Congenital heart defects US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Congenital heart defects. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Congenital heart defects US Medical PG Question 1: A 9-year-old boy is brought to the office due to exertional dyspnea and fatigability. He tires easily when walking or playing. His parents say that he was diagnosed with a congenital heart disease during his infancy, but they refused any treatment. They do not remember much about his diagnosis. The patient also had occasional respiratory infections throughout childhood that did not require hospitalization. He takes no medications. The patient has no family history of heart disease. His vital signs iclude: heart rate 98/min, respiratory rate 16/min, temperature 37.2°C (98.9°F), and blood pressure of 110/80 mm Hg. Physical examination shows toe cyanosis and clubbing but no finger abnormalities. Cardiac auscultation reveals a continuous machine-like murmur. All extremity pulses are full and equal. Which of the following is the most likely diagnosis?
- A. Tetralogy of Fallot
- B. Coarctation of the aorta
- C. Ventricular septal defect
- D. Atrial septal defect
- E. Patent ductus arteriosus (Correct Answer)
Congenital heart defects Explanation: ***Patent ductus arteriosus***
- A **patent ductus arteriosus (PDA)** can cause differential cyanosis and clubbing (lower extremities more affected than upper) due to preferential flow of deoxygenated blood through the PDA to the descending aorta.
- The classic **continuous machine-like murmur** auscultated in the precordium is highly characteristic of a PDA.
*Tetralogy of Fallot*
- Patients typically present with **cyanosis and clubbing of all four extremities** due to right-to-left shunting at the ventricular level, not isolated toe cyanosis.
- While it can cause exertional dyspnea, the murmur is typically a **systolic ejection murmur** from pulmonary stenosis, not a continuous machine-like murmur.
*Coarctation of the aorta*
- This condition presents with **differential blood pressures and pulses** between the upper and lower extremities, with elevated upper extremity pressures.
- It does not typically cause cyanosis or a continuous machine-like murmur.
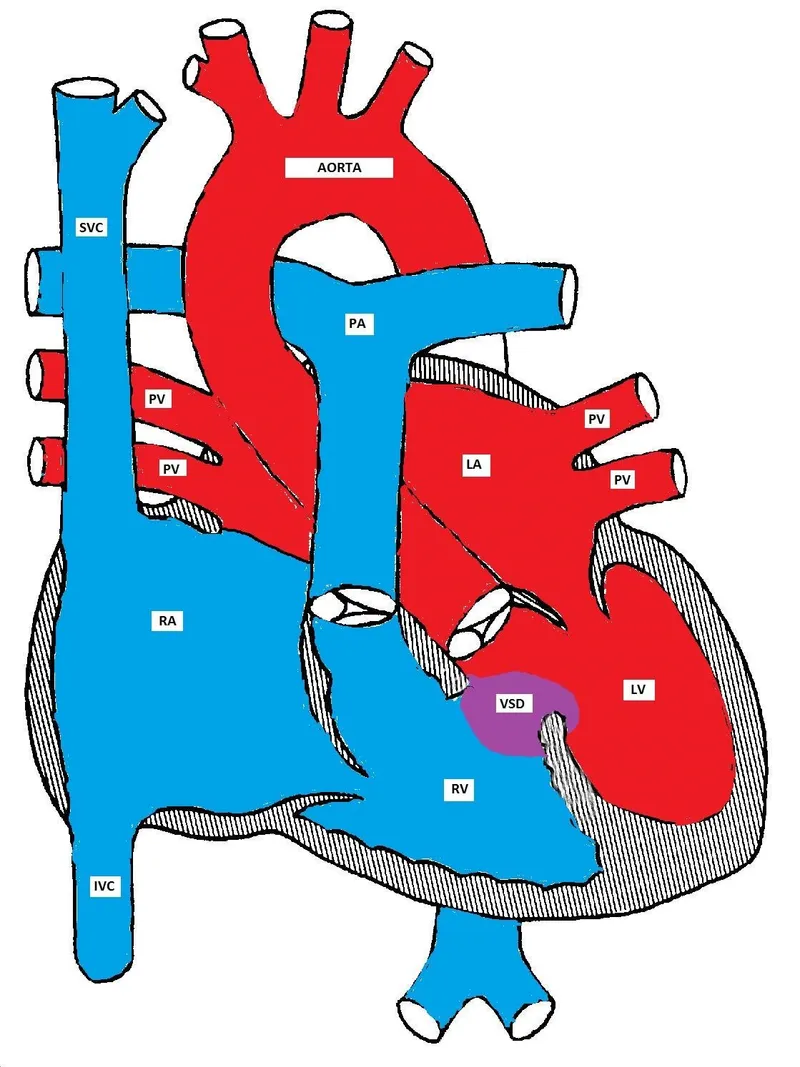
*Ventricular septal defect*
- A **ventricular septal defect (VSD)** typically causes a **holosystolic murmur** loudest at the lower left sternal border.
- Cyanosis develops late due to Eisenmenger syndrome, and if it occurs, it's typically central, affecting all extremities.
*Atrial septal defect*
- An **atrial septal defect (ASD)** usually presents with a **fixed split S2** and a **systolic ejection murmur** at the upper left sternal border due to increased flow across the pulmonic valve.
- Significant cyanosis is rare and occurs only in advanced stages with Eisenmenger syndrome, affecting all extremities if present.
Congenital heart defects US Medical PG Question 2: A 4-year-old male is brought into your office because his mother states he has been fatigued. He has not been acting like himself and has been getting tired easily while running around and playing with other children. As of last week, he has also been complaining of being short of breath. His vitals are temperature 98.6 deg F (37.2 deg C), blood pressure 100/75 mmHg, pulse 98/min, and respirations 22/min. On exam, the patient is short of breath, and there is a holosystolic murmur with an appreciable thrill along the left sternal border. There are no other noticeable abnormalities, and the mother states that the child's prenatal course along with genetic testing was normal. What is the most likely diagnosis?
- A. Atrial septal defect (ASD)
- B. Endocardial cushion defect
- C. Ventricular septal defect (VSD) (Correct Answer)
- D. Patent ductus arteriosus (PDA)
- E. Tetralogy of Fallot
Congenital heart defects Explanation: ***Ventricular septal defect (VSD)***
- A **holosystolic murmur** at the **left sternal border** with an associated **thrill** is a classic finding for a VSD.
- The patient's fatigue and shortness of breath (evidencing activity intolerance) are signs of **left-to-right shunting** causing increased pulmonary blood flow and eventual heart failure.
*Atrial septal defect (ASD)*
- An ASD typically presents with a **systolic ejection murmur** at the upper left sternal border due to increased flow across the pulmonic valve, not a holosystolic murmur.
- While it can cause fatigue and dyspnea, a thrill is less common, and the murmur quality is distinct.
*Endocardial cushion defect*
- This defect involves the atrioventricular septum, often resulting in a **split S2** and a **holosystolic murmur** best heard at the lower left sternal border.
- However, it is strongly associated with **Down syndrome**, which is ruled out by the normal genetic testing.
*Patent ductus arteriosus (PDA)*
- PDA is characterized by a **continuous "machinery" murmur** best heard below the left clavicle, which is distinct from the holosystolic murmur described.
- The associated symptoms of fatigue and dyspnea can occur, but the murmur differentiates it.
*Tetralogy of Fallot*
- This condition presents with **cyanosis** and a **crescendo-decrescendo systolic ejection murmur** at the left sternal border, not a holosystolic murmur with a thrill.
- Patients often exhibit "tet spells" and **clubbing**, which are absent in this presentation.
Congenital heart defects US Medical PG Question 3: One day after doctors helped a 28-year-old primigravid woman deliver a 4700 g (10 lb 6 oz) boy, he has bluish discoloration of his lips and fingernails. Oxygen saturation on room air is 81%. Examination shows central cyanosis. A continuous machine-like murmur is heard over the left upper sternal border. A single S2 heart sound is present. Supplemental oxygen does not improve the cyanosis. Echocardiography shows the pulmonary artery arising from the posterior left ventricle and the aorta arising from the right ventricle with active blood flow between the right and left ventricles. Further evaluation of the mother is most likely to show which of the following?
- A. Prenatal lithium intake
- B. Elevated fasting blood glucose (Correct Answer)
- C. Prenatal alcohol use
- D. Positive rapid plasma reagin test
- E. Prenatal phenytoin intake
Congenital heart defects Explanation: ***Elevated fasting blood glucose***
- The infant's symptoms (cyanosis, continuous machine-like murmur, and transposition of the great arteries with a large ventricular septal defect) are characteristic of a **large for gestational age (LGA) infant** born to a mother with **poorly controlled diabetes**. Maternal diabetes is a significant risk factor for congenital heart defects, including **transposition of the great arteries (TGA)**, and often leads to macrosomia.
- The description of the **pulmonary artery arising from the posterior left ventricle** and the **aorta arising from the right ventricle** confirms **TGA**. The "active blood flow between the right and left ventricles" indicates a **ventricular septal defect (VSD)**, which allows some mixing of blood and survival in TGA.
*Prenatal lithium intake*
- **Lithium exposure** during pregnancy is associated with Ebstein anomaly, a congenital heart defect affecting the tricuspid valve, not TGA.
- The clinical presentation of **Ebstein anomaly** would include right-sided heart failure and tricuspid regurgitation, differing from this case.
*Prenatal alcohol use*
- **Fetal alcohol spectrum disorders** can cause various congenital anomalies, including ventricular septal defects, but TGA is not characteristically associated with alcohol exposure.
- The overall cluster of findings, including the **macrosomic infant** (10 lb 6 oz), points more strongly towards maternal diabetes.
*Positive rapid plasma reagin test*
- A **positive rapid plasma reagin (RPR) test** indicates syphilis, which can cause congenital syphilis in the newborn, leading to conditions like non-immune hydrops fetalis, hepatosplenomegaly, and bone abnormalities.
- **Congenital syphilis** does not typically manifest with isolated congenital heart defects like TGA, nor does it cause macrosomia.
*Prenatal phenytoin intake*
- **Phenytoin exposure** during pregnancy can lead to **fetal hydantoin syndrome**, characterized by specific facial features, intellectual disability, and digit abnormalities.
- While central nervous system and cardiac defects can occur, **TGA is not a classic feature** of fetal hydantoin syndrome, and the infant's macrosomia is also not associated with phenytoin.
Congenital heart defects US Medical PG Question 4: A newborn male is evaluated 30 minutes after birth. He was born at 38 weeks gestation to a 39-year-old gravida 3 via vaginal delivery. The pregnancy was complicated by gestational diabetes, and the patient’s mother received routine prenatal care. The family declined all prenatal testing, including an anatomy ultrasound. The patient’s two older siblings are both healthy. Upon delivery, the patient appeared well and had good respiratory effort. He was noted to have acrocyanosis, and his Apgar scores were 8 and 9 at one and five minutes of life, respectively. The patient’s birth weight is 3840 g (8 lb 7 oz). His temperature is 98.7°F (37.1°C), blood pressure is 66/37 mmHg, pulse is 142/min, and respirations are 34/min. On physical exam, the patient has low-set ears, upslanting palpebral fissures, and a hypoplastic fifth finger.
Which of the following is most likely to be found in this patient?
- A. Complete atrioventricular septal defect (Correct Answer)
- B. Bicuspid aortic valve
- C. Aortic root dilation
- D. Coarctation of the aorta
- E. Truncus arteriosus
Congenital heart defects Explanation: **Complete atrioventricular septal defect**
- The patient's presentation with **low-set ears**, **upslanting palpebral fissures**, and a **hypoplastic fifth finger**, combined with the mother's advanced maternal age, are classic features suggestive of **Down syndrome (Trisomy 21)**.
- **Complete atrioventricular septal defect (AVSD)** is the most common cardiac anomaly seen in individuals with Down syndrome, occurring in approximately 40-50% of cases.
*Bicuspid aortic valve*
- A **bicuspid aortic valve** is a common congenital heart defect but is not specifically associated with Down syndrome.
- It is more commonly seen in familial cases or associated with conditions like **Turner syndrome**, which presents differently.
*Aortic root dilation*
- **Aortic root dilation** is characteristic of connective tissue disorders such as **Marfan syndrome** or **Ehlers-Danlos syndrome**.
- These conditions have distinct phenotypic features not described in this patient.
*Coarctation of the aorta*
- **Coarctation of the aorta** is often associated with Turner syndrome, which affects females, or isolated cases.
- It presents with differences in blood pressure between the upper and lower extremities, a finding not noted here.
*Truncus arteriosus*
- **Truncus arteriosus** is a severe congenital heart defect typically associated with **DiGeorge syndrome (22q11.2 deletion syndrome)**.
- Patients with DiGeorge syndrome often present with specific facial dysmorphisms, hypocalcemia, and immunodeficiency, none of which are described.
Congenital heart defects US Medical PG Question 5: A male neonate is being examined by a pediatrician. His mother informs the doctor that she had a mild fever with rash, muscle pain, and swollen and tender lymph nodes during the second month of gestation. The boy was born at 39 weeks gestation via spontaneous vaginal delivery with no prenatal care. On physical examination, the neonate has normal vital signs. Retinal examination reveals the findings shown in the image. Which of the following congenital heart defects is most likely to be present in this neonate?
- A. Double outlet right ventricle
- B. Atrial septal defect
- C. Patent ductus arteriosus (Correct Answer)
- D. Ventricular septal defect
- E. Tetralogy of Fallot
Congenital heart defects Explanation: ***Patent ductus arteriosus***
- This neonate has **congenital rubella syndrome (CRS)** based on maternal symptoms during the first trimester (fever, rash, lymphadenopathy) and the characteristic **"salt and pepper" retinopathy** shown on retinal examination
- **PDA is the most common cardiac defect** associated with CRS, occurring in approximately 50-85% of affected infants
- Other cardiac manifestations of CRS include peripheral pulmonary artery stenosis, but PDA predominates
- The classic triad of CRS includes cardiac defects, ocular abnormalities (cataracts, glaucoma, retinopathy), and sensorineural deafness
*Double outlet right ventricle*
- This is a **conotruncal anomaly** typically presenting with cyanosis in the neonatal period
- Not associated with maternal rubella infection or congenital rubella syndrome
- Would present with abnormal ventricular anatomy and significant hemodynamic compromise
*Atrial septal defect*
- While ASD is a common congenital heart defect, it is **not characteristically associated with CRS**
- Much less frequently linked to maternal viral infections compared to PDA
- Often asymptomatic in the neonatal period and detected later in childhood
*Ventricular septal defect*
- VSD is less commonly associated with **congenital rubella syndrome** compared to PDA
- When present, typically manifests with a holosystolic murmur at the left lower sternal border
- Can occur with maternal infections but is not the predominant cardiac finding in CRS
*Tetralogy of Fallot*
- Consists of four anatomic abnormalities: VSD, pulmonary stenosis, overriding aorta, and right ventricular hypertrophy
- Presents with **cyanosis** ("tet spells") and is not specifically linked to maternal rubella infection
- Not part of the congenital rubella syndrome spectrum
Congenital heart defects US Medical PG Question 6: A 6-year-old boy is brought in for evaluation by his adopted mother due to trouble starting 1st grade. His teacher has reported that he has been having trouble focusing on tasks and has been acting out while in class. His family history is unknown as he was adopted 2 years ago. His temperature is 36.2°C (97.2°F), pulse is 80/min, respirations are 20/min, and blood pressure 110/70 mm Hg. Visual inspection of the boy's face shows a low set nasal bridge, a smooth philtrum, and small lower jaw. Which of the following findings would also likely be found on physical exam?
- A. Cataracts
- B. Congenital deafness
- C. Holosystolic murmur (Correct Answer)
- D. Limb hypoplasia
- E. Wide notched teeth
Congenital heart defects Explanation: **Holosystolic murmur**
- The child exhibits classic features of **fetal alcohol syndrome** (FAS), including the distinctive facial anomalies (low set nasal bridge, smooth philtrum, small lower jaw) and developmental/behavioral issues (trouble focusing, acting out).
- Up to 50% of children with FAS develop **congenital heart defects**, with **ventricular septal defects (VSDs)** being the most common, which are characterized by a **holosystolic murmur** at the lower left sternal border.
*Cataracts*
- **Cataracts** are not a typical feature of fetal alcohol syndrome but are often associated with congenital infections such as **rubella** or **cytomegalovirus**.
- While some genetic syndromes can include cataracts, they are not a primary finding for the constellation of symptoms observed here.
*Congenital deafness*
- **Congenital deafness** is not a hallmark of fetal alcohol syndrome; rather, it is commonly associated with congenital infections like **rubella**, **CMV**, or genetic syndromes such as **CHARGE syndrome**.
- Children with FAS may have hearing problems due to recurrent ear infections, but not typically congenital deafness.
*Limb hypoplasia*
- **Limb hypoplasia** is typically seen in conditions like **thalidomide embryopathy** or certain genetic syndromes, such as **Roberts syndrome**.
- While growth restriction is common in FAS, significant limb hypoplasia as described is not a characteristic feature.
*Wide notched teeth*
- **Wide notched teeth**, also known as **Hutchinson teeth**, are pathognomonic for **congenital syphilis**.
- This finding is unrelated to fetal alcohol syndrome, and the patient's other symptoms do not suggest congenital syphilis.
Congenital heart defects US Medical PG Question 7: A 1-day-old infant born at full term by uncomplicated spontaneous vaginal delivery is noted to have cyanosis of the oral mucosa. The baby otherwise appears comfortable. On examination, his respiratory rate is 40/min and pulse oximetry is 80%. His left thumb is displaced and hypoplastic. A right ventricular lift is palpated, S1 is normal, S2 is single, and a harsh 3/6 systolic ejection murmur is heard at the left upper sternal border. Chest X-ray is shown. Which of the following is the most likely diagnosis?
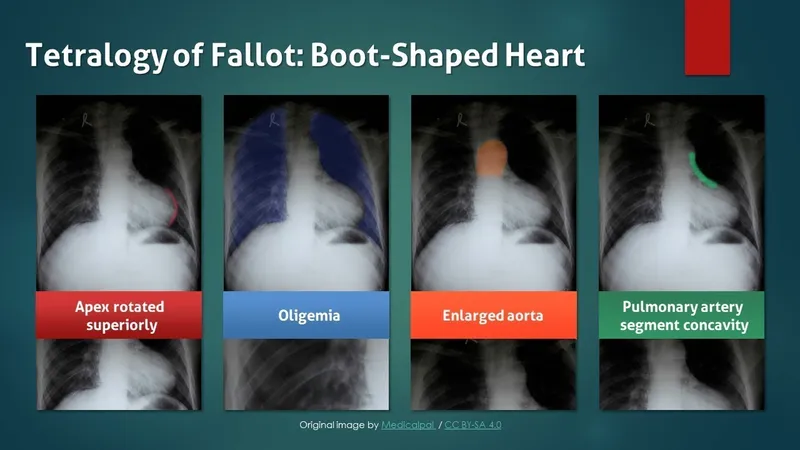
- A. Tetralogy of Fallot (Correct Answer)
- B. Ventricular septal defect
- C. Pneumothorax
- D. Transient tachypnoea of the newborn
- E. Transposition of great vessels
Congenital heart defects Explanation: ***Tetralogy of Fallot***
- The combination of **cyanosis**, a **right ventricular lift**, a harsh **systolic ejection murmur**, and **hypoplastic thumb** (suggesting **VACTERL association** or **TAR syndrome**) with an abnormal chest X-ray (likely showing an **upturned cardiac apex** or "boot-shaped" heart) strongly indicates Tetralogy of Fallot.
- The **single S2** is consistent with **pulmonary stenosis** or **pulmonary atresia**, and the low pulse oximetry (80%) highlights the cyanotic nature of this defect.
*Ventricular septal defect*
- While a VSD can cause a **systolic murmur** and a **right ventricular lift**, it typically presents with **acyanotic heart disease** until pulmonary hypertension develops much later.
- The severe **cyanosis** (80% SpO2) and **single S2** (implying pulmonary obstruction) are not typical features of an isolated VSD.
*Pneumothorax*
- A pneumothorax would present with **respiratory distress** (tachypnea, grunting), **diminished breath sounds** on the affected side, and potentially mediastinal shift, which are not described.
- It does not explain the presence of a **cardiac murmur**, the specific cyanosis patterns, or the associated limb abnormality.
*Transient tachypnoea of the newborn*
- This condition presents with **respiratory distress** and tachypnea, usually resolving within 24-48 hours.
- It does not involve **cyanosis to this degree**, a **cardiac murmur**, or a **hypoplastic thumb**.
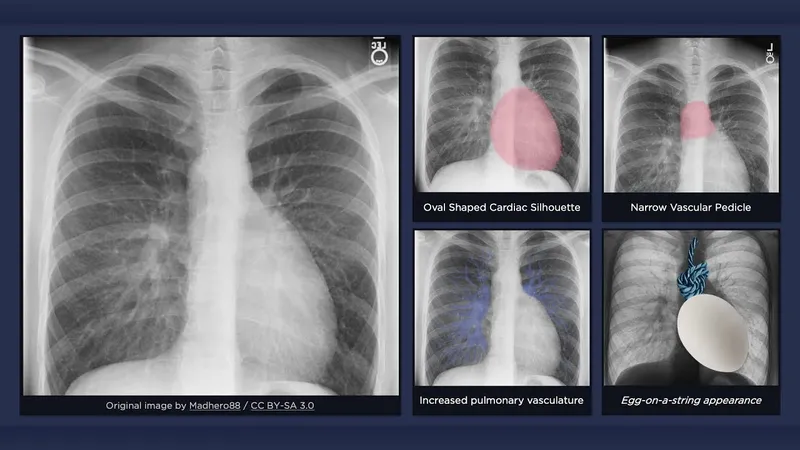
*Transposition of great vessels*
- While TGV presents with severe **cyanosis** and a single S2 (if restrictive VSD), it typically has a **quiet precordium** or a less prominent murmur unless associated with a large VSD, and severe cyanosis does not improve with O2.
- The description of a **harsh systolic ejection murmur** and the hypoplastic thumb are less specific for isolated TGV, and the chest X-ray typically shows a **"egg-on-a-string" appearance**, though not always in the immediate newborn period.
Congenital heart defects US Medical PG Question 8: A 5-month-old boy is brought to the emergency department by his mother because his lips turned blue for several minutes while playing earlier that evening. She reports that he has had similar episodes during feeding that resolved quickly. He was born at term following an uncomplicated pregnancy and delivery. He is at the 25th percentile for length and below the 5th percentile for weight. His temperature is 37°C (98.6°F), pulse is 130/min, blood pressure is 83/55 mm Hg, and respirations are 42/min. Pulse oximetry on room air shows an oxygen saturation of 90%. During the examination, he sits calmly in his mother's lap. He appears well. The patient begins to cry when examination of his throat is attempted; his lips and fingers begin to turn blue. Further evaluation of this patient is most likely to show which of the following?
- A. Pulmonary vascular congestion on x-ray of the chest
- B. Right axis deviation on ECG (Correct Answer)
- C. Anomalous pulmonary venous return on MR angiography
- D. Diminutive left ventricle on echocardiogram
- E. Machine-like hum on auscultation
Congenital heart defects Explanation: ***Right axis deviation on ECG***
- The presentation of **cyanotic spells** ("blue lips for several minutes", "lips and fingers begin to turn blue" with crying), **poor weight gain**, and **hypoxemia** (SpO2 90%) in an infant strongly suggests a **cyanotic congenital heart defect** like **Tetralogy of Fallot** (TOF).
- TOF is characterized by **right ventricular outflow tract obstruction**, leading to **right ventricular hypertrophy** and subsequently **right axis deviation** on ECG.
*Pulmonary vascular congestion on x-ray of the chest*
- **Pulmonary vascular congestion** is typically seen in conditions with **increased pulmonary blood flow** or **left-sided heart failure**, such as a large ventricular septal defect or patent ductus arteriosus.
- In Tetralogy of Fallot, there is often **decreased pulmonary blood flow** due to right ventricular outflow tract obstruction, leading to a **clear lung fields** on chest x-ray.
*Anomalous pulmonary venous return on MR angiography*
- **Total anomalous pulmonary venous return (TAPVR)** is a cyanotic heart defect where all pulmonary veins drain into the systemic circulation.
- While it causes cyanosis, it typically presents with **pulmonary congestion** and signs of **right heart strain**, which is less consistent with the spells described.
*Diminutive left ventricle on echocardiogram*
- A **diminutive left ventricle** is characteristic of **hypoplastic left heart syndrome**, which is a severe cyanotic defect.
- However, patients with hypoplastic left heart syndrome usually present with **severe heart failure** and shock much earlier in infancy, often in the neonatal period, which is not described here.
*Machine-like hum on auscultation*
- A **machine-like hum** is the classic auscultatory finding for a **patent ductus arteriosus (PDA)**.
- While a PDA can cause cyanosis if pulmonary hypertension is severe (Eisenmenger syndrome), isolated PDA typically presents with **left-to-right shunting** and **pulmonary overcirculation**, not the classic cyanotic spells seen with activities like crying, characteristic of TOF.
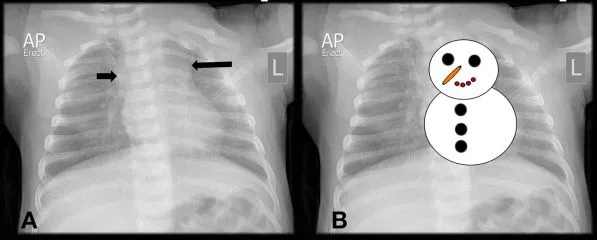
Congenital heart defects US Medical PG Question 9: A 1-day-old infant in the general care nursery, born at full term by uncomplicated cesarean section delivery, is noted to have a murmur, but otherwise appears well. On examination, respiratory rate is 40/min and pulse oximetry is 96%. Precordium is normoactive. With auscultation, S1 is normal, S2 is single, and a 2/6 systolic ejection murmur is heard at the left upper sternal border. Echocardiography shows infundibular pulmonary stenosis, overriding aorta, ventricular septal defect and concentric right ventricular hypertrophy. Which of the following correlate with the presence or absence of cyanosis in this baby?
- A. The degree of right ventricular outflow tract obstruction (Correct Answer)
- B. The ratio of reduced hemoglobin to oxyhemoglobin
- C. The concentration of hemoglobin
- D. The size of ventricular septal defect
- E. The concentration of pulmonary surfactant
Congenital heart defects Explanation: ***The degree of right ventricular outflow tract obstruction***
- The severity of **pulmonary stenosis** in **tetralogy of Fallot** dictates the amount of blood shunted from the right ventricle to the aorta via the **ventricular septal defect (VSD)**.
- A **less severe obstruction** allows more blood to flow to the lungs, leading to less right-to-left shunting and consequently **less cyanosis**.
*The ratio of reduced hemoglobin to oxyhemoglobin*
- While this ratio directly reflects the presence of cyanosis, it does not explain its *cause* in the context of the given congenital heart defect.
- The question asks what *correlates* with the presence or absence of cyanosis, implying a causal or pathophysiological link rather than a descriptive measure.
*The concentration of hemoglobin*
- **Hemoglobin concentration** affects the *visibility* of cyanosis (e.g., polycythemia can make mild desaturation appear more cyanotic), but it doesn't primarily determine the *presence* or *absence* of shunt-related cyanosis itself.
- A patient can be significantly desaturated with a normal hemoglobin concentration, and the degree of desaturation is largely driven by the shunt.
*The size of ventricular septal defect*
- In tetralogy of Fallot, the **VSD is typically large and non-restrictive**, meaning its size itself doesn't limit blood flow between the ventricles.
- The **pulmonary stenosis** is the primary determinant of the shunt direction and magnitude, not the size of the VSD.
*The concentration of pulmonary surfactant*
- **Pulmonary surfactant** is crucial for maintaining alveolar stability and preventing atelectasis, thereby ensuring efficient gas exchange in the lungs.
- While important for overall respiratory function, it does not directly correlate with the degree of shunting and cyanosis in **tetralogy of Fallot**.
Congenital heart defects US Medical PG Question 10: A 4-day-old male infant is brought to the physician because of respiratory distress and bluish discoloration of his lips and tongue. He was born at term and the antenatal period was uncomplicated. His temperature is 37.3°C (99.1°F), pulse is 170/min, respirations are 65/min, and blood pressure is 70/46 mm Hg. Pulse oximetry on room air shows an oxygen saturation of 82%. A grade 3/6 holosystolic murmur is heard over the left lower sternal border. A single S2 that does not split with respiration is present. Echocardiography shows defects in the interatrial and interventricular septae, as well as an imperforate muscular septum between the right atrium and right ventricle. Further evaluation of this patient is most likely to show which of the following?
- A. Elfin facies
- B. Tracheal bowing on chest x-ray
- C. Increased pulmonary vascular markings on chest x-ray
- D. Delta wave on electrocardiogram
- E. Left-axis deviation on electrocardiogram (Correct Answer)
Congenital heart defects Explanation: ***Left-axis deviation on electrocardiogram***
- The combination of **cyanosis**, a **holosystolic murmur**, and defects in the **interatrial and interventricular septa** along with an **imperforate tricuspid valve** (muscular septum between the right atrium and right ventricle) is highly suggestive of **tricuspid atresia** with a **ventricular septal defect (VSD)** and an **atrial septal defect (ASD)**.
- In tricuspid atresia, the **right ventricle is hypoplastic**, leading to LV dominance and a characteristic **left-axis deviation** on the ECG due to an enlarged left ventricle taking over the pumping action for the systemic and pulmonary circulation.
*Elfin facies*
- **Elfin facies** is a characteristic feature of **Williams syndrome**, which is associated with **supravalvular aortic stenosis** and not typically with cyanotic heart defects like tricuspid atresia.
- There is no clinical information in the vignette that suggests features of Williams syndrome.
*Tracheal bowing on chest x-ray*
- **Tracheal bowing or compression** is commonly seen in conditions like a **vascular ring** or **large mediastinal masses**, which can cause respiratory distress but generally do not present with the specific cardiac findings described.
- This finding is not characteristic of tricuspid atresia.
*Increased pulmonary vascular markings on chest x-ray*
- In tricuspid atresia, **pulmonary blood flow is often decreased** due to reduced flow to the right ventricle and pulmonary artery, especially if the VSD is restrictive or there's pulmonary stenosis. This would lead to **decreased, not increased, pulmonary vascular markings**.
- Increased pulmonary vascular markings suggest conditions with **left-to-right shunting** or **pulmonary venous congestion**, which is contradictory to the physiology of complicated tricuspid atresia.
*Delta wave on electrocardiogram*
- A **delta wave** on an ECG is characteristic of **Wolff-Parkinson-White (WPW) syndrome**, indicating a pre-excitation pathway.
- While WPW can occur with congenital heart disease, it is not a direct or expected consequence of tricuspid atresia and does not explain the cyanosis or specific cardiac defects mentioned.
More Congenital heart defects US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.