Prader-Willi and Angelman syndromes US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Prader-Willi and Angelman syndromes. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Prader-Willi and Angelman syndromes US Medical PG Question 1: A mother from rural Louisiana brings her 4-year-old son to a pediatrician. Her son is intellectually disabled, and she hopes that genetic testing will help determine the cause of her son's condition. She had previously been opposed to allowing physicians to treat her son, but his impulsive behavior and learning disabilities are making it difficult to manage his care on her own. On exam, the child has a long, thin face with a large jaw, protruding ears, and macroorchidism. The physician also hears a high-pitched holosystolic murmur at the apex of the heart that radiates to the axilla. Which of the following trinucleotide repeats is most likely affected in this individual?
- A. GAA on chromosome 9
- B. CGG on the sex chromosome X (Correct Answer)
- C. CTG on chromosome 19
- D. CTG on chromosome 8
- E. CAG on chromosome 4
Prader-Willi and Angelman syndromes Explanation: ***CGG on the sex chromosome X***
- The constellation of **intellectual disability**, a **long, thin face with a large jaw**, **protruding ears**, and **macroorchidism** are classic features of **Fragile X syndrome**.
- Fragile X syndrome is caused by an expansion of the **CGG trinucleotide repeat** in the **FMR1 gene** on the **X chromosome**. The **high-pitched holosystolic murmur at the apex radiating to the axilla** suggests **mitral valve prolapse**, which is also frequently associated with Fragile X.
*GAA on chromosome 9*
- This describes the **GAA trinucleotide repeat expansion** associated with **Friedreich's ataxia**, affecting the **FXN gene** on **chromosome 9**.
- Friedreich's ataxia is characterized by **progressive ataxia**, **dysarthria**, and **loss of vibratory/proprioceptive sensation**, not macroorchidism or the specific facial features seen here.
*CTG on chromosome 19*
- This describes the **CTG trinucleotide repeat expansion** associated with **myotonic dystrophy type 1**, affecting the **DMPK gene** on **chromosome 19**.
- Myotonic dystrophy is characterized by **myotonia** (delayed muscle relaxation), **muscle weakness**, and **cataracts**, which are not consistently present in this case.
*CTG on chromosome 8*
- While **CTG repeats** are involved in some genetic conditions, the specific association with **chromosome 8** as a cause for the described symptoms (intellectual disability, specific facial features, macroorchidism, and mitral valve prolapse) is not a common trinucleotide repeat disorder.
- This option does not correspond to a recognized trinucleotide repeat disorder that presents with the given clinical picture.
*CAG on chromosome 4*
- This describes the **CAG trinucleotide repeat expansion** associated with **Huntington's disease**, affecting the **HTT gene** on **chromosome 4**.
- Huntington's disease typically presents with **chorea**, **psychiatric symptoms**, and **dementia** later in life, not with the childhood onset intellectual disability and physical features described.
Prader-Willi and Angelman syndromes US Medical PG Question 2: A 4-year-old child presents with developmental delay, ataxia, and inappropriate laughter. The parents undergo genetic testing to determine the cause of their child's symptoms. Results show no mutations in all three family members that would cause this constellation of symptoms. Karyotyping reveals no deletions, insertions, or gene translocations. However, methylation studies demonstrate abnormal imprinting patterns at the 15q11-q13 region. Based on these findings, the child is diagnosed with Angelman syndrome. Which of the following genetic mechanisms best describes the cause of this disorder?
- A. Variable expressivity
- B. Uniparental disomy
- C. Incomplete penetrance
- D. Anticipation
- E. Imprinting defect (Correct Answer)
Prader-Willi and Angelman syndromes Explanation: ***Imprinting defect***
- **Angelman syndrome** in this case results from a **primary imprinting defect** at the 15q11-q13 region, causing abnormal methylation patterns without deletions, mutations, or uniparental disomy.
- The key diagnostic findings are: **normal karyotype** (ruling out deletions), **no mutations in family members** (ruling out UBE3A mutations), and **abnormal methylation studies** demonstrating the imprinting center defect.
- An **imprinting defect** refers to an error in the establishment or maintenance of methylation patterns at imprinted genes, which in this case leads to silencing of the maternally inherited *UBE3A* gene expression.
- This mechanism accounts for approximately **3-5%** of Angelman syndrome cases and is diagnosed specifically through methylation studies when other causes are excluded.
*Uniparental disomy*
- While **paternal uniparental disomy (UPD)** of chromosome 15 can cause Angelman syndrome, it would typically be detected through genetic testing and represents a different mechanism.
- UPD involves inheriting **two copies of a chromosome from one parent** and none from the other, which **leads to** an imprinting defect as a secondary consequence.
- The question stem emphasizes that methylation studies were the key finding after ruling out mutations and karyotype abnormalities, suggesting a **primary imprinting center defect** rather than UPD.
*Variable expressivity*
- This refers to individuals with the **same genotype** exhibiting **different phenotypes** ranging from mild to severe.
- While Angelman syndrome can show variable severity, this term describes **phenotypic variation**, not the underlying genetic mechanism causing the disorder.
*Incomplete penetrance*
- This occurs when only a **portion of individuals** with a particular genotype actually **express the associated phenotype**.
- In Angelman syndrome due to imprinting defects, the condition is fully penetrant when the genetic abnormality is present, so this is not the relevant mechanism.
*Anticipation*
- **Anticipation** describes symptoms becoming **more severe** and/or appearing at **earlier ages** in succeeding generations.
- This phenomenon is associated with **trinucleotide repeat expansion disorders** (e.g., Huntington disease, myotonic dystrophy), not imprinting disorders like Angelman syndrome.
Prader-Willi and Angelman syndromes US Medical PG Question 3: A 5-year-old boy is brought to the physician because of behavioral problems. His mother says that he has frequent angry outbursts and gets into fights with his classmates. He constantly complains of feeling hungry, even after eating a full meal. He has no siblings, and both of his parents are healthy. He is at the 25th percentile for height and is above the 95th percentile for weight. Physical examination shows central obesity, undescended testes, almond-shaped eyes, and a thin upper lip. Which of the following genetic changes is most likely associated with this patient's condition?
- A. Mitotic nondisjunction of chromosome 21
- B. Mutation of FBN-1 gene on chromosome 15
- C. Microdeletion of long arm of chromosome 7
- D. Loss of paternal gene expression on chromosome 15 (Correct Answer)
- E. Deletion of Phe508 on chromosome 7
Prader-Willi and Angelman syndromes Explanation: ***Loss of paternal gene expression on chromosome 15***
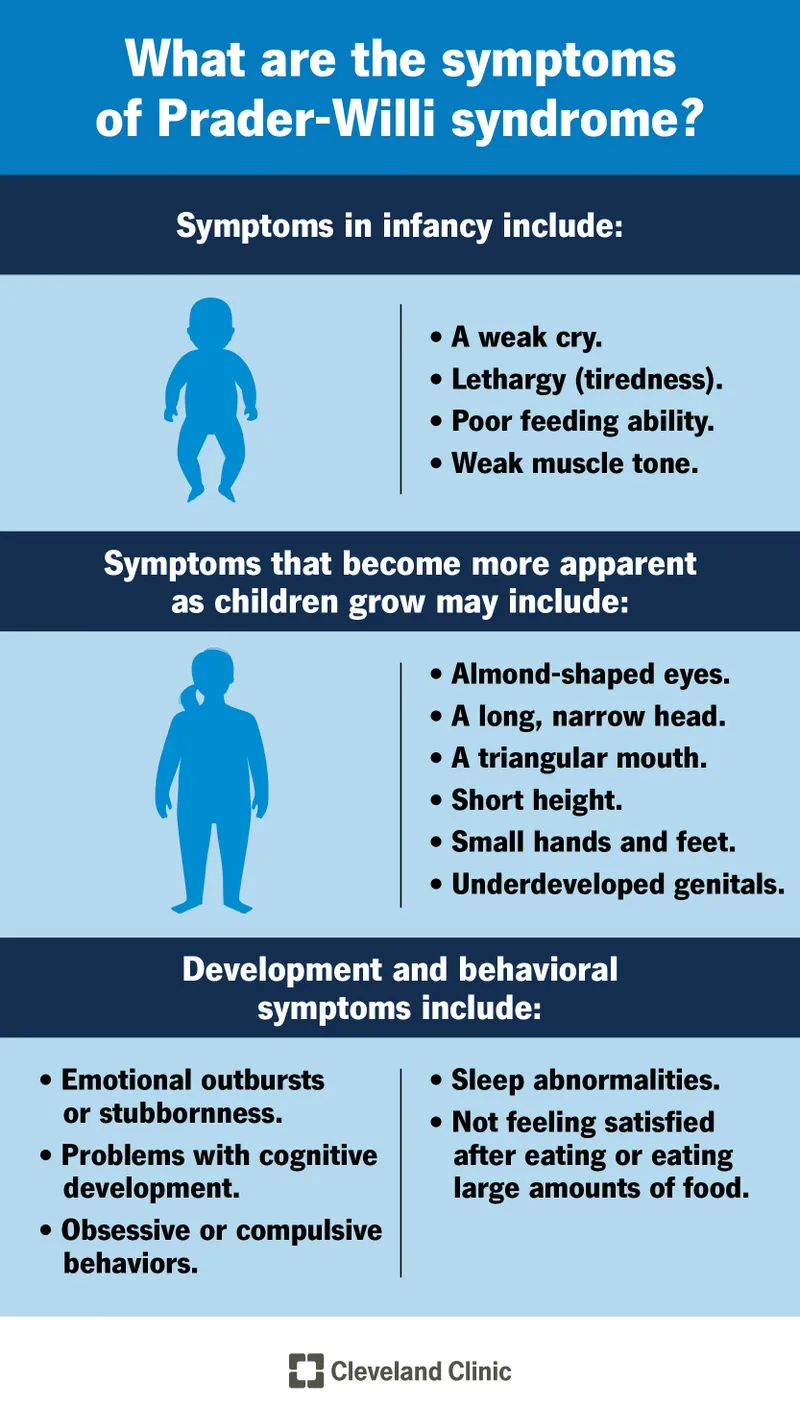
- The patient's symptoms, including **hyperphagia**, **obesity**, behavioral issues, short stature, and **hypogonadism** (undescended testes), are characteristic of **Prader-Willi syndrome**.
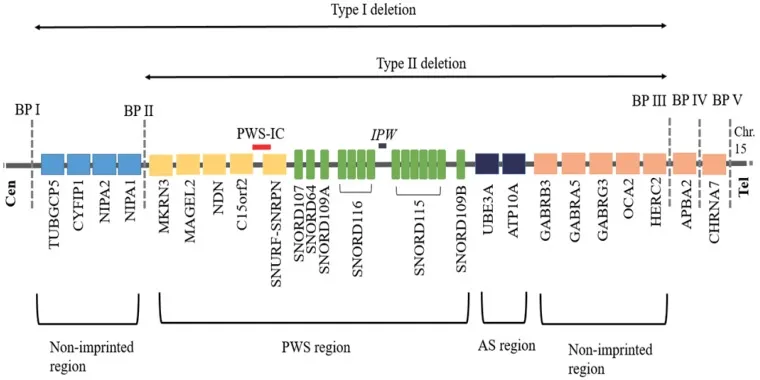
- Prader-Willi syndrome is most commonly caused by the **loss of paternal gene expression** from the **q11-q13 region of chromosome 15**, either due to a paternal deletion, maternal uniparental disomy, or a defect in the imprinting center.
*Microdeletion of long arm of chromosome 7*
- A microdeletion on the long arm of chromosome 7 (7q11.23) is associated with **Williams syndrome**, characterized by an **elfin facial appearance**, supravalvular aortic stenosis, and intellectual disability.
- This does not match the patient's symptoms of obesity, hyperphagia, or hypogonadism.
*Deletion of Phe508 on chromosome 7*
- A deletion of phenylalanine at position 508 (**ΔF508**) on chromosome 7 is the most common mutation in the **cystic fibrosis transmembrane conductance regulator (CFTR)** gene, causing **cystic fibrosis**.
- Cystic fibrosis is an **autosomal recessive disorder** requiring mutations in both alleles (inherited from both parents), and primarily affects the exocrine glands, leading to lung disease, pancreatic insufficiency, and infertility, which are unrelated to the patient's presentation.
*Mutation of FBN-1 gene on chromosome 15*
- A mutation in the **FBN1 gene** on chromosome 15 (15q21.1) causes **Marfan syndrome**, which is a connective tissue disorder.
- Marfan syndrome presents with tall stature, long limbs (**arachnodactyly**), lens dislocation, and aortic root dilation, none of which are described in this patient.
*Mitotic nondisjunction of chromosome 21*
- Mitotic nondisjunction of chromosome 21 can lead to **mosaic Down syndrome**, but **trisomy 21** (due to meiotic nondisjunction) is the most common cause of Down syndrome.
- Down syndrome is associated with characteristic facial features, intellectual disability, and congenital heart defects, which are distinct from the symptoms presented.
Prader-Willi and Angelman syndromes US Medical PG Question 4: An 8-year-old boy is brought to the physician for evaluation of developmental delay and recurrent tonic-clonic seizures. There is no family history of seizures or other serious illness. Current medications include risperidone for hyperactivity. He is at the 17th percentile for head circumference. Examination shows protrusion of the mandible, strabismus, and a laughing facial expression. His gait is unsteady. He has a vocabulary of about 200 words and cannot speak in full sentences. Karyotype analysis shows a 46, XY karyotype without chromosomal deletions. Which of the following genetic mechanisms best explains this patient's findings?
- A. Trinucleotide repeat in FMR1 gene
- B. De novo mutation of MECP2 on the X chromosome
- C. Chromosome 22q11 microdeletion
- D. Uniparental disomy of chromosome 15 (Correct Answer)
- E. Nondisjunction of chromosome 21 during meiosis I
Prader-Willi and Angelman syndromes Explanation: ***Uniparental disomy of chromosome 15***
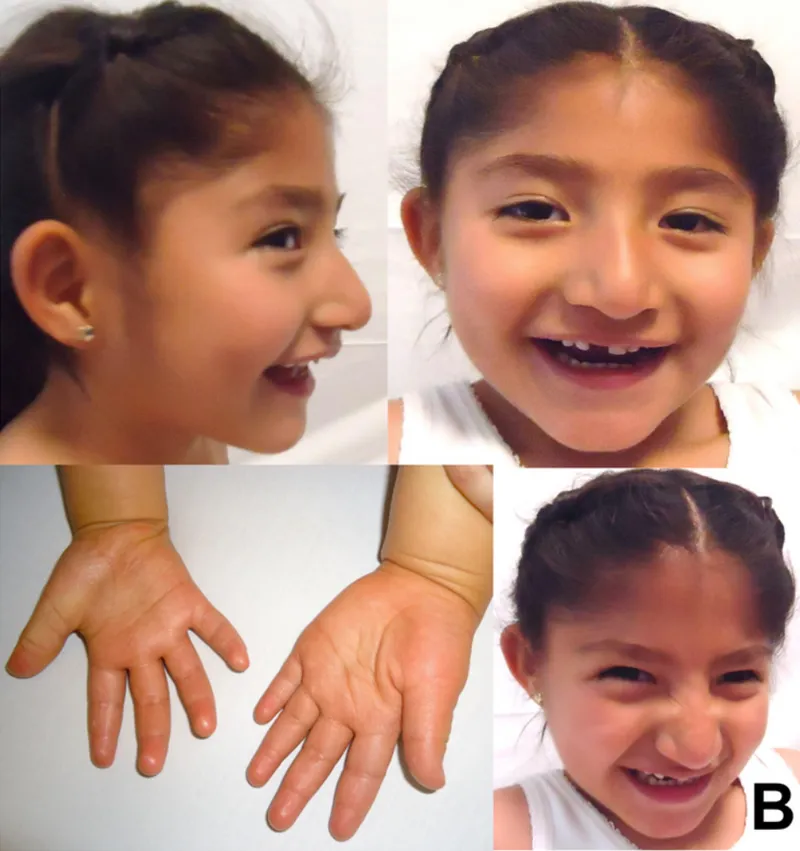
- The presented symptoms—developmental delay, recurrent tonic-clonic seizures, mandibular protrusion, strabismus, paroxysmal laughter, unsteady gait, and speech impairment—are all characteristic features of **Angelman syndrome**.
- **Angelman syndrome** is typically caused by the loss of function of the maternal copy of the *UBE3A* gene on chromosome 15q11-q13. This can occur due to a maternal deletion, a paternal **uniparental disomy** (inheriting both copies of chromosome 15 from the father), or a mutation in the *UBE3A* gene.
- In this case, the normal karyotype without chromosomal deletions points to **paternal uniparental disomy** as the mechanism.
*Trinucleotide repeat in FMR1 gene*
- This describes the genetic basis of **Fragile X syndrome**, which is characterized by intellectual disability, behavioral problems (e.g., hyperactivity, autism-like features), and characteristic physical features such as a **long face**, large ears, and **macro-orchidism in males**.
- While there is developmental delay and hyperactivity, the specific facial features (mandibular protrusion, laughing expression) and unsteady gait are not typical for Fragile X syndrome.
*De novo mutation of MECP2 on the X chromosome*
- This describes the genetic basis of **Rett syndrome**, which almost exclusively affects females and is characterized by a period of normal development followed by regression in communication and motor skills, **stereotypic hand movements**, microcephaly, and seizures.
- The patient is a male and presents with features inconsistent with Rett syndrome.
*Chromosome 22q11 microdeletion*
- This is associated with **DiGeorge syndrome** or velocardiofacial syndrome, characterized by cardiac defects, abnormal facies, thymic hypoplasia, cleft palate, and hypocalcemia.
- The symptoms described in the patient (seizures, laughing expression, gait ataxia) are not typical for 22q11 deletion syndrome.
*Nondisjunction of chromosome 21 during meiosis I*
- This is the most common cause of **Down syndrome** (Trisomy 21), characterized by intellectual disability, characteristic facial features (upslanting palpebral fissures, epicanthic folds, flat nasal bridge), and associated medical problems like congenital heart defects and hypotonia.
- The patient's symptoms, particularly the prominent mandible, strabismus, and laughing expression, do not align with the typical presentation of Down syndrome.
Prader-Willi and Angelman syndromes US Medical PG Question 5: A six-year-old male presents to the pediatrician for a well child visit. The patient’s parents report that they are struggling to manage his temper tantrums, which happen as frequently as several times per day. They usually occur in the morning before school and during mealtimes, when his parents try to limit how much he eats. The patient often returns for second or third helpings at meals and snacks throughout the day. The patient’s parents have begun limiting the patient’s food intake because he has been gaining weight. They also report that the patient recently began first grade but still struggles with counting objects and naming letters consistently. The patient sat without support at 11 months of age and walked at 17 months of age. He is in the 99th percentile for weight and 5th percentile for height. On physical exam, he has almond-shaped eyes and a downturned mouth. He has poor muscle tone.
Which of the following additional findings would most likely be seen in this patient?
- A. Webbed neck
- B. Macroorchidism
- C. Ataxia
- D. Hemihyperplasia
- E. Hypogonadism (Correct Answer)
Prader-Willi and Angelman syndromes Explanation: ***Hypogonadism***
- The patient's presentation, including **hyperphagia**, **obesity**, developmental delay, and distinctive facial features (almond-shaped eyes, downturned mouth, poor muscle tone), is highly suggestive of **Prader-Willi Syndrome**.
- **Hypogonadism** (undescended testes in males, delayed puberty) is a classic feature of **Prader-Willi Syndrome** due to hypothalamic dysfunction, which also causes the voracious appetite.
*Webbed neck*
- A **webbed neck** is characteristic of **Turner Syndrome** (45, XO), which affects females and is associated with short stature, but not typically with the hyperphagia and obesity seen here.
- The patient is a male, making Turner Syndrome an unlikely diagnosis.
*Macroorchidism*
- **Macroorchidism** (enlarged testes) is a hallmark feature of **Fragile X Syndrome**, which is associated with intellectual disability and developmental delays.
- While fragile X syndrome involves developmental delay, it does not typically present with the extreme hyperphagia, obesity, and specific facial features described in the patient.
*Ataxia*
- **Ataxia** (lack of voluntary coordination of muscle movements) in conjunction with developmental delays can be seen in various neurological disorders such as **Friedreich's ataxia** or **cerebral palsy**.
- This symptom is not a primary or characteristic finding in Prader-Willi Syndrome, and the other described features point away from ataxia as the most likely additional finding.
*Hemihyperplasia*
- **Hemihyperplasia** (overgrowth of one side of the body) is associated with conditions like **Beckwith-Wiedemann Syndrome**, which also involves macroglossia and an increased risk of tumors.
- This finding is not typically associated with the constellation of symptoms (hyperphagia, obesity, intellectual disability, hypotonia) seen in Prader-Willi Syndrome.
Prader-Willi and Angelman syndromes US Medical PG Question 6: A 12-year-old boy is brought by his mother to a neurologist for continuing evaluation of seizures. His seizures were previously well-controlled on medication but over the last month he has been having seizures several times per week. The boy is non-verbal and has had severe developmental delays and cognitive disability since birth. On exam, the boy is found to be enthusiastically playing with the toys in the office and laughing at almost any stimulus. Furthermore, his movements are found to be uncoordinated with a wide based gait. Previous genetic testing has revealed an abnormality in an E3 ubiquitin ligase gene. Compared to unaffected individuals, which of the following patterns of gene expression is most likely seen in this patient?
- A. Abnormally increased expression of the gene from the maternal chromosome
- B. Abnormally decreased expression of the gene from the maternal chromosome (Correct Answer)
- C. Abnormally decreased expression of the gene from both chromosomes
- D. Abnormally decreased expression of the gene from the paternal chromosome
- E. Abnormally increased expression of the gene from the paternal chromosome
Prader-Willi and Angelman syndromes Explanation: ***Abnormally decreased expression of the gene from the maternal chromosome***
- This patient's symptoms (non-verbal, severe developmental delays, cognitive disability, seizures, uncoordinated movements, wide-based gait, inappropriate laughter, and an abnormality in an E3 ubiquitin ligase gene) are characteristic of **Angelman syndrome**.
- Angelman syndrome is typically caused by a deletion or mutation on the **maternally inherited copy of chromosome 15q11-q13**, specifically affecting the *UBE3A* gene, which is an E3 ubiquitin ligase. This leads to reduced or absent expression of the *UBE3A* gene in critical brain regions where only the maternal allele is expressed.
*Abnormally increased expression of the gene from the maternal chromosome*
- Angelman syndrome is caused by a **loss of function** of the maternally inherited *UBE3A* gene, not an increase in its expression.
- Increased expression would not lead to the neurodevelopmental deficits seen in Angelman syndrome.
*Abnormally decreased expression of the gene from both chromosomes*
- While there is decreased expression of the functional *UBE3A* gene, the paternal allele is normally **silenced** in specific brain regions relevant to Angelman syndrome pathogenesis due to **genomic imprinting**. Therefore, the issue is with the maternal allele.
- If both chromosomes had decreased expression, it would imply a different genetic mechanism or a more severe, potentially lethal, condition.
*Abnormally decreased expression of the gene from the paternal chromosome*
- In the brain regions relevant to Angelman syndrome, the paternal *UBE3A* allele is normally **silenced** due to genomic imprinting. Therefore, its decreased expression would not be an abnormal finding or contribute to the pathology.
- Problems with the paternal allele in this region are associated with **Prader-Willi syndrome**, which has a different clinical presentation (e.g., hypotonia, hyperphagia, obesity).
*Abnormally increased expression of the gene from the paternal chromosome*
- The paternal *UBE3A* allele is normally **silenced** in the relevant brain regions; therefore, an increased expression would be abnormal but is not the genetic basis of Angelman syndrome.
- Angelman syndrome is caused by the **loss or absence of functional maternal *UBE3A*** expression, not altered paternal expression.
Prader-Willi and Angelman syndromes US Medical PG Question 7: A 1-year-old girl born to a 40-year-old woman is undergoing an examination by a pediatric resident in the hospital. The pregnancy was uneventful and there were no complications during the delivery. The physical examination reveals midface hypoplasia with a flat nasal bridge and upslanting palpebral fissures. She has a small mouth and chest auscultation reveals a blowing holosystolic murmur that is heard best along the sternal border. The family history is unremarkable. A karyotype analysis is ordered because the resident suspects a numerical chromosomal disorder. Which of the following phenomena leads to the infant’s condition?
- A. Meiotic non-disjunction (Correct Answer)
- B. Uniparental disomy
- C. Genomic imprinting
- D. Partial deletion
- E. Trinucleotide repeat
Prader-Willi and Angelman syndromes Explanation: ***Meiotic non-disjunction***
- The combination of **midface hypoplasia**, **upslanting palpebral fissures**, **flat nasal bridge**, and a **holosystolic murmur** (suggesting a **ventricular septal defect**) in an infant born to an older mother is highly characteristic of **Down syndrome (Trisomy 21)**.
- **Trisomy 21** is most commonly caused by **meiotic non-disjunction**, where homologous chromosomes fail to separate during meiosis I or sister chromatids fail to separate during meiosis II, resulting in a gamete with an extra chromosome 21.
*Uniparental disomy*
- **Uniparental disomy** occurs when an individual receives both copies of a chromosome from a single parent, rather than one from each parent.
- While it can lead to various genetic disorders, it does not typically cause **Trisomy 21** or the specific constellation of features described.
*Genomic imprinting*
- **Genomic imprinting** is an epigenetic phenomenon where certain genes are expressed in a parent-of-origin specific manner.
- While relevant to conditions like Prader-Willi or Angelman syndromes, it is not the mechanism responsible for **Trisomy 21**.
*Partial deletion*
- A **partial deletion** refers to the loss of a segment of a chromosome.
- While chromosomal deletions cause various syndromes (e.g., Cri-du-chat syndrome), they would result in a **monosomy or partial monosomy**, not the extra chromosome seen in Trisomy 21.
*Trinucleotide repeat*
- **Trinucleotide repeat disorders** involve an abnormal expansion of a three-nucleotide sequence within a gene, leading to conditions like Huntington's disease or fragile X syndrome.
- This mechanism is not associated with the etiology of **Down syndrome**.
Prader-Willi and Angelman syndromes US Medical PG Question 8: A 4-year-old girl is brought to the physician by her parents because she is severely underweight. She is easily fatigued and has difficulty keeping up with other children at her daycare. She has a good appetite and eats 3 full meals a day. She has 4 to 5 bowel movements daily with bulky, foul-smelling stools that float. She has had recurrent episodes of sinusitis since infancy. Her parents report that she recently started to snore during her sleep. She is at the 15th percentile for height and 3rd percentile for weight. Her vital signs are within normal limits. Examination shows pale conjunctivae. A few scattered expiratory crackles are heard in the thorax. There is abdominal distention. Which of the following is the most likely underlying cause of this patient's failure to thrive?
- A. T. whippelii infiltration of intestinal villi
- B. Impaired intestinal amino acid transport
- C. Exocrine pancreatic insufficiency (Correct Answer)
- D. Small intestine bacterial overgrowth
- E. Intestinal inflammatory reaction to gluten
Prader-Willi and Angelman syndromes Explanation: ***Exocrine pancreatic insufficiency***
- The constellation of **failure to thrive**, **bulky, foul-smelling, floating stools** (suggesting **steatorrhea**), recurrent **sinusitis**, and **recurrent respiratory symptoms** (snoring, expiratory crackles) is highly indicative of **cystic fibrosis**, whose primary cause of malabsorption is **exocrine pancreatic insufficiency**.
- **Cystic fibrosis** leads to thick, viscous secretions that obstruct pancreatic ducts, preventing digestive enzymes from reaching the small intestine and causing **malabsorption of fats and fat-soluble vitamins**.
*T. whippelii infiltration of intestinal villi*
- This describes **Whipple's disease**, which typically affects **middle-aged men** and presents with malabsorption, arthralgia, and neurological symptoms.
- It is rare in children and usually presents with symptoms like diarrhea and weight loss, but not commonly with the **recurrent respiratory infections** and **pancreatic insufficiency** seen here.
*Impaired intestinal amino acid transport*
- This typically refers to conditions like **Hartnup disease**, which involves defective transport of neutral amino acids and can lead to **pellagra-like symptoms** (dermatitis, diarrhea, dementia) due to niacin deficiency.
- This condition does not explain the **steatorrhea**, **recurrent sinusitis**, or **respiratory symptoms** found in the patient.
*Small intestine bacterial overgrowth*
- While **SIBO** can cause malabsorption, **abdominal distention**, and loose stools, it does not typically cause **recurrent sinusitis** or the classic **bulky, foul-smelling, floating stools associated with pancreatic insufficiency**.
- SIBO is also not a primary cause of **failure to thrive** in a global sense, but rather a secondary complication.
*Intestinal inflammatory reaction to gluten*
- This describes **celiac disease**, which presents with **malabsorption**, **abdominal distention**, **failure to thrive**, and **anemia** (pale conjunctivae).
- However, celiac disease does not typically cause **recurrent sinusitis** or the **respiratory symptoms** (snoring, crackles) that are prominent in this patient's presentation.
Prader-Willi and Angelman syndromes US Medical PG Question 9: A 3-month-old male presents to the pediatrician with his mother for a well child visit. The patient drinks 4 ounces of conventional cow’s milk formula every three hours. He usually stools once per day, and urinates up to six times per day. His mother reports that he regurgitates a moderate amount of formula through his nose and mouth after most feeds. He does not seem interested in additional feeding after these episodes of regurgitation, and he has become progressively more irritable around meal times. The patient is starting to refuse some feeds. His mother denies ever seeing blood or streaks of red in his stool, and she denies any family history of food allergies or dermatological problems. The patient’s weight was in the 75th percentile for weight throughout the first month of life. Four weeks ago, he was in the 62nd percentile, and he is now in the 48th percentile. His height and head circumference have followed similar trends. On physical exam, the patient smiles reciprocally and can lift his head and chest when in the prone position. His abdomen is soft, non-tender, and non-distended.
Which of the following is the best next step in management?
- A. Switch to hydrolyzed formula
- B. Obtain abdominal ultrasound
- C. Initiate proton pump inhibitor
- D. Provide reassurance
- E. Counsel on positioning and thickening feeds (Correct Answer)
Prader-Willi and Angelman syndromes Explanation: ***Counsel on positioning and thickening feeds***
- The infant's symptoms, including **regurgitation**, **irritability during feeds**, and **dropping weight percentiles**, are indicative of severe gastroesophageal reflux (GER). Initial management should focus on **conservative measures** like positioning modifications (keeping upright after feeds), thickening feeds, and smaller, more frequent feedings.
- Given the absence of **hematemesis**, **hematochezia**, or **projectile vomiting**, further invasive diagnostics or medication are not immediately warranted.
*Switch to hydrolyzed formula*
- This would be considered if there were signs suggestive of a **cow's milk protein allergy**, such as **bloody stools**, **diarrhea**, **eczema**, or a strong family history of allergies, which are all absent in this case.
- Allergy is less likely to be the primary cause of isolated severe regurgitation with failure to thrive without other allergic manifestations.
*Obtain abdominal ultrasound*
- An **abdominal ultrasound** is primarily used to evaluate for conditions like **pyloric stenosis** if there is **projectile vomiting**, an **olive-shaped mass**, or severe dehydration and electrolyte imbalances, none of which are present.
- While it can assess for **malrotation or intussusception**, these conditions typically present with more acute, severe symptoms like **bilious vomiting**, abdominal distension, or currant jelly stools, which are not described.
*Initiate proton pump inhibitor*
- **Proton pump inhibitors (PPIs)** are reserved for infants with confirmed **erosive esophagitis** or severe symptoms unresponsive to lifestyle modifications.
- Starting a PPI without first attempting conservative measures or confirming pathological acid reflux is generally not recommended, especially given potential side effects like increased risk of infections.
*Provide reassurance*
- While **reassurance** is important, it is not the sole appropriate next step. The infant's **dropping weight percentiles** and significant feeding difficulties suggest that this is beyond typical "spitting up" and requires intervention to prevent further impact on growth and comfort.
- Simply reassuring the mother would ignore the clinical signs of **failure to thrive** and significant discomfort during feeds.
Prader-Willi and Angelman syndromes US Medical PG Question 10: A 4-week-old male infant is brought to the physician due to a 1-week history of refusing to finish bottle feeds and becoming irritable shortly after feeding. He spits up sour-smelling milk after most feeds. Pregnancy and delivery were uncomplicated. The baby is at the 70th percentile for length and 50th percentile for weight. His temperature is 36.6°C (98°F), pulse is 180/min, respirations are 30/min, and blood pressure is 85/55 mm Hg. He appears lethargic. Examination shows sunken fontanelles and a strong rooting reflex. The abdomen is soft with a 1.5-cm nontender epigastric mass. Which of the following is the most appropriate next step in the management of this patient?
- A. Obtain abdominal ultrasound
- B. Initiate IV fluid resuscitation (Correct Answer)
- C. Upper GI series
- D. Nasogastric decompression
- E. Surgical consultation for pyloromyotomy
Prader-Willi and Angelman syndromes Explanation: ***Initiate IV fluid resuscitation***
- This infant presents with classic **pyloric stenosis** (non-bilious vomiting, palpable epigastric "olive" mass, progressive feeding intolerance) and clear signs of **dehydration** (sunken fontanelles, lethargy, tachycardia).
- **IV fluid resuscitation is the immediate priority** to correct hypovolemia and the characteristic **hypochloremic, hypokalemic metabolic alkalosis** that develops from persistent vomiting.
- **Key principle**: "Pyloric stenosis is never a surgical emergency" - metabolic stabilization must precede any intervention, including surgery.
- Fluid resuscitation with **normal saline** followed by electrolyte correction is essential before proceeding with diagnostic imaging or definitive surgical management.
*Nasogastric decompression*
- **NG decompression** is important to decompress the stomach, reduce vomiting, and minimize aspiration risk.
- However, it should occur **after or concurrent with IV access establishment**, not before fluid resuscitation in a dehydrated infant.
- While helpful, it does not address the life-threatening **hypovolemia and electrolyte abnormalities** that require immediate correction.
*Obtain abdominal ultrasound*
- **Abdominal ultrasound** is the diagnostic test of choice for pyloric stenosis, showing pyloric muscle thickness >3 mm and channel length >15 mm.
- However, in a **clinically dehydrated and hemodynamically unstable infant**, stabilization takes priority over confirmatory imaging.
- The diagnosis is already strongly suggested by clinical findings (palpable olive, typical presentation), so imaging can wait until after resuscitation begins.
*Upper GI series*
- An **upper GI series** can diagnose pyloric stenosis by showing the "string sign" (narrow pyloric channel) or "shoulder sign."
- **Ultrasound is preferred** due to higher sensitivity/specificity, no radiation exposure, and faster results.
- This test is unnecessary when ultrasound is available and should not delay critical fluid resuscitation.
*Surgical consultation for pyloromyotomy*
- **Pyloromyotomy** is the definitive surgical treatment for pyloric stenosis with excellent outcomes.
- Surgery should **never be performed on a dehydrated, metabolically unstable infant** - this significantly increases perioperative morbidity and mortality.
- Typical stabilization requires **24-48 hours** of fluid and electrolyte correction before surgery is appropriate.
More Prader-Willi and Angelman syndromes US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.