Muscular dystrophies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Muscular dystrophies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Muscular dystrophies US Medical PG Question 1: A 38-year-old man comes to the physician because of a 6-month history of chest discomfort and progressive dyspnea. He cannot do daily chores without feeling out of breath. He was diagnosed in childhood with a milder X-linked dystrophinopathy that has caused progressive proximal muscle weakness and gait abnormalities over the years. Physical examination shows a waddling gait and weak patellar reflexes. Cardiovascular examination shows a holosystolic murmur, displaced point of maximal impulse, and bilateral pitting edema of the ankles. Laboratory studies show elevated levels of brain natriuretic peptide. Which of the following is the most likely underlying cause of this patient's muscle weakness?
- A. Increased number of CTG repeats in the DMPK gene
- B. Interruption of microtubule depolymerization through stabilization of GDP-tubulin
- C. Impaired connection of cytoskeletal actin filaments to membrane-bound dystroglycan (Correct Answer)
- D. Cell–mediated cytotoxicity against skeletal muscle antigens in the endomysium
- E. Defective lysine-hydroxylysine crosslinking of tropocollagen
Muscular dystrophies Explanation: ***Impaired connection of cytoskeletal actin filaments to membrane-bound dystroglycan***
- The description of a **milder X-linked dystrophinopathy** with progressive muscle weakness and gait abnormalities, coupled with cardiac manifestations like a **holosystolic murmur** and elevated **BNP**, is characteristic of a **dystrophinopathy**, such as **Becker muscular dystrophy**.
- **Dystrophin** is a critical protein that links the **cytoskeletal actin filaments** to the **dystroglycan complex** at the sarcolemma, providing mechanical stability to muscle fibers. Impaired connection leads to muscle fragility and degeneration.
*Increased number of CTG repeats in the DMPK gene*
- This describes **myotonic dystrophy type 1**, which is an autosomal dominant condition, not X-linked.
- While it causes muscle weakness, it is also associated with **myotonia**, testicular atrophy, and cataracts, which are not mentioned.
*Interruption of microtubule depolymerization through stabilization of GDP-tubulin*
- This mechanism is associated with **chemotherapeutic agents** like taxanes (e.g., paclitaxel, docetaxel), which interfere with cell division.
- It does not explain a genetic, progressive muscle weakness disorder.
*Cell–mediated cytotoxicity against skeletal muscle antigens in the endomysium*
- This describes the pathophysiology of **polymyositis**, an **inflammatory myopathy**.
- Polymyositis is an autoimmune condition and does not typically present as an X-linked inherited disorder diagnosed in childhood.
*Defective lysine-hydroxylysine crosslinking of tropocollagen*
- This mechanism is characteristic of disorders affecting **collagen synthesis** and cross-linking, such as **Ehlers-Danlos syndrome**.
- These conditions primarily affect connective tissue, leading to joint hypermobility, skin hyperextensibility, and tissue fragility, not primarily progressive muscle weakness due to dystrophin deficiency.
Muscular dystrophies US Medical PG Question 2: A 16-year-old boy is brought to the emergency department after losing consciousness. He had no preceding chest pain or palpitations. His father has cataracts and had frontal balding in his twenties but has no history of cardiac disease. His paternal grandfather also had early-onset balding. His pulse is 43/min. Physical examination shows frontal hair loss, temporal muscle wasting, and testicular atrophy. Neurologic examination shows bilateral foot drop and weakness of the intrinsic hand muscles. An ECG shows bradycardia with third-degree atrioventricular block. The severity of this patient's symptoms compared to that of his father is most likely due to which of the following genetic properties?
- A. Penetrance
- B. Codominance
- C. Anticipation (Correct Answer)
- D. Loss of heterozygosity
- E. Pleiotropy
Muscular dystrophies Explanation: ***Anticipation***
- **Anticipation** describes a genetic phenomenon where the severity of a genetic disorder increases and/or the age of onset decreases in successive generations. This is typical of disorders caused by **trinucleotide repeat expansions**, such as myotonic dystrophy.
- The patient's severe symptoms (third-degree AV block, foot drop, muscle wasting) occurring at a young age, compared to his father's milder symptoms (cataracts, early balding) without cardiac disease, are a classic presentation of anticipation in **myotonic dystrophy type 1 (DM1)**.
*Penetrance*
- **Penetrance** refers to the proportion of individuals with a particular genotype that express the associated phenotype.
- While it explains whether or not a trait is expressed, it does not explain the increasing severity or earlier onset across generations.
*Codominance*
- **Codominance** occurs when two different alleles for a gene are both expressed, and both phenotypes are observable (e.g., AB blood type).
- This concept does not apply to the increasing severity or earlier onset of symptoms observed in this family.
*Loss of heterozygosity*
- **Loss of heterozygosity** is a genetic event where an individual inheriting one mutated allele for a tumor suppressor gene loses the normal allele, leading to disease (e.g., retinoblastoma).
- This mechanism primarily relates to tumor formation and is not relevant to the progressive worsening of symptoms across generations in the context of myotonic dystrophy.
*Pleiotropy*
- **Pleiotropy** refers to a single gene affecting multiple phenotypic traits (e.g., the FBN1 gene in Marfan syndrome affecting skeletal, ocular, and cardiovascular systems).
- While myotonic dystrophy exhibits pleiotropy (affecting multiple systems), pleiotropy itself does not explain the intergenerational increase in severity or decrease in age of onset, which is specifically attributed to anticipation.
Muscular dystrophies US Medical PG Question 3: A 32-year-old man presents to his primary care provider reporting weakness. He recently noticed that he has difficulty letting go of a doorknob or releasing his hand after shaking hands with others. His past medical history is notable for diabetes, for which he takes metformin. He drinks 2-3 beers per day, uses marijuana occasionally, and works as a security guard. His family history is notable for an early cardiac death in his father. His temperature is 98.6°F (37°C), blood pressure is 130/85 mmHg, pulse is 85/min, and respirations are 18/min. On exam, there is notable muscle atrophy in his hands, feet, and neck. He has delayed hand grip release bilaterally and is slow to return from a smile to a neutral facial expression. His gait is normal, and Romberg's test is negative. He also has frontal balding. This patient’s condition is caused by a mutation in which of the following genes?
- A. Dystrophin
- B. SMN1
- C. Frataxin
- D. DMPK (Correct Answer)
- E. DPC
Muscular dystrophies Explanation: ***DMPK***
- The patient's symptoms, including **myotonia** (difficulty releasing grip, slow return from smile), **muscle atrophy** (hands, feet, neck), and **frontal balding**, are classic for **myotonic dystrophy type 1** (DM1).
- DM1 is an autosomal dominant disorder caused by a **trinucleotide repeat expansion** (CTG) in the **dystrophia myotonica protein kinase (DMPK) gene**.
- The **family history of early cardiac death** is also consistent, as cardiac conduction abnormalities and cardiomyopathy are common complications of DM1.
*Dystrophin*
- Mutations in the **dystrophin gene** cause **Duchenne and Becker muscular dystrophies**.
- These conditions typically present with **progressive muscle weakness** and **atrophy**, but not with myotonia, frontal balding, or the characteristic delayed grip release seen in this patient.
*SMN1*
- Mutations in the **survival motor neuron 1 (SMN1) gene** cause **spinal muscular atrophy (SMA)**.
- SMA is characterized by **progressive muscle weakness** and **atrophy** due to degeneration of anterior horn cells, but it does not present with myotonia or frontal balding.
*Frataxin*
- Mutations in the **FXN (frataxin) gene** cause **Friedreich ataxia**.
- This condition primarily affects the **nervous system** (ataxia, dysarthria, sensory loss) and heart (cardiomyopathy), but it does not cause myotonia or frontal balding.
- The **negative Romberg's test** and **normal gait** make Friedreich ataxia unlikely.
*DPC*
- The gene symbol **DPC** is not commonly associated with a known muscular dystrophy or neuromuscular disorder.
- It may refer to **deleted in pancreatic carcinoma locus 4** (DPC4/SMAD4), which is involved in cancer pathways, not neuromuscular diseases.
Muscular dystrophies US Medical PG Question 4: A 19-year-old man comes to the physician for the evaluation of progressive difficulty climbing stairs over the last 2 years. During this period, he has also had problems with running, occasional falls, and standing from a chair. He has not had any vision problems or muscle cramping. There is no personal or family history of serious illness. Neurological examination shows deep tendon reflexes are 2+ bilaterally and sensation to pinprick and light touch is normal. Musculoskeletal examination shows enlarged calf muscles bilaterally. He has a waddling gait. Laboratory studies show a creatine kinase level of 1700 U/L. Which of the following is the most appropriate next step to confirm the diagnosis?
- A. Tensilon test
- B. Anti-Jo-1 antibodies measurement
- C. CT scan of the chest
- D. Electromyography
- E. Genetic analysis (Correct Answer)
Muscular dystrophies Explanation: ***Genetic analysis***
- The patient's presentation with **progressive proximal muscle weakness**, **calf pseudohypertrophy**, **waddling gait**, and a significantly elevated **creatine kinase** level is highly suggestive of a **dystrophinopathy**.
- Given the patient's **age (19 years) and ambulatory status**, this presentation is most consistent with **Becker muscular dystrophy (BMD)** rather than Duchenne (DMD), as DMD patients typically become wheelchair-bound by age 12-13.
- **Genetic analysis**, specifically testing for **dystrophin gene mutations** (e.g., deletions, duplications, point mutations), is the most definitive method to confirm these diagnoses and distinguish between DMD and BMD based on mutation type and dystrophin expression.
*Tensilon test*
- The **Tensilon test** (edrophonium test) is used to diagnose **myasthenia gravis**, a disorder affecting the neuromuscular junction.
- The patient's symptoms (e.g., progressive onset over years, calf pseudohypertrophy) are not typical of myasthenia gravis, which often presents with **fluctuating weakness** and ocular symptoms.
*Anti-Jo-1 antibodies measurement*
- **Anti-Jo-1 antibodies** are associated with **polymyositis** and dermatomyositis, autoimmune inflammatory myopathies.
- While these conditions cause proximal muscle weakness and elevated CK, they typically have an **inflammatory pattern** and do not cause **calf pseudohypertrophy** or a waddling gait in the same manner as muscular dystrophies.
*CT scan of the chest*
- A **CT scan of the chest** is typically used to investigate conditions such as lung pathology, thymoma (associated with myasthenia gravis), or sarcoidosis.
- It is not a primary diagnostic tool for primary muscle disorders like muscular dystrophy.
*Electromyography*
- **Electromyography (EMG)** can help differentiate between **myopathic** and neuropathic conditions by showing characteristic patterns of muscle fiber degeneration.
- While EMG can support a diagnosis of myopathy, it is not as definitive as **genetic analysis** in confirming a specific muscular dystrophy like BMD, especially given the clear clinical picture.
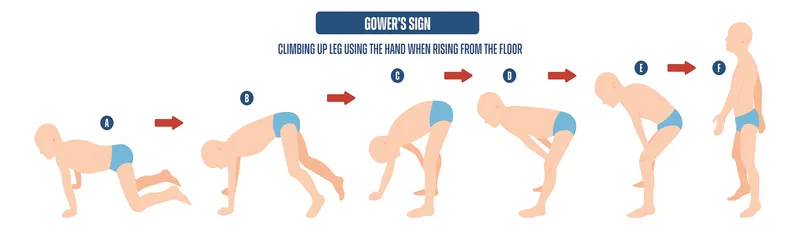
Muscular dystrophies US Medical PG Question 5: A 9-year-old boy is getting fitted for leg braces because he has become too weak to walk without them. He developed normally until age 3 but then he began to get tired more easily and fell a lot. Over time he started having trouble walking and would stand up by using the Gower maneuver. Despite this weakness, his neurologic development is normal for his age. On exam his calves appeared enlarged and he was sent for genetic testing. Sequence data showed that he had a mutation causing a shift in the reading frame, resulting in a severely truncated and non-functional protein. Which of the following types of mutations is most likely the cause of this patient's disorder?
- A. Splice site
- B. Missense
- C. Nonsense
- D. Frameshift (Correct Answer)
- E. Silent
Muscular dystrophies Explanation: ***Frameshift***
- A **frameshift mutation** is caused by the insertion or deletion of nucleotides not in multiples of three, leading to a shift in the reading frame of the mRNA. This results in altered codons downstream of the mutation, typically leading to a **premature stop codon** and a **severely truncated, non-functional protein**.
- The description of a mutation causing "a shift in the reading frame, resulting in a severely truncated and non-functional protein" is characteristic of a frameshift mutation, which is the most common type of mutation in **Duchenne muscular dystrophy** (DMD). The clinical picture (onset around age 3-5, progressive proximal weakness, Gower maneuver, calf pseudohypertrophy) is classic for DMD.
- In DMD, frameshift mutations in the dystrophin gene lead to complete loss of functional dystrophin protein, causing the severe progressive muscle weakness seen in this patient.
*Splice site*
- A **splice site mutation** affects the recognition sequences for intron-exon boundaries during mRNA splicing, potentially leading to exon skipping, intron retention, or use of cryptic splice sites. While splice site mutations can cause DMD (accounting for ~10% of cases), they are less common than frameshifts/deletions.
- The specific description of a "shift in the reading frame" points more directly to a frameshift mutation rather than a splicing defect.
*Missense*
- A **missense mutation** results in a single nucleotide substitution that changes one codon to specify a different amino acid. This produces a full-length protein with a single amino acid substitution.
- Missense mutations typically cause the milder **Becker muscular dystrophy** phenotype (with partially functional dystrophin), not the severe Duchenne phenotype described here. The description of a "severely truncated and non-functional protein" does not fit a missense mutation.
*Nonsense*
- A **nonsense mutation** introduces a premature stop codon directly by changing a codon that normally specifies an amino acid into a stop codon (UAG, UAA, or UGA). This results in a truncated protein.
- While nonsense mutations can cause DMD and do produce truncated proteins, the specific wording "shift in the reading frame" is more characteristic of a frameshift mutation. Nonsense mutations don't shift the reading frame—they directly create a stop signal.
*Silent*
- A **silent (synonymous) mutation** is a nucleotide substitution that does not change the amino acid sequence due to the degeneracy of the genetic code (multiple codons can specify the same amino acid).
- Silent mutations produce normal, full-length proteins and would not cause disease symptoms.
Muscular dystrophies US Medical PG Question 6: A 3-year-old boy presents to the office with his mother. She states that her son seems weak and unwilling to walk. He only learned how to walk recently after a very notable delay. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. He is up to date on all vaccines and is meeting all verbal and social milestones but he has a great deal of trouble with gross and fine motor skills. Past medical history is noncontributory. He takes a multivitamin every day. The mother states that some boys on her side of the family have had similar symptoms and worries that her son might have the same condition. Today, the boy’s vital signs include: blood pressure 110/65 mm Hg, heart rate 90/min, respiratory rate 22/min, and temperature 37.0°C (98.6°F). On physical exam, the boy appears well developed and pleasant. He sits and listens and follows direction. His heart has a regular rate and rhythm and his lungs are clear to auscultation bilaterally. He struggles to get up to a standing position after sitting on the floor. A genetic study is performed that reveals a significant deletion in the gene that codes for dystrophin. Which of the following is the most likely diagnosis?
- A. Limb-girdle muscular dystrophy
- B. Becker muscular dystrophy
- C. Myotonic muscular dystrophy
- D. Emery-Dreifuss muscular dystrophy
- E. Duchenne muscular dystrophy (Correct Answer)
Muscular dystrophies Explanation: ***Duchenne muscular dystrophy***
- The patient's presentation with **delayed walking**, **progressive muscle weakness** (manifesting as difficulty getting up from the floor, i.e., **Gowers' sign**), and the genetic finding of a **significant dystrophin gene deletion** are classic for Duchenne muscular dystrophy (DMD).
- DMD is caused by **out-of-frame deletions** or mutations that result in the **complete absence of functional dystrophin protein**, leading to severe, early-onset muscle weakness.
- DMD is an **X-linked recessive** condition, explaining the maternal family history of similar symptoms in boys, as only males are typically affected.
*Limb-girdle muscular dystrophy*
- This group of disorders also causes progressive muscle weakness, primarily affecting the **proximal muscles** of the shoulders and hips.
- However, these are caused by mutations in genes **other than dystrophin**, and the **specific dystrophin gene deletion** found in this patient points definitively to DMD rather than limb-girdle muscular dystrophy.
*Becker muscular dystrophy*
- Becker muscular dystrophy (BMD) is also caused by mutations in the **dystrophin gene**, but typically involves **in-frame deletions** that produce a **shortened but partially functional** dystrophin protein.
- The **significant deletion** described in this case, combined with the **severe, early-onset presentation** (weakness at age 3, delayed walking), indicates complete loss of dystrophin function characteristic of DMD, not the milder BMD which typically presents later (age 5-15) with slower progression.
*Myotonic muscular dystrophy*
- This condition is characterized by **myotonia** (delayed muscle relaxation) and a multisystemic presentation, often including **facial weakness**, **cataracts**, and cardiac conduction abnormalities.
- It is caused by a **trinucleotide repeat expansion**, not a dystrophin gene deletion, and none of the key features of myotonic dystrophy are described in this patient's presentation.
*Emery-Dreifuss muscular dystrophy*
- Emery-Dreifuss muscular dystrophy (EDMD) is characterized by a classic triad of **early contractures** (elbows, ankles, neck), **progressive muscle weakness** (especially in the humeroperoneal distribution), and **cardiac involvement** (e.g., conduction defects).
- While some forms of EDMD can involve genes related to the dystrophin-associated protein complex, the **dystrophin gene deletion** itself is specific to DMD/BMD, and this patient lacks the characteristic early contractures and cardiac findings of EDMD.
Muscular dystrophies US Medical PG Question 7: A 15-year-old boy comes to the physician for the evaluation of progressive difficulty climbing stairs for the last 2 years. During this period, he has also had problems running and standing up from a seated position. He is at the 50th percentile for height and weight. Examination shows enlarged calf muscles bilaterally and a waddling gait. Which of the following is the most likely cause of this patient's condition?
- A. Large deletions (Correct Answer)
- B. Frameshift mutation
- C. Splice site mutation
- D. Missense mutation
- E. Nonsense mutation
Muscular dystrophies Explanation: ***Large deletions***
- The presented symptoms (progressive difficulty climbing stairs, running, standing, enlarged calf muscles, waddling gait) are classic for **Duchenne muscular dystrophy (DMD)**.
- **Large deletions** (involving one or more exons) are the **most common cause of DMD**, accounting for approximately **60-70%** of cases.
- These deletions typically cause a **frameshift** that leads to a premature stop codon, resulting in absent or severely truncated **dystrophin protein**.
- The **dystrophin gene** is one of the largest human genes, making it particularly susceptible to deletion mutations.
*Frameshift mutation*
- A **frameshift mutation** (insertion or deletion of nucleotides not in multiples of three) leads to an altered reading frame, resulting in a **premature stop codon** downstream.
- While frameshifts do cause **DMD**, they are typically the **consequence** of deletions or small insertions/duplications, not a primary mutation category.
- The question asks for the underlying genetic cause, which is most commonly a large deletion.
*Splice site mutation*
- **Splice site mutations** affect the splicing of introns and exons, potentially leading to exon skipping or inclusion of intronic sequences.
- These account for a small percentage of **DMD** cases but are much less common than large deletions.
- While they can disrupt the reading frame, they represent a minority of causative mutations.
*Missense mutation*
- A **missense mutation** results in a single amino acid change, producing an altered but full-length protein.
- This type of mutation is more characteristic of **Becker muscular dystrophy (BMD)**, a milder form with later onset and slower progression.
- The severe, early-onset phenotype described here is typical of **DMD**, which requires near-complete absence of functional dystrophin.
*Nonsense mutation*
- A **nonsense mutation** introduces a premature stop codon, leading to a truncated protein.
- While nonsense mutations do cause **DMD**, they account for only about **10-15%** of cases as part of the broader category of point mutations.
- Large deletions remain significantly more common as the causative mutation type.
Muscular dystrophies US Medical PG Question 8: A 7-year-old boy is brought to the emergency department by his parents. He is complaining of left-sided knee pain which has progressively increased in severity over the past 2 days. It started when he was playing football with his brothers but he does not recall falling or getting any injury. Past medical history is significant for prolonged bleeding and easy bruising. His maternal uncle has similar problems. Physical exam reveals swollen and painful left knee. His laboratory investigations reveal:
Hemoglobin 11.8 g/dL
WBC count 7,000/mL
Platelets 250,000/mL
INR 0.9
aPTT 62 sec, fully corrected with a mixing study
Which of the following disorders have the same mode of inheritance as this patient’s disease?
- A. Hereditary spherocytosis
- B. Alkaptonuria
- C. Duchenne muscular dystrophy (Correct Answer)
- D. Sickle cell disease
- E. Huntington's disease
Muscular dystrophies Explanation: ***Duchenne muscular dystrophy***
- The patient's presentation with **hemarthrosis** (knee pain and swelling without trauma), **prolonged bleeding**, and **easy bruising**, along with a **prolonged aPTT** that corrects with a mixing study, is highly suggestive of **hemophilia A or B**. Both conditions are **X-linked recessive disorders**, affecting males predominantly.
- **Duchenne muscular dystrophy** is also an **X-linked recessive disorder**, making its mode of inheritance identical to the suspected diagnosis of hemophilia in this patient.
*Hereditary spherocytosis*
- This condition is inherited in an **autosomal dominant** pattern, which is different from the mode of inheritance for hemophilia.
- It is characterized by **hemolytic anemia** due to a defect in red blood cell membrane proteins.
*Alkaptonuria*
- Alkaptonuria is an **autosomal recessive** disorder, caused by a deficiency of homogentisate 1,2-dioxygenase.
- It leads to the accumulation of **homogentisic acid**, causing **dark urine** when exposed to air, **ochronosis**, and **arthropathy**, distinct from the patient's bleeding disorder.
*Sickle cell disease*
- **Sickle cell disease** is an **autosomal recessive** disorder, characterized by abnormal hemoglobin leading to chronic hemolytic anemia and vaso-occlusive crises.
- While it can cause joint pain due to avascular necrosis or infarction, its inheritance pattern is different from the patient's condition.
*Huntington's disease*
- **Huntington's disease** is an **autosomal dominant** neurodegenerative disorder that manifests with progressive motor, cognitive, and psychiatric symptoms, typically in middle age.
- Its inheritance pattern and clinical presentation are distinct from the patient's bleeding disorder.
Muscular dystrophies US Medical PG Question 9: A 17-year-old boy is brought to the pediatrician by his mother for fatigue. The patient reports that he was supposed to try out for winter track this year, but he had to quit because his “legs just give up.” He also reports increased difficulty breathing with exercise but denies chest pain or palpitations. He has no chronic medical conditions and takes no medications. He has had no surgeries in the past. The mother reports that he met all his pediatric milestones and is an “average” student. He is up-to-date on all childhood vaccinations, including a recent flu vaccine. On physical examination, there is mild lumbar lordosis. The patient’s thighs appear thin in diameter compared to his lower leg muscles, and he walks on his toes. An electrocardiogram shows 1st degree atrioventricular nodal block. Which of the following is the most likely cause of the patient’s condition?
- A. Absent dystrophin
- B. Trinucleotide repeats
- C. Abnormal dystrophin (Correct Answer)
- D. Sarcomere protein dysfunction
- E. Peripheral nerve demyelination
Muscular dystrophies Explanation: ***Abnormal dystrophin***
* The patient's presentation with **fatigue**, exercise intolerance, muscular weakness ("legs just give up"), **lumbar lordosis**, **calf pseudohypertrophy** (thighs thin compared to lower legs), and **toe walking** are classic signs of **Becker muscular dystrophy (BMD)**.
* BMD is caused by mutations in the *DMD* gene leading to **abnormally sized or reduced, but still functional, dystrophin protein**. This allows for a milder, later-onset phenotype compared to Duchenne muscular dystrophy.
*Absent dystrophin*
* **Absent dystrophin** is characteristic of **Duchenne muscular dystrophy (DMD)**, which typically presents earlier in childhood with more severe and rapid progression of muscle weakness.
* While both BMD and DMD are X-linked dystrophinopathies, the patient's age (17 years) and milder symptoms are more consistent with the later onset and slower progression seen in BMD.
*Trinucleotide repeats*
* **Trinucleotide repeat disorders** like **myotonic dystrophy** or **Friedreich's ataxia** can cause muscle weakness and cardiac issues but have different clinical presentations.
* Myotonic dystrophy often involves **myotonia** (delayed muscle relaxation), frontal balding, and cataracts, which are not described here.
*Sarcomere protein dysfunction*
* **Sarcomere protein dysfunction** is primarily associated with various forms of **cardiomyopathy** (e.g., hypertrophic cardiomyopathy), which would explain the cardiac findings, but it does not typically cause the specific pattern of limb girdle weakness, calf pseudohypertrophy, and toe walking seen in this patient.
* Conditions like hereditary myopathies can involve sarcomeric proteins, but the overall clinical picture strongly points to a dystrophinopathy.
*Peripheral nerve demyelination*
* **Peripheral nerve demyelination** is characteristic of conditions like **Charcot-Marie-Tooth disease** (CMT), which affects peripheral nerves and causes distal muscle weakness and atrophy, foot deformities (e.g., pes cavus), and sensory loss.
* While CMT can cause toe walking, it typically involves significant distal muscle wasting rather than calf pseudohypertrophy, and the cardiac involvement (1st-degree AV block) is less commonly a prominent feature compared to muscular dystrophies.
Muscular dystrophies US Medical PG Question 10: A 4-year-old male child presents with muscle weakness. His mother tells that her child has difficulty in climbing stairs and getting up from the floor. On muscle biopsy, small muscle fibrils and absence of dystrophin was found. What is the diagnosis out of given options?
- A. Limb-girdle muscular dystrophy
- B. Becker muscular dystrophy
- C. Myotonic dystrophy
- D. Duchenne muscular dystrophy (Correct Answer)
- E. Emery-Dreifuss muscular dystrophy
Muscular dystrophies Explanation: ***Duchenne muscular dystrophy***
- The presentation of **muscle weakness** and difficulty climbing stairs (**Gowers' sign**) in a 4-year-old male is classic for **Duchenne muscular dystrophy (DMD)**.
- The finding of **absent dystrophin** on muscle biopsy is the definitive diagnostic hallmark of DMD, caused by mutations in the **DMD gene**.
*Limb-girdle muscular dystrophy*
- This group of disorders affects **proximal muscles** but typically has a more variable age of onset and progression, and **dystrophin** is usually present, though other muscle proteins may be deficient.
- The molecular defect is diverse, not specifically an **absence of dystrophin**.
*Becker muscular dystrophy*
- Similar to Duchenne, but is a milder form with **reduced, not absent, dystrophin** expression, leading to a later onset and slower progression of muscle weakness.
- While it also affects the **DMD gene**, the presence of some functional dystrophin differentiates it from the severe presentation of DMD.
*Myotonic dystrophy*
- This condition is characterized by **myotonia** (delayed muscle relaxation) and affects multiple systems, including the eyes, heart, and endocrine system, which are not mentioned in this presentation.
- It is caused by CTG trinucleotide repeat expansion in the **DMPK gene**, not by dystrophin deficiency.
*Emery-Dreifuss muscular dystrophy*
- This disorder presents with a characteristic triad of **early contractures** (especially elbow, ankle, and neck), **slowly progressive muscle weakness**, and **cardiac conduction defects**.
- The early age of onset with isolated proximal weakness and **absent dystrophin** on biopsy are not consistent with this diagnosis, which typically involves emerin or lamin A/C protein defects.
More Muscular dystrophies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.