Pediatric oncology treatment principles US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pediatric oncology treatment principles. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Pediatric oncology treatment principles US Medical PG Question 1: A 25-year-old college student is diagnosed with acute myelogenous leukemia after presenting with a 3-week history of fever, malaise, and fatigue. He has a history of type 1 diabetes mellitus, multiple middle ear infections as a child, and infectious mononucleosis in high school. He currently smokes 1 pack of cigarettes per day, drinks a glass of wine per day, and denies any illicit drug use. The vital signs include: temperature 36.7°C (98.0°F), blood pressure 126/74 mm Hg, heart rate 87/min, and respiratory rate 17/min. On physical examination, his pulses are bounding; his complexion is pale, but breath sounds remain clear. A rapidly progressive form of leukemia is identified, and the patient is scheduled to start intravenous chemotherapy. Which of the following treatments should be given to this patient to prevent or decrease the likelihood of developing acute renal failure during treatment?
- A. Sulfinpyrazone
- B. Indomethacin
- C. Probenecid
- D. Colchicine
- E. Allopurinol (Correct Answer)
Pediatric oncology treatment principles Explanation: ***Allopurinol***
- **Allopurinol** inhibits **xanthine oxidase**, preventing the conversion of xanthine and hypoxanthine to uric acid.
- This is crucial in **tumor lysis syndrome** (TLS), a common complication of chemotherapy for rapidly proliferating cancers like AML, where massive cell death releases intracellular contents, including **purines**, which are metabolized to uric acid and can cause **acute renal failure**.
*Sulfinpyrazone*
- **Sulfinpyrazone** is a uricosuric agent, meaning it increases the excretion of uric acid in the urine.
- It is generally contraindicated in TLS because the increased uric acid load in the renal tubules can **aggravate crystal formation** and worsen renal damage, rather than prevent it.
*Indomethacin*
- **Indomethacin** is a non-steroidal anti-inflammatory drug (NSAID) primarily used for pain and inflammation management.
- While it can be used to treat the inflammation associated with **gouty arthritis**, it does not prevent the formation of uric acid during TLS and can even cause direct **renal toxicity**, which would be detrimental in a patient at risk of acute renal failure.
*Probenecid*
- **Probenecid** is another uricosuric agent, similar to sulfinpyrazone, that works by inhibiting the reabsorption of uric acid in the renal tubules.
- Like other uricosurics, it is generally **contraindicated in TLS** due to the risk of exacerbating uric acid nephropathy and acute renal failure by increasing uric acid concentrations in the kidneys.
*Colchicine*
- **Colchicine** is an anti-inflammatory drug mainly used for the treatment of **acute gout attacks** and familial Mediterranean fever.
- It does not lower serum uric acid levels and therefore offers no protection against the **hyperuricemia** and potential renal damage associated with tumor lysis syndrome.
Pediatric oncology treatment principles US Medical PG Question 2: An 18-year-old man comes to the physician with his parents for a routine health maintenance examination. He noticed a swelling on his back 7 months ago. He has a history of using intravenous heroin but has not used illicit drugs for the past 2 months. There is no personal or family history of serious illness. Vital signs are within normal limits. Examination shows a 2-cm soft, lobulated, mobile swelling on the right side of his upper back. The mass slips away from the fingers when its edges are palpated. Healed track marks are present in the bilateral cubital fossae. The patient is told that the mass on his back is most likely a lipoma, a benign mass consisting of fat tissue that does not require any further treatment. He is aware of the diagnosis and informs you that he wants it removed for cosmetic reasons. Four months ago, he had asked another physician to remove it but the physician refused to perform the procedure since he did not consider it necessary. The patient is counseled regarding the potential benefits and risks of the excision and that there is a chance of recurrence. His parents ask the physician not to perform the excision. However, the patient insists on undergoing the procedure. Which of the following is the most appropriate next step in management?
- A. Refer to the hospital ethics committee
- B. Ask the patient to follow up in 6 months
- C. Request parental consent
- D. Perform the excision (Correct Answer)
- E. Refer him to a methadone clinic
Pediatric oncology treatment principles Explanation: ***Perform the excision***
- An **18-year-old** is considered an adult and has the **autonomy** to make his own medical decisions, even if his parents disagree, especially for an elective procedure.
- The patient has been **counseled** on the risks and benefits, indicating informed consent, and his desire for removal is for valid cosmetic reasons despite being benign.
*Refer to the hospital ethics committee*
- An ethics committee review is generally reserved for **complex ethical dilemmas** without clear legal precedents or for disputes that cannot be resolved through standard communication.
- In this case, the patient's right to **autonomy** is straightforward, and the situation does not present unusual ethical challenges beyond a disagreement between an adult patient and his parents.
*Ask the patient to follow up in 6 months*
- This option disregards the patient's expressed desire for the procedure and his **autonomy** in making medical decisions.
- While the mass is benign and delaying treatment might be medically acceptable, it fails to address the patient's **cosmetic concern** and preference.
*Request parental consent*
- The patient is **18 years old**, making him a legal adult, and therefore, parental consent is **not legally required** for his medical treatment.
- Seeking parental consent despite the patient's age would undermine his **autonomy** and his legal right to make independent decisions.
*Refer him to a methadone clinic*
- While the patient has a history of intravenous heroin use, he states he has not used illicit drugs for 2 months, and his request is for a **non-opioid-related cosmetic procedure**.
- Referring him to a methadone clinic without him expressing a need or desire for substance abuse treatment is **inappropriate** and unrelated to his current chief concern.
Pediatric oncology treatment principles US Medical PG Question 3: A 60-year-old female presents to her primary care physician complaining of bloating and fatigue over the past year. On examination, she has abdominal distension and ascites. Abdominal imaging reveals a mass-like lesion affecting the left ovary. A biopsy of the lesion demonstrates serous cystadenocarcinoma. She is subsequently started on a chemotherapeutic medication known to stabilize polymerized microtubules. Which of the following complications should this patient be monitored for following initiation of this medication?
- A. Peripheral neuropathy (Correct Answer)
- B. Pulmonary fibrosis
- C. Acoustic nerve damage
- D. Hemorrhagic cystitis
- E. Cardiotoxicity
Pediatric oncology treatment principles Explanation: ***Peripheral neuropathy***
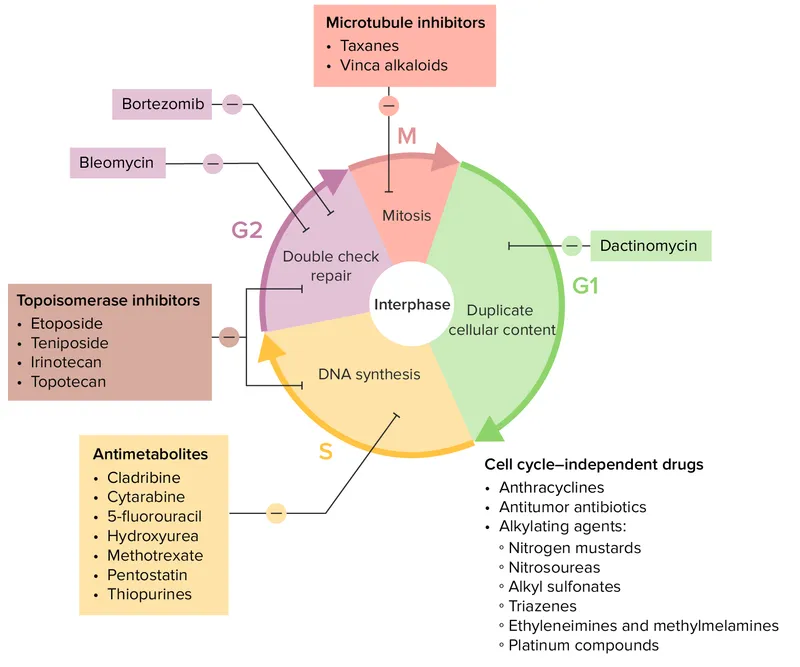
- The chemotherapeutic medication described, which stabilizes **polymerized microtubules**, is likely a **taxane** (e.g., paclitaxel, docetaxel), often used for ovarian cancer.
- Taxanes are well-known to cause **dose-dependent peripheral neuropathy** due to their effects on microtubule dynamics in neuronal axons.
*Pulmonary fibrosis*
- **Pulmonary fibrosis** is a significant side effect associated with certain chemotherapeutic agents like **bleomycin** or **busulfan**, but not typically with taxanes.
- Monitoring for this would involve assessing breath sounds, oxygen saturation, and potentially imaging for interstitial changes.
*Acoustic nerve damage*
- **Acoustic nerve damage** and ototoxicity are characteristic side effects of **platinum-based chemotherapy agents** (e.g., cisplatin), which are also used in ovarian cancer but have a different mechanism of action than microtubule stabilizers.
- This typically manifests as **tinnitus** or **hearing loss**.
*Hemorrhagic cystitis*
- **Hemorrhagic cystitis** is a common and severe side effect of **cyclophosphamide** and **ifosfamide**, alkylating agents, due to the accumulation of their metabolite **acrolein** in the bladder.
- It is not associated with microtubule-stabilizing agents like taxanes.
*Cardiotoxicity*
- **Cardiotoxicity**, including dilated cardiomyopathy, is a serious side effect primarily associated with **anthracyclines** (e.g., doxorubicin), which generate free radicals and damage cardiac myocytes.
- While some taxanes can cause cardiovascular effects, severe cardiotoxicity like that seen with anthracyclines is not their primary or most concerning side effect.
Pediatric oncology treatment principles US Medical PG Question 4: After hospitalization for urgent chemotherapy to treat Burkitt’s lymphoma, a 7-year-old boy developed paresthesias of the fingers, toes, and face. Vital signs are taken. When inflating the blood pressure cuff, the patient reports numbness and tingling of the fingers. His blood pressure is 100/65 mm Hg. Respirations are 28/min, pulse is 100/min, and temperature is 36.2℃ (97.2℉). He has excreted 20 mL of urine in the last 6 hours.
Laboratory studies show the following:
Hemoglobin 15 g/dL
Leukocyte count 6000/mm3 with a normal differential serum
K+ 6.5 mEq/L
Ca+ 6.6 mg/dL
Phosphorus 5.4 mg/dL
HCO3− 15 mEq/L
Uric acid 12 mg/dL
Urea nitrogen 54 mg/dL
Creatinine 3.4 mg/dL
Arterial blood gas analysis on room air:
pH 7.30
PCO2 30 mm Hg
O2 saturation 95%
Which of the following is the most likely cause of this patient’s renal condition?
- A. Direct tubular toxicity through filtered light chains
- B. Pigment-induced nephropathy
- C. Deposition of calcium phosphate in the kidney
- D. Intense renal vasoconstriction and volume depletion
- E. Precipitation of uric acid in renal tubules/tumor lysis syndrome (Correct Answer)
Pediatric oncology treatment principles Explanation: ***Precipitation of uric acid in renal tubules/tumor lysis syndrome***
- This patient's laboratory values, including **hyperkalemia** (K+ 6.5 mEq/L), **hyperphosphatemia** (Phosphorus 5.4 mg/dL), **hypocalcemia** (Ca+ 6.6 mg/dL), and **hyperuricemia** (Uric acid 12 mg/dL), are classic signs of **tumor lysis syndrome (TLS)**. TLS is caused by the rapid breakdown of tumor cells, commonly seen after chemotherapy for highly proliferative cancers like Burkitt's lymphoma.
- The elevated **uric acid** levels lead to the precipitation of uric acid crystals in the renal tubules, causing **acute kidney injury (AKI)**, as evidenced by the high creatinine (3.4 mg/dL) and oliguria (20 mL urine in 6 hours).
*Direct tubular toxicity through filtered light chains*
- This mechanism is characteristic of **myeloma kidney**, where light chains filtered by the glomeruli are directly toxic to the renal tubules, causing kidney damage.
- The patient's diagnosis of Burkitt's lymphoma and the rapid onset of symptoms after chemotherapy point away from light chain nephropathy.
*Pigment-induced nephropathy*
- This condition involves the precipitation of pigments like **myoglobin** (from rhabdomyolysis) or **hemoglobin** (from hemolysis) in the renal tubules, causing obstruction and kidney injury.
- While AKI is present, there is no evidence of rhabdomyolysis (e.g., elevated CK) or significant hemolysis to suggest pigment nephropathy.
*Deposition of calcium phosphate in the kidney*
- **Calcium phosphate deposition** can occur in conditions like **hypercalcemia** or sometimes in TLS due to the inverse relationship between calcium and phosphate; however, the primary driver for AKI in TLS is uric acid precipitation.
- Though **hypocalcemia** and **hyperphosphatemia** are present, the direct cause of renal failure in this scenario is driven by the significant hyperuricemia.
*Intense renal vasoconstriction and volume depletion*
- While **renal vasoconstriction** and **volume depletion** can lead to acute kidney injury (prerenal AKI) and are possible in a hospitalized patient, they do not explain the specific electrolyte abnormalities (hyperkalemia, hyperphosphatemia, hypocalcemia, hyperuricemia) seen in this case.
- The patient's blood pressure (100/65 mmHg) is not severely hypotensive, and while urine output is low, the comprehensive metabolic picture points more strongly to an intrinsic renal issue due to tumor lysis syndrome.
Pediatric oncology treatment principles US Medical PG Question 5: A 1-year-old boy is brought to the physician for a well-child examination. He has no history of serious illness. His older sister had an eye disease that required removal of one eye at the age of 3 years. Examination shows inward deviation of the right eye. Indirect ophthalmoscopy shows a white reflex in the right eye and a red reflex in the left eye. The patient is at increased risk for which of the following conditions?
- A. Gastric cancer
- B. Neuroblastoma
- C. Wilms tumor
- D. Basal cell carcinoma
- E. Osteosarcoma (Correct Answer)
Pediatric oncology treatment principles Explanation: ***Osteosarcoma***
- The presence of **retinoblastoma**, indicated by the **white reflex** (leukocoria) in the right eye and an older sibling with a history of enucleation for eye disease, suggests a heritable form of retinoblastoma.
- Patients with **heritable retinoblastoma** (especially those with germline mutations in the *RB1* tumor suppressor gene) are at significantly increased risk for developing other primary tumors, with **osteosarcoma** being the most common secondary malignancy.
*Gastric cancer*
- While gastric cancer is a serious malignancy, it is **not commonly associated** with germline *RB1* mutations or heritable retinoblastoma.
- There is no direct genetic link or epidemiological evidence supporting an increased risk of gastric cancer in retinoblastoma patients.
*Neuroblastoma*
- **Neuroblastoma** is a childhood cancer originating from neuroblasts, often presenting in the adrenal glands or sympathetic nervous system.
- It is **not typically linked** to retinoblastoma or *RB1* mutations; its genetic associations involve other genes such as MYCN amplification.
*Wilms tumor*
- **Wilms tumor**, a kidney cancer in children, is primarily associated with genetic conditions such as WAGR syndrome (Wilms tumor, aniridia, genitourinary anomalies, intellectual disability) involving the WT1 gene.
- It does **not have a direct genetic association** with retinoblastoma or the RB1 gene.
*Basal cell carcinoma*
- **Basal cell carcinoma** is the most common type of skin cancer, primarily caused by UV radiation exposure.
- It is **not a secondary malignancy commonly seen** in patients with heritable retinoblastoma. Such patients are more prone to sarcomas and other solid tumors.
Pediatric oncology treatment principles US Medical PG Question 6: A 5-year-old African-American boy is brought to the physician because of fatigue and night sweats for the past month. During this time, he has also lost 3 kg (6.6 lbs). Before the onset of symptoms, he had been healthy except for a febrile seizure as an infant. His brother had chickenpox 2 months ago. He is at the 75th percentile for height and 50th percentile for weight. He appears markedly fatigued. His temperature is 38°C (100.4°F), pulse is 95/min, respirations are 19/min, and blood pressure is 100/60 mm Hg. Lung and cardiac examination is normal. There are enlarged, nontender lymph nodes bilaterally in the neck. The abdomen is soft and nontender. A complete blood count shows:
Leukocyte count 8,000/mm³
Hemoglobin 9.1 g/dL
Hematocrit 26.9%
Platelet count 34,000/mm³
Serum
Na+ 135 mEq/L
K+ 4.5 mEq/L
Cl- 101 mEq/L
HCO3- 27 mEq/L
Urea nitrogen 9 mg/dL
Creatinine 0.7 mg/dL
Ca2+ 8.8 mg/dL
PCR testing demonstrates a 9:22 chromosomal translocation. The patient is diagnosed with Philadelphia chromosome-positive acute lymphoblastic leukemia. Which of the following is the most appropriate targeted therapy component?
- A. Cladribine
- B. Imatinib (Correct Answer)
- C. Hydroxyurea
- D. All-trans retinoic acid
- E. Transfuse platelets
Pediatric oncology treatment principles Explanation: ***Imatinib***
- The patient has **Philadelphia chromosome-positive acute lymphoblastic leukemia (Ph+ ALL)**, indicated by the **9:22 chromosomal translocation** (BCR-ABL fusion gene).
- **Imatinib** is a tyrosine kinase inhibitor (TKI) that specifically targets the **BCR-ABL fusion protein**, making it the most appropriate targeted therapy for Ph+ ALL.
*Cladribine*
- **Cladribine** is a purine analog primarily used in the treatment of **hairy cell leukemia** and some forms of lymphoma.
- It is not a targeted therapy for the **BCR-ABL fusion gene** in Ph+ ALL.
*Hydroxyurea*
- **Hydroxyurea** is a myelosuppressive agent used to rapidly lower high blood counts in conditions like **chronic myeloid leukemia (CML)** or **myeloproliferative neoplasms**.
- It does not target the specific genetic abnormality of Ph+ ALL.
*All-trans retinoic acid*
- **All-trans retinoic acid (ATRA)** is a form of vitamin A used in the treatment of **acute promyelocytic leukemia (APL)**.
- ATRA induces differentiation of promyelocytes and is not effective for Ph+ ALL.
*Transfuse platelets*
- While the patient has **thrombocytopenia** (platelet count 34,000/mm³), **platelet transfusion** is a supportive measure, not a targeted therapy for leukemia.
- It addresses a complication of the disease rather than the underlying oncogenic driver.
Pediatric oncology treatment principles US Medical PG Question 7: A 55-year-old male with a 60 pack-year smoking history presents to his oncologist for ongoing management of his recently diagnosed small cell lung cancer. His oncologist discusses several options and decides to start the chemotherapeutic medication, etoposide. The patient is warned that one side effect of this drug is myelosuppression so he should be vigilant for development of any infectious symptoms. The beneficial effect of this drug in treating cancer is most likely due to which of the following effects?
- A. DNA intercalation
- B. Crosslinking of DNA
- C. Stabilization of microtubules
- D. Alkylation of DNA
- E. Inhibition of supercoil relaxation (Correct Answer)
Pediatric oncology treatment principles Explanation: ***Inhibition of supercoil relaxation***
- **Etoposide** is a **topoisomerase II inhibitor**, preventing DNA uncoiling and replication, thus causing DNA strand breaks and **apoptosis** in rapidly dividing cancer cells.
- This mechanism specifically targets the enzyme responsible for managing the topological state of DNA, a crucial process during cell division.
*DNA intercalation*
- **DNA intercalation** involves drugs inserting themselves between the base pairs of DNA, distorting its structure and inhibiting replication and transcription (e.g., **doxorubicin**).
- This is not the primary mechanism of action for **etoposide**, which directly interferes with topoisomerase II enzymes.
*Crosslinking of DNA*
- **Crosslinking of DNA** involves forming covalent bonds within or between DNA strands, preventing DNA replication and transcription (e.g., **cisplatin**, **cyclophosphamide**).
- While effective in chemotherapy, this mechanism is characteristic of **alkylating agents** and is distinct from how etoposide operates.
*Stabilization of microtubules*
- **Stabilization of microtubules** (e.g., **paclitaxel**, **docetaxel**) or destabilization (e.g., **vincristine**, **vinblastine**) are mechanisms of **microtubule-targeting agents** that disrupt cell division.
- **Etoposide** does not primarily affect microtubules but rather targets **DNA topoisomerases**.
*Alkylation of DNA*
- **Alkylation of DNA** involves the addition of an alkyl group to DNA bases, leading to DNA damage, miscoding, and ultimately cell death.
- This mechanism is typical of **alkylating agents** like **cyclophosphamide** and **busulfan**, but it is not the primary mode of action for **etoposide**.
Pediatric oncology treatment principles US Medical PG Question 8: Two days after hospitalization for urgent chemotherapy to treat Burkitt’s lymphoma, a 7-year-old boy develops dyspnea and reduced urine output. He also feels a tingling sensation in his fingers and toes. Blood pressure is 100/65 mm Hg, respirations are 28/min, pulse is 100/min, and temperature is 36.2°C (97.2°F). The lungs are clear to auscultation. He has excreted 20 mL of urine in the last 6 hours. Laboratory studies show:
Hemoglobin 15 g/dL
Leukocyte count 6,000/mm3 with a normal differential serum
K+ 6.5 mEq/L
Ca+ 7.6 mg/dL
Phosphorus 5.4 mg/dL
HCO3− 15 mEq/L
Uric acid 12 mg/dL
Urea nitrogen 44 mg/dL
Creatinine 2.4 mg/dL
Arterial blood gas analysis on room air:
pH 7.30
PCO2 30 mm Hg
O2 saturation 95%
Which of the following is most likely to have prevented this patient’s condition?
- A. Ciprofloxacin
- B. Sodium bicarbonate
- C. No prevention would have been effective
- D. Pneumococcal polysaccharide vaccine
- E. Allopurinol (Correct Answer)
Pediatric oncology treatment principles Explanation: ***Allopurinol***
* This patient's presentation with **hyperkalemia**, **hyperphosphatemia**, **hypocalcemia**, **hyperuricemia**, and **acute kidney injury** (elevated BUN and creatinine, reduced urine output) shortly after chemotherapy for Burkitt's lymphoma is classic for **tumor lysis syndrome (TLS)**.
* **Allopurinol** prevents the formation of uric acid by inhibiting **xanthine oxidase**, thereby reducing the risk of **uric acid nephropathy** and mitigating TLS.
* *Ciprofloxacin*
* Ciprofloxacin is an **antibiotic** used to treat bacterial infections.
* It plays no direct role in preventing tumor lysis syndrome.
* *Sodium bicarbonate*
* While **sodium bicarbonate** can be used to **alkalinize the urine** to increase uric acid solubility, it is not a primary preventative measure for TLS.
* Its use can also exacerbate **hypocalcemia** by increasing ionized calcium binding to bicarbonate.
* *No prevention would have been effective*
* This statement is incorrect as tumor lysis syndrome is a well-known complication of chemotherapy for highly proliferative tumors, and preventative measures like **allopurinol** and **aggressive hydration** are cornerstone treatments.
* Prophylactic measures significantly reduce the incidence and severity of TLS.
* *Pneumococcal polysaccharide vaccine*
* The **pneumococcal polysaccharide vaccine** protects against infections caused by *Streptococcus pneumoniae*.
* It has no relevance to the prevention of tumor lysis syndrome.
Pediatric oncology treatment principles US Medical PG Question 9: A 7-year-old boy is brought to the physician because his parents are concerned about his early sexual development. He has no history of serious illness and takes no medications. His brother was diagnosed with testicular cancer 5 years ago and underwent a radical orchiectomy. The patient is at the 85th percentile for height and 70th percentile for weight. Examination shows greasy facial skin. There is coarse axillary hair. Pubic hair development is at Tanner stage 3 and testicular development is at Tanner stage 2. The remainder of the examination shows no abnormalities. An x-ray of the wrist shows a bone age of 10 years. Basal serum luteinizing hormone and follicle-stimulating hormone are elevated. An MRI of the brain shows no abnormalities. Which of the following is the most appropriate next step in management?
- A. Leuprolide therapy (Correct Answer)
- B. Testicular ultrasound
- C. Cortisol supplementation
- D. Radiation therapy
- E. Observation
Pediatric oncology treatment principles Explanation: ***Leuprolide therapy***
- This patient presents with **central precocious puberty** (CPP), indicated by elevated **basal LH and FSH levels** in the context of advanced bone age, Tanner stage 3 pubic hair, and Tanner stage 2 testicular development at a young age.
- **Leuprolide** is a GnRH analog that, when given continuously, downregulates the pituitary's GnRH receptors, suppressing gonadotropin release and halting pubertal progression. This is the appropriate treatment for CPP.
*Testicular ultrasound*
- While useful for evaluating testicular size and consistency, it is typically performed when there is suspicion of **peripheral precocious puberty** (e.g., Leydig cell tumor) with low LH/FSH or significant testicular asymmetry, which is not the primary presentation here.
- The elevated basal LH and FSH values indicate a **central origin** of puberty, making a testicular ultrasound less immediately relevant as a *next step* compared to directly addressing the central hormonal drive.
*Cortisol supplementation*
- This would be indicated for conditions causing **adrenal insufficiency**, such as **congenital adrenal hyperplasia (CAH)** with salt-wasting or Addison's disease.
- CAH typically presents with virilization and advanced bone age but would show **low LH/FSH** (due to peripheral androgen excess) and elevated adrenal androgens (e.g., DHEA-S, 17-hydroxyprogesterone), which are not described.
*Radiation therapy*
- This is a treatment for **malignant tumors**, often used in cases of brain tumors.
- The MRI of the brain showed **no abnormalities**, ruling out a pituitary or hypothalamic tumor as the cause of CPP in this case, thus making radiation therapy inappropriate.
*Observation*
- **Observation** alone is inappropriate given the significant **advancement of bone age** (10 years in a 7-year-old) and clear signs of central precocious puberty.
- Untreated CPP can lead to **compromised adult height potential** due to premature epiphyseal fusion and psychosocial issues, necessitating intervention.
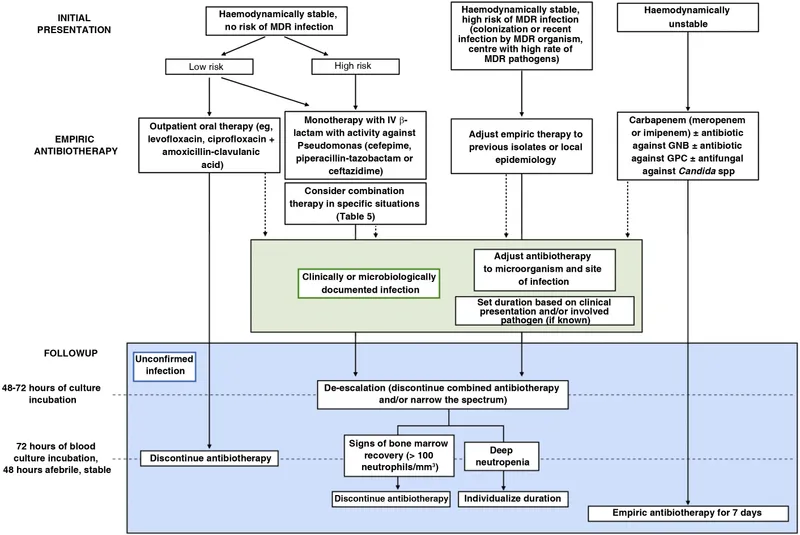
Pediatric oncology treatment principles US Medical PG Question 10: A 13-year-old male is admitted to the hospital for treatment of acute lymphoblastic leukemia. During his hospital course, he develops a fever of 39.0 degrees Celsius. A CBC demonstrates a leukocyte count of <500 /mm^3. Which of the following is the most appropriate initial management of this patient?
- A. Strict quarantine and hand-washing
- B. IV ceftazidime (Correct Answer)
- C. Oral ciprofloxacin and amoxicillin/clavulanic acid
- D. Granulocyte colony-stimulating factor (G-CSF)
- E. Oral doxycycline
Pediatric oncology treatment principles Explanation: ***IV ceftazidime***
- This patient presents with **febrile neutropenia** (fever with a leukocyte count of <500/mm³), a life-threatening condition in immunocompromised patients.
- **Empiric broad-spectrum intravenous antibiotics**, such as ceftazidime, are crucial to cover potential gram-negative and gram-positive bacterial infections, and should be initiated immediately.
*Strict quarantine and hand-washing*
- While **infection control measures** like hand-washing and isolation are important for preventing infections, they are **not sufficient as initial management** for febrile neutropenia.
- Febrile neutropenia requires **prompt empiric antibiotic treatment** to address existing infections, not just prevention.
*Oral ciprofloxacin and amoxicillin/clavulanic acid*
- **Oral antibiotics are generally insufficient** for initial management of febrile neutropenia, especially in a hospitalized patient with a severe presentation.
- Parenteral administration of broad-spectrum antibiotics is initially preferred for better bioavailability and rapid action against potentially life-threatening infections.
*Granulocyte colony-stimulating factor (G-CSF)*
- **G-CSF can be used to promote granulocyte recovery** in some cases of chemotherapy-induced neutropenia, but it is **not indicated for the initial management of active febrile neutropenia**.
- Its role is primarily supportive, to shorten the duration of neutropenia, not to treat presumed bacterial infections.
*Oral doxycycline*
- **Doxycycline has a limited spectrum** of activity and is not a broad-spectrum antibiotic appropriate for empiric treatment of febrile neutropenia.
- It would **not adequately cover common bacterial pathogens** seen in immunocompromised patients.
More Pediatric oncology treatment principles US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.