Genitourinary anomalies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Genitourinary anomalies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Genitourinary anomalies US Medical PG Question 1: A 16-year-old teenager presents to his pediatrician complaining of burning with urination and purulent urethral discharge. He states that he has had unprotected sex with his girlfriend several times and recently she told him that she has gonorrhea. His blood pressure is 119/78 mm Hg, pulse is 85/min, respiratory rate is 14/min, and temperature is 36.8°C (98.2°F). The urethral meatus appears mildly erythematous, but no pus can be expressed. A testicular examination is normal. An in-office urine test reveals elevated leukocyte esterase levels. An additional swab was taken for further analysis. The patient wants to get treated right away but is afraid because he does not want his parents to know he is sexually active. What is the most appropriate next step for the pediatrician?
- A. Inform the patient that his parents will not be informed, but he cannot receive medical care without their consent.
- B. Contact child protective services.
- C. Break confidentiality and inform the patient that his parents must consent to this treatment.
- D. Maintain confidentiality and treat the patient. (Correct Answer)
- E. Treat the patient and then break confidentiality and inform the parents of the care he received.
Genitourinary anomalies Explanation: ***Maintain confidentiality and treat the patient.***
* In many jurisdictions, adolescents (often those 12 and older) can consent to **STI treatment** and other sensitive health services (like contraception or mental health care) **without parental consent**, based on **minor consent laws**.
* Prompt treatment is crucial for **gonorrhea** to prevent complications and further transmission, and maintaining confidentiality encourages adolescents to seek necessary care.
*Inform the patient that his parents will not be informed, but he cannot receive medical care without their consent.*
* This statement is incorrect as, in many places, minors can consent to **STI treatment** independently, recognizing the public health importance and the sensitive nature of these conditions.
* Requiring parental consent for STI treatment would create a barrier to care, potentially leading to **untreated infections** and increased transmission risks among adolescents.
*Contact child protective services.*
* This situation involves an adolescent seeking healthcare for an **STI** and a desire for confidentiality, which does not constitute a reason to contact **child protective services (CPS)**.
* CPS is typically contacted in cases of suspected **child abuse, neglect**, or severe safety concerns, none of which are indicated here.
*Break confidentiality and inform the patient that his parents must consent to this treatment.*
* Breaking confidentiality and insisting on parental consent for **STI treatment** for an adolescent is generally not legally or ethically appropriate in many jurisdictions due to **minor consent laws**.
* This action would likely deter the patient from seeking necessary medical care for fear of parental knowledge, compromising their **health and public health efforts** to control STIs.
*Treat the patient and then break confidentiality and inform the parents of the care he received.*
* While treating the patient is appropriate, breaking **confidentiality** afterward by informing the parents without the patient's consent would be a violation of the trust established and potentially ethical and legal guidelines (depending on the jurisdiction).
* The patient explicitly expressed a desire for confidentiality regarding his sexual activity, and breaching this trust, even after treatment, could harm the **patient-provider relationship** and deter future healthcare-seeking behavior.
Genitourinary anomalies US Medical PG Question 2: A 16-year-old girl is brought to the physician because she has not attained menarche. There is no personal or family history of serious illness. She is 165 cm (5 ft 5 in) tall and weighs 60 kg (132 lb); BMI is 22 kg/m2. Breast development is Tanner stage 4, and pubic hair development is Tanner stage 1. Pelvic examination shows a blind vaginal pouch. This patient is most likely to have which of the following karyotypes?
- A. 47,XYY
- B. 46,XY (Correct Answer)
- C. 47,XXY
- D. 46,XX
- E. 45,XO
Genitourinary anomalies Explanation: ***46,XY***
- This karyotype, in the presence of **androgen insensitivity syndrome (AIS)**, explains the presentation: a genetic male (XY) who phenotypically appears female due to **androgen receptor defects**, leading to lack of masculinization and female external genitalia.
- The **blind vaginal pouch** and **absent uterus/cervix** (implied by lack of menarche despite breast development) are characteristic of AIS, as is the normal range of height and weight, and presence of breast development due to peripheral aromatization of androgens.
*47,XYY*
- This karyotype is associated with **XYY syndrome**, typically affecting males and not causing primary amenorrhea or female phenotypic development.
- Individuals with XYY syndrome are usually tall and may experience learning difficulties or behavioral issues, but they have normal male sexual development.
*47,XXY*
- This karyotype is characteristic of **Klinefelter syndrome**, affecting males and typically presenting with **hypogonadism**, small testes, gynecomastia, and often infertility.
- It does not cause a female phenotype, primary amenorrhea, or a blind vaginal pouch.
*46,XX*
- This is the normal female karyotype; if this patient had 46,XX, the most likely cause of primary amenorrhea would be **Müllerian agenesis (Mayer-Rokitansky-Küster-Hauser syndrome)**.
- However, in Müllerian agenesis, despite underdeveloped or absent vagina, uterus, and cervix, **normal ovarian function** would lead to typical pubic hair development (Tanner stage 4-5) and secondary sexual characteristics congruent with age, which contrasts with the Tanner stage 1 pubic hair here.
*45,XO*
- This karyotype denotes **Turner syndrome**, which presents with primary amenorrhea, but also with characteristic features such as **short stature**, streak gonads, and often specific dysmorphic features (e.g., webbed neck, shield chest).
- The patient's normal height and significant breast development (Tanner stage 4) make Turner syndrome unlikely, as ovarian failure in Turner syndrome typically prevents substantial breast development without hormone therapy.
Genitourinary anomalies US Medical PG Question 3: A 46-year-old woman presents to the clinic complaining that she “wets herself.” She states that over the past year she has noticed increased urinary leakage. At first it occurred only during her job, which involves restocking shelves with heavy appliances. Now she reports that she has to wear pads daily because leakage of urine will occur with simply coughing or sneezing. She denies fever, chills, dysuria, hematuria, or flank pain. She has no significant medical or surgical history, and takes no medications. Her last menstrual period was 8 months ago. She has 3 healthy daughters that were born by vaginal delivery. Which of the following tests, if performed, would most likely identify the patient’s diagnosis?
- A. Methylene blue dye
- B. Post-void residual volume
- C. Urodynamic testing
- D. Estrogen level
- E. Q-tip test (Correct Answer)
Genitourinary anomalies Explanation: ***Q-tip test***
- The patient's symptoms (leakage with coughing/sneezing, lifting heavy objects, vaginal deliveries, recent cessation of menses) are classic for **stress urinary incontinence**, often due to **urethral hypermobility**.
- The **Q-tip test** assesses urethral hypermobility by measuring the angle of deflection of a sterile cotton swab inserted into the urethra during a Valsalva maneuver. An angle >30 degrees from the horizontal indicates hypermobility.
*Methylene blue dye*
- **Methylene blue dye** is primarily used to identify **vesicovaginal or ureterovaginal fistulas**, where dye would be seen leaking into the vagina.
- The patient's symptoms do not suggest a fistula, but rather a problem with sphincter control during increased abdominal pressure.
*Post-void residual volume*
- **Post-void residual volume (PVR)** measures the amount of urine left in the bladder after urination, primarily used to diagnose **overflow incontinence** or **urinary retention**.
- The patient's symptoms are inconsistent with overflow incontinence, which typically involves frequent dribbling or incomplete emptying rather than leakage specifically with physical exertion.
*Urodynamic testing*
- **Urodynamic testing** is a more comprehensive and invasive evaluation that includes cystometry, pressure-flow studies, and electromyography, often used to differentiate types of incontinence when the diagnosis is unclear.
- While it can diagnose stress incontinence, less invasive tests like the Q-tip test are typically preferred as a first step for **urethral hypermobility** before proceeding to complex urodynamic studies.
*Estrogen level*
- An **estrogen level** might be relevant if **atrophic vaginitis** or **urethritis** due to estrogen deficiency were suspected, which can contribute to urgency or mixed incontinence.
- While the patient is peri-menopausal, her primary symptoms (leakage with exertion) are more indicative of structural weakness (stress incontinence) rather than estrogen-related tissue atrophy or inflammation.
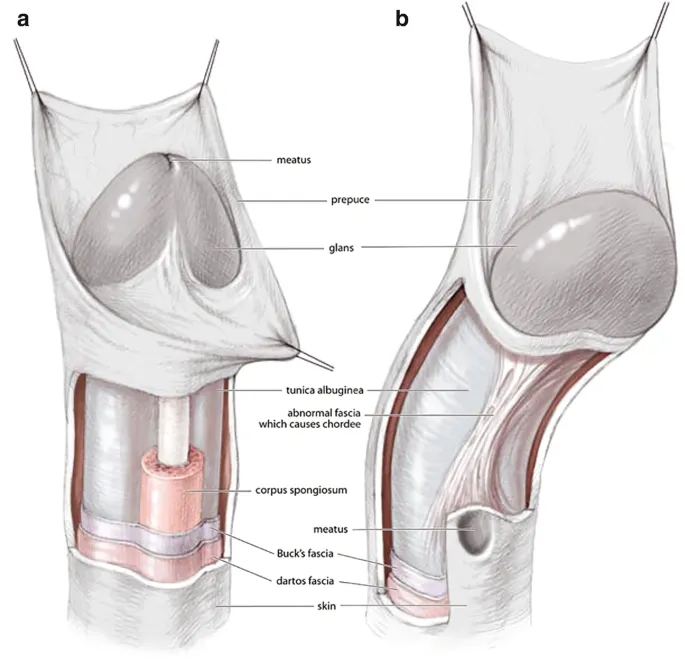
Genitourinary anomalies US Medical PG Question 4: A pregnant woman gives birth to her 1st child at the family farm. After delivery, the assisting midwife notices a triangular defect in the lower anterior abdominal wall of the baby. She clamps the umbilical cord with a cloth and urges the family to seek immediate medical care at the nearest hospital. Upon admission, the attending pediatrician further notices an open bladder plate with an exposed urethra, a low set umbilicus, an anteriorly displaced anus, and an inguinal hernia. No omphalocele is noted. The external genitalia is also affected. On physical exam, a shortened penis with a pronounced upward curvature and the urethral opening along the dorsal surface are also noted. What is the most likely diagnosis?
- A. Posterior urethral valves
- B. Bladder exstrophy (Correct Answer)
- C. Body stalk anomaly
- D. Cloacal exstrophy
- E. Urachal cyst
Genitourinary anomalies Explanation: ***Bladder exstrophy***
- The findings of a **triangular defect in the lower anterior abdominal wall**, an **open bladder plate with an exposed urethra**, a **low set umbilicus**, an **anteriorly displaced anus**, and affected external genitalia including a **shortened penis with pronounced upward curvature** (epispadias) are pathognomonic for **bladder exstrophy**.
- This condition results from a developmental failure of the infraumbilical abdominal wall and anterior bladder wall to close, leading to the bladder being open to the outside and often associated with epispadias due to abnormal tubercle development.
*Posterior urethral valves*
- This condition is characterized by **obstructive membranes within the posterior urethra of male infants**, leading to urinary obstruction and hydronephrosis.
- It does not involve an open bladder plate or abdominal wall defect, and the external genitalia are typically normal save for potential complications of urinary outflow obstruction.
*Body stalk anomaly*
- This is a severe congenital malformation characterized by **defects of the abdominal wall, thorax, and limbs**, with the fetus usually attached to the placenta by a short, thick umbilical cord.
- While it involves abdominal wall defects, it does not typically present with an exposed bladder plate and exposed urethra as the primary defect, nor is it specifically associated with epispadias.
*Cloacal exstrophy*
- Cloacal exstrophy is a more severe and complex defect than bladder exstrophy, involving the **exstrophy of both the bladder and a portion of the hindgut (intestine)**, often with omphalocele.
- The absence of an **omphalocele** and the specific description of an **open bladder plate** without obvious intestinal exposure make bladder exstrophy a more likely diagnosis.
*Urachal cyst*
- An urachal cyst is a **remnant of the allantois** that persists as a cystic structure between the bladder and the umbilicus, often presenting as a palpable mass or a discharge from the umbilicus.
- It does not involve an open abdominal wall defect, exposed bladder, or epispadias, which are central to the patient's presentation.
Genitourinary anomalies US Medical PG Question 5: A 27-year-old female in her 20th week of pregnancy presents for a routine fetal ultrasound screening. An abnormality of the right fetal kidney is detected. It is determined that the right ureteropelvic junction has failed to recanalize. Which of the following findings is most likely to be seen on fetal ultrasound:
- A. Renal cysts
- B. Duplicated ureter
- C. Bilateral renal agenesis
- D. Pelvic kidney
- E. Unilateral hydronephrosis (Correct Answer)
Genitourinary anomalies Explanation: ***Unilateral hydronephrosis***
- Failure of the **ureteropelvic junction (UPJ)** to recanalize leads to an obstruction of urine flow from the **renal pelvis** into the ureter.
- This obstruction causes a buildup of urine in the renal pelvis and calyces, a condition known as **hydronephrosis**, which will be unilateral as only the right kidney is affected.
*Renal cysts*
- **Renal cysts** are typically associated with conditions like polycystic kidney disease or multicystic dysplastic kidney, which involve abnormal development of renal parenchyma, not specifically a UPJ obstruction.
- While hydronephrosis can sometimes lead to cystic changes if severe and prolonged, in the initial stages of a UPJ obstruction detected on fetal ultrasound, **hydronephrosis** itself is the primary and most likely finding.
*Duplicated ureter*
- A **duplicated ureter** is a distinct congenital anomaly involving the formation of two ureters draining a single kidney or separate renal moieties.
- It does not directly result from the failure of **ureteropelvic junction recanalization**.
*Bilateral renal agenesis*
- **Bilateral renal agenesis** means both kidneys failed to develop, which would lead to severe oligohydramnios and is incompatible with sustained fetal life.
- The question describes an abnormality only in the **right kidney**, making bilateral agenesis incorrect.
*Pelvic kidney*
- A **pelvic kidney** (renal ectopia) occurs when the kidney fails to ascend from the pelvis to its normal lumbar position.
- This is a positional anomaly and is not directly caused by a failure of **ureteropelvic junction recanalization**.
Genitourinary anomalies US Medical PG Question 6: A 16-year-old girl is brought to the physician because she has not yet reached menarche. There is no personal or family history of serious illness. She is at the 20th percentile for weight and 50th percentile for height. Vital signs are within normal limits. Examination shows mild facial hair. There is no glandular breast tissue. Pubic hair is coarse and curly and extends to the inner surface of both thighs. Pelvic examination shows clitoromegaly. Ultrasound shows an absence of the uterus and ovaries. Which of the following is the most likely underlying cause for this patient's symptoms?
- A. 5-α reductase deficiency (Correct Answer)
- B. Complete androgen insensitivity
- C. 21-hydroxylase deficiency
- D. Sex chromosome monosomy
- E. Aromatase deficiency
Genitourinary anomalies Explanation: ***5-α reductase deficiency***
- This condition presents with an **absence of uterus and ovaries** (indicating a male genotype, XY) and **clitoromegaly** due to testosterone conversion to dihydrotestosterone (DHT) being impaired, leading to a spectrum of undervirilization in XY individuals.
- The presence of **facial and coarse pubic hair** suggests some androgen effect, while the absence of breast tissue and primary amenorrhea are consistent with an XY genotype and a lack of estrogenization from ovaries.
*Complete androgen insensitivity*
- In this condition, individuals are genotypically male (XY) but phenotypically female due to non-functional androgen receptors, leading to **breast development** and a **blind-ending vagina**, but no clitoromegaly or significant pubic/facial hair.
- The absence of a uterus and ovaries is consistent, but the presence of clitoromegaly and coarse hair along with lack of breast development contradicts this diagnosis.
*21-hydroxylase deficiency*
- This is a common cause of **congenital adrenal hyperplasia (CAH)**, leading to excess androgen production in genetically female (XX) individuals, causing **virilization**, clitoromegaly, and ambiguous genitalia.
- However, patients with 21-hydroxylase deficiency would have a **uterus and ovaries**, which are absent in this patient.
*Sex chromosome monosomy*
- This refers to **Turner syndrome (45, XO)**, where individuals are phenotypically female but typically present with **gonadal dysgenesis** (streak gonads), leading to primary amenorrhea and lack of secondary sexual characteristics like breast development.
- However, Turner syndrome patients do not usually exhibit **clitoromegaly** or significant facial/coarse pubic hair, and would have residual uterine tissue.
*Aromatase deficiency*
- This condition affects genetically female (XX) individuals, impairing the conversion of androgens to estrogens, leading to **virilization** (e.g., clitoromegaly, facial hair) and primary amenorrhea due to lack of estrogen for breast development and uterine maturation.
- While it explains virilization and amenorrhea, the **absence of uterus and ovaries** in this patient rules out aromatase deficiency, as XX individuals would possess these organs.
Genitourinary anomalies US Medical PG Question 7: A 22-month-old girl is brought to the emergency department with a 24-hour history of fever, irritability, and poor feeding. The patient never experienced such an episode in the past. She met the normal developmental milestones, and her vaccination history is up-to-date. She takes no medications, currently. Her temperature is 38.9°C (102.0°F). An abdominal examination reveals general tenderness without organomegaly. The remainder of the physical examination shows no abnormalities. Laboratory studies show the following results:
Urine
Blood 1+
WBC 10–15/hpf
Bacteria Many
Nitrite Positive
Urine culture from a midstream collection reveals 100,000 CFU/mL of Escherichia coli. Which of the following interventions is the most appropriate next step in evaluation?
- A. No further testing
- B. Voiding cystourethrography
- C. Renal and bladder ultrasonography (Correct Answer)
- D. Intravenous pyelography
- E. Dimercaptosuccinic acid renal scan
Genitourinary anomalies Explanation: ***Renal and bladder ultrasonography***
- For a febrile infant or young child (2 to 24 months) with a first **culture-proven urinary tract infection (UTI)**, renal and bladder ultrasonography is the recommended imaging study.
- This imaging is crucial to evaluate for **anatomic abnormalities** of the kidneys and urinary tract that could predispose to recurrent infections or renal damage.
- Current AAP guidelines recommend ultrasound as the **initial imaging modality** to assess for conditions like vesicoureteral reflux (VUR), hydronephrosis, or obstructive uropathy.
*No further testing*
- This option is incorrect because a **febrile UTI** in a young child warrants imaging to rule out **underlying genitourinary abnormalities** that could predispose to recurrent infections or renal damage.
- Skipping further evaluation could miss conditions like **vesicoureteral reflux (VUR)** or obstructive uropathy.
*Voiding cystourethrography*
- **Voiding cystourethrography (VCUG)** was historically recommended for all young children after a first UTI but is now reserved for specific situations, such as **abnormal renal/bladder ultrasound findings** or recurrent UTIs.
- VCUG involves radiation exposure and catheterization, making it less favorable as a first-line imaging study.
*Intravenous pyelography*
- **Intravenous pyelography (IVP)** involves intravenous contrast and radiation, making it an **invasive and high-radiation study** that has largely been replaced by ultrasound and CT for evaluating the urinary tract.
- It is not recommended as the initial imaging of choice for a child with a first UTI due to its **risks and availability of safer alternatives**.
*Dimercaptosuccinic acid renal scan*
- A **dimercaptosuccinic acid (DMSA) renal scan** is primarily used to detect **renal scarring** and assesses differential renal function.
- While it can be useful in identifying long-term consequences of UTIs, it is not the primary imaging study for initial evaluation of **ureteral or bladder abnormalities** in a first febrile UTI.
Genitourinary anomalies US Medical PG Question 8: A 5-year-old male visits his pediatrician for a check-up. His height corresponds to the 99th percentile for his age, and pubic hair is present upon physical examination. Serum renin and potassium levels are high, as is 17-hydroxyprogesterone. Which of the following is likely deficient in this patient?
- A. 11ß-hydroxylase
- B. 21-hydroxylase (Correct Answer)
- C. Aromatase
- D. 5a-reductase
- E. 17a-hydroxylase
Genitourinary anomalies Explanation: ***21-hydroxylase***
- A deficiency in **21-hydroxylase** leads to the accumulation of **17-hydroxyprogesterone**, as conversion to 11-deoxycorticosterone and 11-deoxycortisol is blocked, which aligns with the high levels observed in the patient.
- The shunting of precursors towards **androgen synthesis** due to the block explains the **precocious puberty** (pubic hair, advanced height for age).
- **Mineralocorticoid deficiency** (low aldosterone) causes **salt-wasting** with sodium loss and potassium retention (hyperkalemia), which stimulates compensatory **renin elevation**, explaining the high renin and potassium levels.
*11ß-hydroxylase*
- A deficiency would cause an accumulation of **11-deoxycorticosterone** and **11-deoxycortisol**, not primarily 17-hydroxyprogesterone.
- This deficiency typically presents with **hypertension** and **virilization** due to elevated 11-deoxycorticosterone (has mineralocorticoid activity) and androgens, but mineralocorticoid excess would **suppress renin**, which contradicts the high renin observed.
*Aromatase*
- **Aromatase** is responsible for converting androgens to estrogens. Its deficiency in males would typically result in **tall stature** due to delayed epiphyseal fusion but would not cause precocious puberty or the specific hormonal imbalance seen (high 17-hydroxyprogesterone, high renin/potassium).
- The absence of estrogen conversion would lead to **continued growth** and delayed bone maturation rather than early virilization with adrenal androgen excess.
*5a-reductase*
- **5a-reductase** converts testosterone to the more potent dihydrotestosterone (DHT). A deficiency in males would cause **undervirilization** at birth (ambiguous genitalia) and incomplete masculinization at puberty.
- This scenario contradicts the observed signs of **precocious puberty** and virilization in a 5-year-old male.
*17a-hydroxylase*
- A **17a-hydroxylase deficiency** would block the synthesis of cortisol and sex steroids, leading to increased production of mineralocorticoids like **corticosterone** and **11-deoxycorticosterone**.
- This typically results in **hypertension**, **hypokalemia** (mineralocorticoid excess), and **absent or delayed puberty** (lack of sex steroids), which are contrary to the symptoms presented in this patient (high potassium, precocious puberty).
Genitourinary anomalies US Medical PG Question 9: A 1-week-old baby is brought to the pediatrician’s office for a routine checkup. On examination, she is observed to have microcephaly with a prominent occiput. She also has clenched fists and rocker-bottom feet with prominent calcanei. A cardiac murmur is evident on auscultation. Based on the clinical findings, a diagnosis of nondisjunction of chromosome 18 is suspected. The pediatrician orders a karyotype for confirmation. He goes on to explain to the mother that her child will face severe growth difficulties. Even if her daughter progresses beyond a few months, she will not be able to reach developmental milestones at the appropriate age. In addition to the above, which of the following is most likely a consequence of this genetic disturbance?
- A. Supravalvular aortic stenosis
- B. Alzheimer’s disease
- C. Macroglossia
- D. Cutis aplasia
- E. Death within the first year of life (Correct Answer)
Genitourinary anomalies Explanation: ***Death within the first year of life***
- This patient has Trisomy 18, also known as Edwards syndrome, which is characterized by a high mortality rate, with **90-95% of affected infants dying within the first year** due to severe congenital anomalies, especially cardiac defects.
- **Rocker-bottom feet**, **clenched fists with overlapping fingers**, **microcephaly with a prominent occiput**, and **congenital heart defects** (such as ventricular septal defects or patent ductus arteriosus) are classic features of Trisomy 18.
*Cutis aplasia*
- **Cutis aplasia** (a congenital absence of skin) is a characteristic symptom of **Trisomy 13 (Patau syndrome)**, not Trisomy 18.
- While both are chromosomal abnormalities, their specific phenotypic presentations differ, making cutis aplasia less likely in this case.
*Macroglossia*
- **Macroglossia** (an enlarged tongue) is a common feature of **Down syndrome (Trisomy 21)**.
- It is not typically associated with Trisomy 18, which presents with distinct facial and oral features.
*Alzheimer’s disease*
- Individuals with **Down syndrome (Trisomy 21)** have an increased risk of developing **early-onset Alzheimer's disease**, often by middle age.
- This is due to the triplication of the **APP gene**, located on chromosome 21, which is involved in amyloid-beta plaque formation.
*Supravalvular aortic stenosis*
- **Supravalvular aortic stenosis** (narrowing of the aorta above the aortic valve) is a characteristic cardiac finding in **Williams syndrome**, a microdeletion syndrome involving chromosome 7.
- Williams syndrome is also associated with elfin facies, intellectual disability, and a friendly personality, none of which align with this patient's presentation.
Genitourinary anomalies US Medical PG Question 10: A 45-day-old male infant is brought to a pediatrician by his parents with concerns of poor feeding and excessive perspiration for one week. On physical examination, his temperature is 37.7°C (99.8°F), pulse rate is 190/min, and respiratory rate is 70/min. Mild cyanosis is present over the lips, and over the nail beds. Oxygen is provided and his oxygen saturation is carefully monitored. The pediatrician orders a bedside echocardiogram of the infant. It reveals a single arterial trunk arising from 2 normally formed ventricles. The arterial trunk is separated from the ventricles by a single semilunar valve. There is a defect in the interventricular septum, and the arterial trunk overrides the defect. Which of the following congenital heart diseases can also present with similar clinical features?
- A. Infracardiac total anomalous pulmonary venous return
- B. Pulmonary atresia with intact ventricular septum
- C. Severe Ebstein anomaly
- D. Double-inlet ventricle with unobstructed pulmonary flow
- E. Transposition of the great arteries with ventricular septal defect and pulmonary stenosis (Correct Answer)
Genitourinary anomalies Explanation: ***Transposition of the great arteries with ventricular septal defect and pulmonary stenosis***
- The described echocardiogram findings point to **Truncus Arteriosus**, characterized by a single great artery overriding a **ventricular septal defect (VSD)** and severe **cyanosis**.
- **Transposition of the great arteries (TGA)** with a VSD and pulmonary stenosis also presents with profound cyanosis, heart failure symptoms (poor feeding, tachypnea, tachycardia), and can lead to similar **hemodynamic instability** due to mixing of oxygenated and deoxygenated blood and outflow tract obstruction.
*Infracardiac total anomalous pulmonary venous return*
- This condition involves all pulmonary veins draining into the systemic venous circulation below the diaphragm, often into the **portal vein** or **ductus venosus**.
- While it causes severe cyanosis and cardiopulmonary distress in infancy, the **echocardiogram findings** (single arterial trunk, VSD) are distinct from the typical features of infracardiac TAPVR, which would show abnormal pulmonary venous connection at the systemic level rather than a single great artery.
*Pulmonary atresia with intact ventricular septum*
- This involves a **complete obstruction of the pulmonary valve**, preventing blood flow from the right ventricle to the pulmonary artery, leading to severe cyanosis.
- However, the echocardiogram description of a **single arterial trunk overriding a VSD** is not consistent with pulmonary atresia with an intact ventricular septum.
*Severe Ebstein anomaly*
- This anomaly is characterized by apical displacement of the **tricuspid valve leaflets**, leading to severe tricuspid regurgitation and functional hypoplasia of the right ventricle.
- While it can cause cyanosis and heart failure, the echocardiogram findings of a single arterial trunk and overriding VSD are not typical of **Ebstein anomaly**.
*Double-inlet ventricle with unobstructed pulmonary flow*
- A double-inlet ventricle means both atria connect to a single functional ventricle, but with **unobstructed pulmonary flow**, there would likely be less severe cyanosis (or none) and more symptoms of **congestive heart failure** due to pulmonary overcirculation.
- This condition's echocardiogram findings are also distinct from the described single arterial trunk and overriding VSD, which are characteristic of **Truncus Arteriosus**.
More Genitourinary anomalies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.