Cystic fibrosis US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Cystic fibrosis. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Cystic fibrosis US Medical PG Question 1: A 2720-g (6-lb) female newborn delivered at 35 weeks’ gestation starts vomiting and becomes inconsolable 48 hours after birth. The newborn has not passed her first stool yet. Examination shows abdominal distention and high-pitched bowel sounds. A water-soluble contrast enema study shows microcolon. Serum studies show increased levels of immunoreactive trypsinogen. Which of the following is the most likely additional laboratory finding?
- A. Increased sodium concentration in sweat (Correct Answer)
- B. Decreased hydrogen ion concentration in renal collecting duct
- C. Increased chloride concentration in alveolar fluid
- D. Increased bicarbonate concentration in pancreatic secretions
- E. Increased serum calcium concentration
Cystic fibrosis Explanation: ***Increased sodium concentration in sweat***
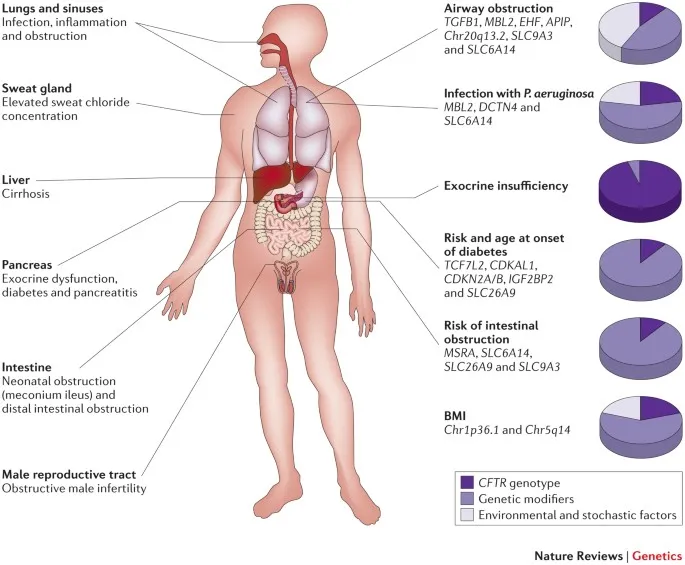
- The clinical picture of **abdominal distention**, **vomiting**, failure to pass meconium, and **microcolon** in a preterm infant, combined with **elevated immunoreactive trypsinogen (IRT)**, is highly suggestive of **cystic fibrosis with meconium ileus**.
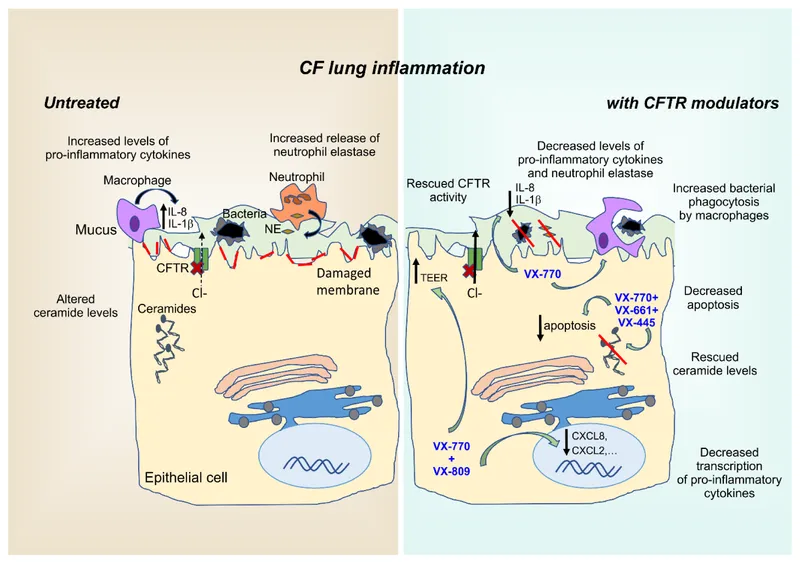
- In cystic fibrosis, the dysfunctional **cystic fibrosis transmembrane conductance regulator (CFTR) protein** impairs **chloride and sodium reabsorption** in sweat ducts, leading to **increased sodium and chloride concentration in sweat**.
- The **sweat chloride test** (which also measures sodium) is the **gold standard diagnostic test** for cystic fibrosis and is the most likely additional laboratory finding.
*Decreased hydrogen ion concentration in renal collecting duct*
- This finding is characteristic of **metabolic alkalosis** or certain forms of **renal tubular acidosis** where there is an inability to excrete hydrogen ions, which is not directly related to the pathophysiology of cystic fibrosis.
- While electrolyte imbalances can occur in cystic fibrosis due to gastrointestinal losses, this specific renal finding is not a primary or direct diagnostic feature.
*Increased chloride concentration in alveolar fluid*
- While it is true that cystic fibrosis causes **increased chloride concentration in airway surface liquid** due to defective CFTR, this is **not a routinely measurable laboratory test** used for diagnosis.
- The airway chloride concentration is a **local pathophysiologic finding** at the tissue level, not a practical diagnostic laboratory test.
- The question asks for an "additional **laboratory finding**," and the sweat chloride/sodium test is the standard diagnostic laboratory test, not measurement of alveolar fluid chloride.
*Increased bicarbonate concentration in pancreatic secretions*
- Patients with cystic fibrosis typically have **decreased bicarbonate secretion** in pancreatic secretions due to the dysfunctional CFTR channel, leading to acidic pancreatic fluid and precipitation of proteins, causing duct obstruction.
- This leads to **pancreatic insufficiency**, not increased bicarbonate concentration.
*Increased serum calcium concentration*
- **Hypercalcemia** is not a characteristic finding in cystic fibrosis; rather, patients with cystic fibrosis may be at risk for **osteopenia** or **osteoporosis** due to malabsorption of fat-soluble vitamins (including vitamin D) and chronic inflammation, potentially leading to **decreased serum calcium** in severe cases.
- This finding would suggest other conditions like hyperparathyroidism or malignancy.
Cystic fibrosis US Medical PG Question 2: A 14-year-old boy is brought to the physician by his parents for a follow-up examination. Since early childhood, he has had recurrent respiratory infections that cause him to miss several weeks of school each year. Last month, he had received treatment for his seventh episode of sinusitis this year. He has always had bulky, foul-smelling, oily stools that are now increasing in frequency. His parents are concerned that he is too thin and not gaining weight appropriately. He has a good appetite and eats a variety of foods. He is in the 10th percentile for height and the 5th percentile for weight. Examination of the nasal cavity shows multiple nasal polyps. The lung fields are clear upon auscultation. Further evaluation is most likely to show which of the following?
- A. Positive methacholine challenge test
- B. Hypersensitivity to aspirin
- C. Selective IgA deficiency
- D. Anti-tissue transglutaminase antibodies
- E. Absent vas deferens (Correct Answer)
Cystic fibrosis Explanation: ***Absent vas deferens***
- This symptom is highly suggestive of **cystic fibrosis (CF)**, as over 95% of males with CF have **congenital bilateral absence of the vas deferens (CBAVD)**, leading to infertility.
- The patient's history of **recurrent respiratory infections** (sinusitis), **nasal polyps**, **malabsorption** (bulky, foul-smelling, oily stools), and **failure to thrive** (low height and weight percentiles) are all classic features of CF.
*Positive methacholine challenge test*
- A positive methacholine challenge test indicates **bronchial hyperreactivity**, often seen in **asthma**. While some patients with cystic fibrosis may develop asthma-like symptoms, this is not the most definitive or specific finding for CF.
- While patients with CF do experience chronic lung disease, conditions like **bronchiectasis** and recurrent infections are more characteristic than isolated bronchial hyperreactivity to methacholine.
*Hypersensitivity to aspirin*
- **Aspirin-exacerbated respiratory disease (AERD)** involves a triad of asthma, recurrent rhinosinusitis with nasal polyposis, and aspirin sensitivity. While nasal polyps and recurrent sinusitis are present, the absence of asthma and the strong evidence for malabsorption point away from AERD.
- AERD is typically triggered by **NSAIDs** and causes acute respiratory symptoms, which is not the primary concern or most likely defining characteristic in this patient's presentation.
*Selective IgA deficiency*
- **Selective IgA deficiency** is characterized by recurrent infections, particularly in the respiratory and gastrointestinal tracts. However, it does not typically cause the severe malabsorption with **fatty stools (steatorrhea)** or **nasal polyps** seen in this patient.
- Although it leads to recurrent infections, the pattern of symptoms including specific GI and respiratory involvement (sinusitis, nasal polyps, malabsorption) does not fit selective IgA deficiency as well as it fits CF.
*Anti-tissue transglutaminase antibodies*
- These antibodies are a hallmark of **celiac disease**, which presents with malabsorption and failure to thrive. However, celiac disease does not explain the **recurrent respiratory infections** and **nasal polyps** present in this case.
- While celiac disease can cause gastrointestinal symptoms similar to CF, the presence of severe respiratory issues makes celiac disease a less likely primary diagnosis.
Cystic fibrosis US Medical PG Question 3: A 7-year-old girl is brought by her parents to her pediatrician's office for a persistent cough observed over the past month. She was diagnosed with cystic fibrosis 2 years ago and has been receiving chest physiotherapy regularly and the flu vaccine yearly. Her parents tell the pediatrician that their daughter has been coughing day and night for the past month, and produces thick, purulent, foul-smelling sputum. They are concerned because this is the first time such an episode has occurred. She has not had a fever, chills or any other flu-like symptoms. On examination, her blood pressure is 100/60 mm Hg, the pulse is 82/min, and the respiratory rate is 16/min. Breath sounds are reduced over the lower lung fields along with a presence of expiratory wheezing. Her sputum culture comes back positive for an aerobic, non-lactose fermenting, oxidase-positive, gram-negative bacillus. Which of the following prophylactic regimes should be considered after treating this patient for her current symptoms?
- A. Oral trimethoprim-sulfamethoxazole
- B. Oral amoxicillin/clavulanic acid
- C. Oral ciprofloxacin
- D. Inhaled levofloxacin
- E. Inhaled tobramycin (Correct Answer)
Cystic fibrosis Explanation: ***Inhaled tobramycin***
- The patient's symptoms (persistent cough, purulent sputum, reduced breath sounds, expiratory wheezing) coupled with a positive culture for an **aerobic, non-lactose fermenting, oxidase-positive, gram-negative bacillus** in a patient with cystic fibrosis (CF) strongly suggest a *Pseudomonas aeruginosa* infection.
- **Inhaled tobramycin** is a recommended prophylactic regimen for CF patients with chronic *Pseudomonas aeruginosa* colonization to reduce exacerbations and preserve lung function after initial eradication therapy.
*Oral trimethoprim-sulfamethoxazole*
- This antibiotic is primarily used for infections caused by *Staphylococcus aureus*, *Haemophilus influenzae*, and *Pneumocystis jirovecii*, but not typically for *Pseudomonas aeruginosa* in CF.
- While it has some activity against certain gram-negative bacteria, it is not the preferred prophylactic agent for *Pseudomonas* in CF due to resistance patterns and lack of efficacy compared to antipseudomonal agents.
*Oral amoxicillin/clavulanic acid*
- This combination antibiotic is effective against a broad spectrum of bacteria, including *Haemophilus influenzae* and *Moraxella catarrhalis*, but it does not have reliable activity against *Pseudomonas aeruginosa*.
- It is not indicated for prophylactic use against *Pseudomonas* in CF patients.
*Oral ciprofloxacin*
- While oral ciprofloxacin is active against *Pseudomonas aeruginosa* and is sometimes used for acute exacerbations, chronic daily oral quinolone use is generally avoided for prophylaxis due to concerns about resistance development and significant side effects.
- **Inhaled antibiotics** are preferred for chronic suppression in CF as they deliver high concentrations directly to the lungs, minimizing systemic side effects.
*Inhaled levofloxacin*
- Similar to other quinolones, inhaled levofloxacin can be used for *Pseudomonas* infections in CF. However, given the options, **inhaled tobramycin** has a more established and broader role as a first-line inhaled prophylactic option for *Pseudomonas* in CF.
- Resistance patterns and individual patient response would guide the choice between different inhaled antibiotics, but tobramycin is a classic prophylactic agent in this setting.
Cystic fibrosis US Medical PG Question 4: A 34-year-old woman comes to the fertility clinic with her husband for infertility treatment. The couple has been having unprotected intercourse for the past 2 years without any pregnancies. This is their first time seeking fertility treatment. The patient's past medical history includes asthma. She denies any menstrual irregularities, menstrual pain, abnormal bleeding or past sexually transmitted infections. The husband reports that "he would get sick easily and would always have some upper respiratory infections." Physical examination of the wife demonstrates nasal polyps bilaterally; vaginal examination is unremarkable. Physical examination of the husband is unremarkable. Semen analysis results are shown below:
Semen analysis:
Volume: 1.9 mL (Normal > 1.5 mL)
pH: 7.4 (Normal: > 7.2)
Sperm concentration: 0 million/mL (Normal: > 15 million/mL)
Total sperm count: 0 million/mL (Normal: > 39 million/mL)
Total motility: N/A (Normal: > 40%)
Morphology: N/A (Normal: > 4% normal forms)
What is the most likely explanation for this couple's infertility?
- A. XO chromosome in wife
- B. Undescended testes in husband
- C. XXY chromosome in husband
- D. Deletion of Phe508 in husband (Correct Answer)
- E. Deletion of Phe508 in wife
Cystic fibrosis Explanation: ***Deletion of Phe508 in husband***
- The husband's history of recurrent respiratory infections combined with **complete azoospermia** (zero sperm despite normal semen volume) is highly suggestive of **Cystic Fibrosis** due to **CFTR gene mutation**, with **deletion of Phe508 (ΔF508)** being the most common mutation.
- CFTR mutations frequently cause **congenital bilateral absence of the vas deferens (CBAVD)**, resulting in obstructive azoospermia where sperm are produced but cannot be ejaculated due to absent vas deferens.
- This provides a **unifying diagnosis** explaining both the male infertility and respiratory symptoms.
*XO chromosome in wife*
- **Turner syndrome (45,XO)** presents with **primary amenorrhea**, **streak gonads**, short stature, and absent secondary sexual characteristics.
- The wife has **normal menstrual history** and unremarkable fertility evaluation, making this diagnosis incompatible with her presentation.
- The semen analysis clearly identifies **male-factor infertility** as the cause.
*Undescended testes in husband*
- **Cryptorchidism** can impair spermatogenesis due to elevated testicular temperature, typically causing **oligospermia** (reduced sperm count) rather than complete azoospermia.
- Physical examination of the husband was unremarkable, making undescended testes unlikely.
- This diagnosis does not explain the recurrent respiratory infections.
*XXY chromosome in husband*
- **Klinefelter syndrome (47,XXY)** causes **primary hypogonadism** with azoospermia, small firm testes, gynecomastia, and often tall stature with eunuchoid proportions.
- While it explains the azoospermia, it **does not account for the recurrent respiratory infections**, whereas CFTR mutation explains both features.
- Physical exam was unremarkable, without typical Klinefelter stigmata.
*Deletion of Phe508 in wife*
- While the wife has asthma and nasal polyps (which can be seen in CF or overlap with asthma-related conditions), her **normal menstrual history** indicates she is likely fertile.
- The **male-factor infertility** (complete azoospermia in the husband) is the direct cause of the couple's inability to conceive.
- Even if the wife has CF, this would not explain the husband's azoospermia, which is the primary barrier to conception.
Cystic fibrosis US Medical PG Question 5: A 2-year-old boy is brought to the physician because of an increasing productive cough with a moderate amount of white phlegm for the past week. He has been treated for pneumonia with antibiotic therapy four times over the past year. A chest x-ray performed 3 months ago showed no anatomical abnormalities. He has had multiple episodes of bulky greasy stools that don't flush easily. He is at 3rd percentile for height and at 5th percentile for weight. His temperature is 38°C (100.4°F), pulse is 132/min, and respirations are 44/min. A few inspiratory crackles are heard in the thorax. The abdomen is soft and nontender. The remainder of the examination shows no abnormalities. Which of the following is the best initial test to determine the underlying etiology of this patient's illness?
- A. X-ray of the chest
- B. Genetic testing
- C. Serum immunoglobulin level
- D. Sweat chloride test (Correct Answer)
- E. Stool analysis
Cystic fibrosis Explanation: ***Sweat chloride test***
- The patient exhibits classic symptoms of **cystic fibrosis**, including recurrent respiratory infections, failure to thrive (low height and weight percentiles), and greasy, bulky stools suggestive of **pancreatic insufficiency**.
- A **sweat chloride test** measures the concentration of chloride in sweat and is the **most reliable initial screening test** for cystic fibrosis, given the characteristic clinical presentation.
*X-ray of the chest*
- While chest X-rays can show evidence of pulmonary involvement (e.g., **bronchiectasis**, hyperinflation), a previous X-ray showed no abnormalities, and it does not directly determine the **underlying etiology** of the multiple symptoms.
- It would be part of the respiratory assessment but is not the best initial test for diagnosing the systemic genetic disorder.
*Genetic testing*
- **Genetic testing** confirms the diagnosis of cystic fibrosis by identifying specific mutations in the **CFTR gene**.
- However, in a patient with a strong clinical suspicion, the **sweat chloride test** is typically performed first as a more accessible and cost-effective initial diagnostic test in many settings, with genetic testing used for confirmation or when sweat test results are equivocal.
*Serum immunoglobulin level*
- **Serum immunoglobulin levels** would assess for **immunodeficiency**, which can cause recurrent infections.
- While recurrent infections are present, the combination of **malabsorption** (greasy stools, failure to thrive) and respiratory symptoms points more strongly towards **cystic fibrosis** than a primary immunodeficiency.
*Stool analysis*
- **Stool analysis** can identify **malabsorption** (e.g., fecal fat content) or indicate **gastrointestinal infections**.
- While it could confirm pancreatic insufficiency, it does not directly diagnose the underlying cause of both respiratory and gastrointestinal symptoms as effectively as a sweat chloride test for cystic fibrosis.
Cystic fibrosis US Medical PG Question 6: An 11-month-old boy is brought to a pediatrician by his parents with a recurrent cough, which he has had since the age of 2 months. He has required 3 hospitalizations for severe wheezing episodes. His mother also mentions that he often has diarrhea. The boy’s detailed history reveals that he required hospitalization for meconium ileus during the neonatal period. Upon physical examination, his temperature is 37.0°C (98.6ºF), pulse rate is 104/min, respiratory rate is 40/min, and blood pressure is 55/33 mm Hg. An examination of the boy’s respiratory system reveals the presence of bilateral wheezing and scattered crepitations. An examination of his cardiovascular system does not reveal any abnormality. His length is 67.3 cm (26.5 in) and weight is 15 kg (33 lbs). His sweat chloride level is 74 mmol/L. His genetic evaluation confirms that he has an autosomal recessive disorder resulting in a dysfunctional membrane-bound protein. Which of the following best describes the mechanism associated with the most common mutation that causes this disorder?
- A. Decreased chloride transport through the protein
- B. Disordered regulation of the protein
- C. Decreased transcription of the protein due to splicing defect
- D. Complete absence of the protein
- E. Defective maturation and early degradation of the protein (Correct Answer)
Cystic fibrosis Explanation: ***Defective maturation and early degradation of the protein***
- The clinical picture (recurrent cough, wheezing, diarrhea, meconium ileus, elevated sweat chloride, autosomal recessive inheritance) strongly points to **cystic fibrosis (CF)**. The most common mutation in CF is **F508del**, which leads to misfolding of the **CFTR protein**, causing retention in the endoplasmic reticulum and subsequent degradation before reaching the cell membrane.
- This **defective processing and early degradation** result in a significant reduction or absence of functional CFTR protein at the cell surface, leading to impaired chloride transport.
*Decreased chloride transport through the protein*
- While **decreased chloride transport** is the ultimate functional consequence of cystic fibrosis, it is not the direct mechanism associated with the **F508del mutation's impact** on the CFTR protein itself.
- This option describes the **physiological result** of the protein defect, not the cellular/molecular mechanism of the most common mutation.
*Disordered regulation of the protein*
- **Disordered regulation** could be a potential mechanism for some CFTR mutations (Class IV mutations), affecting how the channel opens and closes or responds to signaling.
- However, for the **F508del mutation** (Class II mutation), the primary issue is the **lack of properly localized protein** due to misfolding and degradation, rather than a problem with the regulation or gating of the protein once it reaches the membrane.
*Decreased transcription of the protein due to splicing defect*
- **Decreased transcription** or **splicing defects** (Class I and V mutations) would result in reduced mRNA levels or incorrectly formed mRNA, leading to less protein synthesis.
- The **F508del mutation** involves a deletion of three nucleotides in exon 10, leading to a missing phenylalanine at position 508. Importantly, **transcription and splicing occur normally**; the mRNA is produced correctly. The problem arises at the **post-translational level** with protein folding, not at the transcriptional or splicing level.
*Complete absence of the protein*
- While functional CFTR protein is largely absent at the cell surface in F508del, the protein is **initially synthesized** in the endoplasmic reticulum.
- The problem is its **misfolding and rapid degradation**, preventing it from reaching the membrane, rather than a complete failure of protein synthesis from the outset (which would be seen in nonsense or frameshift mutations causing Class I defects).
Cystic fibrosis US Medical PG Question 7: A 1-year-old male with a history of recurrent pseudomonal respiratory infections and steatorrhea presents to the pediatrician for a sweat test. The results demonstrate a chloride concentration of 70 mEq/L (nl < 40 mEq/L). Which of the following defects has a similar AUTOSOMAL RECESSIVE mode of inheritance as the disorder experienced by this patient?
- A. Abnormal production of type IV collagen
- B. Trinucleotide repeat expansion of CAG on chromosome 4
- C. Mutated gene for mitochondrial-tRNA-Lys
- D. Accumulation of glycogen in the lysosome (Correct Answer)
- E. Inability to convert carbamoyl phosphate and ornithine into citrulline
Cystic fibrosis Explanation: ***Accumulation of glycogen in the lysosome***
- The patient's symptoms (recurrent **pseudomonal respiratory infections**, **steatorrhea**, and elevated sweat chloride) are classic for **cystic fibrosis (CF)**, an **autosomal recessive** disorder.
- Accumulation of glycogen in the lysosome describes **Pompe disease (Type II Glycogen Storage Disease)**, which is also an **autosomal recessive** disorder, making this the correct answer.
*Abnormal production of type IV collagen*
- This defect is characteristic of **Alport syndrome**, which is predominantly **X-linked dominant** (~80-85% of cases), though autosomal recessive forms exist.
- The question context and typical board exam framing classify this as X-linked, not autosomal recessive.
- Alport syndrome primarily affects the kidneys, ears, and eyes, and does not present with recurrent pseudomonal infections or steatorrhea.
*Trinucleotide repeat expansion of CAG on chromosome 4*
- This genetic defect is responsible for **Huntington's disease**, which is an **autosomal dominant** neurodegenerative disorder.
- Huntington's disease presents with chorea, cognitive decline, and psychiatric symptoms, which are distinct from CF.
*Mutated gene for mitochondrial-tRNA-Lys*
- A mutated gene for mitochondrial-tRNA-Lys is associated with **MELAS syndrome (Mitochondrial Encephalomyopathy, Lactic Acidosis, and Stroke-like episodes)**, which is inherited through **maternal (mitochondrial)** inheritance.
- This mode of inheritance is distinct from the autosomal recessive pattern seen in cystic fibrosis.
*Inability to convert carbamoyl phosphate and ornithine into citrulline*
- This describes a defect in **ornithine transcarbamylase (OTC) deficiency**, an **X-linked recessive** disorder, not autosomal recessive.
- OTC deficiency leads to hyperammonemia and metabolic disturbances, without the pulmonary and gastrointestinal symptoms typical of cystic fibrosis.
Cystic fibrosis US Medical PG Question 8: A 4-year-old girl is brought to the physician by her parents because she is severely underweight. She is easily fatigued and has difficulty keeping up with other children at her daycare. She has a good appetite and eats 3 full meals a day. She has 4 to 5 bowel movements daily with bulky, foul-smelling stools that float. She has had recurrent episodes of sinusitis since infancy. Her parents report that she recently started to snore during her sleep. She is at the 15th percentile for height and 3rd percentile for weight. Her vital signs are within normal limits. Examination shows pale conjunctivae. A few scattered expiratory crackles are heard in the thorax. There is abdominal distention. Which of the following is the most likely underlying cause of this patient's failure to thrive?
- A. T. whippelii infiltration of intestinal villi
- B. Impaired intestinal amino acid transport
- C. Exocrine pancreatic insufficiency (Correct Answer)
- D. Small intestine bacterial overgrowth
- E. Intestinal inflammatory reaction to gluten
Cystic fibrosis Explanation: ***Exocrine pancreatic insufficiency***
- The constellation of **failure to thrive**, **bulky, foul-smelling, floating stools** (suggesting **steatorrhea**), recurrent **sinusitis**, and **recurrent respiratory symptoms** (snoring, expiratory crackles) is highly indicative of **cystic fibrosis**, whose primary cause of malabsorption is **exocrine pancreatic insufficiency**.
- **Cystic fibrosis** leads to thick, viscous secretions that obstruct pancreatic ducts, preventing digestive enzymes from reaching the small intestine and causing **malabsorption of fats and fat-soluble vitamins**.
*T. whippelii infiltration of intestinal villi*
- This describes **Whipple's disease**, which typically affects **middle-aged men** and presents with malabsorption, arthralgia, and neurological symptoms.
- It is rare in children and usually presents with symptoms like diarrhea and weight loss, but not commonly with the **recurrent respiratory infections** and **pancreatic insufficiency** seen here.
*Impaired intestinal amino acid transport*
- This typically refers to conditions like **Hartnup disease**, which involves defective transport of neutral amino acids and can lead to **pellagra-like symptoms** (dermatitis, diarrhea, dementia) due to niacin deficiency.
- This condition does not explain the **steatorrhea**, **recurrent sinusitis**, or **respiratory symptoms** found in the patient.
*Small intestine bacterial overgrowth*
- While **SIBO** can cause malabsorption, **abdominal distention**, and loose stools, it does not typically cause **recurrent sinusitis** or the classic **bulky, foul-smelling, floating stools associated with pancreatic insufficiency**.
- SIBO is also not a primary cause of **failure to thrive** in a global sense, but rather a secondary complication.
*Intestinal inflammatory reaction to gluten*
- This describes **celiac disease**, which presents with **malabsorption**, **abdominal distention**, **failure to thrive**, and **anemia** (pale conjunctivae).
- However, celiac disease does not typically cause **recurrent sinusitis** or the **respiratory symptoms** (snoring, crackles) that are prominent in this patient's presentation.
Cystic fibrosis US Medical PG Question 9: A 10-year-old girl is admitted to the medical floor for a respiratory infection. The patient lives in a foster home and has been admitted many times. Since birth, the patient has had repeated episodes of pain/pressure over her frontal sinuses and a chronic cough that produces mucus. She was recently treated with amoxicillin for an infection. The patient is in the 25th percentile for height and weight which has been constant since birth. Her guardians state that the patient has normal bowel movements and has been gaining weight appropriately. The patient has a history of tricuspid stenosis. She also recently had magnetic resonance imaging (MRI) of her chest which demonstrated dilation of her airways. Her temperature is 99.5°F (37.5°C), blood pressure is 90/58 mmHg, pulse is 120/min, respirations are 18/min, and oxygen saturation is 94% on room air. Physical exam is notable for bruises along the patient's shins which the guardians state are from playing soccer. The rest of the exam is deferred because the patient starts crying. Which of the following findings is associated with this patient's most likely underlying diagnosis?
- A. Social withdrawal and avoidance of eye contact
- B. Hypocalcemia
- C. Repeat sinus infections secondary to seasonal allergies
- D. Diastolic murmur best heard along the right lower sternal border
- E. Increased chloride in the patient's sweat (Correct Answer)
Cystic fibrosis Explanation: ***Increased chloride in the patient's sweat***
- The patient's history of recurrent respiratory infections, chronic productive cough, frontal sinus pain, and **bronchiectasis** (dilated airways on MRI) are highly suggestive of **cystic fibrosis**.
- **Elevated sweat chloride** is the hallmark diagnostic test for cystic fibrosis, reflecting defective chloride transport in exocrine glands.
*Social withdrawal and avoidance of eye contact*
- These are features associated with **autism spectrum disorder**, which is unrelated to the patient's respiratory and sinus symptoms.
- While possible as a co-occurring condition, it is not directly linked to the most likely **underlying diagnosis** described.
*Hypocalcemia*
- **Hypocalcemia** is typically associated with conditions like **hypoparathyroidism** or severe **vitamin D deficiency**.
- It is not a characteristic feature or direct complication of cystic fibrosis.
*Repeat sinus infections secondary to seasonal allergies*
- While seasonal allergies can cause sinus issues, the patient's history of **chronic, productive cough**, and **bronchiectasis** points to a more severe underlying condition like cystic fibrosis, not just allergies.
- Cystic fibrosis patients often have chronic sinusitis due to thick, inspissated mucus, not primarily due to allergens.
*Diastolic murmur best heard along the right lower sternal border*
- A diastolic murmur at the right lower sternal border might suggest **aortic regurgitation** or a specific type of **pulmonary regurgitation**, but it is not characteristic of the patient's known tricuspid stenosis.
- The patient has **tricuspid stenosis**, which typically causes a mid-diastolic murmur best heard at the left lower sternal border, often increasing with inspiration. This finding is unrelated to cystic fibrosis.
Cystic fibrosis US Medical PG Question 10: A 2-year-old boy is brought to the physician because of a productive cough for 5 days. He has a history of recurrent lower respiratory tract infections and sinusitis treated with oral antibiotics. He frequently has loose stools that do not flush easily. He was born at 37 weeks' gestation and the neonatal period was complicated by meconium ileus. His immunizations are up-to-date. He is at the 15th percentile for height and at the 5th percentile for weight. His temperature is 37.1°C (98.8°F), pulse is 98/min, and respirations are 38/min. Pulse oximetry on room air shows an oxygen saturation of 95%. Examination shows bilateral nasal polyps. There are scattered inspiratory crackles heard in the thorax. Further evaluation of this patient is most likely to show which of the following?
- A. Elevated prothrombin time (Correct Answer)
- B. Decreased residual volume on spirometry
- C. Cytoplasmic anti-neutrophil cytoplasmic antibodies
- D. Metabolic acidosis
- E. Glutamic acid decarboxylase antibodies
Cystic fibrosis Explanation: ***Elevated prothrombin time***
- This patient's presentation is highly suggestive of **cystic fibrosis**, characterized by recurrent respiratory infections, **malabsorption** (loose, foul-smelling stools, failure to thrive), and a history of **meconium ileus**.
- **Malabsorption** in cystic fibrosis leads to deficiencies of **fat-soluble vitamins** (A, D, E, K). **Vitamin K deficiency** impairs the synthesis of clotting factors II, VII, IX, and X, leading to a **prolonged prothrombin time (PT)**.
*Decreased residual volume on spirometry*
- Patients with cystic fibrosis often develop **obstructive lung disease** due to thick mucus, leading to **air trapping** and subsequent **increased residual volume** on spirometry, not decreased.
- Decreased residual volume is typically associated with **restrictive lung diseases**, which are not characteristic of early cystic fibrosis.
*Cytoplasmic anti-neutrophil cytoplasmic antibodies*
- **c-ANCA** (cytoplasmic anti-neutrophil cytoplasmic antibodies) are associated with **granulomatosis with polyangiitis (Wegener's)**, a vasculitic condition, and are not typically found in cystic fibrosis.
- While cystic fibrosis can cause chronic inflammation, the specific autoantibodies for vasculitis are not characteristic.
*Metabolic acidosis*
- While severe lung disease can lead to **respiratory acidosis** (due to CO2 retention), metabolic acidosis is not a primary or typical feature of cystic fibrosis itself.
- In cases of severe dehydration or other complications, metabolic acidosis could occur, but it's not a defining characteristic of the chronic disease.
*Glutamic acid decarboxylase antibodies*
- **Glutamic acid decarboxylase (GAD) antibodies** are markers for **Type 1 diabetes mellitus**, an autoimmune condition affecting pancreatic beta cells.
- While diabetes can be a complication of cystic fibrosis (cystic fibrosis-related diabetes), GAD antibodies are not a direct finding in cystic fibrosis itself, nor are they the most immediate or common complication at this age.
More Cystic fibrosis US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.