Neural tube defects US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neural tube defects. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neural tube defects US Medical PG Question 1: A 65-year-old woman presents with progressive gait difficulty, neck pain, and bladder incontinence. She also complains of urinary urgency. Past medical history is significant for uncontrolled diabetes mellitus with a previous hemoglobin A1c of 10.8%. Physical examination reveals slightly increased muscle tone in all limbs with brisk tendon reflexes. Sensory examination reveals a decrease of all sensations in a stocking and glove distribution. Her gait is significantly impaired. She walks slowly with small steps and has difficulty turning while walking. She scores 23 out of 30 on a mini-mental state examination (MMSE). A brain MRI reveals dilated ventricles with a callosal angle of 60 degrees and mild cortical atrophy. What is the most appropriate next step in the management of this patient?
- A. Donepezil
- B. Acetazolamide
- C. Ventriculoperitoneal shunt
- D. Large-volume lumbar tap (Correct Answer)
- E. Levodopa
Neural tube defects Explanation: **Large-volume lumbar tap**
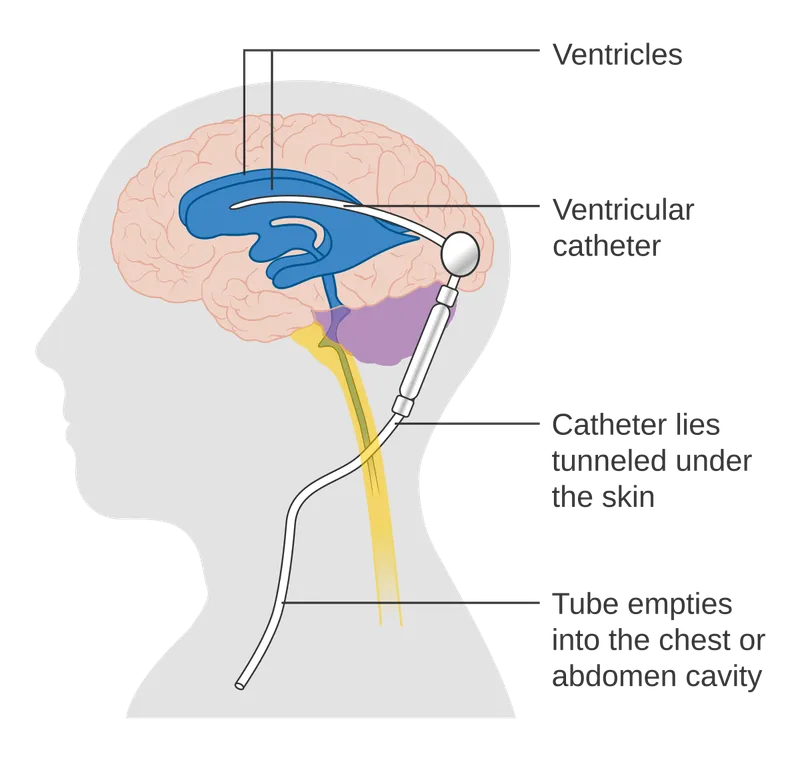
- The symptoms (gait difficulty, urinary incontinence, cognitive decline) in the setting of **hydrocephalus** with a **callosal angle of 60 degrees** are highly suggestive of **Normal Pressure Hydrocephalus (NPH)**. A large-volume lumbar tap is both diagnostic and therapeutic in NPH, as it can temporarily improve symptoms and predict responsiveness to shunting.
- The absence of significant cortical atrophy despite dilated ventricles further supports NPH, as does the improvement in balance and gait after CSF removal.
*Ventriculoperitoneal shunt*
- While a **ventriculoperitoneal shunt** is the definitive treatment for NPH, it is typically performed only after a positive response to a **lumbar tap trial**. This trial helps to confirm the diagnosis and identify patients who are most likely to benefit from the shunt.
- Proceeding directly to shunting without a diagnostic tap could lead to unnecessary surgery in patients who may not benefit or whose symptoms are due to other conditions.
*Donepezil*
- **Donepezil** is an **acetylcholinesterase inhibitor** used in the treatment of **Alzheimer's disease** and other dementias. While cognitive decline is present, the constellation of symptoms (gait disturbance, incontinence, and hydrocephalus) points away from primary Alzheimer's.
- It would not address the underlying pathophysiology of NPH and is unlikely to improve the gait or incontinence.
*Acetazolamide*
- **Acetazolamide** is a **carbonic anhydrase inhibitor** that can reduce **cerebrospinal fluid (CSF) production**. It is sometimes used to manage hydrocephalus in specific circumstances (e.g., communicating hydrocephalus in infants or idiopathic intracranial hypertension).
- However, it is generally not considered effective for NPH, where the issue is impaired CSF absorption rather than overproduction. It also carries side effects that might not be suitable for an elderly patient.
*Levodopa*
- **Levodopa** is a **dopamine precursor** used in the treatment of **Parkinson's disease** to manage motor symptoms like bradykinesia, rigidity, and tremor. While the patient has gait difficulty, the presence of incontinence, cognitive decline, and hydrocephalus points away from Parkinson's disease.
- The gait disturbance in NPH is often described as "magnetic gait" or "gait apraxia," which differs from the shuffling gait of Parkinson's and would not respond to levodopa.
Neural tube defects US Medical PG Question 2: A 25-year-old female comes to her obstetrician’s office for a prenatal visit. She has a transvaginal ultrasound that correlates with her last menstrual period and dates her pregnancy at 4 weeks. She has no complaints except some nausea during the morning that is improving. She comments that she has had some strange food cravings, but has no issues with eating a balanced diet. Her BMI is 23 kg/m^2 and she has gained 1 pound since the start of her pregnancy. She is curious about her pregnancy and asks the physician what her child is now able to do. Which of the following developments is expected of the fetus during this embryological phase?
- A. Formation of male genitalia
- B. Closure of the neural tube (Correct Answer)
- C. Movement of limbs
- D. Creation of the notochord
- E. Cardiac activity visible on ultrasound
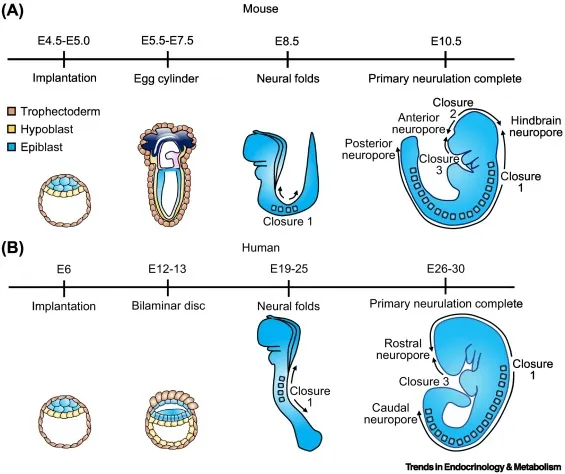
Neural tube defects Explanation: ***Closure of the neural tube***
- At **4 weeks gestation**, the **neural tube** is in the process of closing, forming the precursor for the brain and spinal cord, making this a critical developmental milestone.
- This period is vital for the prevention of neural tube defects like **spina bifida** and **anencephaly**.
*Formation of male genitalia*
- The differentiation of **external genitalia** (male or female) occurs much later, typically around weeks **9-12 of gestation**, much later than the 4-week mark discussed here.
- Prior to this, the genital ridges are bipotential and do not yet show sex-specific characteristics.
*Movement of limbs*
- While limb buds begin to appear around 4-5 weeks, coordinated **limb movements** are typically observed much later, around **10-12 weeks** of gestation, as muscular and neurological systems further develop.
- Early movements are typically subtle and reflex-like, rather than purposeful.
*Creation of the notochord*
- The **notochord** is formed during **gastrulation**, which occurs predominantly in the **third week of gestation**, prior to the 4-week mark.
- It serves as the primary axial support for the embryo and induces the formation of the neural tube.
*Cardiac activity visible on ultrasound*
- **Cardiac activity** typically becomes detectable on transvaginal ultrasound between **5 and 6 weeks gestation**, shortly after the 4-week mark.
- At 4 weeks, the heart tube may have started to form, but discernible beating is usually not yet evident.
Neural tube defects US Medical PG Question 3: A 74-year-old woman is brought to the physician by her daughter for worsening memory for the past 1 month. She can no longer manage her bills and frequently forgets the names of her children. Her daughter is also concerned that her mother has a urinary tract infection because she has had increased urinary urgency and several episodes of urinary incontinence. Vital signs are within normal limits. Physical examination shows poor short-term memory recall and a slow gait with wide, short steps. Which of the following is most likely to improve this patient's condition?
- A. Bromocriptine therapy
- B. Vaginal pessary placement
- C. Cerebral shunt placement (Correct Answer)
- D. Donepezil therapy
- E. Ciprofloxacin therapy
Neural tube defects Explanation: ***Cerebral shunt placement***
- This patient presents with a classic triad of **dementia**, **urinary incontinence**, and **gait disturbance (ataxia)**, highly suggestive of **normal pressure hydrocephalus (NPH)**.
- **Cerebral shunt placement** (e.g., ventriculoperitoneal shunt) is the definitive treatment for NPH, rerouting excess CSF and often leading to significant improvement in symptoms, especially gait and incontinence.
*Bromocriptine therapy*
- **Bromocriptine** is a **dopamine agonist** primarily used in the treatment of **Parkinson's disease** and **hyperprolactinemia**.
- There is no evidence to support its use in improving cognitive or gait symptoms related to normal pressure hydrocephalus.
*Vaginal pessary placement*
- A **vaginal pessary** is used to support pelvic organs and treat **pelvic organ prolapse** or **stress urinary incontinence**.
- While the patient has urinary incontinence, her other symptoms of dementia and gait disturbance point to a central neurological cause rather than a purely gynecological issue.
*Donepezil therapy*
- **Donepezil** is an **acetylcholinesterase inhibitor** used to treat the cognitive symptoms of **Alzheimer's disease** and other dementias.
- While the patient has dementia, the combination of gait disturbance and urinary incontinence makes NPH a more likely diagnosis than Alzheimer's, and donepezil would not address the underlying pathology of NPH.
*Ciprofloxacin therapy*
- **Ciprofloxacin** is an antibiotic used to treat bacterial infections, including **urinary tract infections (UTIs)**.
- Although the patient has urinary symptoms, the presence of dementia and gait disturbance suggests a systemic neurological cause (NPH) rather than just an isolated UTI, and antibiotics would not address these broader issues.
Neural tube defects US Medical PG Question 4: A 24-year-old woman comes to the physician for preconceptional advice. She has been married for 2 years and would like to conceive within the next year. Menses occur at regular 30-day intervals and last 4 days with normal flow. She does not smoke or drink alcohol and follows a balanced diet. She takes no medications. She is 160 cm (5 ft 3 in) tall and weighs 55 kg (121 lb); BMI is 21.5 kg/m2. Physical examination, including pelvic examination, shows no abnormalities. She has adequate knowledge of the fertile days of her menstrual cycle. Which of the following is most appropriate recommendation for this patient at this time?
- A. Begin high-dose vitamin A supplementation
- B. Begin vitamin B12 supplementation
- C. Begin folate supplementation (Correct Answer)
- D. Begin iron supplementation
- E. Gain 2 kg prior to conception
Neural tube defects Explanation: ***Begin folate supplementation***
- **Folate supplementation** of 400 mcg daily is recommended for all women of childbearing age to reduce the risk of **neural tube defects** (NTDs) in the fetus. This should ideally begin at least one month before conception and continue through the first trimester.
- The patient is planning to conceive, making preemptive folate supplementation critical for preventing serious birth defects.
*Begin high-dose vitamin A supplementation*
- **High-dose vitamin A** (more than 10,000 IU/day) can be **teratogenic** and is therefore contraindicated during preconception and pregnancy.
- While vitamin A is essential for fetal development, excessive amounts can lead to fetal abnormalities.
*Begin vitamin B12 supplementation*
- **Vitamin B12 supplementation** is generally not necessary unless the patient has a diagnosed deficiency, such as in strict vegetarians or those with malabsorption issues.
- There is no indication of B12 deficiency in this patient's history or presentation.
*Begin iron supplementation*
- Routine **iron supplementation** is not recommended preconception unless the patient is diagnosed with **iron deficiency anemia**.
- Excessive iron intake without a clear indication can cause gastrointestinal upset and has not been shown to improve pregnancy outcomes in non-anemic women.
*Gain 2 kg prior to conception*
- The patient has a **healthy BMI of 21.5 kg/m2**, which is within the normal range (18.5-24.9 kg/m2).
- There is no medical indication for her to gain weight prior to conception.
Neural tube defects US Medical PG Question 5: A 12-year-old boy follows up with his primary care physician for ongoing management of a urinary tract infection. He recently started middle school and has been having a difficult time navigating the school since he ambulates with leg braces and crutches. Consequently, he has not had sufficient time to use his urinary catheter appropriately. Otherwise, he has been unchanged from the previous visit with both sensory and motor defects in his lower extremities. He has had these defects since birth and has undergone surgeries to repair a bony defect in his spine with protrusion of a membrane through the defect. During what days of embryonic development did the defect responsible for this patient's symptoms most likely occur?
- A. Days 21-35 (Correct Answer)
- B. Days 0-7
- C. Days 8-20
- D. Days 90-birth
- E. Days 36-90
Neural tube defects Explanation: ***Days 21-35***
- This period during embryogenesis is crucial for **neurulation**, the process where the **neural tube** forms and closes. Failure of neural tube closure, particularly in the caudal region, leads to conditions like **spina bifida** (which aligns with the patient's described bony defect and neurological symptoms).
- The patient's history of a **bony defect in the spine with protrusion of a membrane**, along with **sensory and motor defects in the lower extremities** and issues with bladder control (recurrent UTIs and catheter use), strongly indicates a **neural tube defect (NTD)**. Most NTDs occur between days 21 and 28 of embryonic development, encompassing the neural tube closure.
*Days 0-7*
- This initial period involves **fertilization, cleavage**, and **blastulation**. Cellular differentiation and major organ formation have not yet begun.
- Defects during this stage typically result in early embryonic loss or very broad, systemic issues rather than specific structural defects like neural tube closure abnormalities.
*Days 8-20*
- This period includes implantation and early **gastrulation**, where the three germ layers (ectoderm, mesoderm, endoderm) are established.
- While important developmental events occur, **neurulation**, the specific process affected in this patient, primarily begins around day 18-20 and continues into the next period.
*Days 90-birth*
- This period represents the **fetal stage**, characterized by growth and maturation of already formed organs and systems.
- Major structural defects like spina bifida would have already occurred and been established much earlier in embryonic development.
*Days 36-90*
- This period, often referred to as the **fetal period of organogenesis**, involves significant growth and differentiation of organs.
- By this stage, the neural tube would have already closed. While further development and refinement of the nervous system occur, the primary defect of **neural tube closure** would have happened before day 36.
Neural tube defects US Medical PG Question 6: A 34-year-old gravida 2 para 1 woman at 16 weeks gestation presents for prenatal care. Her prenatal course has been uncomplicated. She takes no medications besides her prenatal vitamin which she takes every day, and she has been compliant with routine prenatal care. She has a 7-year-old daughter who is healthy. The results of her recent quadruple screen are listed below:
AFP: Low
hCG: Low
Estriol: Low
Inhibin-A: Normal
Which of the following is the most appropriate next step to confirm the diagnosis?
- A. Chorionic villus sampling
- B. Amniocentesis (Correct Answer)
- C. Ultrasound for nuchal translucency
- D. Folic acid supplementation
- E. Return to clinic in 4 weeks
Neural tube defects Explanation: ***Amniocentesis***
- The presented quad screen results (low AFP, low hCG, low estriol, normal Inhibin-A) are highly suggestive of **trisomy 18 (Edwards syndrome)**. Amniocentesis is a **definitive diagnostic test** that can confirm aneuploidy by providing a fetal karyotype.
- While typically performed between **15 and 20 weeks gestation**, it can differentiate between trisomy 18 and trisomy 21 (Down syndrome), which usually presents with high hCG and high Inhibin-A.
*Chorionic villus sampling (CVS)*
- **CVS** is typically performed earlier in pregnancy, between **10 and 13 weeks gestation**, meaning it is too late to perform at 16 weeks gestation.
- While it can provide a fetal karyotype for genetic diagnosis, the gestational age presented in the vignette makes this option currently inappropriate.
*Ultrasound for nuchal translucency*
- **Nuchal translucency (NT)** is part of the first-trimester screening, usually measured between **11 and 14 weeks gestation**.
- At 16 weeks gestation, measuring NT would be **outside the appropriate timeframe**, and the second-trimester quad screen has already been completed, making further screening rather than diagnosis less useful.
*Folic acid supplementation*
- **Folic acid supplementation** is crucial before and during early pregnancy to prevent neural tube defects, which would be associated with high AFP.
- The patient is already taking prenatal vitamins (which contain folic acid), and her quad screen results are not indicative of a neural tube defect but rather a chromosomal abnormality.
*Return to clinic in 4 weeks*
- The abnormal quad screen results indicate a **high risk for aneuploidy**, specifically trisomy 18, which requires immediate follow-up and definitive diagnosis.
- Delaying further assessment for 4 weeks would be clinically inappropriate and could increase patient anxiety and potentially reduce options for further management.
Neural tube defects US Medical PG Question 7: During development, a fetus is found to have incomplete fusion of the neural tube. Which of the following structures would most likely be affected by this developmental defect?
- A. Notochord
- B. Somites
- C. Vertebral bodies
- D. Spinal cord and meninges (Correct Answer)
Neural tube defects Explanation: ***Spinal cord and meninges***
- Incomplete fusion of the neural tube directly results in defects of the **neural tube closure**, which include the formation of the **spinal cord** and its protective coverings, the **meninges**. [1, 2]
- Conditions like **spina bifida** (meningocele, myelomeningocele) are direct consequences of these fusion failures, exposing or abnormally developing the spinal cord and meninges. [1, 2]
*Notochord*
- The **notochord** is a transient embryonic structure that induces the formation of the neural tube by signaling to the overlying ectoderm; it is not directly formed by the neural tube itself.
- While it plays a critical role in neural tube development, its own structural integrity is typically not primarily affected by neural tube fusion defects.
*Somites*
- **Somites** are blocks of paraxial mesoderm that differentiate into sclerotome (vertebrae and ribs), myotome (skeletal muscle), and dermatome (dermis of the skin).
- While somite development is closely coordinated with neural tube formation, incomplete neural tube fusion primarily affects the neural structures themselves, not the somites directly.
*Vertebral bodies*
- **Vertebral bodies** develop from the sclerotome portion of the somites, which migrate to surround the neural tube and notochord.
- While vertebral defects can be associated with severe neural tube defects (e.g., in spina bifida, the vertebral arches may fail to close), the primary defect of incomplete neural tube fusion directly impacts the neural tissue (spinal cord and meninges), with skeletal defects being secondary or associated. [1, 2]
Neural tube defects US Medical PG Question 8: A male neonate is being examined by a pediatrician. His mother informs the doctor that she had a mild fever with rash, muscle pain, and swollen and tender lymph nodes during the second month of gestation. The boy was born at 39 weeks gestation via spontaneous vaginal delivery with no prenatal care. On physical examination, the neonate has normal vital signs. Retinal examination reveals the findings shown in the image. Which of the following congenital heart defects is most likely to be present in this neonate?
- A. Double outlet right ventricle
- B. Atrial septal defect
- C. Patent ductus arteriosus (Correct Answer)
- D. Ventricular septal defect
- E. Tetralogy of Fallot
Neural tube defects Explanation: ***Patent ductus arteriosus***
- This neonate has **congenital rubella syndrome (CRS)** based on maternal symptoms during the first trimester (fever, rash, lymphadenopathy) and the characteristic **"salt and pepper" retinopathy** shown on retinal examination
- **PDA is the most common cardiac defect** associated with CRS, occurring in approximately 50-85% of affected infants
- Other cardiac manifestations of CRS include peripheral pulmonary artery stenosis, but PDA predominates
- The classic triad of CRS includes cardiac defects, ocular abnormalities (cataracts, glaucoma, retinopathy), and sensorineural deafness
*Double outlet right ventricle*
- This is a **conotruncal anomaly** typically presenting with cyanosis in the neonatal period
- Not associated with maternal rubella infection or congenital rubella syndrome
- Would present with abnormal ventricular anatomy and significant hemodynamic compromise
*Atrial septal defect*
- While ASD is a common congenital heart defect, it is **not characteristically associated with CRS**
- Much less frequently linked to maternal viral infections compared to PDA
- Often asymptomatic in the neonatal period and detected later in childhood
*Ventricular septal defect*
- VSD is less commonly associated with **congenital rubella syndrome** compared to PDA
- When present, typically manifests with a holosystolic murmur at the left lower sternal border
- Can occur with maternal infections but is not the predominant cardiac finding in CRS
*Tetralogy of Fallot*
- Consists of four anatomic abnormalities: VSD, pulmonary stenosis, overriding aorta, and right ventricular hypertrophy
- Presents with **cyanosis** ("tet spells") and is not specifically linked to maternal rubella infection
- Not part of the congenital rubella syndrome spectrum
Neural tube defects US Medical PG Question 9: A 25-year-old pregnant woman, at 18 weeks of gestation, undergoes a routine ultrasound scan. The ultrasound images provided show below. Based on the imaging findings, what is the most likely diagnosis?
- A. Spina bifida (Correct Answer)
- B. Anencephaly
- C. Encephalocele
- D. Holoprosencephaly
- E. Iniencephaly
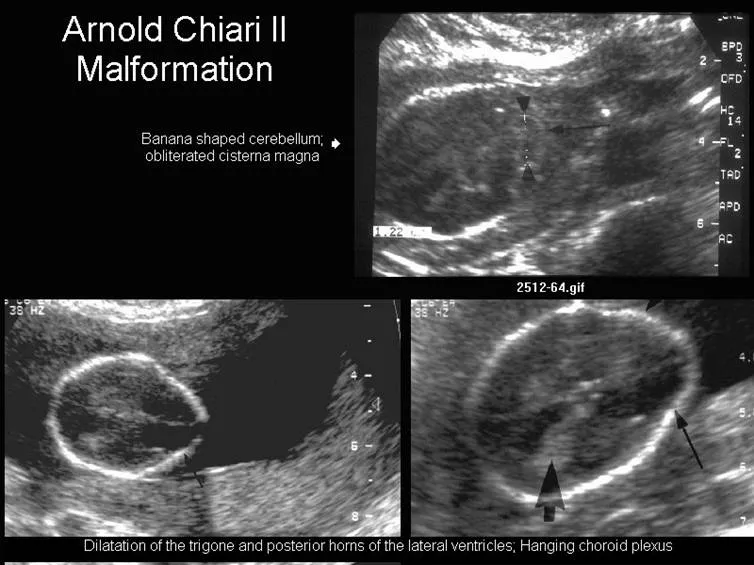
Neural tube defects Explanation: ***Spina bifida***
- The ultrasound image shows a **defect in the posterior elements of the fetal spine**, with characteristic splaying or widening of the vertebral arches.
- This is a **neural tube defect** resulting from incomplete closure of the spinal column during embryonic development.
- Associated findings on prenatal ultrasound may include the **"lemon sign"** (scalloping of frontal bones) and **"banana sign"** (abnormal cerebellar shape).
- Spina bifida is typically detected on **second-trimester anatomy scan** (18-20 weeks).
*Anencephaly*
- This condition involves the **absence of a major portion of the brain, skull, and scalp** due to failure of anterior neural tube closure.
- On ultrasound, anencephaly presents with **absent calvarium above the orbits** and absent cerebral hemispheres, which is distinctly different from a spinal defect.
- This would be a **cranial abnormality**, not a spinal column defect.
*Encephalocele*
- An **encephalocele** is a protrusion of brain tissue and meninges through a defect in the skull, most commonly at the **occipital region**.
- On ultrasound, this appears as a **cranial mass** extending beyond the skull contour, not a spinal defect.
*Holoprosencephaly*
- This condition results from **failure of forebrain (prosencephalon) to divide properly** into two hemispheres.
- Ultrasound findings include **single ventricle**, fused thalami, and absent midline structures, often with associated **facial anomalies**.
- The imaging would show **brain abnormalities**, not spinal column defects.
*Iniencephaly*
- This is a rare **neural tube defect** characterized by extreme retroflexion of the head with severe spinal defects in the cervical and thoracic regions.
- On ultrasound, iniencephaly shows the fetal head in extreme **hyperextension** with the face looking upward, creating a characteristic "stargazing" appearance.
- This differs from the typical spinal defect pattern seen in spina bifida.
Neural tube defects US Medical PG Question 10: What condition is associated with the sign seen in the given USG?
- A. Anencephaly
- B. Spina bifida (Correct Answer)
- C. Dandy-Walker malformation
- D. Encephalocele
Neural tube defects Explanation: ***Spina bifida***
- The ultrasound image displays the **"lemon sign"** (frontal bone indentation), which is a classic indicator of **spina bifida** on antenatal ultrasound.
- The lemon sign is caused by **scalloping of the frontal bones** due to caudal displacement of brain tissue (Arnold-Chiari malformation type II) secondary to an open spinal defect.
- This sign is most commonly seen in the **second trimester** and is associated with neural tube defects.
*Anencephaly*
- **Anencephaly** presents with absence of the cranial vault and cerebral hemispheres on ultrasound.
- The characteristic finding is the **"frog-eye appearance"** with protruding orbits, not frontal bone scalloping.
- This is incompatible with life and has a distinctly different ultrasound appearance.
*Dandy-Walker malformation*
- **Dandy-Walker malformation** shows an enlarged posterior fossa with cystic dilatation of the fourth ventricle and hypoplasia of the cerebellar vermis.
- It may present with the **"banana sign"** (cerebellar compression), but not the lemon sign.
- This is a posterior fossa abnormality, not associated with frontal bone changes.
*Encephalocele*
- **Encephalocele** presents as a herniation of brain tissue and meninges through a cranial defect, typically occipital.
- Ultrasound shows a **cystic mass protruding from the skull**, not frontal bone indentation.
- While it's a neural tube defect, it has a different ultrasound appearance than the lemon sign.
More Neural tube defects US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.
 shunt placement for hydrocephalus)
shunt placement for hydrocephalus)
