Catch-up growth US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Catch-up growth. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Catch-up growth US Medical PG Question 1: A 7-day-old male infant presents to the pediatrician for weight loss. There is no history of excessive crying, irritability, lethargy, or feeding difficulty. The parents deny any history of fast breathing, bluish discoloration of lips/nails, fever, vomiting, diarrhea, or seizures. He was born at full term by vaginal delivery without any perinatal complications and his birth weight was 3.6 kg (8 lb). Since birth he has been exclusively breastfed and passes urine six to eight times a day. His physical examination, including vital signs, is completely normal. His weight is 3.3 kg (7.3 lb); length and head circumference are normal for his age and sex. Which of the following is the next best step in the management of the infant?
- A. Reassurance of parents (Correct Answer)
- B. Evaluation of the mother for malnutrition
- C. Admission of the infant in the NICU to treat with empiric intravenous antibiotics
- D. Emphasize the need to clothe the infant warmly to prevent hypothermia
- E. Supplementation of breastfeeding with an appropriate infant formula
Catch-up growth Explanation: ***Reassurance of parents***
- A **weight loss of 8.3%** (300g from 3.6kg) is within the expected range for a 7-day-old exclusively breastfed infant, which can be up to 7-10% in the first week.
- The infant's normal physical exam, good urine output, and lack of other symptoms suggest **adequate feeding** and overall well-being.
*Evaluation of the mother for malnutrition*
- The mother's nutritional status is not directly indicative of the infant's weight loss within the normal physiological range in this scenario.
- There is no information to suggest the mother is malnourished or that it would directly impact the quality or quantity of breast milk to cause pathological weight loss.
*Admission of the infant in the NICU to treat with empiric intravenous antibiotics*
- This is an overly aggressive intervention as there are **no signs or symptoms of infection** (e.g., fever, lethargy, poor feeding) and the infant appears well.
- Empiric antibiotics are not warranted in an otherwise healthy, full-term infant with normal physiological weight loss.
*Emphasize the need to clothe the infant warmly to prevent hypothermia*
- The infant's **vital signs are normal**, indicating no hypothermia, and there is no clinical evidence to support this as a primary concern.
- While maintaining warmth is important, it is not the next best step for addressing this specific presentation of physiological weight loss.
*Supplementation of breastfeeding with an appropriate infant formula*
- Supplementation is typically not needed for physiological weight loss in an otherwise healthy, exclusively breastfed infant with **adequate urine output** and no signs of dehydration.
- Encouraging continued exclusive breastfeeding and providing support for proper latch and feeding techniques would be more appropriate if there were concerns about inadequate milk intake.
Catch-up growth US Medical PG Question 2: A 15-year-old female presents to her family physician for an annual school physical exam and check-up. She is accompanied by her mother to the visit and is present in the exam room. The patient has no complaints, and she does not have any past medical problems. She takes no medications. The patient reports that she remains active, exercising 5 times a week, and eats a healthy and varied diet. Which of the following would be the best way for the physician to obtain a more in-depth social history, including sexual history and use of alcohol, tobacco, or recreational drugs?
- A. Disallow the mother to be present in the examination room throughout the entirety of the visit
- B. Give the patient a social history questionnaire to fill out in the exam room
- C. Ask the mother to step outside into the hall for a portion of the visit (Correct Answer)
- D. Ask the patient the questions directly, with her mother still in the exam room
- E. Speak softly to the patient so that the mother does not hear and the patient is not embarrassed
Catch-up growth Explanation: ***Ask the mother to step outside into the hall for a portion of the visit***
- This approach allows the physician to speak with the adolescent **privately and confidentially**, which is crucial for obtaining sensitive information such as sexual history, drug use, and mental health concerns.
- Adolescents are more likely to disclose personal information when their parents are not present, fostering trust and ensuring **comprehensive history-taking** vital for their well-being.
*Disallow the mother to be present in the examination room throughout the entirety of the visit*
- This is an **overly restrictive** approach that might create tension or distrust between the physician, patient, and parent, especially at the start of the visit.
- While privacy is essential for sensitive topics, parental presence can be valuable for discussing general health, family history, and **treatment plans**, especially for younger adolescents.
*Give the patient a social history questionnaire to fill out in the exam room*
- While questionnaires can be useful for gathering basic information, they often **lack the nuance** of a direct conversation and may not prompt the patient to elaborate on sensitive issues.
- Furthermore, having the mother present while the patient fills out a questionnaire on sensitive topics still **compromises confidentiality** and may lead to incomplete or dishonest answers.
*Ask the patient the questions directly, with her mother still in the exam room*
- Asking sensitive questions with a parent present is **unlikely to yield truthful and complete answers**, as adolescents may feel embarrassed, judged, or fear parental disapproval.
- This approach compromises the **confidentiality** that is fundamental to building trust with adolescent patients.
*Speak softly to the patient so that the mother does not hear and the patient is not embarrassed*
- Speaking softly is **unprofessional** and still does not guarantee privacy, as the mother might still overhear parts of the conversation.
- This method also **fails to establish true confidentiality**, which is central to building rapport and encouraging open communication with adolescent patients about sensitive topics.
Catch-up growth US Medical PG Question 3: A 4-month-old boy is brought to the physician for a well-child examination. He was born at 39 weeks gestation via spontaneous vaginal delivery and is exclusively breastfed. He weighed 3,400 g (7 lb 8 oz) at birth. At the physician's office, he appears well. His pulse is 146/min, the respirations are 39/min, and the blood pressure is 78/44 mm Hg. He weighs 7.5 kg (16 lb 9 oz) and measures 65 cm (25.6 in) in length. The remainder of the physical examination is normal. Which of the following developmental milestones has this patient most likely met?
- A. Sits with support of pelvis
- B. Grasps small objects between thumb and finger
- C. Transfers objects from hand to hand
- D. Intentionally rolls over (Correct Answer)
- E. Bounces actively when held in standing position
Catch-up growth Explanation: ***Intentionally rolls over***
- Rolling over is a common developmental milestone achieved between **4 to 6 months** of age.
- At 4 months, an infant typically has sufficient **head control** and **trunk strength** to intentionally roll from tummy to back or back to tummy.
*Sits with support of pelvis*
- Sitting with **pelvic support** (tripod sitting) is generally achieved around **6 to 7 months** of age.
- A 4-month-old typically lacks the necessary **trunk stability** and strength for this milestone.
*Grasps small objects between thumb and finger*
- This describes a **pincer grasp**, which is a fine motor skill usually developed around **9-12 months** of age.
- At 4 months, infants primarily use a **palmar grasp** (raking motion) to pick up objects.
*Transfers objects from hand to hand*
- Transferring objects from hand to hand is a fine motor milestone typically achieved between **5 and 7 months** of age.
- A 4-month-old is beginning to reach for objects but usually has difficulty with **smooth transfers** between hands.
*Bounces actively when held in standing position*
- Active bouncing when held in a standing position is typically seen around **6 months** when infants start putting more weight on their legs.
- At 4 months, while an infant might bear some weight, **active bouncing** is usually more rudimentary or absent.
Catch-up growth US Medical PG Question 4: A 2-year-old girl is brought to the physician by her mother for a well-child examination. She is at the 55th percentile for height and the 40th percentile for weight. Vital signs are within normal limits. Physical examination shows no abnormalities. She is able to follow simple commands, such as “close your eyes, then stick out your tongue,” but she is unable to follow 3-step commands. She knows approximately 75 words, and half of her speech is understandable. She can say 2-word phrases, and she is able to name many parts of the body. Assuming normal development, which of the following milestones would be expected in a patient this age?
- A. Hops on one foot
- B. Engages in role-playing
- C. Separates easily from parents
- D. Pedals a tricycle
- E. Builds a tower of 6 cubes (Correct Answer)
Catch-up growth Explanation: ***Builds a tower of 6 cubes***
- At 2 years old, children typically develop fine motor skills enabling them to stack **6 to 7 cubes** to build a tower, demonstrating good hand-eye coordination.
- This milestone aligns well with the described cognitive development, such as following multi-step commands and early language acquisition.
*Hops on one foot*
- **Hopping on one foot** is a gross motor skill usually achieved later, typically around **4 years of age**.
- A 2-year-old child is more likely to be developing skills like running, jumping with two feet, or walking up and down stairs.
*Engages in role-playing*
- While toddlers engage in **imitative play**, true imaginative **role-playing** with complex scenarios and multiple characters typically develops later, around **3 years of age or older**.
- At 2, play is often more focused on mimicking observed actions.
*Separates easily from parents*
- At 2 years old, many children are still experiencing **separation anxiety**, especially in unfamiliar situations.
- **Easy separation** from parents is a milestone typically achieved later as children develop more independence and social confidence, often closer to 3 or 4 years of age.
*Pedals a tricycle*
- **Pedaling a tricycle** requires coordinated gross motor skills, balance, and cognitive understanding that are typically developed around **3 years of age**.
- A 2-year-old may be able to sit on a tricycle and push with their feet, but not yet pedal efficiently.
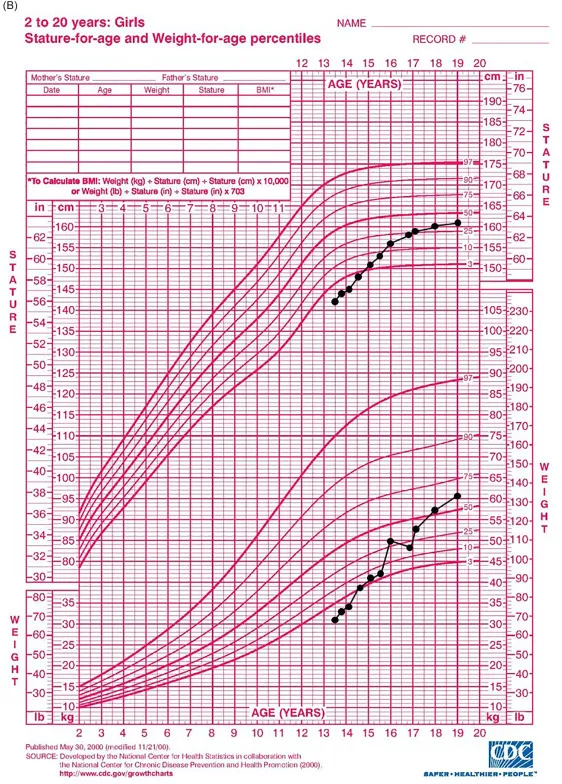
Catch-up growth US Medical PG Question 5: A concerned mother presents to clinic stating that her 14-year-old son has not gone through his growth spurt. She states that, although shorter, he had been growing at the same rate as his peers until the past year. There is no evidence of delayed puberty in the mother, but the father's history is unknown. The patient has no complaints. On physical exam, the patient is a healthy-appearing 14-year-old boy whose height is below the third percentile and whose weight is at the 50th percentile. His bone age is determined to be 11 years. A laboratory workup, including thyroid stimulating hormone (TSH), is unremarkable. What is the most likely diagnosis?
- A. Hypothyroidism
- B. Familial short stature
- C. Constitutional growth delay (Correct Answer)
- D. Growth hormone deficiency
- E. Celiac disease
Catch-up growth Explanation: ***Constitutional growth delay***
- This condition is characterized by **delayed bone age**, normal growth velocity initially followed by a deceleration, and an eventual **catch-up growth spurt** leading to normal adult height. The patient's history of being shorter than peers but growing at the same rate, followed by a recent slow down, and a bone age of 11 years (compared to his chronological age of 14) strongly indicates this.
- The absence of other symptoms, **unremarkable lab workup** (including TSH), and the fact that he was previously growing at the same rate as peers further supports constitutional growth delay, which is often linked to a family history of delayed puberty, even if the mother's history is negative and the father's is unknown.
*Hypothyroidism*
- **Hypothyroidism** would typically present with symptoms such as fatigue, weight gain, constipation, and cold intolerance, none of which are mentioned in the patient's history.
- The **unremarkable TSH** level rules out hypothyroidism as the cause of growth delay in this case.
*Familial short stature*
- In **familial short stature**, children typically grow along a short but otherwise normal percentile curve, and their bone age would typically match their chronological age.
- The patient's growth deceleration and significantly **delayed bone age** are inconsistent with familial short stature.
*Growth hormone deficiency*
- **Growth hormone deficiency** often presents with a significant deceleration of growth velocity and very short stature for age, but usually the bone age delay is more pronounced or proportional to the chronological age.
- While low height is present, the **otherwise healthy appearance** and absence of other metabolic or health issues make constitutional growth delay more likely, especially with the provided bone age and normal lab results.
*Celiac disease*
- **Celiac disease** can cause growth delay, but it would typically be accompanied by gastrointestinal symptoms such as abdominal pain, diarrhea, or malabsorption-related issues like weight loss or anemia.
- This patient is **asymptomatic** and has a normal weight for his height percentiles, which makes celiac disease an unlikely diagnosis.
Catch-up growth US Medical PG Question 6: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Catch-up growth Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Catch-up growth US Medical PG Question 7: A 1-year-old male presents to his pediatrician for a well-child visit. Through a history from the mother and physical examination, the pediatrician learns that the baby babbles non-specifically, takes several steps independently, and picks up his cereal using two fingers. His weight is currently 22 lbs (birth-weight 6 lbs, 9 oz), and his height is 30 inches (birth length 18 inches). Are there any aspects of this child's development that are delayed?
- A. Fine motor skill delay
- B. Language delay (Correct Answer)
- C. Inadequate growth
- D. Gross motor skill delay
- E. There are no developmental concerns
Catch-up growth Explanation: ***Language delay***
- At 1 year of age, a child should typically be babbling with **specific sounds** and attempting to say their **first words**.
- The child's non-specific babbling suggests a delay in typical **expressive language development**.
*Fine motor skill delay*
- The child is able to pick up cereal using **two fingers**, indicating the development of a **pincer grasp**.
- This is an **age-appropriate fine motor skill** for a 1-year-old.
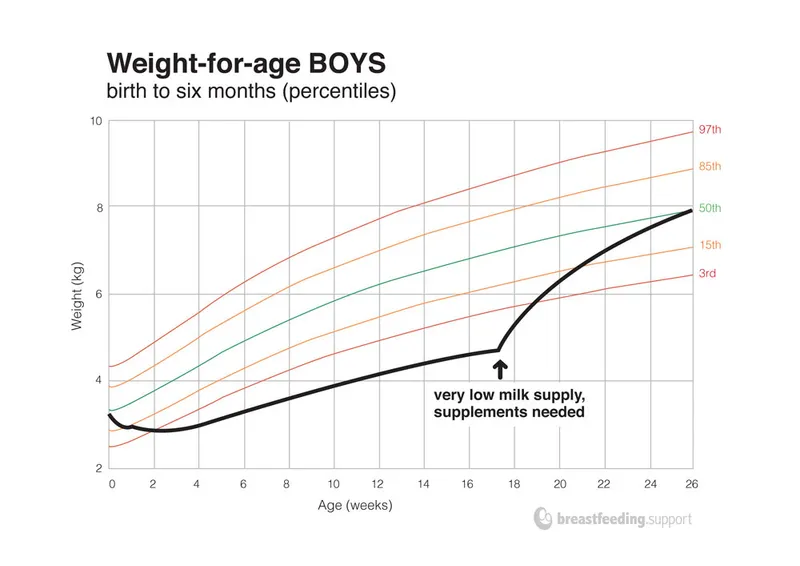
*Inadequate growth*
- The child has over **tripled his birth weight** (from 6 lbs, 9 oz to 22 lbs) and more than doubled his birth length (from 18 to 30 inches), which are **normal growth patterns** for the first year of life.
- While weight values can be plotted on growth charts, the provided information strongly suggests **adequate growth**.
*Gross motor skill delay*
- The child is taking **several steps independently**, which is an **age-appropriate gross motor milestone** for a 1-year-old.
- Many children take their first independent steps between 9 and 15 months.
*There are no developmental concerns*
- While many milestones are met, the **non-specific babbling** at 1 year strongly suggests a **language delay**.
- It is crucial to identify and address any potential delays early for intervention.
Catch-up growth US Medical PG Question 8: An 8-month-old girl is brought to the emergency department because of fever, vomiting, and diarrhea for 3 days. Her parents report at least 10 watery stools daily. She has had three upper respiratory tract infections since she started daycare 2 months ago, but has otherwise been developing normally. Her mother has a history of celiac disease. The patient is at the 57th percentile for height and the 65th percentile for weight. Her immunizations are incomplete. Her temperature is 38.5°C (101.3°F), pulse is 145/min, and blood pressure is 92/54 mm Hg. Examination shows dry mucous membranes and decreased skin turgor. Bowel sounds are hyperactive. A complete blood count and serum concentrations of glucose, urea nitrogen, and creatinine are within the reference range; there is hypokalemia. In addition to intravenous fluid resuscitation, which of the following is the most appropriate next step in management?
- A. Examination of the stool for ova and parasites
- B. Sonography of the abdomen
- C. Administration of antidiarrheal medication
- D. Enzyme immunoassay of stool (Correct Answer)
- E. Blood cultures
Catch-up growth Explanation: ***Enzyme immunoassay of stool***
- The patient presents with classic symptoms of **rotavirus gastroenteritis**, including fever, vomiting, and voluminous watery diarrhea, especially given her age, daycare exposure, and **incomplete immunization status** (missing rotavirus vaccine).
- **Enzyme immunoassay (EIA)** is a rapid, accurate test for detecting rotavirus antigens in stool, providing diagnosis confirmation within hours.
- While rotavirus gastroenteritis is managed primarily with **supportive care and rehydration** (already initiated), diagnostic testing is indicated here for: (1) **confirming the diagnosis** in an incompletely immunized child, (2) **infection control measures** in daycare/hospital settings, and (3) guiding parental counseling about immunization completion.
- EIA is the most appropriate next diagnostic step after stabilization has begun.
*Examination of the stool for ova and parasites*
- Stool O&P examination is appropriate for **persistent or chronic diarrhea** (>7-14 days), travel history, or suspected parasitic infection.
- Acute viral gastroenteritis typically presents with sudden onset of severe watery diarrhea, as seen here, rather than the more protracted course typical of parasitic infections.
- Parasitic causes are less likely in an otherwise healthy infant in a developed country without travel history.
*Sonography of the abdomen*
- **Abdominal sonography** would be indicated if there were concerns for **intussusception** (intermittent colicky pain, currant jelly stools, palpable mass) or other structural abnormalities.
- The patient's presentation with **diffuse watery diarrhea**, fever, and vomiting is classic for infectious gastroenteritis, not a surgical abdomen.
- Hyperactive bowel sounds further support an infectious rather than obstructive process.
*Administration of antidiarrheal medication*
- **Antidiarrheal medications are contraindicated** in infants and young children with acute infectious diarrhea.
- These agents (e.g., loperamide, bismuth subsalicylate) do not treat the underlying infection, can **prolong illness** by retaining pathogens, and risk serious complications including **toxic megacolon**, ileus, and CNS depression.
- The mainstay of treatment remains **oral or intravenous rehydration** and electrolyte replacement.
*Blood cultures*
- **Blood cultures** are indicated when there is concern for **bacteremia or sepsis**, typically suggested by high fever (>39°C), severe systemic toxicity, immunocompromise, or abnormal laboratory findings.
- This patient, while febrile, has **normal CBC, glucose, BUN, and creatinine**, making invasive bacterial infection less likely.
- The clinical picture is most consistent with **viral gastroenteritis**, which rarely causes bacteremia in immunocompetent children.
Catch-up growth US Medical PG Question 9: A 3-month-old African American boy presents to his pediatrician’s office for his routine well visit. He was born full-term from an uncomplicated vaginal delivery. He is exclusively breastfeeding and not receiving any medications or supplements. Today, his parents report no issues or concerns with their child. He is lifting his head for brief periods and smiling. He has received only 2 hepatitis B vaccines. Which of the following is the correct advice for this patient’s parents?
- A. He should be sleeping more.
- B. He should have his serum lead level checked to screen for lead intoxication.
- C. He should start vitamin D supplementation. (Correct Answer)
- D. He should start rice cereal.
- E. He needs a 3rd hepatitis B vaccine.
Catch-up growth Explanation: ***He should start vitamin D supplementation.***
- **Exclusively breastfed** infants, regardless of maternal vitamin D intake, require **vitamin D supplementation** due to insufficient amounts in breast milk.
- The recommended daily dose is **400 IU** starting from the first few days of life, to prevent **rickets** and promote bone health.
- **African American infants** have an additional risk factor due to increased skin melanin content, which reduces cutaneous vitamin D synthesis from sunlight exposure.
*He should be sleeping more.*
- A 3-month-old infant typically sleeps between **14-17 hours per day**, with **waking periods to feed** and interact.
- The case description does not indicate any concerns with the child's sleep patterns, and **developmental milestones** like lifting his head and smiling are being met.
*He should have his serum lead level checked to screen for lead intoxication.*
- **Lead screening** is not routinely recommended for all infants unless specific **risk factors** are present, such as living in an older home with lead paint, or having siblings with elevated lead levels.
- There are no reported risk factors for lead exposure in this patient's history.
*He should start rice cereal.*
- Introduction of solid foods, such as rice cereal, is typically recommended around **6 months of age**, when the infant shows signs of **developmental readiness**.
- These signs include **head control**, sitting with support, and showing interest in food.
*He needs a 3rd hepatitis B vaccine.*
- The **third dose of the hepatitis B vaccine** is typically administered between **6 and 18 months of age**.
- At 3 months old, the infant is not yet due for his third dose.
Catch-up growth US Medical PG Question 10: A 2-month-old girl is brought to the physician for a well-child examination. She was born at 32 weeks' gestation and weighed 1616 g (3 lb 9 oz); she currently weighs 2466 g (5 lb 7 oz). She is exclusively breastfed and receives vitamin D supplementation. Physical examination shows no abnormalities apart from low height and weight. This patient is at increased risk for which of the following complications?
- A. Iron deficiency anemia (Correct Answer)
- B. Hemorrhage
- C. Scurvy
- D. Subacute combined degeneration
- E. Intussusception
Catch-up growth Explanation: ***Iron deficiency anemia***
- Preterm infants have **lower iron stores** at birth due to reduced placental transfer in the third trimester.
- Their rapid growth rate and exclusive breastfeeding (breast milk has low iron content) further increase their risk of **iron deficiency anemia**.
*Hemorrhage*
- While preterm infants are at higher risk for certain hemorrhages (e.g., intraventricular hemorrhage), this typically occurs in the **immediate neonatal period** and risk significantly decreases by 2 months of age.
- Hemorrhage is not a common long-term complication unique to a 2-month-old preterm infant without additional risk factors.
*Scurvy*
- Scurvy is caused by **vitamin C deficiency**, which is typically not a concern in breastfed infants as breast milk provides adequate vitamin C.
- The primary deficiency risk addressed by supplementation in breastfed infants is vitamin D, not vitamin C.
*Subacute combined degeneration*
- This condition is caused by **vitamin B12 deficiency**, leading to demyelination of the spinal cord.
- While possible in infants of vegan mothers, it is unlikely in a breastfed infant without specific dietary restrictions in the mother.
*Intussusception*
- Intussusception is a condition where one segment of the intestine telescopes into another, usually occurring between **3 months and 3 years of age**.
- It is not specifically linked to prematurity or low birth weight as an increased long-term risk.
More Catch-up growth US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.