Delayed puberty US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Delayed puberty. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Delayed puberty US Medical PG Question 1: A 27-year-old man comes to the physician with his wife because they have been unable to conceive. They have had regular unprotected sex for the past 18 months without using contraception. His wife has been tested and is fertile. The patient began puberty at the age of 13 years. He has been healthy except for an infection with Chlamydia trachomatis 10 years ago, which was treated with azithromycin. He is a professional cyclist and trains every day for 3–4 hours. His wife reports that her husband has often been stressed since he started to prepare for the national championships a year ago and is very conscious about his diet. His temperature is 36.5°C (97.7°F), pulse is 50/min, and blood pressure is 154/92 mm Hg. Physical examination of the husband shows an athletic stature with uniform inflammatory papular eruptions of the face, back, and chest. Genital examination shows small testes. Which of the following is the most likely underlying cause of this patient's infertility?
- A. Heat from friction
- B. Psychogenic erectile dysfunction
- C. Kallmann syndrome
- D. Anorexia nervosa
- E. Anabolic steroid use (Correct Answer)
Delayed puberty Explanation: ***Anabolic steroid use***
- The patient's **athletic stature**, **inflammatory papular eruptions** (acne), **small testes**, and dedication to intense training are highly suggestive of anabolic steroid use. Anabolic steroids suppress endogenous **gonadotropin-releasing hormone (GnRH)**, leading to secondary hypogonadism, testicular atrophy, and infertility.
- The history of **Chlamydia trachomatis** 10 years ago is less likely to be the primary cause of current infertility given the effective treatment, and the associated signs point more strongly to steroid use.
*Heat from friction*
- While prolonged cycling can increase **scrotal temperature**, potentially affecting **sperm quality**, it is unlikely to cause the severe **testicular atrophy** and broad systemic effects (acne, hypertension) seen in this patient.
- **Infertility related to heat** typically presents as reduced sperm count or motility, without the endocrine disruptions associated with anabolic steroids.
*Psychogenic erectile dysfunction*
- **Erectile dysfunction** is not explicitly mentioned as a complaint; the primary concern is infertility despite regular unprotected sex. While stress can contribute to ED, it does not explain the **small testes** or systemic dermatological findings.
- **Psychogenic factors** primarily affect the ability to achieve or maintain an erection, not necessarily **sperm production** or testicular size in the absence of other hormonal issues.
*Kallmann syndrome*
- **Kallmann syndrome** is a genetic condition characterized by hypogonadotropic hypogonadism and **anosmia** (inability to smell) due to defective migration of GnRH neurons. Patients typically present with **delayed puberty** (primary amenorrhea in females, lack of secondary sexual characteristics in males).
- This patient began puberty at age 13, which is within the normal range, and there is no mention of anosmia, making Kallmann syndrome unlikely.
*Anorexia nervosa*
- Anorexia nervosa can lead to **hypogonadism** (due to low GnRH output from caloric restriction and excessive exercise), which might cause small testes and infertility. However, it is typically associated with **low body weight**, which contradicts the patient's athletic stature and professional cyclist status.
- While extreme dieting is mentioned, it's in the context of professional cycling, and the other symptoms like **acne** and **hypertension** are not typical findings in anorexia nervosa.
Delayed puberty US Medical PG Question 2: A 15-year-old girl comes to the physician with her father for evaluation of short stature. She feels well overall but is concerned because all of her friends are taller than her. Her birth weight was normal. Menarche has not yet occurred. Her father says he also had short stature and late puberty. The girl is at the 5th percentile for height and 35th percentile for weight. Breast development is Tanner stage 2. Pubic and axillary hair is absent. An x-ray of the left hand and wrist shows a bone age of 12 years. Further evaluation of this patient is most likely to show which of the following sets of laboratory findings?
- A. High FSH, High LH, Normal Estradiol, Normal Prolactin
- B. Normal FSH, Normal LH, Normal Estradiol, Normal Prolactin
- C. Normal FSH, Normal LH, Low Estradiol, Normal Prolactin
- D. Low-normal FSH, Low-normal LH, Low Estradiol, Normal Prolactin (Correct Answer)
- E. Low FSH, Low LH, Low Estradiol, Normal Prolactin
Delayed puberty Explanation: ***Low-normal FSH, Low-normal LH, Low Estradiol, Normal Prolactin***
- This pattern is characteristic of **constitutional delay of growth and puberty (CDGP)**, where the hypothalamic-pituitary-gonadal (HPG) axis has not yet fully matured, resulting in low-normal gonadotropins and low estradiol.
- The key clinical features supporting CDGP include: **delayed bone age** (12 years vs chronologic age 15), **positive family history** of late puberty, normal growth velocity, and absence of pathological findings.
- In CDGP, gonadotropins are in the **low-normal or prepubertal range** but will eventually rise spontaneously as the HPG axis matures, distinguishing this from permanent hypogonadotropic hypogonadism.
- GnRH stimulation testing would show a pubertal (not prepubertal) response, confirming the functional delay rather than a pathologic deficiency.
*Low FSH, Low LH, Low Estradiol, Normal Prolactin*
- This pattern suggests **hypogonadotropic hypogonadism**, such as Kallmann syndrome or functional hypothalamic amenorrhea, where gonadotropins are frankly low (not just low-normal).
- While this also presents with low estradiol and delayed puberty, patients with hypogonadotropic hypogonadism typically lack the **positive family history** and would not show delayed bone age suggesting growth potential.
- The distinction is that in permanent hypogonadotropic hypogonadism, the HPG axis is deficient and will not mature spontaneously without hormonal treatment.
*High FSH, High LH, Normal Estradiol, Normal Prolactin*
- This combination is inconsistent with delayed puberty, as high gonadotropins indicate **hypergonadotropic hypogonadism** (primary ovarian failure such as Turner syndrome).
- Hypergonadotropic hypogonadism presents with **high FSH/LH and low estradiol** (not normal), as the pituitary attempts to stimulate non-responsive ovaries.
- This patient's delayed bone age and family history make a physiologic delay (CDGP) much more likely than ovarian failure.
*Normal FSH, Normal LH, Normal Estradiol, Normal Prolactin*
- **Normal estradiol** at age 15 would indicate that puberty is progressing appropriately, which contradicts this patient's clinical presentation.
- The patient has delayed menarche, absent pubic/axillary hair, only Tanner stage 2 breast development, and bone age of 12 years - all indicating **low estradiol** and delayed pubertal progression.
- If all hormones were normal, we would expect more advanced pubertal development at this age.
*Normal FSH, Normal LH, Low Estradiol, Normal Prolactin*
- While low estradiol correctly reflects delayed puberty, describing FSH and LH as fully "normal" is imprecise for CDGP.
- In CDGP, gonadotropins are characteristically in the **low-normal or prepubertal range**, not at robust normal adult levels, reflecting the immature but eventually functional HPG axis.
- The distinction between "normal" and "low-normal" gonadotropins is clinically important for differentiating constitutional delay from other causes of delayed puberty.
Delayed puberty US Medical PG Question 3: A 16-year-old teenager presents to the pediatrician with his mother. After she leaves the room he tells the physician that he is worried about puberty. All of his friends have had growth spurts, started building muscle mass, and their voices have changed while he still feels underdeveloped. The physician takes a complete history and performs a thorough physical examination. He goes through the patient’s past medical records and growth charts and notes physical findings documented over the last five years, concluding that the patient has delayed puberty. Which of the following findings supports his conclusion?
- A. The absence of testicular enlargement by age of 14 years (Correct Answer)
- B. The absence of an adult type of pubic hair distribution by age of 16 years
- C. The absence of linear growth acceleration by age of 13 years
- D. Presence of gynecomastia at age of 15 years
- E. The absence of penile enlargement by age of 12 years
Delayed puberty Explanation: ***The absence of testicular enlargement by age of 14 years***
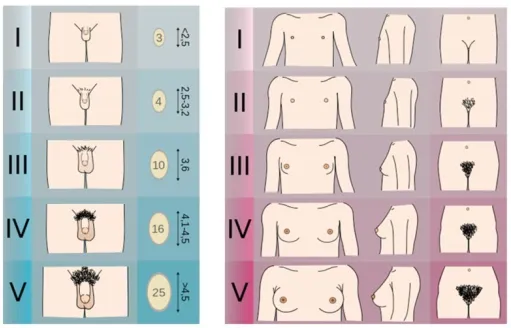
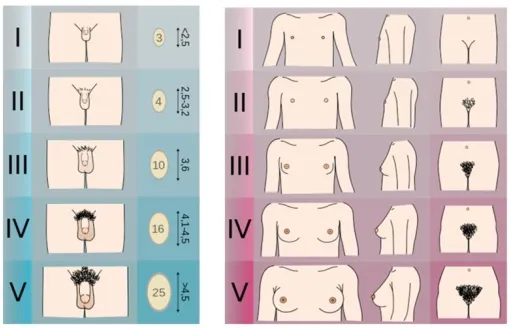
- The first reliable sign of male puberty is an increase in **testicular volume**, typically occurring by age 14.
- Absence of this by age 14 years indicates **delayed puberty** in males.
*The absence of an adult type of pubic hair distribution by age of 16 years*
- While pubic hair development is a sign of puberty, **adult-type distribution** (Tanner stage 5) by age 16 is normal for many.
- The definition of delayed puberty in males is typically based on the **absence of any secondary sexual characteristics** by age 14, or more specifically, testicular enlargement.
*The absence of linear growth acceleration by age of 13 years*
- The pubertal **growth spurt** typically occurs later in puberty, often around 13-14 years in males, following testicular enlargement.
- Its absence by age 13 might suggest early delay, but **testicular enlargement** is the primary diagnostic criterion.
*Presence of gynecomastia at age of 15 years*
- **Gynecomastia** can be a normal, transient finding during puberty due to temporary estrogen-androgen imbalance, not necessarily indicative of delayed puberty.
- Its presence doesn't rule out delayed puberty but isn't a direct sign of delay itself.
*The absence of penile enlargement by age of 12 years*
- **Penile enlargement** typically occurs after testicular enlargement.
- The absence of this by age 12 is less specific than **testicular enlargement by age 14** for defining delayed puberty.
Delayed puberty US Medical PG Question 4: A 7-year-old boy is brought to the physician because his parents are concerned about his early sexual development. He has no history of serious illness and takes no medications. His brother was diagnosed with testicular cancer 5 years ago and underwent a radical orchiectomy. The patient is at the 85th percentile for height and 70th percentile for weight. Examination shows greasy facial skin. There is coarse axillary hair. Pubic hair development is at Tanner stage 3 and testicular development is at Tanner stage 2. The remainder of the examination shows no abnormalities. An x-ray of the wrist shows a bone age of 10 years. Basal serum luteinizing hormone and follicle-stimulating hormone are elevated. An MRI of the brain shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Leuprolide therapy (Correct Answer)
- B. Testicular ultrasound
- C. Cortisol supplementation
- D. Radiation therapy
- E. Observation
Delayed puberty Explanation: ***Leuprolide therapy***
- This patient presents with **central precocious puberty** (CPP), indicated by elevated **basal LH and FSH levels** in the context of advanced bone age, Tanner stage 3 pubic hair, and Tanner stage 2 testicular development at a young age.
- **Leuprolide** is a GnRH analog that, when given continuously, downregulates the pituitary's GnRH receptors, suppressing gonadotropin release and halting pubertal progression. This is the appropriate treatment for CPP.
*Testicular ultrasound*
- While useful for evaluating testicular size and consistency, it is typically performed when there is suspicion of **peripheral precocious puberty** (e.g., Leydig cell tumor) with low LH/FSH or significant testicular asymmetry, which is not the primary presentation here.
- The elevated basal LH and FSH values indicate a **central origin** of puberty, making a testicular ultrasound less immediately relevant as a *next step* compared to directly addressing the central hormonal drive.
*Cortisol supplementation*
- This would be indicated for conditions causing **adrenal insufficiency**, such as **congenital adrenal hyperplasia (CAH)** with salt-wasting or Addison's disease.
- CAH typically presents with virilization and advanced bone age but would show **low LH/FSH** (due to peripheral androgen excess) and elevated adrenal androgens (e.g., DHEA-S, 17-hydroxyprogesterone), which are not described.
*Radiation therapy*
- This is a treatment for **malignant tumors**, often used in cases of brain tumors.
- The MRI of the brain showed **no abnormalities**, ruling out a pituitary or hypothalamic tumor as the cause of CPP in this case, thus making radiation therapy inappropriate.
*Observation*
- **Observation** alone is inappropriate given the significant **advancement of bone age** (10 years in a 7-year-old) and clear signs of central precocious puberty.
- Untreated CPP can lead to **compromised adult height potential** due to premature epiphyseal fusion and psychosocial issues, necessitating intervention.
Delayed puberty US Medical PG Question 5: A 17-year-old female presents to her pediatrician due to lack of menstruation. She states that she developed breasts 4 years ago but has not experienced menses yet. The patient denies abdominal pain and has no past medical history. Her mother underwent menarche at age 13. The patient is a volleyball player at school, is single, and has never attempted intercourse. At this visit, her temperature is 98.3°F (36.8°C), blood pressure is 110/76 mmHg, pulse is 72/min, and respirations are 14/min. She is 5 feet 7 inches tall and weighs 116 pounds (BMI 18.2 kg/m²). Exam shows Tanner IV breasts, Tanner I pubic hair, and minimal axillary hair. External genitalia are normal, but the vagina is a 5-centimeter blind pouch. Which of the following is the most appropriate initial diagnostic test?
- A. Obtain FSH and estrogen levels (Correct Answer)
- B. Vaginoplasty
- C. ACTH stimulation test
- D. Gonadectomy
- E. Estrogen replacement therapy
Delayed puberty Explanation: ***Obtain FSH and estrogen levels***
- The patient presents with **primary amenorrhea**, breast development (Tanner IV), but absent pubic/axillary hair (Tanner I) and a blind pouch vagina. These findings are highly suspicious for **Androgen Insensitivity Syndrome (AIS)**.
- Measuring **Follicle-Stimulating Hormone (FSH)** and **estrogen levels** will help differentiate between causes of primary amenorrhea, particularly in cases of suspected gonadal dysfunction or end-organ unresponsiveness. Elevated FSH would suggest gonadal failure, while normal to high estrogen despite absent menses points towards hormonal unresponsiveness.
*Vaginoplasty*
- This is a surgical procedure to create or lengthen the vagina and is a **definitive treatment** for conditions like Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome or severe vaginal agenesis, but it is not an initial diagnostic step.
- Performing surgery without a clear diagnosis is inappropriate and premature, as the underlying cause of the blind vaginal pouch needs to be identified first.
*ACTH stimulation test*
- An **ACTH stimulation test** is used to diagnose **adrenal insufficiency** or **congenital adrenal hyperplasia (CAH)**.
- While CAH can cause ambiguous genitalia and primary amenorrhea in some forms, this patient has normal female external genitalia and breast development, making CAH less likely, and this test isn't the primary diagnostic step for her presentation.
*Gonadectomy*
- **Gonadectomy** is the surgical removal of gonads and is typically performed in individuals with certain **Disorders of Sex Development (DSDs)**, such as AIS with intra-abdominal testes, to prevent **gonadal malignancy**.
- This is a **treatment** measure, not a diagnostic test, and is only considered after a definitive diagnosis of the underlying condition.
*Estrogen replacement therapy*
- **Estrogen replacement therapy** might be considered as a treatment for **hypogonadism** or to induce secondary sexual characteristics in certain types of primary amenorrhea (e.g., gonadal dysgenesis).
- However, in a patient with breast development (Tanner IV), estrogen production is likely occurring, making it an inappropriate initial diagnostic choice or treatment, especially before determining the cause of amenorrhea.
Delayed puberty US Medical PG Question 6: A 15-year-old boy is brought to the physician by his mother for a well-child examination. He recently stopped attending his swim classes. The patient is at the 97th percentile for height and the 50th percentile for weight. Examination shows decreased facial hair, bilateral breast enlargement, and long extremities. Genital examination shows scant pubic hair, small testes, and a normal-sized penis. Further evaluation is most likely to show which of the following karyotypes?
- A. 45,XO/46,XX
- B. 45,XO
- C. 47,XYY
- D. 46,XX/46,XY
- E. 47,XXY (Correct Answer)
Delayed puberty Explanation: ***47,XXY***
- The patient's presentation with **tall stature**, **gynecomastia**, **small testes**, and **scant pubic hair** is characteristic of **Klinefelter syndrome**, which is caused by a **47,XXY karyotype**.
- **Hypogonadism** in Klinefelter syndrome leads to **decreased testosterone production**, explaining the lack of facial hair and undeveloped secondary sexual characteristics.
*45,XO/46,XX*
- This mosaic karyotype is associated with **Turner syndrome**, which primarily affects females and presents with features like **short stature**, **gonadal dysgenesis**, and **webbed neck**.
- Males with this karyotype are rare and would not exhibit the typical features described, such as **gynecomastia** and eunuchoid body habitus.
*45,XO*
- This is the classic karyotype for **Turner syndrome**, which is exclusively found in phenotypic females.
- Individuals with 45,XO present with **short stature**, **streak gonads**, and a lack of secondary sexual characteristics, none of which align with the male patient's symptoms.
*47,XYY*
- Individuals with **XYY syndrome** (Jacob syndrome) are typically **tall** but usually have **normal sexual development** and **fertility**.
- This karyotype does not explain the **gynecomastia**, **small testes**, or **decreased facial hair** seen in the patient.
*46,XX/46,XY*
- This karyotype indicates **gonadal mosaicism**, also known as **ovotesticular disorder of sex development (DSD)** or **chimerism**, where an individual has both ovarian and testicular tissue.
- While it can present with ambiguous genitalia and mixed secondary sexual characteristics, the specific constellation of **tall stature**, **gynecomastia**, and **small testes** is more indicative of Klinefelter syndrome.
Delayed puberty US Medical PG Question 7: A 17-year-old girl is brought to the physician by her mother because she has not had her menstrual period yet. At birth, she had ambiguous genitalia. The mother reports that during the pregnancy she had noticed abnormal hair growth on her chin. A year ago, the girl broke her distal radius after a minor trauma. She is at the 95th percentile for height and 50th percentile for weight. Physical examination shows nodulocystic acne on the face, chest, and upper back. Breast development is at Tanner stage I. Pelvic examination reveals normal pubic hair with clitoromegaly. A pelvic ultrasound shows ovaries with multiple cysts and a normal uterus. Which of the following is the most likely diagnosis?
- A. Aromatase deficiency
- B. Kallmann syndrome
- C. Polycystic ovary syndrome
- D. Mullerian agenesis
- E. Congenital adrenal hyperplasia (Correct Answer)
Delayed puberty Explanation: ***Congenital adrenal hyperplasia (CAH)***
- The patient's **ambiguous genitalia at birth**, maternal virilization during pregnancy, clitoromegaly, **primary amenorrhea**, and nodulocystic acne are all characteristic signs of **classic congenital adrenal hyperplasia**, specifically 21-hydroxylase deficiency.
- The tall stature (95th percentile for height) is consistent with **accelerated growth** due to excess androgens, while **lack of breast development** (Tanner stage I) and **cystic ovaries** suggest impaired estrogen production and anovulation.
*Aromatase deficiency*
- This condition presents with **ambiguous genitalia at birth** in females and leads to **primary amenorrhea** and **virilization** in adolescence due to the inability to convert androgens to estrogens.
- However, patients with aromatase deficiency often have **tall stature** with delayed epiphyseal fusion due to low estrogen levels, which doesn't fully align with the patient's current growth pattern and other findings.
*Kallmann syndrome*
- This syndrome is characterized by **hypogonadotropic hypogonadism** and **anosmia** (loss of smell), leading to **primary amenorrhea** and **absent/delayed puberty**; however, it does not cause androgen excess or ambiguous genitalia.
- Patients with Kallmann syndrome would typically present with **eunuchoid proportions** rather than tall stature, and would not have clitoromegaly or acne due to androgen excess.
*Polycystic ovary syndrome (PCOS)*
- While PCOS presents with **anovulation**, **hirsutism**, and **polycystic ovaries**, it typically manifests in adolescence or adulthood and does not cause **ambiguous genitalia at birth** or clitoromegaly to the extent described.
- The onset of symptoms in PCOS is usually insidious, and the patient's history of ambiguous genitalia points to a congenital adrenal issue.
*Mullerian agenesis*
- This condition, also known as Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome, causes **primary amenorrhea** due to **absent or underdeveloped uterus and vagina**.
- However, patients with Mullerian agenesis have **normal secondary sexual characteristics** (breast development, pubic hair pattern) and external female genitalia, and do not exhibit signs of androgen excess like ambiguous genitalia or clitoromegaly.
Delayed puberty US Medical PG Question 8: A 15-year-old boy is brought to the physician for a well-child visit. His parents are concerned that he has not had his growth spurt yet. As a child, he was consistently in the 60th percentile for height; now he is in the 25th percentile. His classmates make fun of his height and high-pitched voice. His parents are also concerned that he does not maintain good hygiene. He frequently forgets to shower and does not seem aware of his body odor. As an infant, he had bilateral orchidopexy for cryptorchidism and a cleft palate repair. He is otherwise healthy. Vital signs are within normal limits. On physical exam, axillary and pubic hair is sparse. Genitals are Tanner stage 1 and the testicles are 2 mL bilaterally. Which of the following is the most likely diagnosis?
- A. Constitutional delay of puberty
- B. Hyperprolactinemia
- C. Hypothyroidism
- D. Primary hypogonadism
- E. Kallmann syndrome (Correct Answer)
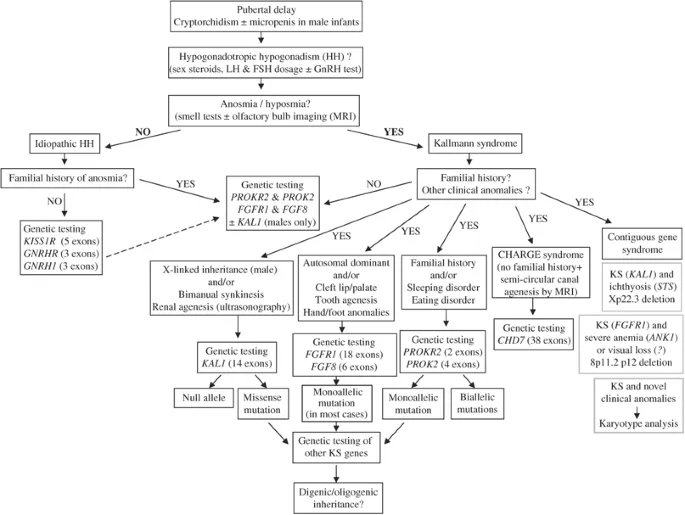
Delayed puberty Explanation: ***Kallmann syndrome***
- This patient's presentation with **anosmia/hyposmia** (implied by poor hygiene and lack of awareness of body odor), **delayed puberty** (Tanner stage 1 at 15 years old, small testicular volume), and a history of **cryptorchidism** and **cleft palate** is highly suggestive of Kallmann syndrome.
- Kallmann syndrome is a form of **congenital hypogonadotropic hypogonadism** characterized by a deficiency in **GnRH** migration and function, leading to impaired sexual development and a lack of olfactory bulb development.
*Constitutional delay of puberty*
- While constitutional delay also presents with delayed puberty, it typically does **not include associated congenital anomalies** like cryptorchidism or cleft palate, nor does it present with features suggestive of anosmia.
- Children with constitutional delay often have a family history of delayed puberty, and their **growth deceleration** is usually less pronounced and still follows a growth curve.
*Hyperprolactinemia*
- **Hyperprolactinemia** causes hypogonadism by inhibiting GnRH, leading to delayed puberty, but it is not associated with **anosmia**, **cryptorchidism**, or **cleft palate**.
- It would typically be investigated if central nervous system symptoms like **headaches** or **visual field defects** were present, or in the context of certain medications.
*Hypothyroidism*
- **Hypothyroidism** can cause delayed puberty and growth deceleration, but it is not associated with **anosmia**, **cryptorchidism**, or **cleft palate**.
- Other classic symptoms of hypothyroidism, such as **fatigue, weight gain, cold intolerance, and constipation**, are not mentioned.
*Primary hypogonadism*
- **Primary hypogonadism** (e.g., Klinefelter syndrome) would present with elevated gonadotropins (LH and FSH) due to testicular failure, unlike the hypogonadotropic hypogonadism seen in Kallmann syndrome.
- While cryptorchidism can lead to primary hypogonadism, the additional features of **anosmia/hyposmia** and **cleft palate** point specifically to Kallmann syndrome.
Delayed puberty US Medical PG Question 9: An 11-year-old girl presents to the pediatrician with her mother, who is concerned about her sexual development. She mentions that she herself experienced the onset of menses at the age of 10.5 years, while her daughter has still not had a menstrual period. However, she is otherwise a healthy girl with no significant medical problems since birth. On physical examination, her vital signs are stable. Evaluation of breast and pubic hair are Tanner stage 2. The pediatrician reassures the mother that her daughter's sexual development is within the normal range for girls and there is nothing to worry about at present. Which is a sign of Tanner stage 2?
- A. Pubarche
- B. Adrenarche
- C. Menarche
- D. Thelarche (Correct Answer)
- E. Coarse pubic hair
Delayed puberty Explanation: ***Thelarche***
- **Thelarche** refers to the initial development of breast buds, which is the defining characteristic of **Tanner stage 2** breast development.
- This stage indicates the beginning of puberty, marked by a slight elevation of the breast and papilla, forming a small mound.
*Pubarche*
- **Pubarche** refers to the appearance of **pubic hair**, which is typically seen in **Tanner stage 2** for pubic hair development, but not breast development.
- While girls often experience pubarche around the same time as thelarche, the term specifically describes pubic hair growth, not breast development.
*Adrenarche*
- **Adrenarche** is the maturation of the adrenal cortex, leading to increased production of adrenal androgens and typically precedes the physical changes of puberty.
- It refers to the biochemical process of adrenal androgen secretion, not a specific physical sign of **Tanner stage 2** development.
*Menarche*
- **Menarche** is the first menstrual period, which occurs much later in puberty, typically after a significant progression through **Tanner stages 2-4**.
- This event signifies reproductive maturity and is not present at the initial stage of breast budding.
*Coarse pubic hair*
- The presence of **coarse pubic hair** indicates a more advanced stage of pubic hair development, typically **Tanner stage 3 or 4**, as hair becomes darker and coarser.
- **Tanner stage 2** pubic hair is usually sparse, long, straight, and lightly pigmented.
Delayed puberty US Medical PG Question 10: An 8-year-old boy is brought to the hospital because of blurred vision and headache for 3 months. During this period, the father has noticed that the child has been tilting his head back to look straight ahead. The patient has also had difficulty falling asleep for 2 months. He has had a 3.5 kg (7.7 lb) weight loss over the past 6 months. His temperature is 37.7°C (99.8°F), pulse is 105/min, and blood pressure is 104/62 mm Hg. Examination shows equal pupils that are not reactive to light. The pupils constrict when an object is brought near the eye. His upward gaze is impaired; there is nystagmus and eyelid retraction while attempting to look upwards. Neurologic examination shows no other focal findings. Which of the following is the most likely sequela of this patient's condition?
- A. Diabetes insipidus
- B. Blindness
- C. Subarachnoid hemorrhage
- D. Diabetic ketoacidosis
- E. Precocious puberty (Correct Answer)
Delayed puberty Explanation: ***Precocious puberty***
- The constellation of **Parinaud syndrome** (impaired upward gaze, nystagmus, eyelid retraction, and pupillary abnormalities) combined with symptoms of **increased intracranial pressure** (headache, blurred vision, weight loss, difficulty sleeping) in a child points to a **pineal tumor**, specifically a **germinoma**.
- Pineal germinomas are known to secrete **human chorionic gonadotropin (hCG)**, which can cross-react with LH receptors, leading to stimulation of **testosterone production** and subsequent **precocious puberty** in boys.
*Diabetes insipidus*
- While diabetes insipidus can be associated with suprasellar tumors, it's less commonly a direct sequela of a **pineal germinoma** itself compared to precocious puberty, although mass effect on the hypothalamus could potentially lead to it.
- The primary symptoms described are classic for **Parinaud syndrome** and increased intracranial pressure, not specific signs of diabetes insipidus (e.g., polyuria, polydipsia).
*Blindness*
- **Vision loss or blindness** can occur due to long-standing **papilledema** from increased intracranial pressure, or direct compression of the **optic chiasm** or **optic nerves** by a large tumor.
- While a possible serious complication, **precocious puberty** is a more specific and direct endocrinological sequela linked to the hormonal activity of a pineal germinoma in boys.
*Subarachnoid hemorrhage*
- Although any intracranial tumor can potentially bleed, a **subarachnoid hemorrhage** typically presents with a sudden onset of **"thunderclap" headache**, stiff neck, and altered consciousness.
- The patient's symptoms have been evolving over 3 months, which is inconsistent with the acute presentation of a subarachnoid hemorrhage.
*Diabetic ketoacidosis*
- **Diabetic ketoacidosis (DKA)** is a severe complication of **type 1 diabetes mellitus**, characterized by hyperglycemia, metabolic acidosis, and ketonemia.
- There are no clinical signs or symptoms in this presentation (e.g., polyuria, polydipsia, Kussmaul respirations, fruity breath) to suggest uncontrolled diabetes or DKA, and it is not a direct sequela of a pineal tumor.
More Delayed puberty US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.