Growth charts and interpretation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Growth charts and interpretation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Growth charts and interpretation US Medical PG Question 1: A 16-year-old teenager presents to the pediatrician with his mother. After she leaves the room he tells the physician that he is worried about puberty. All of his friends have had growth spurts, started building muscle mass, and their voices have changed while he still feels underdeveloped. The physician takes a complete history and performs a thorough physical examination. He goes through the patient’s past medical records and growth charts and notes physical findings documented over the last five years, concluding that the patient has delayed puberty. Which of the following findings supports his conclusion?
- A. The absence of testicular enlargement by age of 14 years (Correct Answer)
- B. The absence of an adult type of pubic hair distribution by age of 16 years
- C. The absence of linear growth acceleration by age of 13 years
- D. Presence of gynecomastia at age of 15 years
- E. The absence of penile enlargement by age of 12 years
Growth charts and interpretation Explanation: ***The absence of testicular enlargement by age of 14 years***
- The first reliable sign of male puberty is an increase in **testicular volume**, typically occurring by age 14.
- Absence of this by age 14 years indicates **delayed puberty** in males.
*The absence of an adult type of pubic hair distribution by age of 16 years*
- While pubic hair development is a sign of puberty, **adult-type distribution** (Tanner stage 5) by age 16 is normal for many.
- The definition of delayed puberty in males is typically based on the **absence of any secondary sexual characteristics** by age 14, or more specifically, testicular enlargement.
*The absence of linear growth acceleration by age of 13 years*
- The pubertal **growth spurt** typically occurs later in puberty, often around 13-14 years in males, following testicular enlargement.
- Its absence by age 13 might suggest early delay, but **testicular enlargement** is the primary diagnostic criterion.
*Presence of gynecomastia at age of 15 years*
- **Gynecomastia** can be a normal, transient finding during puberty due to temporary estrogen-androgen imbalance, not necessarily indicative of delayed puberty.
- Its presence doesn't rule out delayed puberty but isn't a direct sign of delay itself.
*The absence of penile enlargement by age of 12 years*
- **Penile enlargement** typically occurs after testicular enlargement.
- The absence of this by age 12 is less specific than **testicular enlargement by age 14** for defining delayed puberty.
Growth charts and interpretation US Medical PG Question 2: During the selection of subjects for a study on infantile vitamin deficiencies, a child is examined by the lead investigator. She is at the 75th percentile for head circumference and the 80th percentile for length and weight. She can lift her chest and shoulders up when in a prone position, but cannot roll over from a prone position. Her eyes follow objects past the midline. She coos and makes gurgling sounds. When the investigator strokes the sole of her foot, her big toe curls upward and there is fanning of her other toes. She makes a stepping motion when she is held upright and her feet are in contact with the examination table. Which of the following additional skills or behaviors would be expected in a healthy patient of this developmental age?
- A. Cries when separated from her mother
- B. Smiles at her mother (Correct Answer)
- C. Rolls over from her back
- D. Responds to calling of own name
- E. Reaches out for objects
Growth charts and interpretation Explanation: ***Smiles at her mother***
- The child exhibits developmental milestones consistent with a **2-month-old infant**, such as lifting her chest in a prone position, following objects past the midline, cooing, and gurgling. Social smiling typically emerges around **2 months of age**.
- Primitive reflexes like the **Babinski reflex** (big toe curling upward and fanning of other toes) and **stepping reflex** are normally present at this age, supporting the approximate age of 2 months.
*Cries when separated from her mother*
- This behavior suggests **separation anxiety**, which typically develops much later, usually around **8-9 months of age**.
- A 2-month-old infant does not yet have the cognitive understanding or object permanence needed to exhibit true separation anxiety.
*Rolls over from her back*
- Rolling over from the back to the stomach is usually achieved between **4 and 6 months of age**.
- The child in the vignette cannot even roll over from a prone position, indicating she is not yet at the age for rolling from her back.
*Responds to calling of own name*
- Responding to one's own name is a more advanced auditory and cognitive milestone, generally developing between **6 and 9 months of age**.
- At 2 months, infants respond to voices and sounds but do not associate specific words with themselves.
*Reaches out for objects*
- Purposeful reaching and grasping for objects (palmar grasp) typically develops around **4 to 6 months of age**.
- A 2-month-old infant may swat at objects reflexively but does not exhibit coordinated, intentional reaching.
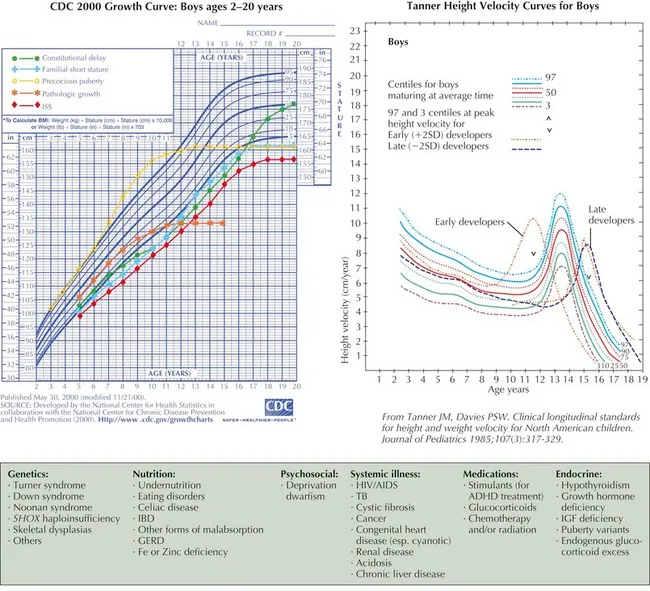
Growth charts and interpretation US Medical PG Question 3: A concerned mother presents to clinic stating that her 14-year-old son has not gone through his growth spurt. She states that, although shorter, he had been growing at the same rate as his peers until the past year. There is no evidence of delayed puberty in the mother, but the father's history is unknown. The patient has no complaints. On physical exam, the patient is a healthy-appearing 14-year-old boy whose height is below the third percentile and whose weight is at the 50th percentile. His bone age is determined to be 11 years. A laboratory workup, including thyroid stimulating hormone (TSH), is unremarkable. What is the most likely diagnosis?
- A. Hypothyroidism
- B. Familial short stature
- C. Constitutional growth delay (Correct Answer)
- D. Growth hormone deficiency
- E. Celiac disease
Growth charts and interpretation Explanation: ***Constitutional growth delay***
- This condition is characterized by **delayed bone age**, normal growth velocity initially followed by a deceleration, and an eventual **catch-up growth spurt** leading to normal adult height. The patient's history of being shorter than peers but growing at the same rate, followed by a recent slow down, and a bone age of 11 years (compared to his chronological age of 14) strongly indicates this.
- The absence of other symptoms, **unremarkable lab workup** (including TSH), and the fact that he was previously growing at the same rate as peers further supports constitutional growth delay, which is often linked to a family history of delayed puberty, even if the mother's history is negative and the father's is unknown.
*Hypothyroidism*
- **Hypothyroidism** would typically present with symptoms such as fatigue, weight gain, constipation, and cold intolerance, none of which are mentioned in the patient's history.
- The **unremarkable TSH** level rules out hypothyroidism as the cause of growth delay in this case.
*Familial short stature*
- In **familial short stature**, children typically grow along a short but otherwise normal percentile curve, and their bone age would typically match their chronological age.
- The patient's growth deceleration and significantly **delayed bone age** are inconsistent with familial short stature.
*Growth hormone deficiency*
- **Growth hormone deficiency** often presents with a significant deceleration of growth velocity and very short stature for age, but usually the bone age delay is more pronounced or proportional to the chronological age.
- While low height is present, the **otherwise healthy appearance** and absence of other metabolic or health issues make constitutional growth delay more likely, especially with the provided bone age and normal lab results.
*Celiac disease*
- **Celiac disease** can cause growth delay, but it would typically be accompanied by gastrointestinal symptoms such as abdominal pain, diarrhea, or malabsorption-related issues like weight loss or anemia.
- This patient is **asymptomatic** and has a normal weight for his height percentiles, which makes celiac disease an unlikely diagnosis.
Growth charts and interpretation US Medical PG Question 4: A 7-year-old boy is brought to the physician because his parents are concerned about his early sexual development. He has no history of serious illness and takes no medications. His brother was diagnosed with testicular cancer 5 years ago and underwent a radical orchiectomy. The patient is at the 85th percentile for height and 70th percentile for weight. Examination shows greasy facial skin. There is coarse axillary hair. Pubic hair development is at Tanner stage 3 and testicular development is at Tanner stage 2. The remainder of the examination shows no abnormalities. An x-ray of the wrist shows a bone age of 10 years. Basal serum luteinizing hormone and follicle-stimulating hormone are elevated. An MRI of the brain shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Leuprolide therapy (Correct Answer)
- B. Testicular ultrasound
- C. Cortisol supplementation
- D. Radiation therapy
- E. Observation
Growth charts and interpretation Explanation: ***Leuprolide therapy***
- This patient presents with **central precocious puberty** (CPP), indicated by elevated **basal LH and FSH levels** in the context of advanced bone age, Tanner stage 3 pubic hair, and Tanner stage 2 testicular development at a young age.
- **Leuprolide** is a GnRH analog that, when given continuously, downregulates the pituitary's GnRH receptors, suppressing gonadotropin release and halting pubertal progression. This is the appropriate treatment for CPP.
*Testicular ultrasound*
- While useful for evaluating testicular size and consistency, it is typically performed when there is suspicion of **peripheral precocious puberty** (e.g., Leydig cell tumor) with low LH/FSH or significant testicular asymmetry, which is not the primary presentation here.
- The elevated basal LH and FSH values indicate a **central origin** of puberty, making a testicular ultrasound less immediately relevant as a *next step* compared to directly addressing the central hormonal drive.
*Cortisol supplementation*
- This would be indicated for conditions causing **adrenal insufficiency**, such as **congenital adrenal hyperplasia (CAH)** with salt-wasting or Addison's disease.
- CAH typically presents with virilization and advanced bone age but would show **low LH/FSH** (due to peripheral androgen excess) and elevated adrenal androgens (e.g., DHEA-S, 17-hydroxyprogesterone), which are not described.
*Radiation therapy*
- This is a treatment for **malignant tumors**, often used in cases of brain tumors.
- The MRI of the brain showed **no abnormalities**, ruling out a pituitary or hypothalamic tumor as the cause of CPP in this case, thus making radiation therapy inappropriate.
*Observation*
- **Observation** alone is inappropriate given the significant **advancement of bone age** (10 years in a 7-year-old) and clear signs of central precocious puberty.
- Untreated CPP can lead to **compromised adult height potential** due to premature epiphyseal fusion and psychosocial issues, necessitating intervention.
Growth charts and interpretation US Medical PG Question 5: A 6-year-old girl is brought to the pediatrician by her father for an annual physical examination. The father reports that the patient is a happy and healthy child, but he sometimes worries about her weight. He says that she is a “picky” eater and only wants chicken nuggets and French fries. He also notes some mild acne on her cheeks and forehead but thinks it’s because she “doesn’t like baths.” The father says she has met all her pediatric milestones. She has recently started kindergarten, can tell time, and is beginning to read. Her teacher says she gets along with her classmates well. The patient was born at 38 weeks gestation. She has no chronic medical conditions and takes only a multivitamin. Height and weight are above the 95th percentile. Physical examination reveals scattered comedones on the patient’s forehead and bilateral cheeks. There is palpable breast tissue bilaterally with raised and enlarged areolae. Scant axillary hair and coarse pubic hair are also noted. A radiograph of the left hand shows a bone age of 9 years. Serum follicular stimulating hormone (FSH) level is 9.6 mU/mL (normal range 0.7-5.3 mU/mL) and luteinizing hormone (LH) level is 6.4 mU/mL (normal range < 0.26 mU/mL). Which of the following is the most appropriate diagnostic test?
- A. Pelvic ultrasound
- B. Estrogen levels
- C. 17-hydroxyprogesterone levels
- D. Dehydroepiandrosterone sulfate levels
- E. Brain magnetic resonance imaging (MRI) (Correct Answer)
Growth charts and interpretation Explanation: ***Brain magnetic resonance imaging (MRI)***
- The constellation of **precocious puberty** (breast development, pubic and axillary hair, advanced bone age) and **elevated FSH and LH levels** in a 6-year-old girl indicates central precocious puberty, which is often caused by a CNS lesion.
- **Brain MRI is the gold standard imaging** to rule out **hypothalamic hamartomas**, **gliomas**, **craniopharyngiomas**, or other structural abnormalities of the **hypothalamic-pituitary axis**.
- MRI provides superior soft tissue resolution without radiation exposure, making it the preferred modality in children.
*Pelvic ultrasound*
- A pelvic ultrasound is primarily used to evaluate **gonadal tumors** or cysts in cases of **peripheral precocious puberty**, where FSH and LH levels would be suppressed.
- Given the elevated FSH and LH, the puberty is central (gonadotropin-dependent), making CNS imaging more appropriate than ovarian imaging.
*Estrogen levels*
- While estrogen levels would certainly be elevated in this patient, measuring them would confirm sexual precocity but would not differentiate between **central** and **peripheral precocious puberty**.
- The **elevated FSH and LH levels** already indicate active gonadal stimulation, making direct estrogen measurement less informative for pinpointing the etiology.
*17-hydroxyprogesterone levels*
- Elevated 17-hydroxyprogesterone levels are indicative of **congenital adrenal hyperplasia (CAH)**, particularly the 21-hydroxylase deficiency.
- CAH typically causes signs of **virilization** (e.g., clitoromegaly) but not breast development, and would not cause elevated FSH and LH levels.
*Dehydroepiandrosterone sulfate levels*
- Elevated DHEAS levels suggest an **adrenal source of androgens**, which could contribute to **pubic and axillary hair growth** (adrenarche).
- However, DHEAS elevation alone would not explain the **breast development** and **elevated gonadotropins**, which point towards central precocious puberty.
Growth charts and interpretation US Medical PG Question 6: A 7-year-old girl is brought to the physician because of vaginal bleeding for 2 days. There is no personal or family history of serious illness. She is at the 95th percentile for height and at the 90th percentile for weight. Examination shows enlarged breasts, and the areola and papilla have formed a secondary mound. There is coarse pubic hair that does not extend to the inner thigh. The remainder of the examination show no abnormalities. An x-ray of the left hand and wrist shows a bone age of 11 years. Her serum luteinizing hormone concentration is 0.1 mIU/mL (N < 0.2 mIU/mL). Which of the following is the most appropriate next step in management?
- A. Serum dehydroepiandrosterone level
- B. Reassurance and follow-up
- C. Ultrasound of the pelvis
- D. GnRH stimulation test (Correct Answer)
- E. MRI of the brain
Growth charts and interpretation Explanation: ***GnRH stimulation test***
- This patient presents with signs of **precocious puberty** (vaginal bleeding, enlarged breasts, pubic hair, advanced bone age) but a **low basal LH level**. A **GnRH stimulation test** is crucial to differentiate between **central (gonadotropin-dependent)** and **peripheral (gonadotropin-independent)** precocious puberty.
- A significant rise in LH after GnRH administration indicates **central precocious puberty**, while a lack of significant response suggests **peripheral precocious puberty**.
*Serum dehydroepiandrosterone level*
- **DHEA** is a precursor to androgens and its elevation might indicate **adrenal causes** of precocious puberty (e.g., congenital adrenal hyperplasia, adrenal tumor).
- However, the prominent signs of **breast development** and **vaginal bleeding** point more towards estrogen production, making a GnRH stimulation test a more direct and comprehensive initial step to evaluate the source of puberty.
*Reassurance and follow-up*
- Reassurance is inappropriate given the presence of **vaginal bleeding** and signs of **accelerated skeletal maturation** (bone age of 11 years at chronological age 7).
- These findings warrant further investigation to determine the underlying cause and initiate appropriate management to prevent complications like **compromised adult height**.
*Ultrasound of the pelvis*
- A **pelvic ultrasound** would be useful to evaluate for ovarian cysts or tumors, which can cause **peripheral precocious puberty**.
- However, the GnRH stimulation test is a **more critical first step** to determine whether the puberty is central or peripheral before focusing on specific peripheral etiologies.
*MRI of the brain*
- An **MRI of the brain** is indicated if **central precocious puberty** is confirmed by the GnRH stimulation test, especially in a young child, to rule out **hypothalamic or pituitary tumors** or other CNS lesions.
- Doing an MRI of the brain before establishing the type of precocious puberty (central vs. peripheral) is **premature** as it is only indicated for central causes.
Growth charts and interpretation US Medical PG Question 7: A 1-year-old male presents to his pediatrician for a well-child visit. Through a history from the mother and physical examination, the pediatrician learns that the baby babbles non-specifically, takes several steps independently, and picks up his cereal using two fingers. His weight is currently 22 lbs (birth-weight 6 lbs, 9 oz), and his height is 30 inches (birth length 18 inches). Are there any aspects of this child's development that are delayed?
- A. Fine motor skill delay
- B. Language delay (Correct Answer)
- C. Inadequate growth
- D. Gross motor skill delay
- E. There are no developmental concerns
Growth charts and interpretation Explanation: ***Language delay***
- At 1 year of age, a child should typically be babbling with **specific sounds** and attempting to say their **first words**.
- The child's non-specific babbling suggests a delay in typical **expressive language development**.
*Fine motor skill delay*
- The child is able to pick up cereal using **two fingers**, indicating the development of a **pincer grasp**.
- This is an **age-appropriate fine motor skill** for a 1-year-old.
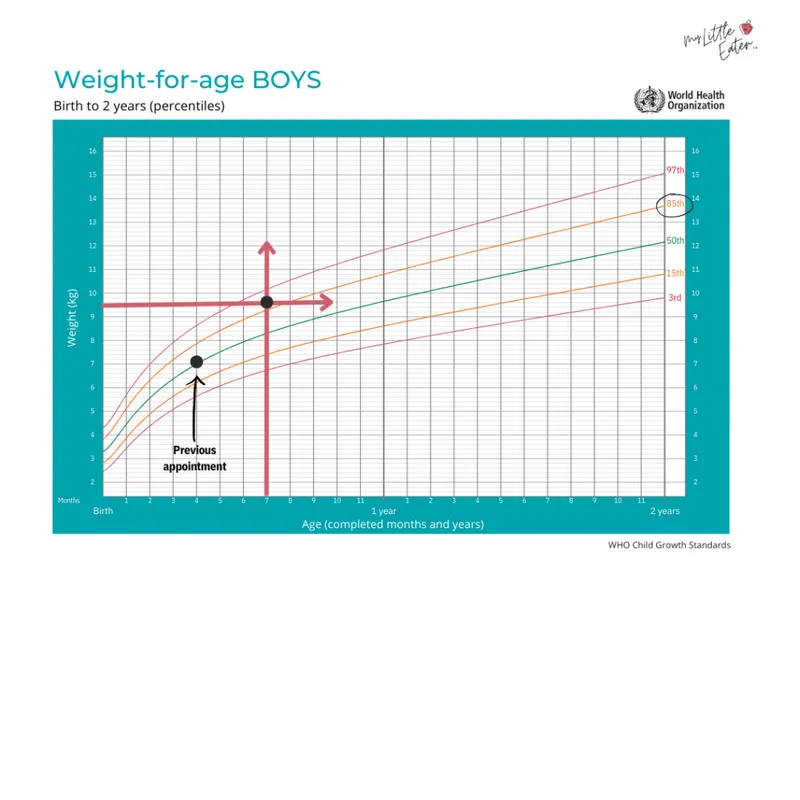
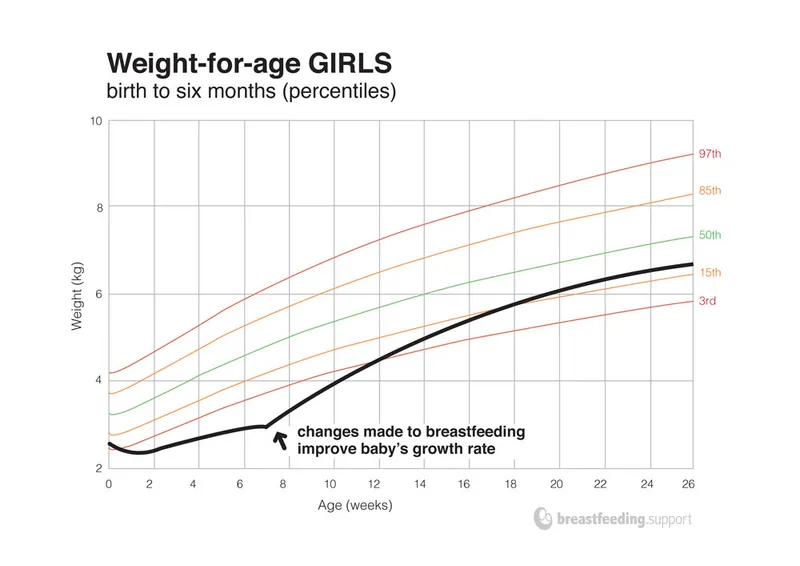
*Inadequate growth*
- The child has over **tripled his birth weight** (from 6 lbs, 9 oz to 22 lbs) and more than doubled his birth length (from 18 to 30 inches), which are **normal growth patterns** for the first year of life.
- While weight values can be plotted on growth charts, the provided information strongly suggests **adequate growth**.
*Gross motor skill delay*
- The child is taking **several steps independently**, which is an **age-appropriate gross motor milestone** for a 1-year-old.
- Many children take their first independent steps between 9 and 15 months.
*There are no developmental concerns*
- While many milestones are met, the **non-specific babbling** at 1 year strongly suggests a **language delay**.
- It is crucial to identify and address any potential delays early for intervention.
Growth charts and interpretation US Medical PG Question 8: An 8-month-old girl is brought to the emergency department because of fever, vomiting, and diarrhea for 3 days. Her parents report at least 10 watery stools daily. She has had three upper respiratory tract infections since she started daycare 2 months ago, but has otherwise been developing normally. Her mother has a history of celiac disease. The patient is at the 57th percentile for height and the 65th percentile for weight. Her immunizations are incomplete. Her temperature is 38.5°C (101.3°F), pulse is 145/min, and blood pressure is 92/54 mm Hg. Examination shows dry mucous membranes and decreased skin turgor. Bowel sounds are hyperactive. A complete blood count and serum concentrations of glucose, urea nitrogen, and creatinine are within the reference range; there is hypokalemia. In addition to intravenous fluid resuscitation, which of the following is the most appropriate next step in management?
- A. Examination of the stool for ova and parasites
- B. Sonography of the abdomen
- C. Administration of antidiarrheal medication
- D. Enzyme immunoassay of stool (Correct Answer)
- E. Blood cultures
Growth charts and interpretation Explanation: ***Enzyme immunoassay of stool***
- The patient presents with classic symptoms of **rotavirus gastroenteritis**, including fever, vomiting, and voluminous watery diarrhea, especially given her age, daycare exposure, and **incomplete immunization status** (missing rotavirus vaccine).
- **Enzyme immunoassay (EIA)** is a rapid, accurate test for detecting rotavirus antigens in stool, providing diagnosis confirmation within hours.
- While rotavirus gastroenteritis is managed primarily with **supportive care and rehydration** (already initiated), diagnostic testing is indicated here for: (1) **confirming the diagnosis** in an incompletely immunized child, (2) **infection control measures** in daycare/hospital settings, and (3) guiding parental counseling about immunization completion.
- EIA is the most appropriate next diagnostic step after stabilization has begun.
*Examination of the stool for ova and parasites*
- Stool O&P examination is appropriate for **persistent or chronic diarrhea** (>7-14 days), travel history, or suspected parasitic infection.
- Acute viral gastroenteritis typically presents with sudden onset of severe watery diarrhea, as seen here, rather than the more protracted course typical of parasitic infections.
- Parasitic causes are less likely in an otherwise healthy infant in a developed country without travel history.
*Sonography of the abdomen*
- **Abdominal sonography** would be indicated if there were concerns for **intussusception** (intermittent colicky pain, currant jelly stools, palpable mass) or other structural abnormalities.
- The patient's presentation with **diffuse watery diarrhea**, fever, and vomiting is classic for infectious gastroenteritis, not a surgical abdomen.
- Hyperactive bowel sounds further support an infectious rather than obstructive process.
*Administration of antidiarrheal medication*
- **Antidiarrheal medications are contraindicated** in infants and young children with acute infectious diarrhea.
- These agents (e.g., loperamide, bismuth subsalicylate) do not treat the underlying infection, can **prolong illness** by retaining pathogens, and risk serious complications including **toxic megacolon**, ileus, and CNS depression.
- The mainstay of treatment remains **oral or intravenous rehydration** and electrolyte replacement.
*Blood cultures*
- **Blood cultures** are indicated when there is concern for **bacteremia or sepsis**, typically suggested by high fever (>39°C), severe systemic toxicity, immunocompromise, or abnormal laboratory findings.
- This patient, while febrile, has **normal CBC, glucose, BUN, and creatinine**, making invasive bacterial infection less likely.
- The clinical picture is most consistent with **viral gastroenteritis**, which rarely causes bacteremia in immunocompetent children.
Growth charts and interpretation US Medical PG Question 9: A laborer's younger child is brought to the OPD with a swollen belly and dull face. He has been fed rice water (rice milk) in his diet mostly. On investigations, the child is found to have low serum protein and low albumin. What is the probable diagnosis?
- A. Kwashiorkor (Correct Answer)
- B. Kawasaki disease
- C. Marasmus
- D. Indian childhood cirrhosis
- E. Nephrotic syndrome
Growth charts and interpretation Explanation: ***Kwashiorkor***
- The symptoms of a **swollen belly** (due to **edema** from low albumin), **dull face**, and a diet primarily of **rice water** (low in protein) are classic signs of Kwashiorkor.
- Kwashiorkor is a form of severe protein-energy malnutrition characterized by **protein deficiency** that is greater than the calorie deficit, leading to **hypoalbuminemia** and fluid retention.
- The **dietary history** of rice water (carbohydrate-rich but protein-poor) is the key distinguishing feature.
*Kawasaki disease*
- This is an **acute vasculitis** primarily affecting young children, presenting with fever, rash, conjunctivitis, mouth changes, and lymphadenopathy.
- It does not involve a swollen belly or dull face as primary symptoms, nor is it linked to dietary protein deficiency.
*Marasmus*
- Marasmus is a form of severe malnutrition characterized by an **overall deficiency of calories** and nutrients, resulting in severe **wasting** of muscle and fat.
- While it involves low weight and energy deficit, the prominent **edema** (swollen belly) seen in this case points away from marasmus.
*Indian childhood cirrhosis*
- This is a rare, **fatal liver disease** in young children, often characterized by jaundice, hepatosplenomegaly, and liver failure.
- It is not primarily caused by protein deficiency and its symptoms are distinct from the presentation described.
*Nephrotic syndrome*
- While nephrotic syndrome also presents with **hypoalbuminemia and edema**, it would show **proteinuria** (>3.5 g/day), hyperlipidemia, and lipiduria on urinalysis.
- The **dietary history** and absence of urinary findings distinguish kwashiorkor from nephrotic syndrome.
Growth charts and interpretation US Medical PG Question 10: A 12-year-old boy presents with symptoms of headaches, visual disturbances, and growth retardation. An MRI scan is performed, and the image provided shows a cystic mass with both solid and calcified components in the suprasellar region, extending into the third ventricle. Based on the clinical presentation and MRI findings, what is the most likely diagnosis?
- A. Craniopharyngioma (Correct Answer)
- B. Germinoma
- C. Meningioma
- D. Pituitary adenoma
- E. Optic glioma
Growth charts and interpretation Explanation: ***Craniopharyngioma***
- This tumor is classically described as having **cystic** and **solid components** with **calcification**, which is evident in the provided MRI image. Its location in the **suprasellar region** and extension into the **third ventricle** are also typical.
- The clinical presentation of **headaches**, **visual disturbances** (due to compression of the optic chiasm), and **growth retardation** (due to hypothalamic-pituitary axis dysfunction) in a 12-year-old boy is highly suggestive of a craniopharyngioma, which commonly affects children and young adults.
*Germinoma*
- While germinomas can occur in the suprasellar region and cause similar endocrine and visual symptoms, they typically appear as **solid, homogeneously enhancing masses** on MRI and are less commonly cystic and calcified.
- They are more common in adolescence and are highly sensitive to radiation therapy, but their imaging characteristics differ from the described lesion.
*Meningioma*
- Meningiomas typically arise from the **arachnoid mater** and are usually **solid, extra-axial masses** that often have a **dural tail sign** on MRI.
- They are less common in children, and while they can calcify, their characteristic imaging features (extra-axial, dural attachment) are not consistent with the described suprasellar, intra-axial cystic mass.
*Pituitary adenoma*
- Pituitary adenomas originate from the **pituitary gland** and are usually located within the sella turcica, extending superiorly. While they can be cystic, **calcification is rare**, and they are more commonly solid and homogeneously enhancing.
- Although they can cause visual disturbances and hormonal imbalances, the prominent cystic-solid appearance with calcification and clear suprasellar origin extending into the third ventricle makes craniopharyngioma a more likely diagnosis in this age group and imaging.
*Optic glioma*
- Optic gliomas (pilocytic astrocytomas) are common **suprasellar tumors in children**, especially those with neurofibromatosis type 1, and can cause visual disturbances and endocrine dysfunction.
- However, they typically appear as **solid, fusiform masses** involving the optic nerve or chiasm with **homogeneous enhancement** and rarely show the characteristic cystic-solid architecture with prominent calcification seen in craniopharyngiomas.
More Growth charts and interpretation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.