Long-term outcomes and follow-up US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Long-term outcomes and follow-up. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Long-term outcomes and follow-up US Medical PG Question 1: A 14-year-old girl is brought to the physician because she frequently experiences cramping and pain in her legs during school sports. She is at the 10th percentile for height. Her blood pressure is 155/90 mm Hg. Examination shows a high-arched palate with maloccluded teeth and a low posterior hairline. The patient has a broad chest with widely spaced nipples. Pelvic examination shows normal external female genitalia with scant pubic hair. Without appropriate treatment, this patient is at the greatest risk of developing which of the following complications?
- A. Alzheimer disease
- B. Hyperphagia
- C. Pulmonary stenosis
- D. Osteoporosis (Correct Answer)
- E. Severe acne
Long-term outcomes and follow-up Explanation: ***Osteoporosis***
- This patient's presentation with **short stature**, high blood pressure, **webbed neck** (implied by low posterior hairline), and **wide-spaced nipples** is highly suggestive of **Turner syndrome (45,X0)**.
- Turner syndrome is characterized by **gonadal dysgenesis**, leading to **estrogen deficiency**, which is a major risk factor for developing **osteoporosis**.
- Without estrogen replacement therapy, patients with Turner syndrome have significantly increased risk of **low bone mineral density** and **fractures**.
*Pulmonary stenosis*
- While Turner syndrome is associated with **cardiac anomalies** such as **bicuspid aortic valve** and **coarctation of the aorta**, these are typically **congenital defects** present from birth rather than complications that develop over time.
- **Pulmonary stenosis** itself is not a primary cardiac finding in Turner syndrome.
- The question asks about complications that develop without treatment, making **osteoporosis** more appropriate as it progressively worsens due to chronic **estrogen deficiency**.
*Alzheimer disease*
- **Alzheimer disease** is a neurodegenerative disorder primarily associated with aging and genetics, not typically a direct complication of Turner syndrome.
- While cognitive profiles in Turner syndrome can differ (particularly with visuospatial skills), there is no established increased risk of Alzheimer disease.
*Hyperphagia*
- **Hyperphagia** (excessive eating) is characteristically associated with **Prader-Willi syndrome** due to hypothalamic dysfunction.
- It is not a feature or complication of **Turner syndrome**.
*Severe acne*
- **Severe acne** is often related to increased androgen levels or hormonal fluctuations during puberty.
- In Turner syndrome, there is typically **hypogonadism** and **estrogen deficiency**, which would not predispose to severe acne.
Long-term outcomes and follow-up US Medical PG Question 2: A 15-month-old boy is brought to the pediatrician for immunizations and assessment. His parents report that he is eating well and produces several wet diapers every day. He is occasionally fussy, but overall a happy and curious child. The boy was born at 39 weeks gestation via spontaneous vaginal delivery. On physical examination his vital signs are stable. His weight and height are above the 85th percentile for his age and sex. On chest auscultation, the pediatrician detects a loud harsh holosystolic murmur over the left lower sternal border. The first and second heart sounds are normal. An echocardiogram confirms the diagnosis of the muscular ventricular septal defect without pulmonary hypertension. Which of the following is the best management strategy for this patient?
- A. Surgical closure of the defect using cardiopulmonary bypass
- B. Reassurance of the parents and regular follow-up (Correct Answer)
- C. Oral digoxin and regular follow-up
- D. Antibiotic prophylaxis against infective endocarditis
- E. Transcatheter occlusion closure of the defect
Long-term outcomes and follow-up Explanation: **Reassurance of the parents and regular follow-up**
- Most **small muscular VSDs (Ventricular Septal Defects)**, especially in asymptomatic children with normal growth and no signs of heart failure or pulmonary hypertension, **close spontaneously**.
- Given the patient's normal development, stable vital signs, good feeding, and lack of pulmonary hypertension, a conservative approach with **monitoring for spontaneous closure** is appropriate.
*Surgical closure of the defect using cardiopulmonary bypass*
- **Surgical VSD closure** is typically reserved for large defects causing **symptoms, growth failure, pulmonary hypertension**, or those that fail to close spontaneously.
- The patient in the scenario is asymptomatic and thriving, which does not warrant an invasive procedure at this time.
*Oral digoxin and regular follow-up*
- **Digoxin** is a medication used to improve **cardiac contractility** and manage symptoms of **heart failure**, which this patient does not exhibit.
- It would only be considered if there were signs of **congestive heart failure** due to a large VSD, which is not the case here.
*Antibiotic prophylaxis against infective endocarditis*
- Current guidelines from the American Heart Association (AHA) generally **do not recommend routine antibiotic prophylaxis** for VSDs unless there's a history of infective endocarditis or uncorrected cyanotic heart disease.
- The risk of **infective endocarditis** is very low in isolated VSDs and the potential side effects of prophylactic antibiotics outweigh the benefits.
*Transcatheter occlusion closure of the defect*
- **Transcatheter closure** is an option for certain types of VSDs, often **muscular VSDs**, but typically for those that are **larger, symptomatic**, and have not closed spontaneously.
- Similar to surgical closure, this invasive procedure is not indicated for an **asymptomatic, thriving child** with a muscular VSD that is likely to close on its own.
Long-term outcomes and follow-up US Medical PG Question 3: A 3-year-old girl is brought to the physician for a well-child examination. She was born at term and has been healthy since. She can climb up and down the stairs and can pedal a tricycle. She has difficulty using a spoon to feed herself but can copy a line. She speaks in 2- to 3-word sentences that can be understood by most people. She is selfish while playing with children her age and throws tantrums quite often. She cannot put on her own shoes and socks. She does not tolerate separation from her parents. She is at 60th percentile for height and weight. Physical examination including neurologic examination reveals no abnormalities. Which of the following is the most appropriate assessment of her development?
- A. Fine motor: Normal | Gross motor: Normal | Language: Delayed | Social skills: Delayed
- B. Fine motor: Delayed | Gross motor: Delayed | Language: Normal | Social skills: Normal
- C. Fine motor: Delayed | Gross motor: Normal | Language: Normal | Social skills: Delayed (Correct Answer)
- D. Fine motor: Normal | Gross motor: Delayed | Language: Normal | Social skills: Delayed
- E. Fine motor: Normal | Gross motor: Delayed | Language: Delayed | Social skills: Normal
Long-term outcomes and follow-up Explanation: ***Fine motor: Delayed | Gross motor: Normal | Language: Normal | Social skills: Delayed***
- The child can copy a line (expected at 3 years) and climb stairs and pedal a tricycle (expected for a 3-year-old), indicating **normal gross motor skills**. However, difficulty using a spoon and putting on shoes/socks suggests **delayed fine motor skills**.
- Speaking in 2- to 3-word sentences understood by most (expected for 2-3 years) indicates **normal language development**. Being selfish and throwing tantrums (normal for 2-3 years) but not tolerating separation (suggests earlier developmental stage for separation anxiety) point to **delayed social skills**.
*Fine motor: Normal | Gross motor: Normal | Language: Delayed | Social skills: Delayed*
- This option incorrectly assesses fine motor skills as normal when the child struggles with tasks like using a spoon and dressing herself.
- While language and social skills are correctly identified as delayed, the overall assessment of fine motor makes this option incorrect.
*Fine motor: Delayed | Gross motor: Delayed | Language: Normal | Social skills: Normal*
- This option incorrectly assesses gross motor skills as delayed, despite the child's ability to climb stairs and pedal a tricycle, which are age-appropriate.
- It also incorrectly assesses social skills as normal, overlooking the persistent separation anxiety and aggressive social play for her age.
*Fine motor: Normal | Gross motor: Delayed | Language: Normal | Social skills: Delayed*
- This option incorrectly describes fine motor skills as normal and gross motor skills as delayed.
- Her ability to pedal a tricycle and climb stairs indicates age-appropriate gross motor development, while her difficulty with a spoon suggests delayed fine motor skills.
*Fine motor: Normal | Gross motor: Delayed | Language: Delayed | Social skills: Normal*
- This option incorrectly states that both fine motor and gross motor skills are affected and also mischaracterizes social skills as normal.
- The child's language development is within the normal range for a 3-year-old, and her social behavior, particularly the separation anxiety, indicates a delay.
Long-term outcomes and follow-up US Medical PG Question 4: Five minutes after initiating a change of position and oxygen inhalation, the oxytocin infusion is discontinued. A repeat CTG that is done 10 minutes later shows recurrent variable decelerations and a total of 3 uterine contractions in 10 minutes. Which of the following is the most appropriate next step in management?
- A. Restart oxytocin infusion
- B. Emergent Cesarean section
- C. Administer terbutaline
- D. Monitor without intervention
- E. Amnioinfusion (Correct Answer)
Long-term outcomes and follow-up Explanation: ***Amnioinfusion***
- **Recurrent variable decelerations** persisting after discontinuing oxytocin and changing maternal position often indicate **cord compression**, which can be relieved by amnioinfusion.
- Adding fluid to the amniotic cavity **cushions the umbilical cord**, reducing compression during uterine contractions.
*Restart oxytocin infusion*
- Reinitiating oxytocin would likely **worsen the recurrent variable decelerations** by increasing uterine contraction frequency and intensity, thereby exacerbating cord compression.
- The goal is to alleviate fetal distress, not to intensify uterine activity that is already causing issues.
*Emergent Cesarean section*
- While an emergent Cesarean section is indicated for **unresolved fetal distress**, it's usually considered after less invasive measures, such as amnioinfusion, have failed.
- There is still an opportunity for a simpler intervention to resolve the issue before resorting to surgery.
*Administer terbutaline*
- Terbutaline is a **tocolytic agent** used to reduce uterine contractions, which can be helpful in cases of tachysystole or hyperstimulation.
- In this scenario, the contraction frequency is low (3 in 10 minutes), so reducing contractions is not the primary aim; rather, the focus is on resolving the cord compression causing decelerations.
*Monitor without intervention*
- **Recurrent variable decelerations** are an concerning sign of **fetal distress** and require intervention to prevent potential harm to the fetus.
- Simply monitoring without intervention would be inappropriate and could lead to worsening fetal hypoxemia and acidosis.
Long-term outcomes and follow-up US Medical PG Question 5: A 1-day-old infant in the general care nursery, born at full term by uncomplicated cesarean section delivery, is noted to have a murmur, but otherwise appears well. On examination, respiratory rate is 40/min and pulse oximetry is 96%. Precordium is normoactive. With auscultation, S1 is normal, S2 is single, and a 2/6 systolic ejection murmur is heard at the left upper sternal border. Echocardiography shows infundibular pulmonary stenosis, overriding aorta, ventricular septal defect and concentric right ventricular hypertrophy. Which of the following correlate with the presence or absence of cyanosis in this baby?
- A. The degree of right ventricular outflow tract obstruction (Correct Answer)
- B. The ratio of reduced hemoglobin to oxyhemoglobin
- C. The concentration of hemoglobin
- D. The size of ventricular septal defect
- E. The concentration of pulmonary surfactant
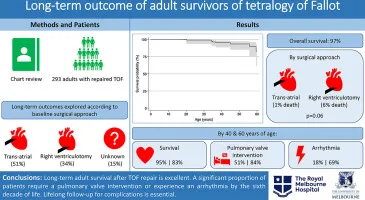
Long-term outcomes and follow-up Explanation: ***The degree of right ventricular outflow tract obstruction***
- The severity of **pulmonary stenosis** in **tetralogy of Fallot** dictates the amount of blood shunted from the right ventricle to the aorta via the **ventricular septal defect (VSD)**.
- A **less severe obstruction** allows more blood to flow to the lungs, leading to less right-to-left shunting and consequently **less cyanosis**.
*The ratio of reduced hemoglobin to oxyhemoglobin*
- While this ratio directly reflects the presence of cyanosis, it does not explain its *cause* in the context of the given congenital heart defect.
- The question asks what *correlates* with the presence or absence of cyanosis, implying a causal or pathophysiological link rather than a descriptive measure.
*The concentration of hemoglobin*
- **Hemoglobin concentration** affects the *visibility* of cyanosis (e.g., polycythemia can make mild desaturation appear more cyanotic), but it doesn't primarily determine the *presence* or *absence* of shunt-related cyanosis itself.
- A patient can be significantly desaturated with a normal hemoglobin concentration, and the degree of desaturation is largely driven by the shunt.
*The size of ventricular septal defect*
- In tetralogy of Fallot, the **VSD is typically large and non-restrictive**, meaning its size itself doesn't limit blood flow between the ventricles.
- The **pulmonary stenosis** is the primary determinant of the shunt direction and magnitude, not the size of the VSD.
*The concentration of pulmonary surfactant*
- **Pulmonary surfactant** is crucial for maintaining alveolar stability and preventing atelectasis, thereby ensuring efficient gas exchange in the lungs.
- While important for overall respiratory function, it does not directly correlate with the degree of shunting and cyanosis in **tetralogy of Fallot**.
Long-term outcomes and follow-up US Medical PG Question 6: A 4-year-old girl is brought to the physician by her parents because she is severely underweight. She is easily fatigued and has difficulty keeping up with other children at her daycare. She has a good appetite and eats 3 full meals a day. She has 4 to 5 bowel movements daily with bulky, foul-smelling stools that float. She has had recurrent episodes of sinusitis since infancy. Her parents report that she recently started to snore during her sleep. She is at the 15th percentile for height and 3rd percentile for weight. Her vital signs are within normal limits. Examination shows pale conjunctivae. A few scattered expiratory crackles are heard in the thorax. There is abdominal distention. Which of the following is the most likely underlying cause of this patient's failure to thrive?
- A. T. whippelii infiltration of intestinal villi
- B. Impaired intestinal amino acid transport
- C. Exocrine pancreatic insufficiency (Correct Answer)
- D. Small intestine bacterial overgrowth
- E. Intestinal inflammatory reaction to gluten
Long-term outcomes and follow-up Explanation: ***Exocrine pancreatic insufficiency***
- The constellation of **failure to thrive**, **bulky, foul-smelling, floating stools** (suggesting **steatorrhea**), recurrent **sinusitis**, and **recurrent respiratory symptoms** (snoring, expiratory crackles) is highly indicative of **cystic fibrosis**, whose primary cause of malabsorption is **exocrine pancreatic insufficiency**.
- **Cystic fibrosis** leads to thick, viscous secretions that obstruct pancreatic ducts, preventing digestive enzymes from reaching the small intestine and causing **malabsorption of fats and fat-soluble vitamins**.
*T. whippelii infiltration of intestinal villi*
- This describes **Whipple's disease**, which typically affects **middle-aged men** and presents with malabsorption, arthralgia, and neurological symptoms.
- It is rare in children and usually presents with symptoms like diarrhea and weight loss, but not commonly with the **recurrent respiratory infections** and **pancreatic insufficiency** seen here.
*Impaired intestinal amino acid transport*
- This typically refers to conditions like **Hartnup disease**, which involves defective transport of neutral amino acids and can lead to **pellagra-like symptoms** (dermatitis, diarrhea, dementia) due to niacin deficiency.
- This condition does not explain the **steatorrhea**, **recurrent sinusitis**, or **respiratory symptoms** found in the patient.
*Small intestine bacterial overgrowth*
- While **SIBO** can cause malabsorption, **abdominal distention**, and loose stools, it does not typically cause **recurrent sinusitis** or the classic **bulky, foul-smelling, floating stools associated with pancreatic insufficiency**.
- SIBO is also not a primary cause of **failure to thrive** in a global sense, but rather a secondary complication.
*Intestinal inflammatory reaction to gluten*
- This describes **celiac disease**, which presents with **malabsorption**, **abdominal distention**, **failure to thrive**, and **anemia** (pale conjunctivae).
- However, celiac disease does not typically cause **recurrent sinusitis** or the **respiratory symptoms** (snoring, crackles) that are prominent in this patient's presentation.
Long-term outcomes and follow-up US Medical PG Question 7: A 3-year-old male presents with his parents to a pediatrician for a new patient visit. The child was recently adopted and little is known about his prior medical or family history. The parents report that the child seems to be doing well, but they are concerned because the patient is much larger than any of the other 3-year-olds in his preschool class. They report that he eats a varied diet at home, and that they limit juice and snack foods. On physical exam, the patient is in the 73rd percentile for weight, 99th percentile for height, and 86th percentile for head circumference. He appears mildly developmentally delayed. He has a fair complexion and tall stature with a prominent sternum. The patient also has joint hypermobility and hyperelastic skin. He appears to have poor visual acuity and is referred to an ophthalmologist, who diagnoses upward lens subluxation of the right eye.
This child is most likely to develop which of the following complications?
- A. Osteoarthritis
- B. Wilms tumor
- C. Medullary thyroid cancer
- D. Aortic dissection (Correct Answer)
- E. Thromboembolic stroke
Long-term outcomes and follow-up Explanation: ***Aortic dissection***
- The constellation of **tall stature**, **prominent sternum**, **joint hypermobility**, **hyperelastic skin**, and **upward lens subluxation (ectopia lentis)** in a young child strongly suggests **Marfan syndrome**.
- **Aortic root dilation** and subsequent **aortic dissection** are the most serious cardiovascular complications in Marfan syndrome due to weakened connective tissue in the aortic wall caused by **fibrillin-1 deficiency**.
- This is the **leading cause of mortality** in untreated Marfan syndrome.
*Osteoarthritis*
- While joint hypermobility can contribute to **joint instability** and accelerate degenerative changes, typical **osteoarthritis** is less common as a primary, severe complication in childhood Marfan syndrome.
- Early-onset, severe osteoarthritis is not the major life-threatening complication associated with Marfan syndrome at this age.
*Wilms tumor*
- **Wilms tumor** is a type of kidney cancer typically associated with syndromes like **WAGR (Wilms tumor, Aniridia, Genitourinary anomalies, intellectual disability)** or **Beckwith-Wiedemann syndrome**, none of which fit the patient's presentation.
- There is no known direct association between Wilms tumor and Marfan syndrome.
*Medullary thyroid cancer*
- **Medullary thyroid cancer** is a feature of **Multiple Endocrine Neoplasia type 2 (MEN 2) syndromes**, which also present with pheochromocytomas and parathyroid hyperplasia.
- The clinical features described in the patient are not consistent with MEN 2.
*Thromboembolic stroke*
- While Marfan syndrome can lead to cardiovascular issues, a **thromboembolic stroke** is not a primary or characteristic complication, especially in comparison to the high risk of aortic dissection.
- The main vascular pathology in Marfan is related to connective tissue weakness, not primarily hypercoagulability or mural thrombi leading to stroke.
- Thromboembolic complications are more characteristic of **homocystinuria**, which presents with **downward** lens subluxation.
Long-term outcomes and follow-up US Medical PG Question 8: A 2860-g (6-lb 3-oz) male newborn is born at term to a primigravid woman via spontaneous vaginal delivery. The mother has had no routine prenatal care. She reports that there is no family history of serious illness. The initial examination of the newborn shows bowing of the legs and respiratory distress upon palpation of the chest. The skin and joints are hyperextensible. X-rays of the chest and skull show multiple rib fractures and small, irregular bones along the cranial sutures. The patient is at increased risk of which of the following complications?
- A. Hearing loss (Correct Answer)
- B. Spinal canal stenosis
- C. Costochondral junction enlargement
- D. Intestinal rupture
- E. Intellectual disability
Long-term outcomes and follow-up Explanation: ***Hearing loss***
- The described clinical picture of **bone fragility (multiple rib fractures, bowing of legs)**, **hyperextensible skin and joints**, and **wormian bones** (small, irregular bones along cranial sutures) is classic for **osteogenesis imperfecta (OI)**.
- Individuals with OI are at increased risk for **conductive or sensorineural hearing loss**, which can manifest in childhood or adolescence.
*Spinal canal stenosis*
- While patients with OI can develop **scoliosis** and **vertebral compression fractures**, resulting in spinal cord compression, **spinal canal stenosis** itself is not a primary or direct complication of the underlying collagen defect in the same way hearing loss is.
- The primary spinal complications are related to **vertebral fractures** and **deformities**.
*Costochondral junction enlargement*
- **Costochondral junction enlargement** (rachitic rosary) is a hallmark of **rickets**, a disorder of **vitamin D or phosphate metabolism**, not osteogenesis imperfecta.
- The described features point to a **collagen synthesis defect**, not mineralization issues.
*Intestinal rupture*
- While there can be some smooth muscle abnormalities, **intestinal rupture** is not a commonly described or significant complication of osteogenesis imperfecta.
- The primary systemic manifestations relate to **collagen defects** in bone, skin, tendons, and blood vessels, but not typically leading to spontaneous gastrointestinal rupture.
*Intellectual disability*
- **Intellectual function** is typically **unaffected** in osteogenesis imperfecta.
- The disease primarily affects **connective tissue**, particularly bone development, and does not directly cause cognitive impairment.
Long-term outcomes and follow-up US Medical PG Question 9: A 3-month-old African American boy presents to his pediatrician’s office for his routine well visit. He was born full-term from an uncomplicated vaginal delivery. He is exclusively breastfeeding and not receiving any medications or supplements. Today, his parents report no issues or concerns with their child. He is lifting his head for brief periods and smiling. He has received only 2 hepatitis B vaccines. Which of the following is the correct advice for this patient’s parents?
- A. He should be sleeping more.
- B. He should have his serum lead level checked to screen for lead intoxication.
- C. He should start vitamin D supplementation. (Correct Answer)
- D. He should start rice cereal.
- E. He needs a 3rd hepatitis B vaccine.
Long-term outcomes and follow-up Explanation: ***He should start vitamin D supplementation.***
- **Exclusively breastfed** infants, regardless of maternal vitamin D intake, require **vitamin D supplementation** due to insufficient amounts in breast milk.
- The recommended daily dose is **400 IU** starting from the first few days of life, to prevent **rickets** and promote bone health.
- **African American infants** have an additional risk factor due to increased skin melanin content, which reduces cutaneous vitamin D synthesis from sunlight exposure.
*He should be sleeping more.*
- A 3-month-old infant typically sleeps between **14-17 hours per day**, with **waking periods to feed** and interact.
- The case description does not indicate any concerns with the child's sleep patterns, and **developmental milestones** like lifting his head and smiling are being met.
*He should have his serum lead level checked to screen for lead intoxication.*
- **Lead screening** is not routinely recommended for all infants unless specific **risk factors** are present, such as living in an older home with lead paint, or having siblings with elevated lead levels.
- There are no reported risk factors for lead exposure in this patient's history.
*He should start rice cereal.*
- Introduction of solid foods, such as rice cereal, is typically recommended around **6 months of age**, when the infant shows signs of **developmental readiness**.
- These signs include **head control**, sitting with support, and showing interest in food.
*He needs a 3rd hepatitis B vaccine.*
- The **third dose of the hepatitis B vaccine** is typically administered between **6 and 18 months of age**.
- At 3 months old, the infant is not yet due for his third dose.
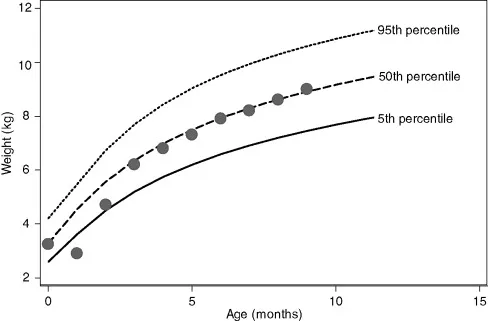
Long-term outcomes and follow-up US Medical PG Question 10: A 3-month-old male presents to the pediatrician with his mother for a well child visit. The patient drinks 4 ounces of conventional cow’s milk formula every three hours. He usually stools once per day, and urinates up to six times per day. His mother reports that he regurgitates a moderate amount of formula through his nose and mouth after most feeds. He does not seem interested in additional feeding after these episodes of regurgitation, and he has become progressively more irritable around meal times. The patient is starting to refuse some feeds. His mother denies ever seeing blood or streaks of red in his stool, and she denies any family history of food allergies or dermatological problems. The patient’s weight was in the 75th percentile for weight throughout the first month of life. Four weeks ago, he was in the 62nd percentile, and he is now in the 48th percentile. His height and head circumference have followed similar trends. On physical exam, the patient smiles reciprocally and can lift his head and chest when in the prone position. His abdomen is soft, non-tender, and non-distended.
Which of the following is the best next step in management?
- A. Switch to hydrolyzed formula
- B. Obtain abdominal ultrasound
- C. Initiate proton pump inhibitor
- D. Provide reassurance
- E. Counsel on positioning and thickening feeds (Correct Answer)
Long-term outcomes and follow-up Explanation: ***Counsel on positioning and thickening feeds***
- The infant's symptoms, including **regurgitation**, **irritability during feeds**, and **dropping weight percentiles**, are indicative of severe gastroesophageal reflux (GER). Initial management should focus on **conservative measures** like positioning modifications (keeping upright after feeds), thickening feeds, and smaller, more frequent feedings.
- Given the absence of **hematemesis**, **hematochezia**, or **projectile vomiting**, further invasive diagnostics or medication are not immediately warranted.
*Switch to hydrolyzed formula*
- This would be considered if there were signs suggestive of a **cow's milk protein allergy**, such as **bloody stools**, **diarrhea**, **eczema**, or a strong family history of allergies, which are all absent in this case.
- Allergy is less likely to be the primary cause of isolated severe regurgitation with failure to thrive without other allergic manifestations.
*Obtain abdominal ultrasound*
- An **abdominal ultrasound** is primarily used to evaluate for conditions like **pyloric stenosis** if there is **projectile vomiting**, an **olive-shaped mass**, or severe dehydration and electrolyte imbalances, none of which are present.
- While it can assess for **malrotation or intussusception**, these conditions typically present with more acute, severe symptoms like **bilious vomiting**, abdominal distension, or currant jelly stools, which are not described.
*Initiate proton pump inhibitor*
- **Proton pump inhibitors (PPIs)** are reserved for infants with confirmed **erosive esophagitis** or severe symptoms unresponsive to lifestyle modifications.
- Starting a PPI without first attempting conservative measures or confirming pathological acid reflux is generally not recommended, especially given potential side effects like increased risk of infections.
*Provide reassurance*
- While **reassurance** is important, it is not the sole appropriate next step. The infant's **dropping weight percentiles** and significant feeding difficulties suggest that this is beyond typical "spitting up" and requires intervention to prevent further impact on growth and comfort.
- Simply reassuring the mother would ignore the clinical signs of **failure to thrive** and significant discomfort during feeds.
More Long-term outcomes and follow-up US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.