Neuroblastoma US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Neuroblastoma. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Neuroblastoma US Medical PG Question 1: A 3-year-old boy presents to the clinic for evaluation of leg pain. This has been persistent for the past 3 days and accompanied by difficulty walking. He has also had some erythema and ecchymoses in the periorbital region over the same time period. The vital signs are unremarkable. The physical exam notes the above findings, as well as some swelling of the upper part of the abdomen. The laboratory results are as follows:
Erythrocyte count 3.3 million/mm3
Leukocyte count 3,000/mm3
Neutrophils 54%
Eosinophils 1%
Basophils 1%
Lymphocytes 43%
Monocytes 3%
Platelet count 80,000/mm3
A magnetic resonance image (MRI) scan of the abdomen shows a mass of adrenal origin. Which of the following is the most likely cause of this patient's symptoms?
- A. Hepatoblastoma
- B. Rhabdomyosarcoma
- C. Neuroblastoma (Correct Answer)
- D. Wilms tumor
- E. Retinoblastoma
Neuroblastoma Explanation: ***Neuroblastoma***
- This diagnosis is strongly suggested by the combination of **an adrenal mass**, **periorbital ecchymoses** (often called "raccoon eyes" due to orbital metastases), and **bone pain/difficulty walking** (indicating bone marrow involvement).
- The **pancytopenia** (low erythrocyte, leukocyte, and platelet counts) further supports widespread bone marrow infiltration by metastatic disease, a common feature of advanced neuroblastoma.
*Hepatoblastoma*
- This is a primary **liver tumor** that typically presents with an abdominal mass and elevated alpha-fetoprotein.
- It does not typically cause periorbital ecchymoses or widespread bone pain/marrow suppression as seen in this patient.
*Rhabdomyosarcoma*
- This is a **soft tissue sarcoma** that can occur in various locations but does not commonly originate in the adrenal gland or present with the classic periorbital ecchymoses of neuroblastoma.
- While it can metastasize, the specific pattern of an adrenal mass with orbital and bone marrow involvement is less typical.
*Wilms tumor*
- This is a **kidney tumor** (nephroblastoma) that usually presents as a palpable abdominal mass and can sometimes cause hypertension or hematuria.
- It originates in the kidney, not the adrenal gland, and does not typically cause periorbital ecchymoses or widespread bone marrow metastasis leading to pancytopenia.
*Retinoblastoma*
- This is a **malignant tumor of the retina** in the eye, usually presenting with leukocoria (white pupillary reflex) or strabismus.
- It does not present with an adrenal mass, leg pain, or periorbital ecchymoses, although genetic predisposition can be associated with other cancers.
Neuroblastoma US Medical PG Question 2: A 1-year-old boy is brought to the physician for a well-child examination. He has no history of serious illness. His older sister had an eye disease that required removal of one eye at the age of 3 years. Examination shows inward deviation of the right eye. Indirect ophthalmoscopy shows a white reflex in the right eye and a red reflex in the left eye. The patient is at increased risk for which of the following conditions?
- A. Gastric cancer
- B. Neuroblastoma
- C. Wilms tumor
- D. Basal cell carcinoma
- E. Osteosarcoma (Correct Answer)
Neuroblastoma Explanation: ***Osteosarcoma***
- The presence of **retinoblastoma**, indicated by the **white reflex** (leukocoria) in the right eye and an older sibling with a history of enucleation for eye disease, suggests a heritable form of retinoblastoma.
- Patients with **heritable retinoblastoma** (especially those with germline mutations in the *RB1* tumor suppressor gene) are at significantly increased risk for developing other primary tumors, with **osteosarcoma** being the most common secondary malignancy.
*Gastric cancer*
- While gastric cancer is a serious malignancy, it is **not commonly associated** with germline *RB1* mutations or heritable retinoblastoma.
- There is no direct genetic link or epidemiological evidence supporting an increased risk of gastric cancer in retinoblastoma patients.
*Neuroblastoma*
- **Neuroblastoma** is a childhood cancer originating from neuroblasts, often presenting in the adrenal glands or sympathetic nervous system.
- It is **not typically linked** to retinoblastoma or *RB1* mutations; its genetic associations involve other genes such as MYCN amplification.
*Wilms tumor*
- **Wilms tumor**, a kidney cancer in children, is primarily associated with genetic conditions such as WAGR syndrome (Wilms tumor, aniridia, genitourinary anomalies, intellectual disability) involving the WT1 gene.
- It does **not have a direct genetic association** with retinoblastoma or the RB1 gene.
*Basal cell carcinoma*
- **Basal cell carcinoma** is the most common type of skin cancer, primarily caused by UV radiation exposure.
- It is **not a secondary malignancy commonly seen** in patients with heritable retinoblastoma. Such patients are more prone to sarcomas and other solid tumors.
Neuroblastoma US Medical PG Question 3: A 3-year-old girl is brought to the physician by her parents due to observations of rapid, random, horizontal and vertical eye movements along with occasional jerking movements of her limbs and head. CT scan reveals an abdominal mass that crosses the midline. Further work-up reveals elevated 24-hour urinary homovanillic acid and vanillylmandelic acid. Neuroblastoma is suspected. Which of the following diseases pathologically originates from the same type of cells as Neuroblastoma?
- A. Pilocytic astrocytoma
- B. Craniopharyngioma
- C. Medulloblastoma
- D. Hirschsprung disease (Correct Answer)
- E. Retinoblastoma
Neuroblastoma Explanation: ***Hirschsprung disease***
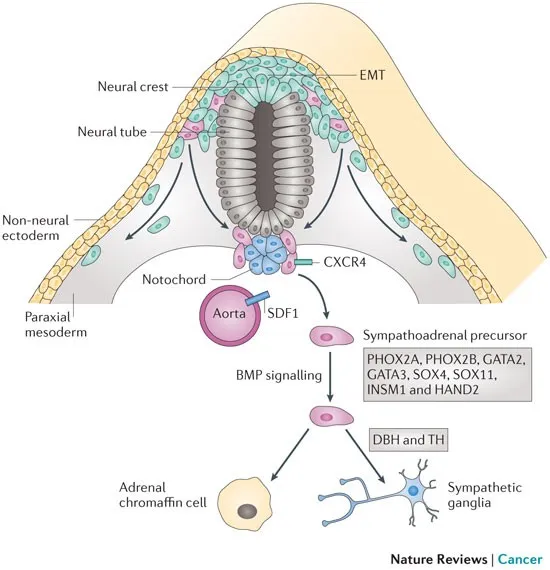
- Both **neuroblastoma** and **Hirschsprung disease** originate from neural crest cells. Neuroblastomas arise from the adrenal medulla or sympathetic ganglia, while Hirschsprung disease results from failed neural crest cell migration to the distal colon, leading to an **aganglionic segment**.
- The shared embryological origin from the **neural crest** explains their occasional coexistence or shared genetic predispositions.
*Pilocytic astrocytoma*
- This tumor originates from **astrocytes**, which are glial cells derived from the **neuroectoderm** (specifically the neural tube).
- It is distinct from the neural crest cells that give rise to neuroblastoma.
*Craniopharyngioma*
- This tumor is derived from remnants of **Rathke's pouch**, an embryonic invagination of the stomodeum (oral ectoderm).
- It is not related to neural crest cells.
*Medulloblastoma*
- This highly malignant brain tumor arises from primitive neuroectodermal cells in the **cerebellum**.
- While also part of the neuroectoderm, its specific origin is distinct from the neural crest cells that form neuroblastomas.
*Retinoblastoma*
- This pediatric eye cancer originates from immature **retinal cells** (retinoblasts), which are part of the **neuroectoderm** (specifically the optic vesicle).
- Its cellular origin is different from the neural crest lineage of neuroblastoma.
Neuroblastoma US Medical PG Question 4: A 5-year-old boy is brought to the physician because of early morning headaches for the past 6 months. During this period, he has had severe nausea and occasional episodes of vomiting. For the past month, he has had difficulty walking and intermittent double vision. He was born at term and has been healthy apart from an episode of sinusitis 8 months ago that resolved spontaneously. He is at the 60th percentile for height and 50th percentile for weight. His temperature is 37.1°C (98.8°F), pulse is 80/min, and blood pressure is 105/64 mm Hg. Examination shows normal muscle strength and 2+ deep tendon reflexes bilaterally. He has a broad-based gait and impaired tandem gait. Fundoscopy shows bilateral swelling of the optic disc. There is esotropia of the left eye. Which of the following is the most likely diagnosis?
- A. Schwannoma
- B. Optic glioma
- C. Meningioma
- D. Hemangioblastoma
- E. Medulloblastoma (Correct Answer)
Neuroblastoma Explanation: ***Medulloblastoma***
- The constellation of **early morning headaches**, **nausea/vomiting**, **papilledema** (swelling of the optic disc), **ataxia** (difficulty walking, broad-based gait, impaired tandem gait), and **cranial nerve palsy** (esotropia from abducens nerve dysfunction) in a young child strongly indicates increased intracranial pressure secondary to a posterior fossa tumor. **Medulloblastoma** is the most common malignant posterior fossa tumor in children.
- The location in the **cerebellum** explains the gait abnormalities (ataxia), and its rapid growth often leads to **hydrocephalus** and raised ICP symptoms.
*Schwannoma*
- **Schwannomas** typically arise from cranial nerves (most commonly the vestibular nerve, causing acoustic neuromas) and are rare in children.
- They tend to be **slow-growing** and usually present with localized symptoms like hearing loss or facial nerve weakness, rather than diffuse signs of increased ICP and ataxia.
*Optic glioma*
- **Optic gliomas** arise from the optic nerve and primarily cause **vision loss**, proptosis, and strabismus.
- While they can cause hydrocephalus if large and compressive, they typically do not cause pronounced cerebellar signs like ataxia, and primary presentation with early morning headaches and vomiting would be less common than vision issues.
*Meningioma*
- **Meningiomas** are typically **benign tumors** arising from the meninges that are rare in children and usually occur in older adults.
- They are slow-growing and often present with focal neurological deficits related to their location, but they are an improbable diagnosis given the age and constellation of rapidly developing symptoms of increased ICP and cerebellar dysfunction.
*Hemangioblastoma*
- **Hemangioblastomas** are vascular tumors, often associated with **von Hippel-Lindau disease**, and are typically found in the cerebellum, brainstem, or spinal cord.
- While they can cause cerebellar symptoms and increased ICP, they are more commonly seen in **adults** and are much rarer than medulloblastomas in children of this age.
Neuroblastoma US Medical PG Question 5: A 43-year-old woman presents to your clinic for the evaluation of an abnormal skin lesion on her forearm. The patient is worried because her mother passed away from melanoma. You believe that the lesion warrants biopsy for further evaluation for possible melanoma. Your patient is concerned about her risk for malignant disease. What is the most important prognostic factor of melanoma?
- A. Depth of invasion of atypical cells (Correct Answer)
- B. S-100 tumor marker present
- C. Evolution of lesion over time
- D. Age at presentation
- E. Level of irregularity of the borders
Neuroblastoma Explanation: ***Depth of invasion of atypical cells***
- The **Breslow depth**, which measures the vertical thickness of the melanoma from the granular layer of the epidermis to the deepest part of the tumor, is the **single most important prognostic factor** for localized melanoma.
- A greater depth of invasion correlates directly with a higher risk of **metastasis** and a poorer prognosis due to increased likelihood of reaching dermal lymphatics or blood vessels.
*S-100 tumor marker present*
- While **S-100 protein** is a marker expressed in melanoma cells and can be used to detect metastatic disease (e.g., in lymph nodes), its mere presence does not serve as the primary prognostic indicator for the primary lesion itself.
- S-100 reflects the presence of melanoma cells but does not provide information about the **depth or biological aggressiveness** of the initial tumor.
*Evolution of lesion over time*
- The **evolution or change** in a lesion (e.g., in size, shape, color, new symptoms) is a crucial diagnostic criterion for identifying suspicious lesions for biopsy.
- While important for diagnosis, it is not a direct prognostic factor once melanoma is confirmed; the **pathological features** after biopsy, particularly depth, determine prognosis.
*Age at presentation*
- **Age** can influence treatment decisions and overall health status, but it is not the most important independent prognostic factor for melanoma.
- Prognosis is primarily driven by tumor-specific characteristics rather than the patient's age.
*Level of irregularity of the borders*
- **Border irregularity** is one of the ABCDE criteria (Asymmetry, Border irregularity, Color variation, Diameter >6mm, Evolving) used to identify suspicious pigmented lesions.
- It is a diagnostic indicator that warrants further investigation but does not independently determine **prognosis** as definitively as the Breslow depth after biopsy.
Neuroblastoma US Medical PG Question 6: A 2-year-old boy is brought to the physician because of progressive difficulty breathing and a productive cough for the past 2 days. During the past 6 months, he has had recurrent episodes of pneumonia treated with antibiotics. He has not gained weight in this time period. His temperature is 38.5°C (101.3°F), pulse is 130/min, respirations are 18/min, and blood pressure is 100/60 mm Hg. Auscultation of the lungs shows decreased breath sounds over the right lung fields. Ocular examination shows periorbital subcutaneous bleeding and bulging of both eyes. His leukocyte count is 16,000/mm3. An x-ray of the chest shows a right-sided opacity and a collapsed right lung. An MRI of the chest shows a heterogeneous mass in the posterior mediastinum that compresses the heart and the great vessels to the left side. Further evaluation is most likely to show which of the following?
- A. Unregulated B-cell proliferation in the mediastinum
- B. Acid-fast bacteria on sputum microscopy
- C. Increased lymphoblast count in the bone marrow
- D. Overexpression of the N-myc oncogene (Correct Answer)
- E. Autoantibodies against nicotinic acetylcholine receptors
Neuroblastoma Explanation: ***Overexpression of the N-myc oncogene***
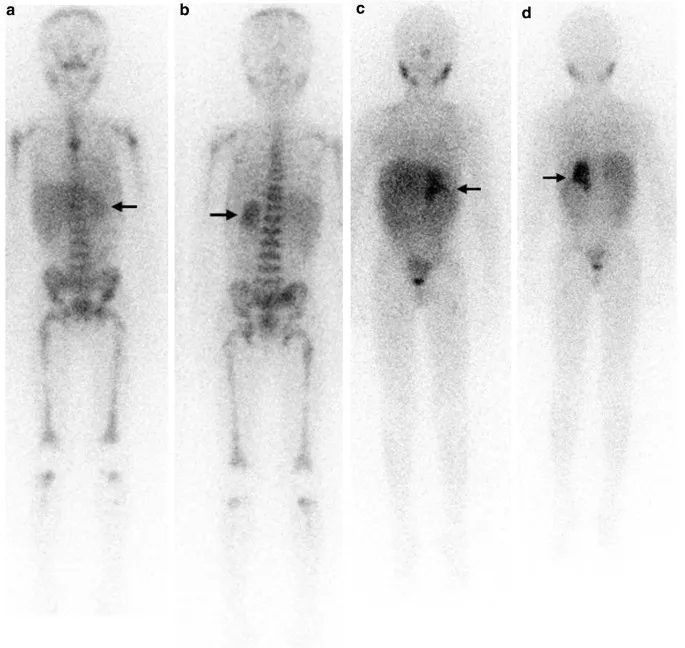
- The combination of a posterior mediastinal mass, periorbital bruising (**raccoon eyes**), and proptosis in a 2-year-old child with recurrent infections and failure to thrive is highly suggestive of **neuroblastoma**.
- **N-myc oncogene amplification** is a common genetic abnormality found in high-risk neuroblastoma and correlates with aggressive disease and poor prognosis.
*Unregulated B-cell proliferation in the mediastinum*
- This would suggest a **lymphoma**, which typically presents with anterior or superior mediastinal masses and often involves lymphadenopathy.
- The specific ocular findings of periorbital ecchymoses and proptosis are not characteristic of lymphoma but are classic for metastatic neuroblastoma.
*Acid-fast bacteria on sputum microscopy*
- This finding is indicative of **tuberculosis**, which can cause mediastinal lymphadenopathy and pulmonary symptoms.
- However, tuberculosis would not typically cause a large heterogeneous posterior mediastinal mass with associated periorbital ecchymoses and proptosis.
*Increased lymphoblast count in the bone marrow*
- This points to **acute lymphoblastic leukemia (ALL)**. While ALL can cause mediastinal masses (T-cell ALL often presents with an anterior mediastinal mass) and systemic symptoms, the **periorbital bruising and proptosis** are specific features that distinguish neuroblastoma.
- Also, a significantly increased lymphoblast count in the bone marrow is the defining diagnostic criterion for leukemia, which is not directly suggested by the initial presentation beyond general systemic illness.
*Autoantibodies against nicotinic acetylcholine receptors*
- This finding is characteristic of **myasthenia gravis**, an autoimmune neuromuscular disorder.
- Myasthenia gravis presents with **muscle weakness and fatigue**, not a posterior mediastinal mass, recurrent pneumonia, failure to thrive, or ocular bulging/bruising as described.
Neuroblastoma US Medical PG Question 7: An 18-month-old boy is brought to the doctor’s office for evaluation of abdominal pain. The boy looks emaciated and he is now significantly below his growth chart predicted weight. The family history is non-contributory. The vital signs are unremarkable. On physical examination, a non-tender mass is felt in the upper part of the abdomen. A magnetic resonance image (MRI) scan of his abdomen demonstrates a mass in his right adrenal gland. Biopsy of the mass demonstrates an abundance of small round blue cells. With this biopsy result, which 1 of the following findings would confirm the diagnosis?
- A. Elevation of vanillylmandelic acid in the urine (Correct Answer)
- B. MRI showing the intrarenal origin of the mass
- C. Increased lactic dehydrogenase
- D. Increased alpha-fetoprotein
- E. Radiograph of the bone showing the presence of lytic bone lesion with periosteal reaction
Neuroblastoma Explanation: ***Elevation of vanillylmandelic acid in the urine***
- The clinical presentation (abdominal mass, emaciation, age) and biopsy finding of **small round blue cells** in the adrenal gland are highly suggestive of **neuroblastoma**.
- **Neuroblastomas** arise from neural crest cells and characteristically produce **catecholamines**, leading to elevated urinary levels of their metabolites like **vanillylmandelic acid (VMA)** and **homovanillic acid (HVA)**.
*MRI showing the intrarenal origin of the mass*
- An **intrarenal origin** of the mass would suggest a **Wilms tumor** (nephroblastoma), which is another common pediatric abdominal malignancy.
- However, the mass is described as being in the **adrenal gland**, and the biopsy shows small round blue cells, which are characteristic of neuroblastoma rather than Wilms tumor.
*Increased lactic dehydrogenase*
- Elevated **lactic dehydrogenase (LDH)** is a non-specific tumor marker often associated with a high tumor burden and rapid cell turnover in various malignancies, including neuroblastoma.
- While it can be elevated in neuroblastoma, it is not a specific diagnostic marker and would not confirm the diagnosis over other pediatric cancers.
*Increased alpha-fetoprotein*
- Elevated **alpha-fetoprotein (AFP)** is primarily associated with **hepatoblastoma** and **germ cell tumors**.
- It is not typically elevated in neuroblastoma and would therefore not confirm this diagnosis.
*Radiograph of the bone showing the presence of lytic bone lesion with periosteal reaction*
- While **neuroblastoma** can metastasize to bones, causing **lytic bone lesions** and a periosteal reaction, these findings indicate metastatic disease rather than confirming the primary diagnosis.
- A bone radiograph showing such lesions points to advanced disease but doesn't specifically confirm neuroblastoma as the primary tumor type.
Neuroblastoma US Medical PG Question 8: A 7-year-old girl is brought to the physician by her mother because of a 2-week history of generalized fatigue, intermittent fever, and progressively worsening shortness of breath. Physical examination shows pallor, jugular venous distention, and nontender cervical and axillary lymphadenopathy. Inspiratory stridor is heard on auscultation of the chest. The liver is palpated 3 cm below the right costal margin. Her hemoglobin concentration is 9.5 g/dL, leukocyte count is 66,000/mm³, and platelet count is 102,000/mm³. An x-ray of the chest shows a mediastinal mass. A bone marrow aspirate predominantly shows leukocytes and presence of 35% lymphoblasts. Which of the following additional findings is most likely in this patient?
- A. t(8;14) translocation
- B. Positive myeloperoxidase staining
- C. Positive CD3/CD7 staining (Correct Answer)
- D. t(9;22) translocation
- E. Reed-Sternberg cells
Neuroblastoma Explanation: ***Positive CD3/CD7 staining***
- The presence of a **mediastinal mass** with **T-cell lymphoblastic leukemia/lymphoma (T-ALL)** is highly associated with a **T-cell immunophenotype**. **CD3** and **CD7** are **T-cell surface markers**.
- The constellation of findings, including **lymphadenopathy**, **hepatomegaly**, **bone marrow involvement** with 35% lymphoblasts, and a **mediastinal mass** causing **stridor**, is classic for T-ALL, which is typically of T-cell origin.
*t(8;14) translocation*
- This translocation is characteristic of **Burkitt lymphoma**, which typically presents as an **extranodal mass** (e.g., jaw, abdomen) rather than a primary mediastinal mass causing stridor.
- While Burkitt lymphoma is also a B-cell non-Hodgkin lymphoma and can have bone marrow involvement, the clinical picture here is not typical for Burkitt lymphoma.
*Positive myeloperoxidase staining*
- **Myeloperoxidase** is an enzyme found in the granules of **myeloid cells**, and its staining is characteristic of **acute myeloid leukemia (AML)**.
- While the patient has leukocytosis and anemia, the predominance of **lymphoblasts** in the bone marrow aspirate points away from AML.
*t(9;22) translocation*
- The **Philadelphia chromosome**, associated with **t(9;22) translocation**, is highly characteristic of **chronic myeloid leukemia (CML)** and can be seen in a subset of **B-cell acute lymphoblastic leukemia (B-ALL)**.
- However, the clinical presentation with a large mediastinal mass causing stridor is more typical of T-ALL, which is not strongly associated with t(9;22).
*Reed-Sternberg cells*
- **Reed-Sternberg cells** are the hallmark of **Hodgkin lymphoma**.
- While Hodgkin lymphoma can present with **mediastinal mass** and **lymphadenopathy**, it typically affects older children/adolescents or young adults, and the presence of **35% lymphoblasts** in the bone marrow indicates leukemia, not Hodgkin lymphoma.
Neuroblastoma US Medical PG Question 9: A 4-year-old boy with Down syndrome presents with fatigue and recurrent infections. CBC shows WBC 150,000/μL with 90% myeloblasts, hemoglobin 6.5 g/dL, platelets 15,000/μL. Flow cytometry confirms acute myeloid leukemia with megakaryoblastic features (AMKL). The parents are concerned about treatment intensity given their child's baseline developmental delays and increased treatment-related toxicity risk in Down syndrome. Evaluate the treatment approach considering the unique biology and competing risks.
- A. Modified chemotherapy protocol with dose reductions of cytarabine but standard anthracyclines, given Down syndrome-associated AML excellent prognosis (Correct Answer)
- B. Bone marrow transplantation as first-line therapy
- C. Palliative care approach given poor baseline function and high treatment toxicity
- D. Reduced-intensity chemotherapy due to Down syndrome and baseline developmental concerns
- E. Standard AML chemotherapy protocol without modification
Neuroblastoma Explanation: ***Modified chemotherapy protocol with dose reductions of cytarabine but standard anthracyclines, given Down syndrome-associated AML excellent prognosis***
- Children with **Down syndrome-associated AML (DS-AML)**, specifically the **megakaryoblastic (AMKL)** subtype, exhibit hyper-sensitivity to **cytarabine** due to lower levels of the enzyme cytidine deaminase.
- While they have an **excellent prognosis** (cure rates >80%), they face a high risk of **treatment-related toxicity**, necessitating dose modifications to improve safety without sacrificing efficacy.
*Bone marrow transplantation as first-line therapy*
- **Hematopoietic stem cell transplant** is not indicated as first-line therapy because DS-AML responds exceptionally well to **chemotherapy** alone.
- Transplant carries a high risk of **morbidity and mortality**, which is unnecessary given the high survival rates with modified chemo regimens.
*Palliative care approach given poor baseline function and high treatment toxicity*
- Palliative care is inappropriate as the primary strategy because DS-AML is a **highly curable** malignancy in pediatric patients.
- Developmental delays and baseline status do not preclude aggressive **curative intent** therapy, as long as protocols are adjusted for toxicity.
*Reduced-intensity chemotherapy due to Down syndrome and baseline developmental concerns*
- While toxicity is a concern, broad "reduced-intensity" therapy may lead to **under-treatment** and increased risk of **relapse**.
- Specific modifications, rather than blanket reductions, are required to maintain the **high cure rate** associated with the **GATA1 mutation** characteristic of this disease.
*Standard AML chemotherapy protocol without modification*
- Using standard AML protocols in children with Down syndrome leads to **excessive toxicity**, particularly severe **mucositis** and life-threatening infections.
- The unique **pharmacogenomics** of Down syndrome patients requires dedicated protocols like the **Children's Oncology Group (COG) AAML0431** to manage treatment risks.
Neuroblastoma US Medical PG Question 10: A 15-year-old boy presents with right distal femur pain and a palpable mass. X-ray shows a mixed lytic-sclerotic lesion with periosteal elevation creating a Codman triangle and sunburst pattern. Biopsy confirms osteosarcoma. Staging shows pulmonary micrometastases. Alkaline phosphatase is markedly elevated. The family requests consideration of alternative therapies and limb salvage options. Synthesize the treatment plan addressing oncologic outcomes and functional preservation.
- A. Limb salvage surgery without chemotherapy followed by observation
- B. Radiation therapy alone as primary treatment
- C. Palliative care focus given metastatic disease at presentation
- D. Immediate amputation without chemotherapy due to metastatic disease
- E. Neoadjuvant chemotherapy, tumor necrosis assessment, limb salvage with endoprosthesis, and adjuvant chemotherapy with potential pulmonary metastasectomy (Correct Answer)
Neuroblastoma Explanation: ***Neoadjuvant chemotherapy, tumor necrosis assessment, limb salvage with endoprosthesis, and adjuvant chemotherapy with potential pulmonary metastasectomy***
- This comprehensive approach is the standard of care; **neoadjuvant chemotherapy** treats micrometastases and allows for **tumor necrosis assessment**, a critical prognostic factor (>90% necrosis).
- **Limb salvage** is oncologically equivalent to amputation when **wide margins** are achievable, and aggressive resection of **pulmonary metastases** can still lead to long-term survival in up to 40% of patients.
*Limb salvage surgery without chemotherapy followed by observation*
- Surgery alone is insufficient because **osteosarcoma** is considered a systemic disease at diagnosis, with **pulmonary micrometastases** present in nearly all patients.
- Omitting **adjuvant chemotherapy** results in high recurrence rates and significantly lower survival outcomes.
*Radiation therapy alone as primary treatment*
- Osteosarcoma is traditionally considered a **radioresistant** tumor, making radiation therapy ineffective as a primary or sole curative modality.
- Surgical resection with **clear margins** is mandatory for local control and achieving a cure.
*Palliative care focus given metastatic disease at presentation*
- Unlike many other adult cancers, **pediatric osteosarcoma** with limited metastatic disease (especially to the lungs) is potentially curable with aggressive therapy.
- A shift to purely **palliative care** would be premature and denies the patient a significant chance at long-term survival.
*Immediate amputation without chemotherapy due to metastatic disease*
- **Immediate amputation** does not address systemic micrometastases and provides no clinical benefit over **limb salvage** if negative margins can be obtained.
- Bypassing **neoadjuvant chemotherapy** loses the opportunity to assess **chemosensitivity**, which is vital for tailoring postoperative treatment.
More Neuroblastoma US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.