Growth hormone disorders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Growth hormone disorders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Growth hormone disorders US Medical PG Question 1: A 5-year-old boy is brought to the physician for excessive weight gain. The mother reports that her son has been “chubby” since he was a toddler and that he has gained 10 kg (22 lbs) over the last year. During this period, he fractured his left arm twice from falling on the playground. He had cryptorchidism requiring orchiopexy at age 2. He is able to follow 1-step instructions and uses 2-word sentences. He is at the 5th percentile for height and 95th percentile for weight. Vital signs are within normal limits. Physical examination shows central obesity. There is mild esotropia and coarse, dry skin. In addition to calorie restriction, which of the following is the most appropriate next step in management of this patient?
- A. Levothyroxine
- B. Fluoxetine
- C. Laparoscopic gastric banding
- D. Growth hormone therapy (Correct Answer)
- E. Octreotide
Growth hormone disorders Explanation: ***Growth hormone therapy***
- This patient's constellation of symptoms, including **obesity**, **short stature**, developmental delay (**1-step instructions, 2-word sentences at age 5**), **cryptorchidism**, and **bone fractures**, is highly suggestive of **Prader-Willi syndrome (PWS).**
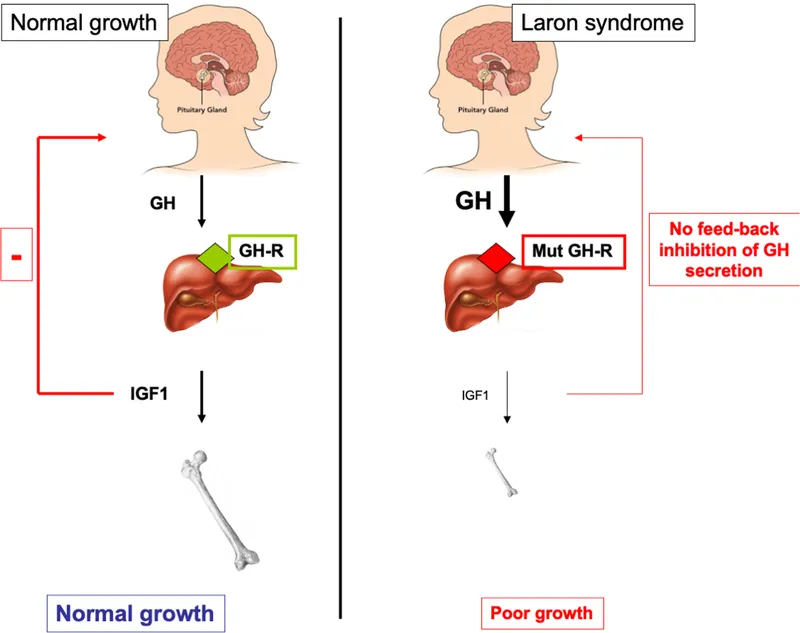
- **Growth hormone therapy** is the most appropriate next step and is crucial for improving growth, body composition, muscle strength, and bone density in patients with Prader-Willi syndrome.
- Growth hormone therapy should be initiated in early childhood and has been shown to significantly improve height, lean body mass, and motor development in PWS patients.
- **Note:** While PWS is associated with hypogonadism, testosterone replacement is not initiated at age 5; it is typically reserved for adolescent males approaching puberty.
*Levothyroxine*
- While **coarse, dry skin** can suggest **hypothyroidism**, the overall clinical picture, including developmental delay, cryptorchidism, hyperphagia with obesity, and short stature, is classic for **Prader-Willi syndrome** rather than primary hypothyroidism.
- There are no other clear signs of hypothyroidism such as bradycardia, lethargy, or significant goiter.
*Fluoxetine*
- **Fluoxetine** is an SSRI that may be used for behavioral issues like hyperphagia, compulsive behaviors, or anxiety often seen in Prader-Willi syndrome, but it does **not address the underlying hormonal deficiencies** or growth failure.
- Behavioral management and psychiatric medications are adjunctive but secondary to addressing the growth and metabolic issues with hormone therapy.
*Laparoscopic gastric banding*
- This is a surgical option for severe, refractory obesity, but it is **not appropriate for a 5-year-old child**, especially not as a first-line treatment for obesity in Prader-Willi syndrome.
- The **underlying hormonal and metabolic issues** must be addressed first with growth hormone therapy and dietary management, and such invasive bariatric procedures carry significant risks and are not indicated in young children.
*Octreotide*
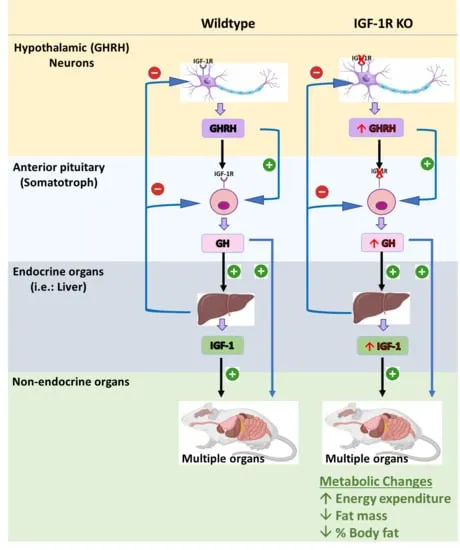
- **Octreotide** is a somatostatin analog used to inhibit growth hormone secretion in conditions like acromegaly or to manage symptoms of neuroendocrine tumors.
- In Prader-Willi syndrome, the issue is **growth hormone deficiency**, not excess, making octreotide contraindicated as it would worsen the growth failure.
Growth hormone disorders US Medical PG Question 2: A 45 year-old gentleman presents to his primary care physician complaining of wrist pain and is diagnosed with carpal tunnel syndrome. Upon further questioning, the patient admits that he has recently been outgrowing his gloves and shoes and has had to purchase a new hat as well due to increased head size. Upon exam, he is found to have new mild hypertension and on basic labs he is found to be hyperglycemic. Which of the following is the best blood test to diagnose his suspected disorder?
- A. Hydroxyproline level
- B. Cortisol level
- C. Alkaline Phosphatase level
- D. IGF-1 level (Correct Answer)
- E. Growth Hormone level
Growth hormone disorders Explanation: ***IGF-1 level***
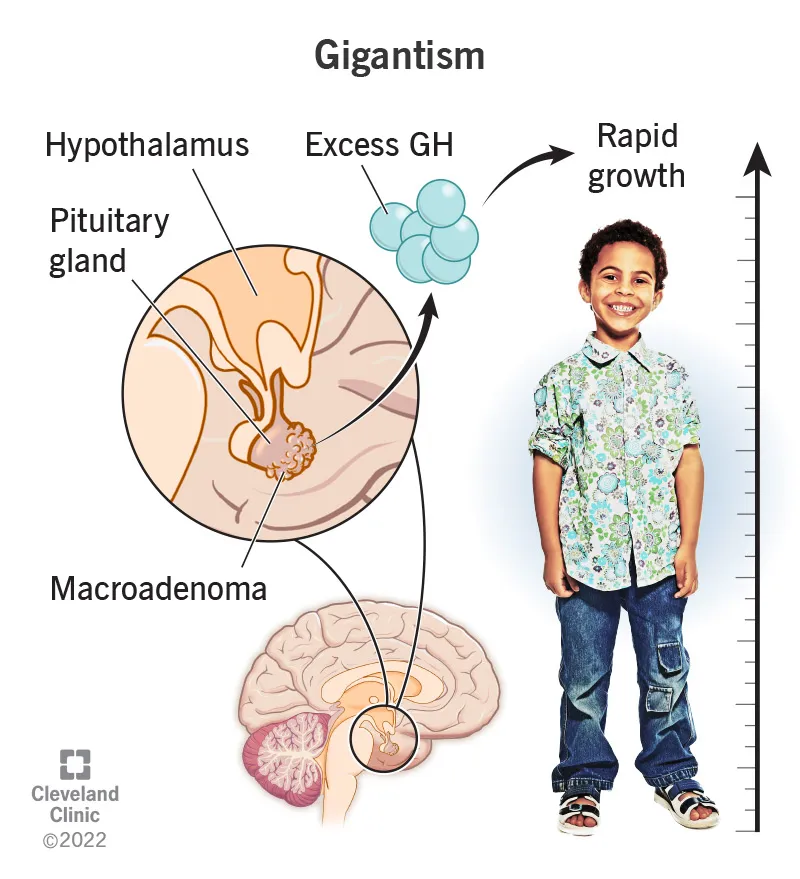
- The patient's symptoms of increased glove, shoe, and hat size, along with carpal tunnel syndrome, hypertension, and hyperglycemia, are highly suggestive of **acromegaly**.
- **IGF-1 (Insulin-like Growth Factor 1)** levels are generally stable throughout the day and are directly correlated with average growth hormone (GH) levels, making it the **best initial screening test** for acromegaly.
*Growth Hormone level*
- While acromegaly is caused by **excess growth hormone**, a single random GH level can be misleading due to its **pulsatile secretion**.
- A more definitive diagnostic test for acromegaly involves a **glucose suppression test** by measuring GH levels after an oral glucose load, but IGF-1 is the preferred initial screening.
*Hydroxyproline level*
- **Hydroxyproline** is an amino acid primarily found in **collagen** and its urinary excretion can indicate collagen turnover.
- It is not a primary diagnostic marker for acromegaly and is more relevant in conditions involving bone metabolism or collagen degradation.
*Cortisol level*
- **Cortisol** is a steroid hormone associated with stress response and conditions like **Cushing's syndrome** or **Addison's disease**.
- While acromegaly can sometimes coexist with other pituitary disorders, cortisol levels are not the most appropriate initial test for the suspected diagnosis of acromegaly.
*Alkaline Phosphatase level*
- **Alkaline phosphatase (ALP)** is an enzyme found in various tissues, including bone, liver, and kidneys.
- Elevated ALP typically indicates **bone turnover** (e.g., Paget's disease, osteomalacia) or liver disease, and is not a specific diagnostic marker for acromegaly.
Growth hormone disorders US Medical PG Question 3: A 42-year-old man who is employed as a construction worker presents to his primary care physician with complaints of moderate headaches and profuse sweating. He reports the need to carry up to 3 additional shirt changes to work because they drench quickly even with tasks of low physical exertion. His coworkers have commented about his changing glove and boot sizes, which have increased at least 4 times since he joined the company 10 years ago. Physical examination is unremarkable except for blood pressure of 160/95 mm Hg, hyperhidrosis, noticeably large pores, hypertrichosis, widely spaced teeth, and prognathism. Which of the following best explains the patient’s clinical manifestations?
- A. Increased serum cortisol
- B. Increased thyroid-stimulating hormone
- C. Increased serum metanephrines
- D. Increased serum insulin-like growth factor 1 (IGF-1) (Correct Answer)
- E. Increased serum testosterone
Growth hormone disorders Explanation: ***Increased serum insulin-like growth factor 1 (IGF-1)***
- Elevated **IGF-1** levels are indicative of **acromegaly**, a condition caused by excess growth hormone (GH) secretion, which explains the gradual changes in glove and boot sizes, prognathism, widely spaced teeth, and large pores.
- The symptoms of **profuse sweating**, **hypertrichosis**, **headaches**, and **hypertension** are common clinical manifestations of acromegaly due to the systemic effects of chronic GH excess.
*Increased serum cortisol*
- **Increased cortisol** (Cushing's syndrome) would present with central obesity, moon facies, buffalo hump, and striae, which are not described in the patient.
- While hypertension and hyperhidrosis can occur in Cushing's, the characteristic physical changes related to growth are absent.
*Increased thyroid-stimulating hormone*
- Elevated **TSH** suggests **hypothyroidism**, which would typically cause fatigue, weight gain, cold intolerance, and bradycardia, rather than profuse sweating and hypertension.
- **Hyperthyroidism** (low TSH, high thyroid hormones) can cause sweating and hypertension, but it would not explain the gradual increase in body and appendage size.
*Increased serum metanephrines*
- Elevated **metanephrines** are a hallmark of **pheochromocytoma**, which typically presents with paroxysmal episodes of hypertension, palpitations, and sweating.
- While sweating and hypertension are present, the absence of episodic symptoms and the long-term changes in body size make pheochromocytoma less likely.
*Increased serum testosterone*
- **Increased testosterone** in a male would typically lead to increased muscle mass, acne, and potentially male-pattern baldness, but not the specific skeletal and soft tissue growth patterns observed, such as increased shoe and glove size or prognathism.
- While some skin changes might occur, **hyperhidrosis** and the dramatic facial and extremity changes are not characteristic features of testosterone excess.
Growth hormone disorders US Medical PG Question 4: A 40-year-old woman visits her physician’s office with her husband. Her husband says that she has been complaining of recurring headaches over the past few months. A year ago she was diagnosed with diabetes and is currently on treatment for it. About 6 months ago, she was diagnosed with high blood pressure and is also taking medication for it. Her husband is concerned about the short span during which she has been getting all these symptoms. He also says that she occasionally complains of changes and blurring in her vision. In addition to all these complaints, he has observed changes in her appearance, more prominently her face. Her forehead and chin seem to be protruding more than usual. Suspecting a hormonal imbalance, which of the following initial tests would the physician order to indicate a possible diagnosis?
- A. Chest X-ray
- B. Pituitary magnetic resonance image (MRI)
- C. Serum growth hormone
- D. Glucose suppression test
- E. Serum insulin-like growth factor-1 (IGF-1) (Correct Answer)
Growth hormone disorders Explanation: ***Serum insulin-like growth factor-1 (IGF-1)***
- Elevated **serum IGF-1 levels** are the most sensitive and reliable initial screening test for **acromegaly**, reflecting sustained growth hormone excess.
- The clinical presentation with **new-onset diabetes**, **hypertension**, **headaches**, **visual changes**, and **facial prognathism** strongly suggests acromegaly, a condition caused by excessive growth hormone (GH) secretion.
*Chest X-ray*
- A chest X-ray is primarily used to evaluate **pulmonary or cardiac conditions** and would not directly screen for hormonal imbalances like acromegaly.
- While acromegaly can lead to **cardiomegaly** or **sleep apnea**, a chest X-ray is not the initial diagnostic test for growth hormone excess itself.
*Pituitary magnetic resonance image (MRI)*
- A **pituitary MRI** is the imaging study of choice to confirm the presence of a **pituitary adenoma** after biochemical confirmation of acromegaly, not an initial screening test.
- It visualizes the pituitary gland and helps locate the tumor but is ordered *after* biochemical tests indicate GH excess.
*Serum growth hormone*
- A single random **serum growth hormone (GH) level** can be misleading because GH secretion is pulsatile, making a single measurement unreliable for diagnosing acromegaly.
- While acromegaly involves elevated GH, a random sample is not the optimal initial diagnostic test due to its **fluctuating levels**.
*Glucose suppression test*
- The **oral glucose tolerance test (OGTT)** with GH measurement is the confirmatory test for acromegaly, used to demonstrate **failure of GH suppression** after glucose load.
- This is a diagnostic procedure performed *after* an elevated IGF-1 level suggests acromegaly, not an initial screening test.
Growth hormone disorders US Medical PG Question 5: A concerned mother presents to clinic stating that her 14-year-old son has not gone through his growth spurt. She states that, although shorter, he had been growing at the same rate as his peers until the past year. There is no evidence of delayed puberty in the mother, but the father's history is unknown. The patient has no complaints. On physical exam, the patient is a healthy-appearing 14-year-old boy whose height is below the third percentile and whose weight is at the 50th percentile. His bone age is determined to be 11 years. A laboratory workup, including thyroid stimulating hormone (TSH), is unremarkable. What is the most likely diagnosis?
- A. Hypothyroidism
- B. Familial short stature
- C. Constitutional growth delay (Correct Answer)
- D. Growth hormone deficiency
- E. Celiac disease
Growth hormone disorders Explanation: ***Constitutional growth delay***
- This condition is characterized by **delayed bone age**, normal growth velocity initially followed by a deceleration, and an eventual **catch-up growth spurt** leading to normal adult height. The patient's history of being shorter than peers but growing at the same rate, followed by a recent slow down, and a bone age of 11 years (compared to his chronological age of 14) strongly indicates this.
- The absence of other symptoms, **unremarkable lab workup** (including TSH), and the fact that he was previously growing at the same rate as peers further supports constitutional growth delay, which is often linked to a family history of delayed puberty, even if the mother's history is negative and the father's is unknown.
*Hypothyroidism*
- **Hypothyroidism** would typically present with symptoms such as fatigue, weight gain, constipation, and cold intolerance, none of which are mentioned in the patient's history.
- The **unremarkable TSH** level rules out hypothyroidism as the cause of growth delay in this case.
*Familial short stature*
- In **familial short stature**, children typically grow along a short but otherwise normal percentile curve, and their bone age would typically match their chronological age.
- The patient's growth deceleration and significantly **delayed bone age** are inconsistent with familial short stature.
*Growth hormone deficiency*
- **Growth hormone deficiency** often presents with a significant deceleration of growth velocity and very short stature for age, but usually the bone age delay is more pronounced or proportional to the chronological age.
- While low height is present, the **otherwise healthy appearance** and absence of other metabolic or health issues make constitutional growth delay more likely, especially with the provided bone age and normal lab results.
*Celiac disease*
- **Celiac disease** can cause growth delay, but it would typically be accompanied by gastrointestinal symptoms such as abdominal pain, diarrhea, or malabsorption-related issues like weight loss or anemia.
- This patient is **asymptomatic** and has a normal weight for his height percentiles, which makes celiac disease an unlikely diagnosis.
Growth hormone disorders US Medical PG Question 6: A 5-year-old boy is brought to the emergency department by a neighbor who saw him struck by a car. The man reports that the boy is intellectually disabled, and his parents frequently leave him unattended at home for most of the day. He walks around the neighborhood and sometimes has difficulty finding his way home. Today he was struck by a car that sped off. The man called the boy’s mother by phone, but she said that she was too busy to leave her job and asked the man to take the boy to the emergency department for her. A quick review of the boy's electronic medical record reveals that he has not been seen by a physician in several years and has missed several vaccines. On physical exam, the vital signs are normal. He appears dirty, thin, and small for his age with a large bruise forming on his right hip. Which of the following is the most appropriate term for this type of child abuse?
- A. Psychological abuse
- B. Factitious disorder
- C. Physical abuse
- D. Sexual abuse
- E. Neglect (Correct Answer)
Growth hormone disorders Explanation: ***Neglect***
- The parents' failure to provide adequate supervision, medical care (missed vaccines, no physician visits), and basic needs (appears dirty, thin, small for age) for the intellectually disabled child despite being able to do so, constitutes **neglect**.
- Their refusal to come to the ED and leaving him unattended further supports the diagnosis of **neglect**.
*Psychological abuse*
- This involves behaviors that harm a child's **self-worth** or **emotional well-being**, such as constant criticism, threats, or terrorizing.
- While emotional harm may be present due to neglect, the primary and most comprehensive description of the actions is neglect of basic needs and care.
*Factitious disorder*
- This is a mental disorder where an individual fakes or induces illness in themselves or someone else (often a child, known as **Factitious Disorder Imposed on Another**) for attention or sympathy.
- The scenario describes a failure of care rather than a deliberate fabrication or induction of illness.
*Physical abuse*
- This involves causing **physical harm** to a child, such as hitting, burning, or shaking. The large bruise on the hip is a sign of injury, but the *cause* is being struck by a car, not direct parental physical harm.
- While a bruise is present, the overall pattern of parental behavior points to a failure to protect and care rather than direct infliction of injury by the parents on the child.
*Sexual abuse*
- This involves any sexual act or exploitation of a child by an adult.
- There are **no indicators** in the provided scenario to suggest sexual abuse.
Growth hormone disorders US Medical PG Question 7: A 1-year-old male presents to his pediatrician for a well-child visit. Through a history from the mother and physical examination, the pediatrician learns that the baby babbles non-specifically, takes several steps independently, and picks up his cereal using two fingers. His weight is currently 22 lbs (birth-weight 6 lbs, 9 oz), and his height is 30 inches (birth length 18 inches). Are there any aspects of this child's development that are delayed?
- A. Fine motor skill delay
- B. Language delay (Correct Answer)
- C. Inadequate growth
- D. Gross motor skill delay
- E. There are no developmental concerns
Growth hormone disorders Explanation: ***Language delay***
- At 1 year of age, a child should typically be babbling with **specific sounds** and attempting to say their **first words**.
- The child's non-specific babbling suggests a delay in typical **expressive language development**.
*Fine motor skill delay*
- The child is able to pick up cereal using **two fingers**, indicating the development of a **pincer grasp**.
- This is an **age-appropriate fine motor skill** for a 1-year-old.
*Inadequate growth*
- The child has over **tripled his birth weight** (from 6 lbs, 9 oz to 22 lbs) and more than doubled his birth length (from 18 to 30 inches), which are **normal growth patterns** for the first year of life.
- While weight values can be plotted on growth charts, the provided information strongly suggests **adequate growth**.
*Gross motor skill delay*
- The child is taking **several steps independently**, which is an **age-appropriate gross motor milestone** for a 1-year-old.
- Many children take their first independent steps between 9 and 15 months.
*There are no developmental concerns*
- While many milestones are met, the **non-specific babbling** at 1 year strongly suggests a **language delay**.
- It is crucial to identify and address any potential delays early for intervention.
Growth hormone disorders US Medical PG Question 8: Two hours after a 2280-g male newborn is born at 38 weeks' gestation to a 22-year-old primigravid woman, he has 2 episodes of vomiting and jitteriness. The mother has noticed that the baby is not feeding adequately. She received adequate prenatal care and admits to smoking one pack of cigarettes daily while pregnant. His temperature is 36.3°C (97.3°F), pulse is 171/min and respirations are 60/min. Pulse oximetry on room air shows an oxygen saturation of 92%. Examination shows pale extremities. There is facial plethora. Capillary refill time is 3 seconds. Laboratory studies show:
Hematocrit 70%
Leukocyte count 7800/mm3
Platelet count 220,000/mm3
Serum
Glucose 38 mg/dL
Calcium 8.3 mg/dL
Which of the following is the most likely cause of these findings?
- A. Intrauterine hypoxia (Correct Answer)
- B. Transient tachypnea of the newborn
- C. Hyperinsulinism
- D. Congenital heart disease
- E. Intraventricular hemorrhage
Growth hormone disorders Explanation: ***Intrauterine hypoxia***
- **Chronic intrauterine hypoxia** stimulates erythropoietin production, leading to **polycythemia** (Hct 70%) and **hyperviscosity**, which can cause poor feeding, vomiting, jitteriness, and circulatory disturbances like prolonged capillary refill and facial plethora.
- The mother's history of **smoking** during pregnancy is a significant risk factor for intrauterine hypoxia and **intrauterine growth restriction (IUGR)**, contributing to the newborn's small size for gestational age (2280g at 38 weeks).
*Transient tachypnea of the newborn*
- Characterized by **respiratory distress** due to delayed clearance of fetal lung fluid, presenting with tachypnea, grunting, and retractions.
- While this newborn has tachypnea (respirations 60/min), the primary symptoms point towards **hyperviscosity syndrome** and hypoglycemia, not primarily respiratory issues.
*Hyperinsulinism*
- This condition primarily causes **hypoglycemia** (glucose 38 mg/dL) due to excessive insulin production.
- However, it does not explain the presence of **polycythemia**, facial plethora, prolonged capillary refill, or the mother's smoking history.
*Congenital heart disease*
- Can cause symptoms like **cyanosis**, poor feeding, and tachypnea, and some forms could contribute to hypoxia.
- It does not directly explain the **polycythemia** or the mother's smoking history as a causal factor for all presenting signs.
*Intraventricular hemorrhage*
- Typically seen in **premature infants** and can cause neurological symptoms like lethargy, hypotonia, and seizures.
- While jitteriness can be a symptom, it does not account for the **polycythemia**, facial plethora, or improved feeding with interventions for hyperviscosity.
Growth hormone disorders US Medical PG Question 9: A 5-day-old male newborn is brought to the physician by his mother because of yellowish discoloration of the skin for 1 day. The discoloration first appeared on his face and then spread to his trunk. There have been no changes in his bowel habits or urination. He was born at 38 weeks' gestation via uncomplicated vaginal delivery. He is exclusively breastfed every 2–3 hours. Examination shows scleral icterus and jaundice of the face, chest, and abdomen. Laboratory studies show:
Hemoglobin 17.6 g/dL
Reticulocytes 0.3%
Maternal blood group A, Rh-negative
Fetal blood group 0, Rh-positive
Serum
Bilirubin, total 7 mg/dL
Direct 0.6 mg/dL
Free T4 12 μg/dL
Which of the following is the most likely diagnosis?
- A. Biliary atresia
- B. Dubin-Johnson syndrome
- C. Physiological neonatal jaundice (Correct Answer)
- D. Rhesus incompatibility
- E. Congenital hypothyroidism
Growth hormone disorders Explanation: ***Physiological neonatal jaundice***
- This newborn’s jaundice is **unconjugated (indirect) hyperbilirubinemia**, indicated by a total bilirubin of 7 mg/dL and a direct bilirubin of 0.6 mg/dL (direct bilirubin is less than 20% of total).
- The onset of jaundice after 24 hours of age (day 4-5), peak at 3-5 days, resolution within 1-2 weeks, and the absence of other concerning symptoms in an otherwise healthy term infant strongly suggest **physiological jaundice**.
*Biliary atresia*
- Characterized by **conjugated (direct) hyperbilirubinemia**, often with dark urine and pale stools, which are not present here.
- Typically presents later, around 2-4 weeks of age, and would show a higher direct bilirubin percentage.
*Dubin-Johnson syndrome*
- An **autosomal recessive disorder** causing conjugated hyperbilirubinemia due to a defect in bilirubin excretion into bile.
- Presents with a high proportion of **direct bilirubin**, not seen in this case.
*Rhesus incompatibility*
- Would cause **hemolytic anemia** with jaundice typically appearing within the first 24 hours of life and often severe.
- The **normal reticulocyte count (0.3%)** and stable hemoglobin (17.6 g/dL) rule out significant hemolysis.
*Congenital hypothyroidism*
- Can cause **prolonged unconjugated jaundice** (lasting beyond 2 weeks of age) due to delayed bilirubin conjugation.
- However, the free T4 level of 7 µg/dL (assuming it's a TSH newborn screen or a total T4 value given the units) is within or near the normal range, and jaundice in this case is not yet prolonged.
Growth hormone disorders US Medical PG Question 10: A 1-month-old girl presents to her pediatrician with her mother. The patient was born at 38 weeks gestation via Caesarian section for cervical incompetence. The patient’s mother has no complaints, although she notes that the child had a runny nose and cough for a few days last week. The patient’s mother endorses decreased appetite during the aforementioned illness which has now returned to baseline. The patient’s family history is significant for an older brother with glucose-6-phosphate dehydrogenase (G6PD) deficiency and a maternal uncle with cirrhosis secondary to chronic hepatitis B. On physical exam, the patient has scleral icterus and dark urine staining her diaper. Laboratory testing reveals the following:
Serum:
Na+: 137 mEq/L
Cl-: 102 mEq/L
K+: 4.2 mEq/L
HCO3-: 24 mEq/L
Urea nitrogen: 12 mg/dL
Glucose: 96 mg/dL
Creatinine: 0.36 mg/dL
Alkaline phosphatase: 146 U/L
Aspartate aminotransferase (AST): 86 U/L
Alanine aminotransferase (ALT): 76 U/L
Total bilirubin: 4.6 mg/dL
Direct bilirubin: 3.8 mg/dL
Which of the following is the most likely diagnosis?
- A. Increased production of bilirubin
- B. Increased enterohepatic circulation of bilirubin
- C. Decreased metabolism of bilirubin
- D. Obstruction of the extrahepatic biliary tree (Correct Answer)
- E. Obstruction of the intrahepatic biliary tree
Growth hormone disorders Explanation: ***Obstruction of the extrahepatic biliary tree***
- The elevated **direct bilirubin** (3.8 mg/dL out of 4.6 mg/dL total) in a 1-month-old, along with **scleral icterus** and **dark urine**, is highly suggestive of **biliary atresia**, which is an extrahepatic biliary obstruction.
- While other forms of cholestasis can occur, this presentation with significant direct hyperbilirubinemia in a young infant points strongly towards a structural issue in the extrahepatic bile ducts.
*Increased production of bilirubin*
- This would primarily cause an elevation in **unconjugated (indirect) bilirubin**, as the liver would conjugate it efficiently.
- The patient's lab results show a predominant elevation in **direct (conjugated) bilirubin**, making overproduction less likely as the primary cause.
*Increased enterohepatic circulation of bilirubin*
- This typically occurs in **physiologic jaundice** of the newborn, characterized by increased **unconjugated bilirubin** returning to the liver, often exacerbated by poor feeding.
- The predominance of **direct bilirubin** in this case rules out increased enterohepatic circulation as the main etiology.
*Decreased metabolism of bilirubin*
- Conditions causing decreased bilirubin metabolism, such as **Crigler-Najjar syndrome** or **Gilbert's syndrome**, primarily affect the **conjugation process**, leading to elevated **unconjugated bilirubin**.
- This patient presents with predominantly **conjugated hyperbilirubinemia**, indicating that conjugation is occurring but excretion is impaired.
*Obstruction of the intrahepatic biliary tree*
- While intrahepatic cholestasis can cause conjugated hyperbilirubinemia, conditions like **Alagille syndrome** or progressive familial intrahepatic cholestasis typically lack the complete obstruction seen in biliary atresia.
- Biliary atresia is a more common and severe cause of **extrahepatic obstruction** presenting similarly to this case, often requiring surgical intervention.
More Growth hormone disorders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.