Gastrointestinal malformations US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Gastrointestinal malformations. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Gastrointestinal malformations US Medical PG Question 1: A 42-year-old woman presents to the emergency department in active labor. She has had no prenatal care and is unsure of the gestational age. Labor progresses rapidly and spontaneous vaginal delivery of a baby boy occurs 3 hours after presentation. On initial exam, the child is 1.9 kg (4.2 lb) with a small head and jaw. A sac-like structure containing intestine, as can be seen in the picture, protrudes from the abdominal wall. What complication is closely associated with this presentation?
- A. Lack of abdominal wall muscles
- B. Dehydration and necrosis of bowel
- C. Duodenal atresia
- D. Twisting of the bowel around itself
- E. Cardiac defect (Correct Answer)
Gastrointestinal malformations Explanation: ***Cardiac defect***
- The presentation of a **sac-like structure containing intestine protruding from the abdominal wall** (suggesting an **omphalocele**) along with **microcephaly** (small head), **micrognathia** (small jaw), and **low birth weight** are classic features of **Patau syndrome (Trisomy 13)** or **Edwards syndrome (Trisomy 18)**.
- These chromosomal abnormalities are strongly associated with various significant anomalies, including severe **cardiac defects** (e.g., ventricular septal defects, patent ductus arteriosus, atrial septal defects), which occur in **>80% of cases**.
- **Omphalocele** itself is associated with cardiac anomalies in approximately **30-50% of cases**, making cardiac defects the most closely associated complication.
*Lack of abdominal wall muscles*
- This description is more indicative of **prune belly syndrome (Eagle-Barrett syndrome)**, characterized by absence or deficiency of abdominal wall musculature.
- With **gastroschisis**, there is also an abdominal wall defect, but the defect is typically lateral to the umbilicus and there is no protective sac covering the bowel.
*Dehydration and necrosis of bowel*
- This complication is more characteristic of **gastroschisis** due to the direct exposure of the unprotected bowel to amniotic fluid, leading to inflammation, thickening, and potential vascular compromise.
- In an **omphalocele**, the bowel is protected by a sac (containing peritoneum and amnion), significantly reducing the immediate risk of dehydration and necrosis unless the sac ruptures.
*Duodenal atresia*
- **Duodenal atresia** is strongly associated with **Down syndrome (Trisomy 21)**, characterized by a "double bubble" sign on imaging.
- While omphalocele can occasionally occur with Trisomy 21, the constellation of findings in this case (microcephaly, micrognathia, low birth weight) is more consistent with Trisomy 13 or 18 rather than Trisomy 21.
*Twisting of the bowel around itself*
- **Volvulus** refers to the twisting of a loop of intestine around its mesentery, which can lead to bowel obstruction and ischemia.
- While volvulus can occur with intestinal malrotation (which may be present with omphalocele), it is not the most closely associated **congenital** complication of the chromosomal syndrome suggested by this clinical presentation.
Gastrointestinal malformations US Medical PG Question 2: A new mother expresses her concerns because her 1-day-old newborn has been having feeding difficulties. The child vomits after every feeding and has had a continuous cough since shortly after birth. The mother denies any greenish coloration of the vomit and says that it is only composed of whitish milk that the baby just had. The child exhibits these coughing spells during the exam, at which time the physician notices the child’s skin becoming cyanotic. The mother states that the child was born vaginally with no complications, although her records show that she had polyhydramnios during her last ultrasound before the delivery. Which of the following is the most likely cause of the patient’s symptoms?
- A. Failure of recanalization of duodenum
- B. Obstruction due to failure of rotation of pancreatic tissue
- C. Hypertrophy of the pyloric sphincter
- D. Failure of neural crest cells to migrate into the myenteric plexus
- E. Defective formation of the esophagus with tracheoesophageal connection (Correct Answer)
Gastrointestinal malformations Explanation: ***Defective formation of the esophagus with tracheoesophageal connection***
- The combination of **feeding difficulties**, vomiting of **undigested milk**, **continuous coughing**, and **cyanosis** during coughing spells in a newborn strongly suggests a **tracheoesophageal fistula (TEF)**, often with **esophageal atresia**.
- **Polyhydramnios** during pregnancy is a classic prenatal sign due to the fetal inability to swallow amniotic fluid.
*Failure of recanalization of duodenum*
- This condition, known as **duodenal atresia**, typically presents with **bilious vomiting** if the obstruction is distal to the ampulla of Vater, or non-bilious if proximal, but typically does not cause continuous coughing or cyanosis during feeds.
- While it causes vomiting, it primarily affects digestion and nutrient absorption, and **polyhydramnios** can also be present due to impaired fetal swallowing.
*Obstruction due to failure of rotation of pancreatic tissue*
- This describes **annular pancreas**, where pancreatic tissue encircles the duodenum, causing obstruction and **vomiting** (often bilious).
- Like duodenal atresia, it doesn't explain the characteristic **coughing and cyanosis** with feeds seen in this case.
*Hypertrophy of the pyloric sphincter*
- **Pyloric stenosis** typically presents later (2-8 weeks of age) with **projectile non-bilious vomiting**, and an **olive-shaped mass** may be palpable in the abdomen.
- It does not cause coughing or cyanosis that correlates directly with feeding in a 1-day-old.
*Failure of neural crest cells to migrate into the myenteric plexus*
- This describes **Hirschsprung disease**, which primarily affects the colon and presents with symptoms of **intestinal obstruction** (e.g., abdominal distension, failure to pass meconium, bilious vomiting if severe).
- It is not associated with feeding difficulties, coughing, or cyanosis in the manner described.
Gastrointestinal malformations US Medical PG Question 3: A 5-week-old male infant is brought to the physician by his mother because of a 4-day history of recurrent nonbilious vomiting after feeding. He was born at 36 weeks' gestation via spontaneous vaginal delivery. Vital signs are within normal limits. Physical examination shows a 2-cm epigastric mass. Further diagnostic evaluation of this patient is most likely to show which of the following?
- A. Dilated colon segment on abdominal x-ray
- B. Elongated and thickened pylorus on abdominal ultrasound (Correct Answer)
- C. Double bubble sign on abdominal x-ray
- D. High serum 17-hydroxyprogesterone concentration
- E. Corkscrew sign on upper gastrointestinal contrast series
Gastrointestinal malformations Explanation: ***Elongated and thickened pylorus on abdominal ultrasound***
- The classic presentation of **hypertrophic pyloric stenosis** includes **nonbilious projectile vomiting** in an infant, often with an **epigastric olive-shaped mass**.
- **Abdominal ultrasound** is the diagnostic study of choice for pyloric stenosis and will reveal a **thickened and elongated pylorus**.
*Dilated colon segment on abdominal x-ray*
- This finding is more consistent with **Hirschsprung disease**, which typically presents with **constipation**, **abdominal distention**, and **failure to pass meconium**, not recurrent nonbilious vomiting.
- The clinical picture provided points away from a distal bowel obstruction.
*Double bubble sign on abdominal x-ray*
- The **double bubble sign** on an abdominal x-ray is characteristic of a **duodenal obstruction**, such as **duodenal atresia** or **annular pancreas**, and usually presents with **bilious vomiting** shortly after birth.
- The described vomiting is nonbilious, making this less likely.
*High serum 17-hydroxyprogesterone concentration*
- A high serum **17-hydroxyprogesterone** concentration is indicative of **congenital adrenal hyperplasia (CAH)**, which can present with **salt-wasting crises** and **vomiting** but typically involves **electrolyte abnormalities** and hormonal symptoms, not an epigastric mass.
- The nonbilious vomiting and palpable mass are not typical for CAH.
*Corkscrew sign on upper gastrointestinal contrast series*
- The **corkscrew sign** on an upper GI series is pathognomonic for **midgut volvulus**, which presents with **bilious vomiting**, **abdominal pain**, and signs of **peritonitis** or **sepsis**.
- The vomiting in this case is explicitly stated as nonbilious, ruling out malrotation with volvulus.
Gastrointestinal malformations US Medical PG Question 4: A 45-year-old woman comes to the office with a 2-week history of rectal bleeding that occurs every day with her bowel movements. She denies any pain during defecation. Apart from this, she does not have any other complaints. Her past medical history is insignificant except for 5 normal vaginal deliveries. Her vitals are a heart rate of 72/min, a respiratory rate of 15/min, a temperature of 36.7°C (98.1°F), and a blood pressure of 115/85 mm Hg. On rectovaginal examination, there is a palpable, non-tender, prolapsed mass that can be pushed back by the examiner's finger into the anal sphincter. What is the most likely diagnosis?
- A. Rectal ulcer
- B. Anal fissure
- C. Hemorrhoids (Correct Answer)
- D. Proctitis
- E. Anorectal fistula
Gastrointestinal malformations Explanation: ***Hemorrhoids***
- The presentation of **painless rectal bleeding** with bowel movements and a **palpable, prolapsed, reducible mass** is classic for hemorrhoids, especially common in multiparous women.
- The absence of pain and the ability to reduce the prolapsed mass are key differentiating features from other perianal conditions.
*Rectal ulcer*
- Rectal ulcers typically present with **painful defecation** and may cause blood in the stool, but are not usually associated with a reducible prolapsed mass.
- They are often associated with other inflammatory conditions or trauma, which are not described here.
*Anal fissure*
- Anal fissures are characterized by **severe pain during and after defecation** due to a tear in the anal canal lining, and the bleeding is usually bright red and minimal.
- The primary symptom is pain, which this patient explicitly denies.
*Proctitis*
- Proctitis involves **inflammation of the rectal lining**, leading to symptoms like tenesmus, urgency, and bloody or purulent discharge, often with abdominal pain.
- It does not typically present with a palpable, prolapsed, reducible anal mass.
*Anorectal fistula*
- Anorectal fistulas are abnormal tracts between the anal canal or rectum and the perianal skin, usually causing **pain, swelling, and purulent discharge**.
- While bleeding can occur, the primary symptom is drainage, and they do not present as a reducible prolapsed mass.
Gastrointestinal malformations US Medical PG Question 5: A 3-week-old firstborn baby girl is brought to the pediatric emergency room with projectile vomiting. She started vomiting while feeding 12 hours ago and has been unable to keep anything down since then. After vomiting, she appears well and hungry, attempting to feed again. The vomitus has been non-bloody and non-bilious. The last wet diaper was 10 hours ago. The child was born at 40 weeks gestation to a healthy mother. On examination, the child appears sleepy but has a healthy cry during the exam. The child has dry mucous membranes and delayed capillary refill. There is a palpable olive-shaped epigastric mass on palpation. Which of the following is the most likely cause of this patient's condition?
- A. Failure of neural crest cell migration into the rectum
- B. Telescoping of the small bowel into the large bowel
- C. Hypertrophic muscularis externa (Correct Answer)
- D. Patent tract between the trachea and esophagus
- E. Failure of duodenal lumen recanalization
Gastrointestinal malformations Explanation: ***Hypertrophic muscularis externa***
- The presented symptoms, including **projectile vomiting** in a 3-week-old, **non-bilious** emesis, post-vomiting **hunger**, and a **palpable olive-shaped mass** in the epigastrium, are classic signs of **pyloric stenosis**. This condition is caused by the **hypertrophy of the pyloric sphincter's muscularis externa**.
- Pyloric stenosis commonly presents between **2-8 weeks of age** and leads to an obstruction of gastric outflow, causing the characteristic vomiting and signs of dehydration like **dry mucous membranes** and **delayed capillary refill**.
*Failure of neural crest cell migration into the rectum*
- This describes **Hirschsprung disease**, which typically presents with **constipation**, **abdominal distension**, and a **failure to pass meconium** in the neonatal period.
- While it involves GI obstruction, its symptoms and location of obstruction are distinctly different from the projectile vomiting seen in this case.
*Telescoping of the small bowel into the large bowel*
- This is known as **intussusception**, which usually presents with **intermittent, colicky abdominal pain**, **"currant jelly" stools** (due to blood and mucus), and a sausage-shaped abdominal mass, typically in older infants (3 months to 3 years).
- The type of vomiting (often bilious) and stool characteristics are different from the patient's presentation.
*Patent tract between the trachea and esophagus*
- This describes a **tracheoesophageal fistula (TEF)**, often associated with esophageal atresia. Infants with TEF typically present with **choking, coughing, and cyanosis** during feeds, as well as aspiration, due to misdirection of fluid into the lungs.
- The symptoms are immediate and severe with initial feeds and do not typically involve progressive projectile vomiting after several weeks of life.
*Failure of duodenal lumen recanalization*
- This leads to **duodenal atresia**, which typically presents with **bilious vomiting** within the first 24-48 hours of life, and the classic "double bubble" sign on X-ray.
- The vomiting in this case is **non-bilious** and started later, which rules out duodenal atresia.
Gastrointestinal malformations US Medical PG Question 6: A 2-week-old boy has developed bilious vomiting. He was born via cesarean section at term. On physical exam, his pulse is 140, blood pressure is 80/50 mmHg, and respirations are 40/min. His abdomen appears distended and appears diffusely tender to palpation. Abdominal imaging is obtained (Figures A). Which of the following describes the mechanism that caused this child's disorder?
- A. Hypertrophy of the pylorus
- B. Abnormal rotation of the midgut (Correct Answer)
- C. Ischemia-reperfusion injury in premature neonate
- D. Partial absence of ganglion cells in large intestine
- E. Telescoping segment of bowel
Gastrointestinal malformations Explanation: ***Abnormal rotation of the midgut***
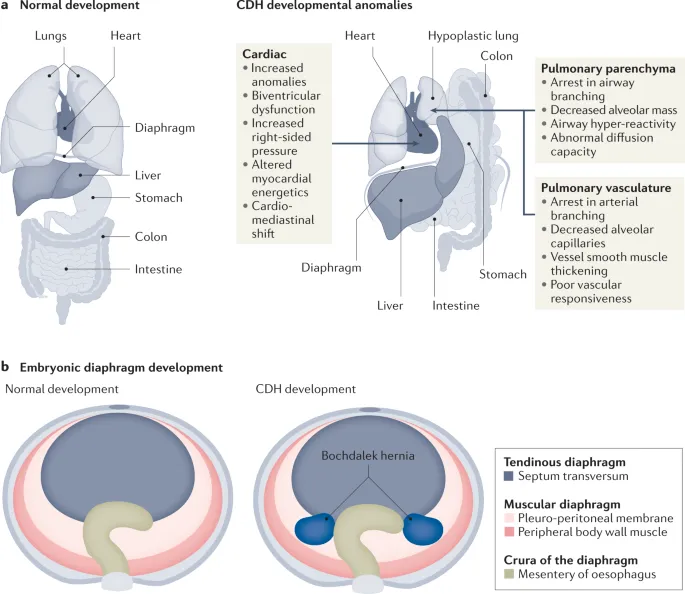
- The presentation of **bilious vomiting** in a neonate, along with abdominal distension and tenderness, is highly suggestive of a **malrotation with midgut volvulus**. This condition results from an incomplete or abnormal rotation of the fetal midgut during development, leading to an improperly fixed mesentery.
- The narrow mesenteric base, characteristic of malrotation, predisposes to twisting of the bowel around the superior mesenteric artery, causing **bowel obstruction and ischemia**. The provided image would likely show findings consistent with obstruction, such as dilated loops of bowel and possibly signs of compromised blood flow (e.g., pneumatosis intestinalis in severe cases, though not explicitly mentioned for this image).
*Hypertrophy of the pylorus*
- This condition is known as **pyloric stenosis** and typically presents with **non-bilious projectile vomiting** around 3-6 weeks of age, not bilious vomiting.
- While it causes gastric outlet obstruction, the vomiting is non-bilious because the obstruction is proximal to the entry of bile ducts into the duodenum.
*Ischemia-reperfusion injury in premature neonate*
- This mechanism is associated with **necrotizing enterocolitis (NEC)**, which primarily affects **premature neonates** and presents with abdominal distension, feeding intolerance, and bloody stools.
- The patient in the question is a **term neonate**, making NEC less likely, and the primary symptom is bilious vomiting rather than bloody stools.
*Partial absence of ganglion cells in large intestine*
- This describes **Hirschsprung disease**, which typically presents with **constipation**, abdominal distension, and failure to pass meconium, rather than acute bilious vomiting as the primary symptom in an infant.
- While it can cause bowel obstruction, the pathology involves the large intestine and often has a more chronic presentation of obstructive symptoms.
*Telescoping segment of bowel*
- This describes **intussusception**, which is characterized by sudden onset of **intermittent, crampy abdominal pain**, **vomiting (often bilious)**, and "currant jelly" stools.
- While intussusception can cause bilious vomiting and bowel obstruction, it typically occurs in infants aged 6 months to 3 years and is less common in a 2-week-old neonate where malrotation/volvulus is more prominent for acute obstructive symptoms.
Gastrointestinal malformations US Medical PG Question 7: A newborn boy born vaginally to a healthy 37-year-old G3P1 from a pregnancy complicated by hydramnios fails to pass meconium after 24 hours of life. The vital signs are within normal limits for his age. The abdomen is distended, the anus is patent, and the rectal examination reveals pale mucous with non-pigmented meconium. Based on a barium enema, the boy is diagnosed with sigmoid colonic atresia. Disruption of which structure during fetal development could lead to this anomaly?
- A. Inferior mesenteric artery (Correct Answer)
- B. Superior mesenteric artery
- C. Vitelline duct
- D. Cloaca
- E. Celiac artery
Gastrointestinal malformations Explanation: ***Inferior mesenteric artery***
- **Sigmoid colonic atresia**, as observed in this case, results from an ischemic event affecting the segment of the bowel supplied by the **inferior mesenteric artery** during fetal development.
- Interruption of blood flow to this region can lead to subsequent **atresia** as the affected part of the intestine necroses and is reabsorbed.
*Superior mesenteric artery*
- The **superior mesenteric artery** primarily supplies the midgut structures, including the small intestine and parts of the large intestine up to the transverse colon.
- Disruption of the superior mesenteric artery would typically lead to atresias higher up in the **gastrointestinal tract**, such as jejunal or ileal atresias, not sigmoid colonic atresia.
*Vitelline duct*
- The **vitelline duct** (also known as the omphalomesenteric duct) connects the midgut to the yolk sac during early fetal development.
- Persistent patency or partial obliteration of the vitelline duct can lead to anomalies like **Meckel's diverticulum** or vitelline cysts, which are distinct from colonic atresia.
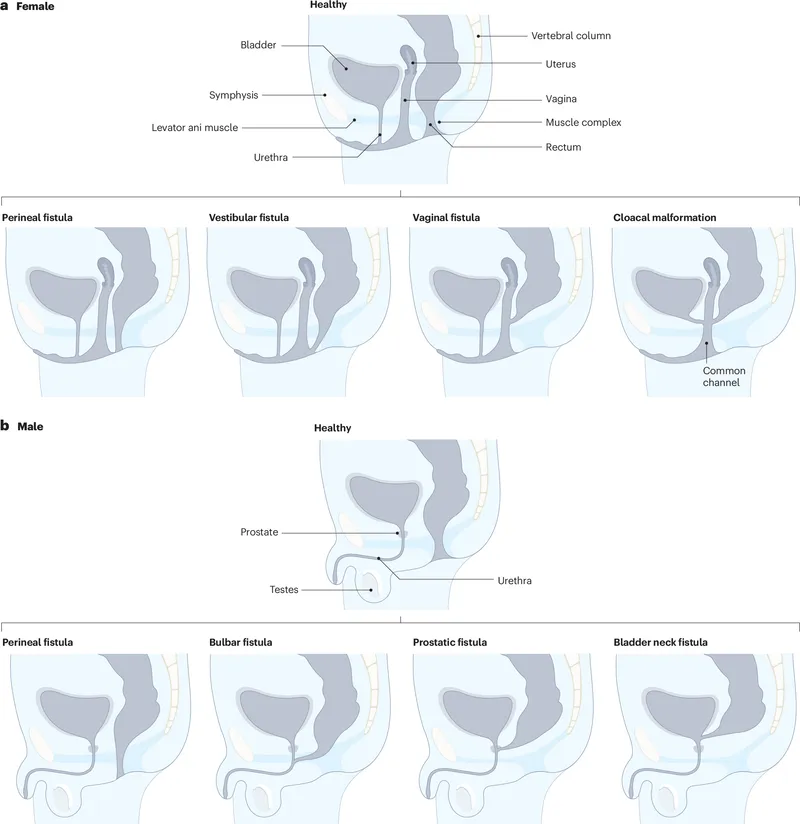
*Cloaca*
- The **cloaca** is a common cavity for the digestive, urinary, and reproductive tracts during early embryonic development.
- Defects in cloacal development lead to complex malformations involving these systems, such as **imperforate anus** or persistent cloaca, rather than isolated colonic atresia with a patent anus.
*Celiac artery*
- The **celiac artery** supplies the foregut structures, including the stomach, duodenum, liver, and spleen.
- Disruption of the celiac artery during fetal development would result in malformations of these upper gastrointestinal organs, not the sigmoid colon.
Gastrointestinal malformations US Medical PG Question 8: A 10-year-old boy is brought to a family physician by his mother with a history of recurrent headaches. The headaches are moderate-to-severe in intensity, unilateral, mostly affecting the left side, and pulsatile in nature. Past medical history is significant for mild intellectual disability and complex partial seizures that sometimes progress to secondary generalized seizures. He was adopted at the age of 7 days. His birth history and family history are not available. His developmental milestones were slightly delayed. There is no history of fever or head trauma. His vital signs are within normal limits. His height and weight are at the 67th and 54th percentile for his age. Physical examination reveals an area of bluish discoloration on his left eyelid and cheek. The rest of the examination is within normal limits. A computed tomography (CT) scan of his head is shown in the exhibit. Which of the following additional clinical findings is most likely to be present?
- A. Glaucoma (Correct Answer)
- B. Ash leaf spots
- C. Charcot-Bouchard aneurysm
- D. Café-au-lait spots
- E. Iris hamartoma
Gastrointestinal malformations Explanation: ***Glaucoma***
- The clinical presentation, including recurrent headaches, complex partial seizures, developmental delay, and a **bluish discoloration on the left eyelid and cheek (facial port-wine stain)**, along with the CT scan showing **cortical calcifications**, is highly suggestive of **Sturge-Weber syndrome**.
- **Glaucoma** is a common ocular manifestation of Sturge-Weber syndrome, particularly on the ipsilateral side of the facial port-wine stain, due to abnormal episcleral vasculature.
*Ash leaf spots*
- **Ash leaf spots** are hypopigmented macules characteristic of **Tuberous Sclerosis Complex**, which also manifests with seizures and intellectual disability but not typically with a facial port-wine stain or cortical calcifications in this pattern.
- While both Sturge-Weber and Tuberous Sclerosis are **neurocutaneous syndromes**, their specific diagnostic features differ.
*Charcot-Bouchard aneurysm*
- **Charcot-Bouchard aneurysms** are small aneurysms that occur in the brain's small penetrating arteries, typically associated with **chronic hypertension**, and can cause **intracerebral hemorrhage**.
- They are not related to the clinical picture of a facial port-wine stain, seizures, or developmental delay seen in this patient.
*Café-au-lait spots*
- **Café-au-lait spots** are hyperpigmented macules and are a hallmark feature of **Neurofibromatosis Type 1 (NF1)**, which is also associated with seizures and developmental delays.
- However, NF1 does not typically present with the facial port-wine stain or the specific cortical calcifications seen in Sturge-Weber syndrome.
*Iris hamartoma*
- **Iris hamartomas**, also known as **Lisch nodules**, are characteristic ocular findings in **Neurofibromatosis Type 1 (NF1)**.
- While NF1 can involve seizures and developmental delays, it does not present with a facial port-wine stain or the typical brain calcifications of Sturge-Weber syndrome.
Gastrointestinal malformations US Medical PG Question 9: A 26-year-old G1P0 mother is in the delivery room in labor. Her unborn fetus is known to have a patent urachus. Which of the following abnormalities would you expect to observe in the infant?
- A. Myelomeningocele
- B. Gastroschisis
- C. Urine discharge from umbilicus (Correct Answer)
- D. Omphalocele
- E. Meconium discharge from umbilicus
Gastrointestinal malformations Explanation: ***Urine discharge from umbilicus***
- A **patent urachus** is a congenital anomaly where the **urachus**, a remnant of the **allantois**, fails to close completely, allowing a direct connection between the bladder and the umbilicus.
- This patent tract results in the **continuous discharge of urine from the umbilicus**, especially upon crying or straining, as the bladder pressure increases.
*Myelomeningocele*
- **Myelomeningocele** is a severe form of **spina bifida** where the spinal cord and nerves protrude through an opening in the back.
- It results from incomplete closure of the neural tube and is not directly related to the urachus or umbilical discharge.
*Gastroschisis*
- **Gastroschisis** is a birth defect where the intestines protrude through an opening in the abdominal wall, typically to the right of the umbilicus.
- Unlike a patent urachus, it involves the protrusion of abdominal contents and is not associated with umbilical urine discharge.
*Omphalocele*
- An **omphalocele** is a birth defect in which parts of the abdominal organs, such as the intestines, liver, or stomach, protrude through the umbilical opening, covered by a sac.
- This condition is also an abdominal wall defect but distinct from a patent urachus, which specifically involves the connection between the bladder and the umbilicus.
*Meconium discharge from umbilicus*
- **Meconium discharge from the umbilicus** would suggest a persistent communication between the bowel and the umbilicus, rather than the bladder.
- This condition, known as a **patent vitelline duct** or omphalomesenteric duct, is anatomically distinct from a patent urachus.
Gastrointestinal malformations US Medical PG Question 10: A 4-year-old girl is brought to the emergency department by her parents with a sudden onset of breathlessness. She has been having similar episodes over the past few months with a progressive increase in frequency over the past week. They have noticed that the difficulty in breathing is more prominent during the day when she plays in the garden with her siblings. She gets better once she comes indoors. During the episodes, she complains of an inability to breathe and her parents say that she is gasping for breath. Sometimes they hear a noisy wheeze while she breathes. The breathlessness does not disrupt her sleep. On examination, she seems to be in distress with noticeable intercostal retractions. Auscultation reveals a slight expiratory wheeze. According to her history and physical findings, which of the following mechanisms is most likely responsible for this child’s difficulty in breathing?
- A. Defective chloride channel function leading to mucus plugging
- B. Chronic mucus plugging and inflammation leading to impaired mucociliary clearance
- C. Airway hyperreactivity to external allergens causing intermittent airway obstruction (Correct Answer)
- D. Inflammation leading to permanent dilation and destruction of alveoli
- E. Destruction of the elastic layers of bronchial walls leading to abnormal dilation
Gastrointestinal malformations Explanation: **Airway hyperreactivity to external allergens causing intermittent airway obstruction**
- The child's symptoms of **recurrent breathlessness** and **wheezing**, especially while playing in the garden (suggesting **allergen exposure**), and subsequent improvement indoors, are highly indicative of **allergen-induced bronchoconstriction**.
- The history points to **intermittent airway obstruction** triggered by environmental factors, characteristic of conditions like **asthma** where airways are hyperresponsive to triggers.
*Defective chloride channel function leading to mucus plugging*
- This mechanism is characteristic of **cystic fibrosis**, which typically presents with chronic respiratory issues, recurrent infections, and growth failure, not the acute, intermittent, and allergen-triggered episodes described.
- While mucus plugging can occur, it's a chronic process in cystic fibrosis and doesn't align with the acute, reversible nature and specific triggers mentioned in the case.
*Chronic mucus plugging and inflammation leading to impaired mucociliary clearance*
- This describes conditions like **bronchiectasis** or chronic bronchitis, which involve persistent cough, sputum production, and recurrent infections, rather than acute episodic wheezing based on allergen exposure.
- Impaired mucociliary clearance would lead to more continuous respiratory issues, not the relief experienced upon coming indoors.
*Inflammation leading to permanent dilation and destruction of alveoli*
- This mechanism is characteristic of **emphysema**, a condition primarily seen in adults, typically due to smoking, and presenting with chronic shortness of breath and airflow limitation, rather than episodic, allergen-triggered wheezing in a child.
- Emphysema involves alveolar damage, not primarily bronchial obstruction or hyperreactivity.
*Destruction of the elastic layers of bronchial walls leading to abnormal dilation*
- This describes **bronchiectasis**, which is characterized by permanent dilation of the bronchi, leading to chronic cough with sputum production and recurrent respiratory infections.
- The symptoms presented by the child are acute, reversible episodes of breathlessness and wheezing, not indicative of permanent structural damage to the bronchial walls.
More Gastrointestinal malformations US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.