Genetic testing approaches US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Genetic testing approaches. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Genetic testing approaches US Medical PG Question 1: A 39-year-old pregnant woman at 16 weeks gestation recently underwent a quad-screen which revealed elevated beta-hCG, elevated inhibin A, decreased alpha-fetoprotein, and decreased estradiol. An ultrasound was performed which found increased nuchal translucency. Which of the following is recommended for diagnosis?
- A. Biopsy and pathologic examination of fetus
- B. Confirmatory amniocentesis and chromosomal analysis of the fetal cells (Correct Answer)
- C. Fetus is normal, continue with pregnancy as expected
- D. Maternal karyotype
- E. Cell-free fetal DNA analysis
Genetic testing approaches Explanation: ***Confirmatory amniocentesis and chromosomal analysis of the fetal cells***
- The combination of **quad-screen results** (elevated 𝛽-hCG, elevated inhibin A, decreased AFP, decreased estradiol) and **increased nuchal translucency** strongly suggests an aneuploidy, particularly **Down Syndrome (Trisomy 21)**.
- **Amniocentesis** is a **diagnostic procedure** that provides fetal cells for definitive chromosomal analysis (karyotyping), confirming or ruling out aneuploidy with high accuracy.
*Biopsy and pathologic examination of fetus*
- A **fetal biopsy** is generally not a standard diagnostic test for aneuploidy and carries higher risks than amniocentesis or chorionic villus sampling (CVS).
- This procedure would typically be considered for specific fetal anomalies requiring tissue diagnosis, not for confirming chromosomal disorders.
*Fetus is normal, continue with pregnancy as expected*
- The abnormal **quad-screen results** and **increased nuchal translucency** are significant indicators of potential chromosomal abnormalities, making it unlikely that the fetus is normal.
- Ignoring these findings could lead to the birth of a child with an undiagnosed genetic condition.
*Maternal karyotype*
- A **maternal karyotype** evaluates the mother's chromosomes to identify balanced translocations or other inherited chromosomal abnormalities that could increase the risk in offspring.
- While helpful for identifying a parental genetic cause, it does not directly diagnose the fetal condition; a fetal sample is still needed for that.
*Cell-free fetal DNA analysis*
- **Cell-free fetal DNA (cfDNA) analysis** is a **screening test** with high sensitivity and specificity for common aneuploidies, but it is not a diagnostic test.
- While it can guide further investigation, a positive cfDNA result still requires a **confirmatory diagnostic procedure** like amniocentesis or CVS before making definitive clinical decisions.
Genetic testing approaches US Medical PG Question 2: A 16-year-old presents to the primary care physician because he has noticed an increase in the size of his breast tissue over the past 3 years. He states that he is significantly taller than his entire class at school although he feels increasingly weak and uncoordinated. He performs at the bottom of his grade level academically. On physical exam the patient has marked gynecomastia with small firm testes. The physician decides to perform a karyotype on the patient. What is the most likely outcome of this test?
- A. 47, XYY
- B. 45, XO
- C. 47, XXY (Correct Answer)
- D. 47, XXX
- E. 46, XY
Genetic testing approaches Explanation: ***47, XXY***
The constellation of **gynecomastia, tall stature, learning difficulties, and small testes** is classic for **Klinefelter syndrome**, which is characterized by a **47, XXY** karyotype.
The presence of an extra X chromosome leads to **hypogonadism** and **endocrine imbalances**, explaining the physical and developmental findings.
*47, XYY*
- Individuals with **47, XYY syndrome** are typically tall but do not usually present with breast enlargement or other features of hypogonadism.
- They may have an increased risk of learning difficulties and behavioral problems.
*45, XO*
- This karyotype, also known as **Turner syndrome**, is characterized by the absence of an X chromosome and typically affects **females**.
- Common features include **short stature, webbed neck, and ovarian dysfunction**, which are inconsistent with the patient's presentation.
*47, XXX*
- This karyotype, known as **Triple X syndrome**, affects **females** and is characterized by the presence of an extra X chromosome.
- While some individuals may experience learning difficulties or developmental delays, it does not cause gynecomastia or small testes in males.
*46, XY*
- This is the **normal male karyotype** and would not explain the patient's symptoms of gynecomastia, small testes, tall stature, or learning difficulties.
- These symptoms suggest an underlying chromosomal abnormality.
Genetic testing approaches US Medical PG Question 3: A 16-year-old girl presents with primary amenorrhea. On exam, you note that she is short and has a shield chest. You order abdominal imaging, which suggests the presence of streak gonads.
Of the choices listed below, which of the following karyotypes is possible in this patient?
I: 45,XO
II: 45,XO/46,XX mosaicism
III: 46,X,del(Xp) or other structural X abnormalities
- A. I and III
- B. I, II, and III (Correct Answer)
- C. II and III
- D. I and II
- E. I only
Genetic testing approaches Explanation: ***I, II, and III***
- The patient's presentation with **primary amenorrhea**, **short stature**, a **shield chest**, and **streak gonads** is classic for **Turner syndrome**.
- All three listed karyotypes (I: **45,XO**, II: **45,XO/46,XX mosaicism**, and III: **46,X,del(Xp)** or other structural X abnormalities) are recognized variants that cause Turner syndrome.
*I and III*
- This option incorrectly excludes 45,XO/46,XX mosaicism, which is a common and clinically significant **karyotype in Turner syndrome**.
- Mosaicism can lead to a milder phenotype but still presents with the characteristic features described.
*II and III*
- This option incorrectly excludes **45,XO**, which is the most classic and common karyotype found in individuals with Turner syndrome.
- The absence of a second X chromosome is the hallmark genetic defect.
*I and II*
- This option incorrectly excludes **structural X abnormalities** (e.g., deletion of the short arm of the X chromosome, **46,X,del(Xp)**), which are known causes of Turner syndrome.
- These structural changes lead to a similar clinical picture due to the loss of critical genes on the X chromosome.
*I only*
- While **45,XO** is the most common karyotype in Turner syndrome, confining the possibility to only this option is too restrictive.
- Both mosaicism and structural X abnormalities also result in the clinical features of Turner syndrome.
Genetic testing approaches US Medical PG Question 4: A 34-year-old gravida 2 para 1 woman at 16 weeks gestation presents for prenatal care. Her prenatal course has been uncomplicated. She takes no medications besides her prenatal vitamin which she takes every day, and she has been compliant with routine prenatal care. She has a 7-year-old daughter who is healthy. The results of her recent quadruple screen are listed below:
AFP: Low
hCG: Low
Estriol: Low
Inhibin-A: Normal
Which of the following is the most appropriate next step to confirm the diagnosis?
- A. Chorionic villus sampling
- B. Amniocentesis (Correct Answer)
- C. Ultrasound for nuchal translucency
- D. Folic acid supplementation
- E. Return to clinic in 4 weeks
Genetic testing approaches Explanation: ***Amniocentesis***
- The presented quad screen results (low AFP, low hCG, low estriol, normal Inhibin-A) are highly suggestive of **trisomy 18 (Edwards syndrome)**. Amniocentesis is a **definitive diagnostic test** that can confirm aneuploidy by providing a fetal karyotype.
- While typically performed between **15 and 20 weeks gestation**, it can differentiate between trisomy 18 and trisomy 21 (Down syndrome), which usually presents with high hCG and high Inhibin-A.
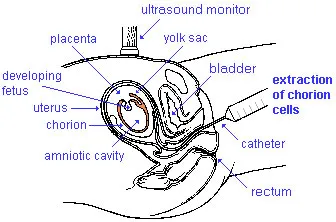
*Chorionic villus sampling (CVS)*
- **CVS** is typically performed earlier in pregnancy, between **10 and 13 weeks gestation**, meaning it is too late to perform at 16 weeks gestation.
- While it can provide a fetal karyotype for genetic diagnosis, the gestational age presented in the vignette makes this option currently inappropriate.
*Ultrasound for nuchal translucency*
- **Nuchal translucency (NT)** is part of the first-trimester screening, usually measured between **11 and 14 weeks gestation**.
- At 16 weeks gestation, measuring NT would be **outside the appropriate timeframe**, and the second-trimester quad screen has already been completed, making further screening rather than diagnosis less useful.
*Folic acid supplementation*
- **Folic acid supplementation** is crucial before and during early pregnancy to prevent neural tube defects, which would be associated with high AFP.
- The patient is already taking prenatal vitamins (which contain folic acid), and her quad screen results are not indicative of a neural tube defect but rather a chromosomal abnormality.
*Return to clinic in 4 weeks*
- The abnormal quad screen results indicate a **high risk for aneuploidy**, specifically trisomy 18, which requires immediate follow-up and definitive diagnosis.
- Delaying further assessment for 4 weeks would be clinically inappropriate and could increase patient anxiety and potentially reduce options for further management.
Genetic testing approaches US Medical PG Question 5: A 5-year-old patient presents to the pediatrician's office with fatigue and swollen lymph nodes. Extensive work-up reveals a diagnosis of acute lymphoblastic leukemia. In an effort to better tailor the patient's treatments, thousands of genes are arranged on a chip and a probe is made from the patient's mRNA (converted to cDNA). This probe is then hybridized to the chip in order to measure the gene expression of thousands of genes. The technology used to investigate this patient's gene expression profile is best for detecting which of the following types of genetic abnormalities?
- A. Trisomies
- B. Large scale chromosomal deletions
- C. Frame-shift mutations
- D. Chromosomal translocations (Correct Answer)
- E. Single nucleotide polymorphisms
Genetic testing approaches Explanation: ***Chromosomal translocations***
- The described process, involving gene expression analysis using a **DNA chip** (microarray), is effective at identifying translocations indirectly by detecting abnormal **fusion transcripts** or altered **gene expression patterns** resulting from the translocation.
- Many leukemias, especially **acute lymphoblastic leukemia (ALL)**, are characterized by specific chromosomal translocations that lead to the creation of **oncogenic fusion genes**, thereby altering gene expression.
*Trisomies*
- Trisomies are **numerical chromosomal abnormalities** involving an extra copy of an entire chromosome, which are typically detected by **karyotyping** or **fluorescence in situ hybridization (FISH)**, not by gene expression arrays directly unless they cause a widespread, quantifiable change in dosage.
- While gene expression might be altered, a microarray designed for gene expression profiling is not the primary or most sensitive tool for identifying the presence of an entire extra chromosome.
*Large scale chromosomal deletions*
- Large-scale deletions would lead to a **reduced expression** of a large number of genes in the affected region, but direct detection of the deletion itself is usually done with **comparative genomic hybridization (CGH)** or **karyotyping**, which are designed to identify copy number variations.
- While gene chips can show altered expression, they are less precise for delineating the exact boundaries of a deletion compared to genetic-level analyses.
*Frame-shift mutations*
- **Frame-shift mutations** are small insertions or deletions within a gene that alter the reading frame, leading to a truncated or non-functional protein.
- These are typically detected by **DNA sequencing**, not broadly by gene expression microarrays, which measure the abundance of mRNA transcripts rather than sequence changes.
*Single nucleotide polymorphisms*
- **Single nucleotide polymorphisms (SNPs)** are variations in a single nucleotide at a specific position in the genome.
- While specialized SNP arrays exist, general gene expression microarrays are designed to quantify mRNA levels and are not the primary method for identifying individual SNPs, which require **genotyping** techniques.
Genetic testing approaches US Medical PG Question 6: An investigator studying viral mutation isolates a virus strain from the gastric contents of an infant with gastroenteritis. This virus has a nonenveloped RNA genome with 11 segments and an icosahedral symmetrical capsid. The investigator finds that if 2 strains of this virus coinfect a single host cell, some of the resulting viral progeny have genome segments derived from both parental viruses. The observed phenomenon is most likely also seen in which of the following viral families?
- A. Caliciviruses
- B. Orthomyxoviruses (Correct Answer)
- C. Flaviviruses
- D. Retroviruses
- E. Picornaviruses
Genetic testing approaches Explanation: ***Orthomyxoviruses***
- The description of a virus with a **segmented RNA genome** undergoing reassortment (mixing segments from coinfecting strains) is characteristic of **Orthomyxoviruses**, which notably include the influenza virus.
- Influenza virus is well-known for its ability to **reassort** its **8 segmented RNA genome**, leading to antigenic shifts responsible for pandemics.
*Caliciviruses*
- **Caliciviruses** (e.g., Norovirus) have a **single-stranded, non-segmented RNA genome** and do not undergo genomic reassortment.
- They are a common cause of **gastroenteritis** but their genetic features differ.
*Flaviviruses*
- **Flaviviruses** (e.g., Dengue, Yellow Fever, Zika) possess a **single-stranded, non-segmented RNA genome**.
- They replicate via a polyprotein cleavage mechanism and do not exhibit genomic reassortment.
*Retroviruses*
- **Retroviruses** (e.g., HIV) have a **diploid, positive-sense, single-stranded RNA genome** that is reverse transcribed into DNA.
- While they can undergo **recombination** during reverse transcription, this is distinct from the described reassortment of segmented genomes.
*Picornaviruses*
- **Picornaviruses** (e.g., Poliovirus, Rhinovirus) have a **single-stranded, non-segmented RNA genome**.
- They are known for their rapid replication but do not exhibit genomic segmentation or reassortment.
Genetic testing approaches US Medical PG Question 7: A 12-year-old girl with a recently diagnosed seizure disorder is brought to the physician by her mother for genetic counseling. She has difficulties in school due to a learning disability. Medications include carbamazepine. She is at the 95th percentile for height. Genetic analysis shows a 47, XXX karyotype. An error in which of the following stages of cell division is most likely responsible for this genetic abnormality?
- A. Paternal meiosis, anaphase I
- B. Maternal meiosis, telophase II
- C. Maternal meiosis, metaphase II
- D. Paternal meiosis, metaphase II
- E. Maternal meiosis, anaphase II (Correct Answer)
Genetic testing approaches Explanation: ***Maternal meiosis, anaphase II***
- A 47,XXX karyotype indicates an extra X chromosome, which most commonly results from **nondisjunction during maternal meiosis**.
- **Nondisjunction in anaphase II** occurs when sister chromatids fail to separate properly, leading to an ovum containing two X chromosomes, which upon fertilization by an X-bearing sperm results in an XXX zygote.
- While nondisjunction can occur in either meiosis I or II, both produce the same 47,XXX outcome; anaphase is the critical stage where chromosome separation occurs.
*Paternal meiosis, anaphase I*
- Nondisjunction during paternal meiosis I would lead to sperm with either no sex chromosomes or both X and Y chromosomes, resulting in **45,X0 (Turner syndrome) or 47,XXY (Klinefelter syndrome)** upon fertilization, not 47,XXX.
- This involves improper segregation of **homologous chromosomes**.
*Maternal meiosis, telophase II*
- While telophase II is the final stage of meiosis II, the critical event of nondisjunction (failure of sister chromatids to separate) occurs during **anaphase II**, not telophase.
- Errors in telophase II would affect nuclear reformation but do not cause the chromosomal separation failure responsible for **aneuploidy**.
*Maternal meiosis, metaphase II*
- Metaphase II is when sister chromatids align at the metaphase plate; while improper alignment could theoretically contribute to aneuploidy, the actual **physical separation failure** defining nondisjunction occurs during **anaphase II**.
- Nondisjunction is specifically an anaphase phenomenon.
*Paternal meiosis, metaphase II*
- Paternal meiosis II nondisjunction would result in sperm carrying either two sex chromosomes (XX or YY) or none, leading to karyotypes like **47,XYY or 47,XXY**, not 47,XXX.
- Paternal contribution of two X chromosomes would require the rare scenario of an X-bearing sperm with nondisjunction fertilizing an X-bearing ovum that also had nondisjunction, which is extremely unlikely.
Genetic testing approaches US Medical PG Question 8: A homeless 45-year-old man presents to the emergency room in December complaining of malaise, body aches, chills, and fever. He reports that his symptoms started 4 days ago. His myalgias and chills have begun to resolve, but now he is starting to develop a dry cough, dyspnea, and a sore throat. He does not have a primary care provider and has not had any vaccinations in over 2 decades. He receives medical care from the emergency room whenever he is feeling ill. His temperature is 103°F (39.4°C), blood pressure is 130/70 mmHg, pulse is 115/min, and respirations are 22/min. On exam, he appears fatigued with mildly increased work of breathing. A chest radiograph is negative. A nasopharyngeal viral culture is positive for an orthomyxovirus. Upon further review of the patient’s medical record, he was diagnosed with the same condition 1 year ago in November. Which of the following mechanisms is responsible for pandemics of this patient’s disease?
- A. Reassortment (Correct Answer)
- B. Complementation
- C. Transduction
- D. Phenotypic mixing
- E. Recombination
Genetic testing approaches Explanation: ***Reassortment***
- This patient presents with **influenza**, confirmed by a positive nasopharyngeal viral culture for an **orthomyxovirus**. The seasonal nature of his illness, despite having it before, points to antigenic changes.
- **Reassortment** (also known as **antigenic shift**) is the primary mechanism responsible for **influenza pandemics**. It involves the exchange of entire gene segments between different influenza strains (e.g., human and avian or swine strains) when a host cell is co-infected with two distinct viral strains, leading to a new subtype with novel hemagglutinin (HA) or neuraminidase (NA) proteins that human populations have little to no immunity against.
*Complementation*
- **Complementation** occurs when two viruses infect the same cell, and one virus provides a **necessary gene product** that the other mutated or defective virus lacks, allowing the latter to replicate.
- This mechanism does not involve genetic exchange leading to new viral subtypes and is therefore not responsible for the emergence of pandemic strains.
*Transduction*
- **Transduction** is a process by which **bacteriophages** (viruses that infect bacteria) transfer bacterial DNA from one bacterium to another.
- This is a mechanism of gene transfer in bacteria and is not relevant to the genetic changes in influenza viruses.
*Phenotypic mixing*
- **Phenotypic mixing** occurs when the genome of one virus is packaged into the **capsid** of another virus, or when genetic material from two viruses is packaged into a mixed capsid.
- While it can alter the tropism or antigenicity of progeny viruses temporarily, it does not involve a change in the viral genome itself and is therefore not responsible for permanent shifts leading to pandemics.
*Recombination*
- **Recombination** involves the exchange of genetic material between two homologous DNA or RNA molecules, leading to new combinations of genes within the same gene segment.
- While recombination can occur in viruses, **reassortment** of entire gene segments (antigenic shift) is the specific and most significant mechanism for creating novel influenza strains capable of causing pandemics, rather than recombination within gene segments.
Genetic testing approaches US Medical PG Question 9: An investigator is studying the function of the endoplasmic reticulum in genetically modified lymphocytes. A gene is removed that facilitates the binding of ribosomes to the endoplasmic reticulum. Which of the following processes is most likely to be impaired as a result of this genetic modification?
- A. Production of secretory proteins (Correct Answer)
- B. Neutralization of toxins
- C. Ubiquitination of proteins
- D. α-Oxidation of fatty acids
- E. Synthesis of ketone bodies
Genetic testing approaches Explanation: ***Production of secretory proteins***
- Ribosomes bound to the **rough endoplasmic reticulum (RER)** are responsible for synthesizing proteins destined for secretion, insertion into membranes, or delivery to organelles like lysosomes.
- If ribosomes cannot bind to the ER, these proteins will be synthesized in the **cytosol** and lack the proper signals and processing for their intended destination and function.
*Neutralization of toxins*
- The **smooth endoplasmic reticulum (SER)**, not the RER, is primarily involved in **detoxification** processes, particularly drug metabolism and neutralization of toxins.
- This function relies on enzymes embedded within the SER membrane and is largely independent of ribosome binding.
*Ubiquitination of proteins*
- **Ubiquitination** is a post-translational modification that tags proteins for degradation by the **proteasome** or for trafficking to specific cellular compartments.
- This process occurs primarily in the **cytosol** and does not directly rely on ribosome binding to the ER for protein synthesis.
*α-Oxidation of fatty acids*
- **α-oxidation of fatty acids** is a metabolic pathway that occurs primarily in the **peroxisomes**.
- It is distinct from protein synthesis on the ER and would not be directly impacted by the inability of ribosomes to bind to the ER.
*Synthesis of ketone bodies*
- The **synthesis of ketone bodies** (ketogenesis) primarily occurs in the **mitochondria** of liver cells.
- This metabolic pathway is not directly dependent on ribosome binding to the endoplasmic reticulum for its function.
Genetic testing approaches US Medical PG Question 10: A 41-year-old woman is referred by her radiation oncologist to the medical genetics clinic. She was recently diagnosed with an infiltrating ductal carcinoma of the breast. She has a previous history of colonic polyps for which she undergoes bi-annual colonoscopy. The maternal and paternal family history is unremarkable for polyps and malignant or benign tumors. However, the patient reports that her 10-year-old son has dark brown pigmentation on his lips, and she also had similar pigmentation as a child. Histology of colonic polyps in this patient will most likely reveal which of the following?
- A. Adenomatous polyps
- B. Inflammatory polyps
- C. Retention polyps
- D. Hyperplastic polyps
- E. Hamartomatous polyps (Correct Answer)
Genetic testing approaches Explanation: ***Hamartomatous polyps***
- The constellation of **breast carcinoma**, a history of **colonic polyps**, and **mucocutaneous pigmentation** (dark brown pigmentation on lips in the patient and her son) is highly suggestive of **Peutz-Jeghers Syndrome**.
- **Peutz-Jeghers Syndrome** is an autosomal dominant disorder characterized by the development of **hamartomatous polyps** in the gastrointestinal tract and an increased risk of various cancers, including breast and colorectal cancer.
*Adenomatous polyps*
- While adenomatous polyps are common and can be a precursor to colorectal cancer, the presence of associated **mucocutaneous pigmentation** points away from typical adenomatous familial or sporadic polyposis syndromes (e.g., FAP).
- These polyps are characteristic of **Familial Adenomatous Polyposis (FAP)** or sporadic colorectal cancer, but FAP usually presents with hundreds to thousands of polyps and does not typically involve mucocutaneous pigmentation.
*Inflammatory polyps*
- **Inflammatory polyps** are typically a reactive process secondary to chronic inflammation, such as in inflammatory bowel disease (Crohn's disease or ulcerative colitis), and are not associated with specific hereditary syndromes like Peutz-Jeghers or mucocutaneous pigmentation.
- They do not carry the same increased risk of malignancy as hamartomatous or adenomatous polyps in the context of a syndrome.
*Retention polyps*
- **Retention polyps**, also known as juvenile polyps, are usually found in children and are typically benign; however, they can occur sporadically in adults.
- They are generally solitary or few in number and are not associated with the distinct syndromic features of mucocutaneous pigmentation or the wide range of cancer risks seen in Peutz-Jeghers syndrome.
*Hyperplastic polyps*
- **Hyperplastic polyps** are generally considered benign and do not typically lead to cancer, although some serrated hyperplastic polyps can have malignant potential.
- They are not associated with hereditary syndromes presenting with cutaneous pigmentation and multiple extracolic malignancies.
More Genetic testing approaches US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.