonatal period needing ventilation, **recurrent infections** (otitis media), and classic gastrointestinal symptoms of **greasy, foul-smelling stools** and **failure to thrive** is highly suggestive of cystic fibrosis.
- The gastrointestinal symptoms are due to **pancreatic exocrine insufficiency**, where thick mucus blocks pancreatic ducts, preventing digestive enzymes from reaching the intestine, leading to **malabsorption of fats** and fat-soluble vitamins.
*Celiac disease*
- While celiac disease also presents with **malabsorption** and **failure to thrive**, it typically manifests after the introduction of **gluten-containing foods**, usually around 6-12 months of age.
- It does not explain the early **respiratory issues** or the recurrent infections seen in this patient.
*Shwachman-Diamond syndrome*
- This syndrome presents with **pancreatic exocrine insufficiency** and **bone marrow dysfunction** (neutropenia leading to recurrent infections), which could explain some symptoms.
- However, it typically lacks the prominent **respiratory findings** and chronic cough that are a hallmark of cystic fibrosis.
*Cow's milk protein allergy*
- This allergy often causes **vomiting, loose stools, and poor growth**, especially after formula feeding.
- However, it does not account for the **chronic cough**, **respiratory distress at birth**, or the **greasy, foul-smelling nature of the stools**, which points more specifically to fat malabsorption.
*Giardiasis*
- This parasitic infection can cause **diarrhea, abdominal cramps, and malabsorption**, leading to **poor growth**, especially in children in daycare settings.
- It would not explain the **neonatal respiratory distress**, **chronic cough**, or recurrent upper respiratory infections described in the patient.
Impact of chronic disease on growth US Medical PG Question 5: A concerned mother presents to clinic stating that her 14-year-old son has not gone through his growth spurt. She states that, although shorter, he had been growing at the same rate as his peers until the past year. There is no evidence of delayed puberty in the mother, but the father's history is unknown. The patient has no complaints. On physical exam, the patient is a healthy-appearing 14-year-old boy whose height is below the third percentile and whose weight is at the 50th percentile. His bone age is determined to be 11 years. A laboratory workup, including thyroid stimulating hormone (TSH), is unremarkable. What is the most likely diagnosis?
- A. Hypothyroidism
- B. Familial short stature
- C. Constitutional growth delay (Correct Answer)
- D. Growth hormone deficiency
- E. Celiac disease
Impact of chronic disease on growth Explanation: ***Constitutional growth delay***
- This condition is characterized by **delayed bone age**, normal growth velocity initially followed by a deceleration, and an eventual **catch-up growth spurt** leading to normal adult height. The patient's history of being shorter than peers but growing at the same rate, followed by a recent slow down, and a bone age of 11 years (compared to his chronological age of 14) strongly indicates this.
- The absence of other symptoms, **unremarkable lab workup** (including TSH), and the fact that he was previously growing at the same rate as peers further supports constitutional growth delay, which is often linked to a family history of delayed puberty, even if the mother's history is negative and the father's is unknown.
*Hypothyroidism*
- **Hypothyroidism** would typically present with symptoms such as fatigue, weight gain, constipation, and cold intolerance, none of which are mentioned in the patient's history.
- The **unremarkable TSH** level rules out hypothyroidism as the cause of growth delay in this case.
*Familial short stature*
- In **familial short stature**, children typically grow along a short but otherwise normal percentile curve, and their bone age would typically match their chronological age.
- The patient's growth deceleration and significantly **delayed bone age** are inconsistent with familial short stature.
*Growth hormone deficiency*
- **Growth hormone deficiency** often presents with a significant deceleration of growth velocity and very short stature for age, but usually the bone age delay is more pronounced or proportional to the chronological age.
- While low height is present, the **otherwise healthy appearance** and absence of other metabolic or health issues make constitutional growth delay more likely, especially with the provided bone age and normal lab results.
*Celiac disease*
- **Celiac disease** can cause growth delay, but it would typically be accompanied by gastrointestinal symptoms such as abdominal pain, diarrhea, or malabsorption-related issues like weight loss or anemia.
- This patient is **asymptomatic** and has a normal weight for his height percentiles, which makes celiac disease an unlikely diagnosis.
Impact of chronic disease on growth US Medical PG Question 6: An 8-year-old boy presents to his pediatrician for a well visit. His parents state that he has been doing well in school and has many friends. The patient is a member of the chess club and enjoys playing video games. He has a past medical history of asthma which is treated with albuterol. The patient is in the 99th percentile for weight and 30th percentile for height. His temperature is 99.5°F (37.5°C), blood pressure is 122/88 mmHg, pulse is 90/min, respirations are 11/min, and oxygen saturation is 98% on room air. The patient's body mass index is 39.1 kg/m^2 at this visit. On physical exam, you note a young boy who maintains eye contact and is excited to be at the doctor's office. Cardiopulmonary exam is within normal limits. Abdominal exam reveals normal bowel sounds and is non-tender in all 4 quadrants. Neurological and musculoskeletal exams are within normal limits. Which of the following is the most likely outcome in this patient?
- A. Constitutional growth delay
- B. Precocious puberty
- C. Hypertension
- D. Slipped capital femoral epiphysis (Correct Answer)
- E. Atherosclerotic heart disease
Impact of chronic disease on growth Explanation: ***Slipped capital femoral epiphysis***
- The patient's **obesity** (BMI 39.1 kg/m^2, 99th percentile for weight) is a significant risk factor for **slipped capital femoral epiphysis (SCFE)**, especially during periods of rapid growth.
- SCFE presents with hip, groin, thigh, or knee pain and a limp, often requiring emergency surgical intervention to prevent further slippage and complications like avascular necrosis.
*Constitutional growth delay*
- This condition is characterized by **short stature** and delayed puberty, usually with a family history of delayed growth spurts.
- While it involves growth, it does not explain the patient's obesity or increased risk of musculoskeletal complications associated with it.
*Precocious puberty*
- Precocious puberty is defined by the onset of secondary sexual characteristics before age 8 in girls or age 9 in boys.
- While obesity can be a risk factor for earlier puberty, it is not the most immediate or likely outcome given the clinical scenario, and there are no signs of puberty mentioned.
*Hypertension*
- The patient's blood pressure (122/88 mmHg) is elevated for an 8-year-old and indicative of **hypertension**, a common comorbidity of obesity.
- However, while present, hypertension is a *current finding* and comorbidity, not a *future outcome* in the same immediate risk category as SCFE for an obese child of this age.
*Atherosclerotic heart disease*
- While obesity in childhood increases the long-term risk of **atherosclerotic heart disease**, this is a chronic process that develops over many years, typically manifesting in adulthood.
- It is a long-term consequence rather than the *most likely immediate outcome* during childhood, unlike conditions directly precipitated by childhood obesity.
Impact of chronic disease on growth US Medical PG Question 7: An 18-month-old boy is brought to the physician by his mother because of concern that he has not yet begun to walk. He was born at term and exclusively breastfed until 15 months of age. His mother says he has been well, apart from an episode of high fever and seizure 4 months ago for which she did not seek medical attention. He has an older brother who is currently receiving medical treatment for failure to thrive. His parents have no history of serious illness; they are of normal height. His last vaccine was at the age of 4 months. He is at the 20th percentile for length, 10th percentile for weight, and 50th percentile for head circumference. Physical examination shows dry mucous membranes and erosion of the enamel on the lingual surface of the incisors and carious molars. He has frontal bossing. His wrists are widened, his legs seem bent, and there is beading of the ribs. Which of the following is the most likely underlying cause of this patient's delay in walking?
- A. Deficiency of osteoclasts to reabsorb bone
- B. Osteoid proliferation in the subperiosteal bone
- C. Defect in type I collagen
- D. Mutation of fibroblast growth factor receptor 3
- E. Defective growth plate mineralization (Correct Answer)
Impact of chronic disease on growth Explanation: ***Defective growth plate mineralization***
- The patient's symptoms, including **delayed walking**, **frontal bossing**, **widened wrists**, **bowed legs** (bent legs), and **rachitic rosary** (beading of the ribs), are classic signs of **rickets**.
- **Rickets** is caused by a deficiency of vitamin D, leading to impaired mineralization of the cartilage and newly formed bone at the growth plates, resulting in soft and weak bones. The prolonged **exclusive breastfeeding** in this case, without vitamin D supplementation, increases the risk.
*Deficiency of osteoclasts to reabsorb bone*
- This describes conditions like **osteopetrosis** (Albers-Schonberg disease), which typically presents with **dense, brittle bones**, prone to fractures, and often associated with **bone marrow failure**.
- While osteopetrosis can cause skeletal deformities and delayed milestones, the specific findings of widened wrists, bowed legs, and rachitic rosary are not characteristic of osteopetrosis, which involves increased bone density.
*Osteoid proliferation in the subperiosteal bone*
- This is a feature of conditions like **secondary hyperparathyroidism** or some bone tumors, which do not typically present with the widespread skeletal deformities and growth plate abnormalities seen in rickets.
- While it can lead to bone pain and fragility, it does not explain the characteristic signs of rickets, such as widened growth plates and bone softening.
*Defect in type I collagen*
- A defect in type I collagen is characteristic of **osteogenesis imperfecta**, a genetic disorder leading to **brittle bones** that are prone to frequent fractures.
- Patients with osteogenesis imperfecta often have **blue sclerae** and **dentinogenesis imperfecta** (which can cause dental issues, but not specifically enamel erosion and caries in the manner described), but not the specific rickets-like skeletal deformities.
*Mutation of fibroblast growth factor receptor 3*
- A mutation in **fibroblast growth factor receptor 3 (FGFR3)** causes **achondroplasia**, the most common form of dwarfism.
- Achondroplasia is characterized by **short limbs**, a **normal trunk size**, and a **large head with frontal bossing**, but it does not cause the specific skeletal findings of widely spaced growth plates, bowed legs, and rachitic rosary associated with defective mineralization.
Impact of chronic disease on growth US Medical PG Question 8: A 57-year-old woman comes to the physician because of a 6-month history of tinnitus and progressive hearing loss in the left ear. She has type 2 diabetes mellitus and Raynaud syndrome. Her current medications include metformin, nifedipine, and a multivitamin. She appears well. Vital signs are within normal limits. Physical examination shows no abnormalities. A vibrating tuning fork is placed on the left mastoid process. Immediately after the patient does not hear a tone, the tuning fork is held over the left ear and she reports hearing the tuning fork again. The same test is repeated on the right side and shows the same pattern. The vibration tuning fork is then placed on the middle of the forehead and the patient hears the sound louder in the right ear. Which of the following is the most likely diagnosis?
- A. Acoustic neuroma (Correct Answer)
- B. Meningioma
- C. Cerumen impaction
- D. Ménière disease
- E. Presbycusis
Impact of chronic disease on growth Explanation: ***Acoustic neuroma***
- The patient presents with **unilateral tinnitus** and **progressive sensorineural hearing loss** in the left ear, which is a classic presentation of an acoustic neuroma.
- The **Rinne test** results (air conduction > bone conduction bilaterally) indicate **no conductive hearing loss**, while the **Weber test lateralizing to the right ear** confirms **sensorineural hearing loss in the left ear**.
*Meningioma*
- While a meningioma could present with neurological symptoms, it typically does not selectively cause **unilateral tinnitus** and **hearing loss** in this specific pattern without other focal neurological deficits.
- Meningiomas are usually **slow-growing** and would likely present with mass effect symptoms, such as headache or seizures, depending on their location, which are not described here.
*Cerumen impaction*
- **Cerumen impaction** would cause a **conductive hearing loss**, where bone conduction would be *louder* than air conduction on the Rinne test (BC > AC).
- The patient's Rinne test results (AC > BC) are consistent with **sensorineural hearing loss**, not conductive.
*Ménière disease*
- **Ménière disease** is characterized by episodic **vertigo, tinnitus, fluctuating hearing loss**, and aural fullness.
- The patient's symptoms are primarily **progressive hearing loss** and constant tinnitus, without the episodic vertigo typical of Ménière disease.
*Presbycusis*
- **Presbycusis** is **age-related bilateral sensorineural hearing loss**, typically symmetric and affecting high frequencies.
- The patient's symptoms are **unilateral** (affecting the left ear predominantly) and present with specific tuning fork findings that point to a localized lesion rather than general aging.
Impact of chronic disease on growth US Medical PG Question 9: A pathologist receives a skin biopsy specimen from a patient who is suspected to have developed graft-versus-host disease (GVHD) following allogeneic stem-cell transplantation. The treating physician informs the pathologist that he is specifically concerned about the diagnosis as the patient developed skin lesions on the 90th-day post-transplantation and therefore, by definition, it should be considered a case of acute GVHD. However, the lesions clinically appear like those of chronic GVHD. The pathologist examines the slide under the microscope and confirms the diagnosis of chronic GVHD. Which of the following findings on skin biopsy is most likely to have helped the pathologist to confirm the diagnosis?
- A. Complete separation of the dermis and epidermis
- B. Focal vacuolization in the basal cell layer
- C. Lymphocytic infiltration of the superficial dermis
- D. Hypergranulosis (Correct Answer)
- E. Diffuse vacuolization in the basal cell layer
Impact of chronic disease on growth Explanation: ***Hypergranulosis***
- The presence of **hypergranulosis** (thickening of the granular layer) is a characteristic histological feature often seen in **chronic graft-versus-host disease (GVHD)**, especially in the sclerodermoid variant.
- This finding, along with other changes like epidermal atrophy and dermal fibrosis, helps differentiate chronic GVHD from acute forms.
*Complete separation of the dermis and epidermis*
- **Dermal-epidermal separation** (e.g., **subepidermal bullae**) is characteristic of severe acute GVHD (grade III-IV), indicating extensive tissue damage.
- It is not a typical feature of chronic GVHD, and its presence would suggest a more acute process.
*Focal vacuolization in the basal cell layer*
- **Focal vacuolization** and **dyskeratosis** (apoptotic keratinocytes) in the basal layer are classic microscopic signs of **acute graft-versus-host disease (GVHD)**.
- While some basal layer changes can occur in chronic GVHD, focal involvement specifically points towards an acute process rather than chronic features.
*Lymphocytic infiltration of the superficial dermis*
- **Lymphocytic infiltrate** in the superficial dermis is present in both acute and chronic GVHD, making it a **non-specific finding** for differentiating between the two.
- More specific features are needed to confirm a diagnosis of chronic GVHD.
*Diffuse vacuolization in the basal cell layer*
- Diffuse **vacuolar degeneration** of the basal cell layer is also a hallmark of **acute graft-versus-host disease (GVHD)**, indicating early epidermal damage.
- This feature points towards an acute process rather than the typical changes observed in chronic GVHD.
Impact of chronic disease on growth US Medical PG Question 10: A 55-year-old man comes to the physician because of episodic retrosternal chest pain and shortness of breath for the past 6 months. His symptoms occur when he takes long walks or climbs stairs but resolve promptly with rest. He has a history of chronic obstructive pulmonary disease, for which he takes ipratropium bromide. His pulse is 81/min and blood pressure is 153/82 mm Hg. Physical examination shows mild expiratory wheezing over both lungs. Additional treatment with a beta blocker is considered. Which of the following agents should be avoided in this patient?
- A. Betaxolol
- B. Esmolol
- C. Bisoprolol
- D. Atenolol
- E. Labetalol (Correct Answer)
Impact of chronic disease on growth Explanation: ***Labetalol***
- **Labetalol** is a **non-selective beta-blocker** with additional **alpha-1 blocking activity**.
- Its **non-selective beta-blocking** effects can exacerbate **bronchoconstriction** in patients with **COPD**, leading to worsening respiratory symptoms.
*Betaxolol*
- **Betaxolol** is a **beta-1 selective blocker (cardioselective)**, meaning it primarily targets the heart.
- While no beta-blocker is entirely safe in **COPD**, cardioselective agents are generally preferred due to their reduced risk of **bronchospasm**.
*Esmolol*
- **Esmolol** is an **ultra-short-acting**, **beta-1 selective blocker** often used for acute cardiac conditions.
- Its **cardioselective nature** and rapid metabolism make it relatively safer in patients with **COPD** compared to non-selective agents.
*Bisoprolol*
- **Bisoprolol** is a **highly beta-1 selective blocker** commonly used for chronic cardiac conditions.
- Its high **cardioselectivity** minimizes its impact on **bronchial beta-2 receptors**, making it a safer option for patients with **COPD**.
*Atenolol*
- **Atenolol** is a **beta-1 selective blocker** used for conditions like hypertension and angina.
- Like other cardioselective beta-blockers, it has a lower risk of causing **bronchoconstriction** in patients with **COPD** compared to non-selective agents.
More Impact of chronic disease on growth US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.