Failure to thrive evaluation US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Failure to thrive evaluation. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
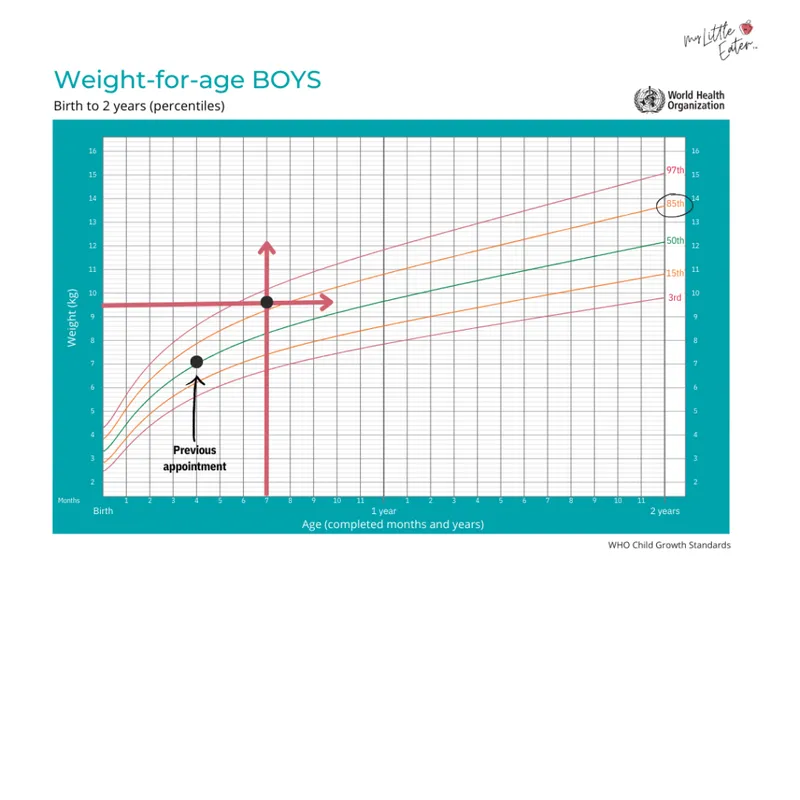
Failure to thrive evaluation US Medical PG Question 1: A 7-day-old male infant presents to the pediatrician for weight loss. There is no history of excessive crying, irritability, lethargy, or feeding difficulty. The parents deny any history of fast breathing, bluish discoloration of lips/nails, fever, vomiting, diarrhea, or seizures. He was born at full term by vaginal delivery without any perinatal complications and his birth weight was 3.6 kg (8 lb). Since birth he has been exclusively breastfed and passes urine six to eight times a day. His physical examination, including vital signs, is completely normal. His weight is 3.3 kg (7.3 lb); length and head circumference are normal for his age and sex. Which of the following is the next best step in the management of the infant?
- A. Reassurance of parents (Correct Answer)
- B. Evaluation of the mother for malnutrition
- C. Admission of the infant in the NICU to treat with empiric intravenous antibiotics
- D. Emphasize the need to clothe the infant warmly to prevent hypothermia
- E. Supplementation of breastfeeding with an appropriate infant formula
Failure to thrive evaluation Explanation: ***Reassurance of parents***
- A **weight loss of 8.3%** (300g from 3.6kg) is within the expected range for a 7-day-old exclusively breastfed infant, which can be up to 7-10% in the first week.
- The infant's normal physical exam, good urine output, and lack of other symptoms suggest **adequate feeding** and overall well-being.
*Evaluation of the mother for malnutrition*
- The mother's nutritional status is not directly indicative of the infant's weight loss within the normal physiological range in this scenario.
- There is no information to suggest the mother is malnourished or that it would directly impact the quality or quantity of breast milk to cause pathological weight loss.
*Admission of the infant in the NICU to treat with empiric intravenous antibiotics*
- This is an overly aggressive intervention as there are **no signs or symptoms of infection** (e.g., fever, lethargy, poor feeding) and the infant appears well.
- Empiric antibiotics are not warranted in an otherwise healthy, full-term infant with normal physiological weight loss.
*Emphasize the need to clothe the infant warmly to prevent hypothermia*
- The infant's **vital signs are normal**, indicating no hypothermia, and there is no clinical evidence to support this as a primary concern.
- While maintaining warmth is important, it is not the next best step for addressing this specific presentation of physiological weight loss.
*Supplementation of breastfeeding with an appropriate infant formula*
- Supplementation is typically not needed for physiological weight loss in an otherwise healthy, exclusively breastfed infant with **adequate urine output** and no signs of dehydration.
- Encouraging continued exclusive breastfeeding and providing support for proper latch and feeding techniques would be more appropriate if there were concerns about inadequate milk intake.
Failure to thrive evaluation US Medical PG Question 2: A two-year-old female presents to the pediatrician with her mother for a routine well-child visit. Her mother is concerned that the patient is a picky eater and refuses to eat vegetables. She drinks milk with meals and has juice sparingly. She goes to sleep easily at night and usually sleeps for 11-12 hours. The patient has trouble falling asleep for naps but does nap for 1-2 hours a few times per week. She is doing well in daycare and enjoys parallel play with the other children. Her mother reports that she can walk down stairs with both feet on each step. She has a vocabulary of 10-25 words that she uses in the form of one-word commands. She is in the 42nd percentile for height and 48th percentile for weight, which is consistent with her growth curves. On physical exam, she appears well nourished. She can copy a line and throw a ball. She can follow the command to “give me the ball and then close the door.”
This child is meeting her developmental milestones in all but which of the following categories?
- A. Social and receptive language skills
- B. Fine motor skills
- C. This child is developmentally normal
- D. Gross motor skills
- E. Expressive language skills (Correct Answer)
Failure to thrive evaluation Explanation: ***Expressive language skills***
- At two years old, a child should typically have an **expressive vocabulary of 50-200 words** and be putting **two-word sentences** together.
- This child's vocabulary of 10-25 words, used primarily as one-word commands, is significantly below the expected range for her age.
*Social and receptive language skills*
- The child is reported to be doing well in daycare and enjoys **parallel play**, which reflects appropriate **social development** for her age.
- Her ability to follow the two-step command "give me the ball and then close the door" demonstrates intact **receptive language skills**.
*This child is developmentally normal*
- While many areas of her development appear normal, her **expressive language skills** are clearly delayed, indicating that she is not entirely developmentally normal.
- Identifying specific areas of delay is crucial for early intervention.
*Gross motor skills*
- The child's ability to **walk down stairs with both feet on each step** is a normal gross motor milestone for a two-year-old.
- Other gross motor skills like running and kicking a ball are typically present, and there is no information to suggest a deficit.
*Fine motor skills*
- The ability to **copy a line** is an expected fine motor skill for a two-year-old.
- Throwing a ball also involves fine motor coordination and is within the expected range for this age.
Failure to thrive evaluation US Medical PG Question 3: A 7-year-old girl presents to her primary care physician for a routine check-up. The physician allows the medical student to perform a physical examination. The medical student notes hearing impairment as well as the findings show in Figures A and B. Radiographs show indications of multiple old fractures of the humerus that have healed. After questioning the girl’s parents, the medical student learns that in addition, the patient is extremely picky with her food and eats a diet consisting mainly of cereal and pasta. What is the most likely etiology of the patient’s disease?
- A. Dietary deficiency of ascorbic acid
- B. Defect in type I collagen (Correct Answer)
- C. Defective mineralization of cartilage
- D. Decreased bone mineral density
- E. Non-accidental trauma
Failure to thrive evaluation Explanation: ***Defect in type I collagen***
- The constellation of **frequent fractures**, **hearing impairment**, and **blue sclerae** (as indicated by Figure A, which shows a bluish tint to the white part of the eye) is characteristic of **osteogenesis imperfecta (OI)**, a genetic disorder caused by mutations in COL1A1 or COL1A2 genes leading to **defective type I collagen synthesis**.
- Type I collagen is the primary structural protein in bone, and defects result in brittle bones, blue sclerae (due to thin sclera allowing choroid visibility), and conductive hearing loss (from ossicle abnormalities).
- While the patient's diet is described as "picky," the primary features point towards a genetic collagen defect rather than a nutritional deficiency as the underlying cause for the bone and connective tissue abnormalities.
*Dietary deficiency of ascorbic acid*
- A deficiency in **ascorbic acid (vitamin C)** leads to **scurvy**, characterized by **gingivitis**, **poor wound healing**, **petechiae**, and easy bruising due to impaired collagen synthesis.
- While collagen synthesis is affected, the specific presentation of blue sclerae, hearing impairment, and multiple fractures as primary symptoms is not typical for scurvy.
*Defective mineralization of cartilage*
- **Defective mineralization of cartilage** often points to **rickets in children** or **osteomalacia in adults**, usually due to **vitamin D deficiency** or disorders of phosphate metabolism.
- While these conditions can cause bone fragility, they do not typically present with blue sclerae or hearing impairment as defining features. The "old fractures" suggest a chronic bone fragility predating any acute nutritional issues.
*Decreased bone mineral density*
- **Decreased bone mineral density (BMD)** is a general term seen in many conditions, including **osteoporosis** and **osteogenesis imperfecta**.
- While the patient likely has decreased BMD due to their frequent fractures, this option describes a symptom rather than the **underlying etiology** of the disorder.
*Non-accidental trauma*
- **Non-accidental trauma (child abuse)** should always be considered in a child with multiple fractures.
- However, the presence of other systemic findings like **blue sclerae** and **hearing impairment** strongly suggests an underlying genetic disorder like osteogenesis imperfecta, making non-accidental trauma less likely as the primary cause for all observed symptoms.
Failure to thrive evaluation US Medical PG Question 4: A 4-year-old girl is brought to the physician by her parents because she is severely underweight. She is easily fatigued and has difficulty keeping up with other children at her daycare. She has a good appetite and eats 3 full meals a day. She has 4 to 5 bowel movements daily with bulky, foul-smelling stools that float. She has had recurrent episodes of sinusitis since infancy. Her parents report that she recently started to snore during her sleep. She is at the 15th percentile for height and 3rd percentile for weight. Her vital signs are within normal limits. Examination shows pale conjunctivae. A few scattered expiratory crackles are heard in the thorax. There is abdominal distention. Which of the following is the most likely underlying cause of this patient's failure to thrive?
- A. T. whippelii infiltration of intestinal villi
- B. Impaired intestinal amino acid transport
- C. Exocrine pancreatic insufficiency (Correct Answer)
- D. Small intestine bacterial overgrowth
- E. Intestinal inflammatory reaction to gluten
Failure to thrive evaluation Explanation: ***Exocrine pancreatic insufficiency***
- The constellation of **failure to thrive**, **bulky, foul-smelling, floating stools** (suggesting **steatorrhea**), recurrent **sinusitis**, and **recurrent respiratory symptoms** (snoring, expiratory crackles) is highly indicative of **cystic fibrosis**, whose primary cause of malabsorption is **exocrine pancreatic insufficiency**.
- **Cystic fibrosis** leads to thick, viscous secretions that obstruct pancreatic ducts, preventing digestive enzymes from reaching the small intestine and causing **malabsorption of fats and fat-soluble vitamins**.
*T. whippelii infiltration of intestinal villi*
- This describes **Whipple's disease**, which typically affects **middle-aged men** and presents with malabsorption, arthralgia, and neurological symptoms.
- It is rare in children and usually presents with symptoms like diarrhea and weight loss, but not commonly with the **recurrent respiratory infections** and **pancreatic insufficiency** seen here.
*Impaired intestinal amino acid transport*
- This typically refers to conditions like **Hartnup disease**, which involves defective transport of neutral amino acids and can lead to **pellagra-like symptoms** (dermatitis, diarrhea, dementia) due to niacin deficiency.
- This condition does not explain the **steatorrhea**, **recurrent sinusitis**, or **respiratory symptoms** found in the patient.
*Small intestine bacterial overgrowth*
- While **SIBO** can cause malabsorption, **abdominal distention**, and loose stools, it does not typically cause **recurrent sinusitis** or the classic **bulky, foul-smelling, floating stools associated with pancreatic insufficiency**.
- SIBO is also not a primary cause of **failure to thrive** in a global sense, but rather a secondary complication.
*Intestinal inflammatory reaction to gluten*
- This describes **celiac disease**, which presents with **malabsorption**, **abdominal distention**, **failure to thrive**, and **anemia** (pale conjunctivae).
- However, celiac disease does not typically cause **recurrent sinusitis** or the **respiratory symptoms** (snoring, crackles) that are prominent in this patient's presentation.
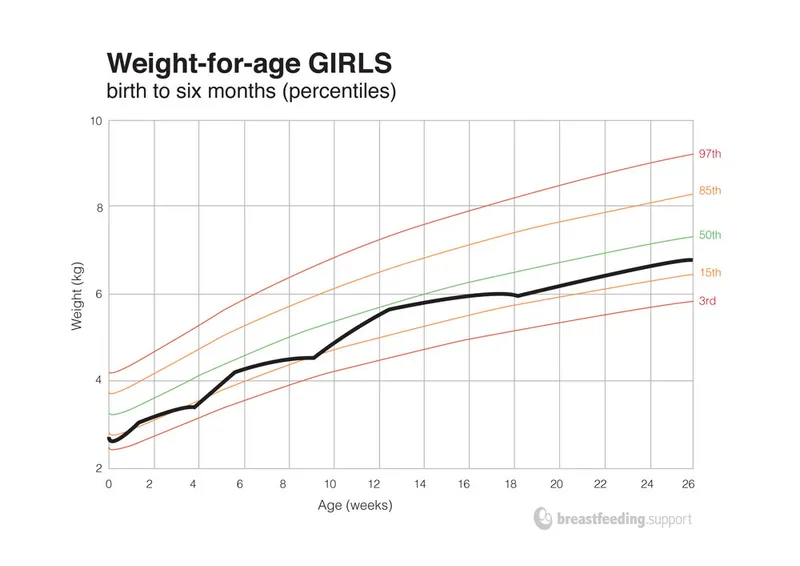
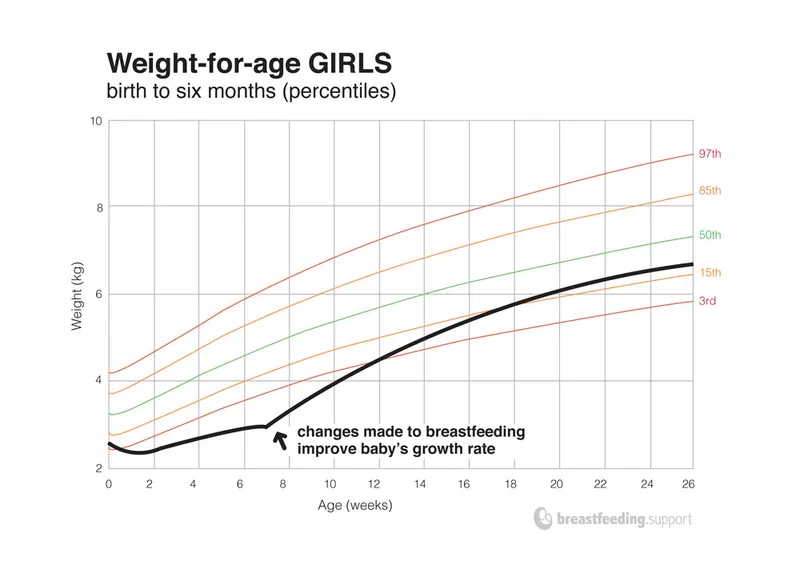
Failure to thrive evaluation US Medical PG Question 5: A 4-day-old male newborn is brought to the physician for a well-child examination. His mother is concerned that he is losing weight. He was born at 40 weeks' gestation and weighed 2980g (6-lb 9-oz); he currently weighs 2830g (6-lb 4-oz). Pregnancy was uncomplicated. He passed stool and urine 8 and 10 hours after delivery. He has been exclusively breast fed since birth and feeds 11–12 times daily. His mother says she changes 5–6 heavy diapers daily. Examination shows an open and firm anterior fontanelle. Mucous membranes are moist. Capillary refill time is less than 2 seconds. Cardiopulmonary examination shows no abnormalities. Which of the following is the most appropriate next best step in management?
- A. Continue breastfeeding (Correct Answer)
- B. Add rice based cereal
- C. Add cow milk based formula
- D. Serum creatinine and urea nitrogen
- E. Switch to soy-based formula
Failure to thrive evaluation Explanation: ***Continue breastfeeding***
- A 4-day-old newborn losing less than 7% of birth weight, with good feeding frequency, adequate wet diapers, and normal physical examination findings, is considered typical for **physiological weight loss** in breastfed infants.
- The infant's current weight of 2830g is within the expected range, as healthy full-term newborns may lose up to 7-10% of their birth weight in the first few days, and his weight loss is only about 5%.
*Add rice based cereal*
- **Solid foods**, including rice cereal, should not be introduced before 4-6 months of age due to the immaturity of the infant's digestive system and potential for choking.
- Introducing solids too early can interfere with nutrient absorption from breast milk and increase the risk of allergies.
*Add cow milk based formula*
- Supplementing with formula is unnecessary in a healthy, breastfed infant exhibiting normal physiological weight loss and adequate feeding cues.
- Early introduction of formula can interfere with **successful breastfeeding establishment** and alter the infant's gut microbiome.
*Serum creatinine and urea nitrogen*
- These tests are used to assess **renal function** and are not indicated here, as the infant shows no signs of renal impairment (e.g., adequate urine output, moist mucous membranes).
- The physical examination findings and feeding pattern suggest a healthy newborn, not one requiring investigation for kidney issues.
*Switch to soy-based formula*
- Switching to any formula is unwarranted given the normal weight loss and breastfeeding progress, and specifically, soy-based formula is not routinely recommended for healthy infants.
- Soy formula is often reserved for infants with **cow's milk protein allergy** or **galactosemia**, neither of which is suggested by this clinical picture.
Failure to thrive evaluation US Medical PG Question 6: A 13-year-old boy is being evaluated for failure to thrive and bad performance at school. He has a history of microcytic anemia and takes a multivitamin every morning with breakfast. An electrophoresis analysis shows no adult hemoglobin (HbA), elevated hemoglobin adult type 2 (HbA2), and normal fetal hemoglobin (HbF). A skull X-ray revealed a crewcut appearance. Which of the following is the most likely diagnosis?
- A. β-thal minor
- B. Hb Bart disease
- C. α-thal trait
- D. β-thal major (Correct Answer)
- E. HbH disease
Failure to thrive evaluation Explanation: ***β-thal major***
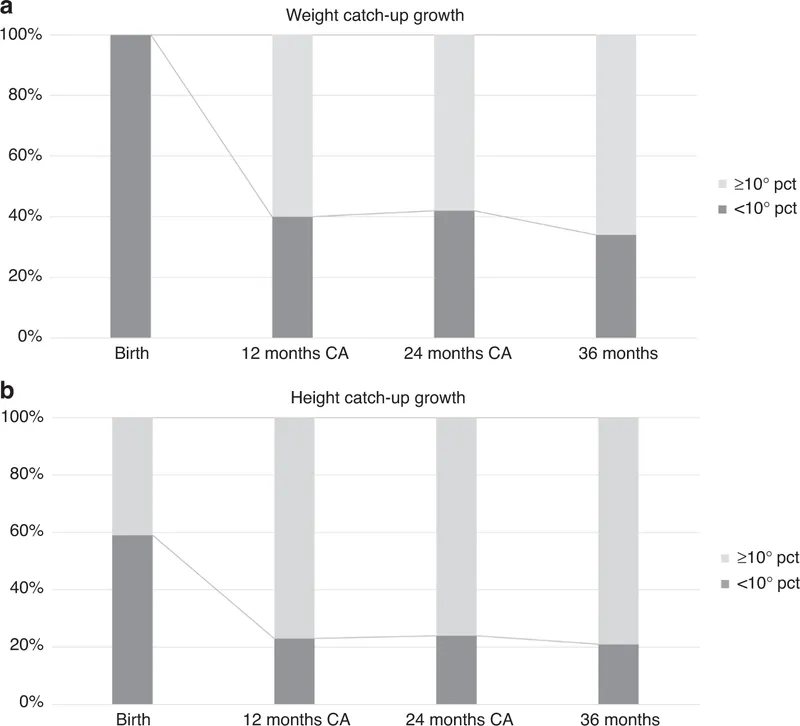
- The absence of **HbA**, elevated **HbA2**, and normal HbF (which is usually also elevated) in the presence of severe microcytic anemia, failure to thrive, and a **crewcut appearance** on skull X-ray are classic signs of **β-thalassemia major**, also known as **Cooley's anemia**.
- The "crewcut" appearance is due to **extramedullary hematopoiesis** to compensate for severe anemia, leading to widening of the diploic space and typical perpendicular **spicules of new bone formation** on the skull X-ray.
*β-thal minor*
- This condition is typically **asymptomatic** or only causes **mild microcytic anemia** and would not lead to failure to thrive or the severe skeletal changes seen here.
- While it features elevated **HbA2** and potentially slightly reduced HbA, it would still have significant HbA production.
*Hb Bart disease*
- This is the most severe form of **α-thalassemia**, characterized by the complete absence of alpha-globin chains.
- It results in **hydrops fetalis** and is usually lethal in utero or shortly after birth, so a 13-year-old would not present with this.
*α-thal trait*
- This refers to two forms: **silent carrier** (one gene deleted) or **α-thalassemia minor** (two genes deleted).
- Both are usually **asymptomatic** or cause **mild microcytic anemia**, and would not present with the severe clinical picture or bone changes described.
*HbH disease*
- This is an intermediate form of **α-thalassemia** where three out of four alpha-globin genes are deleted.
- It presents with **moderate to severe hemolytic anemia**, but the **hemoglobin electrophoresis** would show the presence of **HbH** (a tetramer of four beta-globin chains) and not the described pattern of HbA, HbA2, and HbF.
Failure to thrive evaluation US Medical PG Question 7: A 6-month-old girl is brought to the physician because of drooling and excessive crying for 3 days. She calms down when cuddled or with a pacifier in her mouth. She feeds well and has no vomiting or diarrhea. She was breastfed exclusively for 5 months. She is given no medications and was born at 39 weeks gestation via spontaneous vaginal delivery. She is up to date on all vaccines and is meeting all developmental milestones. At the clinic, her weight is 7.3 kg (16 lb 1 oz) and her height is 65.8 cm (25.9 in) in length. She appears irritable. Her pulse is 124/min, the respirations are 32/min, the blood pressure is 92/63 mm Hg, and the temperature is 36.8°C (98.2°F). On physical examination, she has no conjunctivitis, cervical lymphadenopathy, or pharyngeal erythema. Which element of the physical examination is most likely to be present in this patient?
- A. The rooting reflex
- B. Crying on frontal sinus palpation
- C. Eruption of mandibular incisors (Correct Answer)
- D. Closure of the anterior fontanel
- E. Erythema and fluctuance of the submandibular area
Failure to thrive evaluation Explanation: ***Eruption of mandibular incisors***
- The patient's age (6 months), **drooling**, and **irritability** strongly suggest **teething**, which commonly involves the eruption of the mandibular incisors.
- Teething pain and discomfort can be relieved by pacifiers or cuddling, consistent with the patient's presentation.
*The rooting reflex*
- The **rooting reflex** is a primitive reflex typically present at birth and usually disappears by **4 months of age**; this patient is 6 months old.
- Its presence would not explain the current symptoms of irritability and drooling.
*Crying on frontal sinus palpation*
- **Frontal sinuses** are typically underdeveloped or absent in infants and children until later ages (around 6-10 years old), so their palpation is not clinically relevant in a 6-month-old.
- Crying on palpation would only be significant if the sinuses were developed and inflamed, which is unlikely and not indicated by other symptoms.
*Closure of the anterior fontanel*
- The **anterior fontanel** typically remains open until **12-18 months of age**, allowing for brain growth; abnormal closure at 6 months would be a concerning finding but is not indicated by the drooling and irritability.
- Premature closure of the fontanel is usually associated with microcephaly or other cranial abnormalities, not teething symptoms.
*Erythema and fluctuance of the submandibular area*
- **Erythema** and **fluctuance** in the submandibular area suggest an **infection or abscess**, which would likely be accompanied by fever and other signs of systemic illness not present in this patient.
- While teething can cause local inflammation, it does not typically lead to a submandibular abscess without other contributing factors.
Failure to thrive evaluation US Medical PG Question 8: A laborer's younger child is brought to the OPD with a swollen belly and dull face. He has been fed rice water (rice milk) in his diet mostly. On investigations, the child is found to have low serum protein and low albumin. What is the probable diagnosis?
- A. Kwashiorkor (Correct Answer)
- B. Kawasaki disease
- C. Marasmus
- D. Indian childhood cirrhosis
- E. Nephrotic syndrome
Failure to thrive evaluation Explanation: ***Kwashiorkor***
- The symptoms of a **swollen belly** (due to **edema** from low albumin), **dull face**, and a diet primarily of **rice water** (low in protein) are classic signs of Kwashiorkor.
- Kwashiorkor is a form of severe protein-energy malnutrition characterized by **protein deficiency** that is greater than the calorie deficit, leading to **hypoalbuminemia** and fluid retention.
- The **dietary history** of rice water (carbohydrate-rich but protein-poor) is the key distinguishing feature.
*Kawasaki disease*
- This is an **acute vasculitis** primarily affecting young children, presenting with fever, rash, conjunctivitis, mouth changes, and lymphadenopathy.
- It does not involve a swollen belly or dull face as primary symptoms, nor is it linked to dietary protein deficiency.
*Marasmus*
- Marasmus is a form of severe malnutrition characterized by an **overall deficiency of calories** and nutrients, resulting in severe **wasting** of muscle and fat.
- While it involves low weight and energy deficit, the prominent **edema** (swollen belly) seen in this case points away from marasmus.
*Indian childhood cirrhosis*
- This is a rare, **fatal liver disease** in young children, often characterized by jaundice, hepatosplenomegaly, and liver failure.
- It is not primarily caused by protein deficiency and its symptoms are distinct from the presentation described.
*Nephrotic syndrome*
- While nephrotic syndrome also presents with **hypoalbuminemia and edema**, it would show **proteinuria** (>3.5 g/day), hyperlipidemia, and lipiduria on urinalysis.
- The **dietary history** and absence of urinary findings distinguish kwashiorkor from nephrotic syndrome.
Failure to thrive evaluation US Medical PG Question 9: A 12-year-old boy presents with symptoms of headaches, visual disturbances, and growth retardation. An MRI scan is performed, and the image provided shows a cystic mass with both solid and calcified components in the suprasellar region, extending into the third ventricle. Based on the clinical presentation and MRI findings, what is the most likely diagnosis?
- A. Craniopharyngioma (Correct Answer)
- B. Germinoma
- C. Meningioma
- D. Pituitary adenoma
- E. Optic glioma
Failure to thrive evaluation Explanation: ***Craniopharyngioma***
- This tumor is classically described as having **cystic** and **solid components** with **calcification**, which is evident in the provided MRI image. Its location in the **suprasellar region** and extension into the **third ventricle** are also typical.
- The clinical presentation of **headaches**, **visual disturbances** (due to compression of the optic chiasm), and **growth retardation** (due to hypothalamic-pituitary axis dysfunction) in a 12-year-old boy is highly suggestive of a craniopharyngioma, which commonly affects children and young adults.
*Germinoma*
- While germinomas can occur in the suprasellar region and cause similar endocrine and visual symptoms, they typically appear as **solid, homogeneously enhancing masses** on MRI and are less commonly cystic and calcified.
- They are more common in adolescence and are highly sensitive to radiation therapy, but their imaging characteristics differ from the described lesion.
*Meningioma*
- Meningiomas typically arise from the **arachnoid mater** and are usually **solid, extra-axial masses** that often have a **dural tail sign** on MRI.
- They are less common in children, and while they can calcify, their characteristic imaging features (extra-axial, dural attachment) are not consistent with the described suprasellar, intra-axial cystic mass.
*Pituitary adenoma*
- Pituitary adenomas originate from the **pituitary gland** and are usually located within the sella turcica, extending superiorly. While they can be cystic, **calcification is rare**, and they are more commonly solid and homogeneously enhancing.
- Although they can cause visual disturbances and hormonal imbalances, the prominent cystic-solid appearance with calcification and clear suprasellar origin extending into the third ventricle makes craniopharyngioma a more likely diagnosis in this age group and imaging.
*Optic glioma*
- Optic gliomas (pilocytic astrocytomas) are common **suprasellar tumors in children**, especially those with neurofibromatosis type 1, and can cause visual disturbances and endocrine dysfunction.
- However, they typically appear as **solid, fusiform masses** involving the optic nerve or chiasm with **homogeneous enhancement** and rarely show the characteristic cystic-solid architecture with prominent calcification seen in craniopharyngiomas.
Failure to thrive evaluation US Medical PG Question 10: A baby was playing unattended and suddenly developed respiratory distress. Based on the X-ray provided, where is the foreign object most likely located?
- A. Trachea
- B. Gastrointestinal tract
- C. Esophagus (Correct Answer)
- D. Below diaphragm
- E. Right main bronchus
Failure to thrive evaluation Explanation: ***Esophagus***
- The frontal X-ray shows a **coin-shaped foreign body** that is oriented in the **coronal plane** (flat face visible), which is characteristic of an object lodged in the esophagus.
- The foreign body is located in the **upper mediastinum**, directly in the known anatomical path of the esophagus, causing respiratory distress due to **extrinsic compression** of the trachea or aspiration.
*Trachea*
- Foreign bodies in the trachea, especially flat objects like coins, typically orient themselves in the **sagittal plane** (on edge) due to the C-shaped cartilaginous rings.
- While tracheal foreign bodies can cause respiratory distress, the orientation on the image is inconsistent with a tracheal location.
*Right main bronchus*
- The **right main bronchus** is the most common site for aspirated foreign bodies in children due to its wider diameter and more vertical orientation.
- However, foreign bodies in the bronchus would typically show air trapping or atelectasis on chest X-ray, and the location and orientation of this object in the upper mediastinum are not consistent with bronchial placement.
*Gastrointestinal tract*
- The foreign body is located in the **chest cavity**, well above the stomach and intestines.
- If a foreign body reaches the gastrointestinal tract, it would typically be beyond the esophagus and would not usually cause acute respiratory distress.
*Below diaphragm*
- The diaphragm separates the chest cavity from the abdominal cavity. The foreign body is clearly visible within the **chest cavity**, high up in the mediastinum.
- A foreign body below the diaphragm in the gastrointestinal tract would not result in the appearance or the acute respiratory distress described without other symptoms.
More Failure to thrive evaluation US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.