Lymphomas in pediatric population US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Lymphomas in pediatric population. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Lymphomas in pediatric population US Medical PG Question 1: A 10-year-old boy with trisomy 21 arrives for his annual check-up with his pediatrician. His parents explain that over the past week, he has been increasingly withdrawn and lethargic. On examination, lymph nodes appear enlarged around the left side of his neck; otherwise, there are no remarkable findings. The pediatrician orders some routine blood work.
These are the results of his complete blood count:
WBC 30.4 K/μL
RBC 1.6 M/μL
Hemoglobin 5.1 g/dL
Hematocrit 15%
MCV 71 fL
MCH 19.5 pg
MCHC 28 g/dL
Platelets 270 K/μL
Differential:
Neutrophils 4%
Lymphocytes 94%
Monocytes 2%
Peripheral smear demonstrates evidence of immature cells and the case is referred to hematopathology. On flow cytometry, the cells are found to be CALLA (CD10) negative. Which of the following diseases is most associated with these clinical and cytological findings?
- A. Precursor B-cell acute lymphoblastic leukemia/lymphoma
- B. Hairy cell leukemia
- C. Classic Hodgkin’s lymphoma
- D. Diffuse large B-cell lymphoma
- E. Precursor T-cell acute lymphoblastic leukemia/lymphoma (Correct Answer)
Lymphomas in pediatric population Explanation: ***Precursor T-cell acute lymphoblastic leukemia/lymphoma***
- The patient's **trisomy 21 (Down syndrome)** increases the risk for leukemia, and the CBC shows signs of **acute leukemia** (marked leukocytosis with lymphoblastic predominance and severe anemia).
- **Enlarged lymph nodes**, particularly on one side of the neck (unilateral cervical lymphadenopathy), and the **immature cells** on peripheral smear, coupled with **CALLA (CD10) negativity**, strongly indicate a **T-cell lineage** for the ALL.
- **CD10 (CALLA) is characteristically positive in precursor B-cell ALL** but **negative in T-cell ALL**, making this the key diagnostic feature distinguishing between B-ALL and T-ALL in this case.
*Precursor B-cell acute lymphoblastic leukemia/lymphoma*
- While this is the most common form of childhood ALL and is associated with Down syndrome, this diagnosis is unlikely due to the **CALLA (CD10) negativity**.
- **CD10 is typically positive in precursor B-ALL**, making this immunophenotype inconsistent with B-cell lineage.
- The presentation of **enlarged lymph nodes** is consistent with ALL, but the specific immunophenotype points away from B-cell lineage here.
*Hairy cell leukemia*
- This is a rare, **indolent B-cell leukemia** typically seen in middle-aged to older adults, not a child.
- It is characterized by **pancytopenia** and abnormal "hairy" lymphocytes with cytoplasmic projections, which does not match the acute presentation or the CBC findings showing marked lymphocytosis.
*Classic Hodgkin's lymphoma*
- This lymphoma is characterized by **Reed-Sternberg cells** and typically presents with localized lymphadenopathy, but the CBC findings (marked leukocytosis with 94% immature lymphocytes) are not typical of Hodgkin's lymphoma.
- It is a **lymphoma**, not a leukemia presenting with widespread immature cells in the blood.
*Diffuse large B-cell lymphoma*
- This is an aggressive **B-cell lymphoma**, primarily affecting adults, though it can occur in children.
- It typically presents as a **mass lesion** and while it can have systemic symptoms, the **CBC findings with overwhelming immature cells in the peripheral blood** pointing to a leukemia are not characteristic of DLBCL.
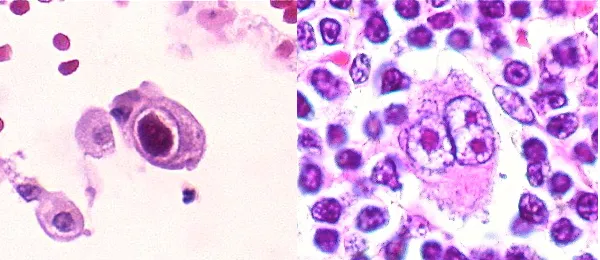
Lymphomas in pediatric population US Medical PG Question 2: A 53-year-old man comes to the physician for recurring fever and night sweats for the past 6 months. The fevers persist for 7 to 10 days and then subside completely for about a week before returning again. During this period, he has also noticed two painless lumps on his neck that have gradually increased in size. Over the past year, he has had an 8.2-kg (18.1 lbs) weight loss. Two years ago, he had a severe sore throat and fever, which was diagnosed as infectious mononucleosis. He has smoked a pack of cigarettes daily for the past 10 years. He does not drink alcohol. His job involves monthly international travel to Asia and Africa. He takes no medications. His temperature is 39°C (102.2°F), pulse is 90/min, respirations are 22/min, and blood pressure is 105/60 mm Hg. Physical examination shows 2 enlarged, nontender, fixed cervical lymph nodes on each side of the neck. Microscopic examination of a specimen obtained on biopsy of a cervical lymph node is shown. Which of the following additional findings is most likely present in this patient?
- A. Acid fast bacilli in the sputum
- B. Leukocyte count > 500,000/μL
- C. CD15/30 positive cells (Correct Answer)
- D. Auer rods on peripheral smear
- E. Anti-viral capsid antigen IgG and IgM positive
Lymphomas in pediatric population Explanation: ***CD15/30 positive cells***
- The patient's symptoms of **recurring fever and night sweats (B symptoms)**, significant **weight loss**, and **enlarged, nontender, fixed cervical lymph nodes** are classic presentations of **Hodgkin lymphoma**.
- **Hodgkin lymphoma** is characterized by the presence of **Reed-Sternberg cells**, which are large, often binucleated cells originating from B lymphocytes and are typically positive for **CD15 and CD30 markers**.
*Acid fast bacilli in the sputum*
- While **tuberculosis** can cause fever, night sweats, and weight loss, the presence of **painless, fixed lymph nodes** and the characteristic recurring fever pattern (Pel-Ebstein fever, though not explicitly named, the description fits) are more indicative of lymphoma.
- Absence of respiratory symptoms like cough and the lack of specific risk factors for active tuberculosis (other than travel to endemic areas) make it less likely, though it should be in the differential.
*Leukocyte count > 500,000/μL*
- An extremely high leukocyte count (>500,000/μL) is characteristic of **leukostasis** seen in severe cases of **chronic myeloid leukemia (CML)** or other leukemias.
- The patient's symptoms are not consistent with CML, which typically presents with splenomegaly and less specific B symptoms, and the lymph node biopsy points away from leukemia.
*Auer rods on peripheral smear*
- **Auer rods** are pathognomonic for **acute myeloid leukemia (AML)** and would be found in myeloid blast cells on a peripheral smear or bone marrow biopsy.
- The clinical picture of waxing and waning fevers, night sweats, weight loss, and localized lymphadenopathy is not typical for AML, which usually presents with rapid onset of pancytopenia-related symptoms.
*Anti-viral capsid antigen IgG and IgM positive*
- A positive **anti-viral capsid antigen (VCA) IgM** indicates a **recent or active Epstein-Barr virus (EBV) infection (infectious mononucleosis)**, while positive VCA IgG indicates past infection. The patient had infectious mononucleosis two years ago.
- While **EBV is associated with some types of Hodgkin lymphoma**, currently positive IgM would suggest a new or reactivated infection, not the long-standing progressive symptoms described by the patient. His prior infectious mononucleosis is a risk factor for Hodgkin lymphoma, but not necessarily an active finding.
Lymphomas in pediatric population US Medical PG Question 3: A 5-year-old boy presents to his pediatrician with weakness. His father observed that his son seemed less energetic at daycare and kindergarten classes. He was becoming easily fatigued from mild play. His temperature is 98°F (37°C), blood pressure is 90/60 mmHg, pulse is 100/min, and respirations are 20/min. Physical exam reveals pale conjunctiva, poor skin turgor and capillary refill, and cervical and axillary lymphadenopathy with assorted bruises throughout his body. A complete blood count reveals the following:
Leukocyte count: 3,000/mm^3
Segmented neutrophils: 30%
Bands: 5%
Eosinophils: 5%
Basophils: 10%
Lymphocytes: 40%
Monocytes: 10%
Hemoglobin: 7.1 g/dL
Hematocrit: 22%
Platelet count: 50,000/mm^3
The most specific diagnostic assessment would most likely show which of the following?
- A. Bone marrow biopsy with ≥ 20% lymphoblasts (Correct Answer)
- B. Fluorescence in situ hybridization analysis with 9:22 translocation
- C. Peripheral blood smear with > 50% lymphoblasts
- D. Flow cytometry with positive terminal deoxynucleotidyl transferase staining
- E. Fluorescence in situ hybridization analysis with 12:21 translocation
Lymphomas in pediatric population Explanation: ***Bone marrow biopsy with ≥ 20% lymphoblasts***
- The patient's symptoms (weakness, fatigue, pallor, bruising, lymphadenopathy) and blood counts (anemia, thrombocytopenia, leukopenia with relative lymphocytosis) are highly suggestive of **Acute Lymphoblastic Leukemia (ALL)**.
- The most specific diagnostic assessment for ALL involves a **bone marrow biopsy** showing **≥20% lymphoblasts** per WHO 2016 classification, confirming the abnormal proliferation of immature lymphoid cells.
- This is the **gold standard** for diagnosing ALL and distinguishes it from other hematologic disorders.
*Fluorescence in situ hybridization analysis with 9:22 translocation*
- The **Philadelphia chromosome (t[9;22])** is characteristic of **Chronic Myeloid Leukemia (CML)**, which is rare in children and presents differently.
- While t(9;22) can occur in 3-5% of childhood ALL and indicates poor prognosis, it is a **prognostic marker**, not the primary diagnostic criterion for ALL itself.
*Peripheral blood smear with > 50% lymphoblasts*
- While lymphoblasts can be seen in the peripheral blood in ALL, a specific percentage threshold in peripheral blood is **not a diagnostic criterion** for ALL.
- The peripheral blood smear can be suggestive, but the **bone marrow blast percentage is the gold standard** for definitive diagnosis.
*Flow cytometry with positive terminal deoxynucleotidyl transferase staining*
- **Terminal deoxynucleotidyl transferase (TdT)** is a nuclear enzyme expressed in pre-B and pre-T lymphoblasts and is an important marker for ALL.
- Flow cytometry with positive TdT staining helps **characterize and classify the blasts** but does not quantify the blast percentage required for diagnosis, which is provided by the bone marrow biopsy.
*Fluorescence in situ hybridization analysis with 12:21 translocation*
- The **t(12;21) [ETV6-RUNX1] translocation** is the most common cytogenetic abnormality in childhood B-cell ALL (20-25% of cases) and is associated with favorable prognosis.
- While its presence is relevant for risk stratification and treatment planning, the primary diagnostic criterion for ALL is the **percentage of lymphoblasts in the bone marrow**.
Lymphomas in pediatric population US Medical PG Question 4: A 4-year-old girl is brought to the physician because of a 3-week history of generalized fatigue and easy bruising. During the past week, she has also had fever and severe leg pain that wakes her up at night. Her temperature is 38.3°C (100.9°F), pulse is 120/min, and respirations are 30/min. Examination shows cervical and axillary lymphadenopathy. The abdomen is soft and nontender; the liver is palpated 3 cm below the right costal margin, and the spleen is palpated 2 cm below the left costal margin. Laboratory studies show:
Hemoglobin 10.1 g/dL
Leukocyte count 63,000/mm3
Platelet count 27,000/mm3
A bone marrow aspirate predominantly shows immature cells that stain positive for CD10, CD19, and TdT. Which of the following is the most likely diagnosis?
- A. Aplastic anemia
- B. Hodgkin lymphoma
- C. Acute lymphoblastic leukemia (Correct Answer)
- D. Acute myeloid leukemia
- E. Hairy cell leukemia
Lymphomas in pediatric population Explanation: ***Acute lymphoblastic leukemia***
- The constellation of **generalized fatigue**, **easy bruising** (due to **thrombocytopenia**), fever, **severe leg pain** (bone marrow infiltration), **hepatosplenomegaly**, and **lymphadenopathy** in a child is highly suggestive of **acute leukemia**.
- The laboratory findings of **anemia** (Hb 10.1 g/dL), **thrombocytopenia** (platelet count 27,000/mm³), and a **markedly elevated leukocyte count** (63,000/mm³) with **immature cells** (blasts) in the bone marrow, staining positive for **CD10, CD19, and TdT**, are pathognomonic for **B-cell acute lymphoblastic leukemia (ALL)**.
*Aplastic anemia*
- This condition is characterized by **pancytopenia** (low levels of all blood cell types) due to bone marrow failure, but it would not typically present with **lymphadenopathy**, **hepatosplenomegaly**, or an extremely high leukocyte count with immature cells.
- The bone marrow would be **hypocellular** rather than hypercellular with blasts, as seen in this patient.
*Hodgkin lymphoma*
- While Hodgkin lymphoma can cause **lymphadenopathy** and systemic symptoms like fever and fatigue (B symptoms), it is less common in this age group and does not present with **pancytopenia** or an overwhelming presence of immature cells in the bone marrow.
- Diagnosis relies on the identification of **Reed-Sternberg cells** in lymph node biopsy.
*Acute myeloid leukemia*
- **AML** can also present with similar symptoms and pancytopenia with elevated blasts, but the immunophenotype would differ, typically showing markers like **CD13, CD33, and myeloid-specific markers**, not **CD10, CD19, and TdT**.
- **TdT** positivity is characteristic of lymphoid progenitors.
*Hairy cell leukemia*
- This is a rare, **chronic B-cell leukemia** primarily affecting older adults, not children, and is characterized by cells with **"hairy" projections**, **massive splenomegaly**, and typically **pancytopenia** without a high blast count.
- The immunophenotype involves **CD11c, CD25, CD103, and CD123**.
Lymphomas in pediatric population US Medical PG Question 5: A 37-year old man is being evaluated due to a recent history of fatigue that started 3 weeks ago. The patient presents with a history of HIV, which was first diagnosed 7 years ago. He has been on an antiretroviral regimen and takes it regularly. His CD4+ count is 350 cells/mm3. According to the patient, his partner passed away from a "blood cancer", and he is worried that his fatigue might be connected to a similar pathology. The physician clarifies that there is an increased risk for HIV patients to develop certain kinds of lymphomas. Which one of the conditions below is the patient more likely to develop based on his medical history?
- A. Diffuse large B cell lymphoma (Correct Answer)
- B. Follicular lymphoma
- C. Burkitt’s lymphoma
- D. Extranodal marginal zone lymphoma
- E. Small lymphocytic lymphoma
Lymphomas in pediatric population Explanation: ***Diffuse large B cell lymphoma***
- **Diffuse large B-cell lymphoma (DLBCL)** is the most common type of lymphoma diagnosed in HIV-positive patients, accounting for about 50% of cases.
- The increased risk of DLBCL in HIV patients is related to chronic immune stimulation and dysregulation, often exacerbated by co-infection with viruses like **Epstein-Barr virus (EBV)**.
*Follicular lymphoma*
- **Follicular lymphoma** is generally *less common* in HIV-positive patients compared to the general population.
- Its incidence does not significantly increase in the context of HIV infection.
*Burkitt’s lymphoma*
- **Burkitt's lymphoma** is also more common in HIV patients, but typically presents in those with *more severe immunosuppression* (lower CD4 counts) and is specifically associated with **Epstein-Barr virus (EBV)** co-infection.
- While a possibility, DLBCL is the *overall most likely* lymphoma.
*Extranodal marginal zone lymphoma*
- **Extranodal marginal zone lymphoma** is *not typically associated* with an increased incidence in HIV-positive individuals.
- It often correlates with chronic inflammation or specific infections (e.g., *H. pylori* in gastric MALT lymphoma).
*Small lymphocytic lymphoma*
- **Small lymphocytic lymphoma (SLL)**, which is essentially the nodal form of chronic lymphocytic leukemia (CLL), is *not increased* in incidence in HIV-positive patients.
- CLL/SLL is generally considered to be *less common* or have no increased risk in HIV-infected individuals.
Lymphomas in pediatric population US Medical PG Question 6: A 17-year-old girl comes to the physician because of a sore throat, fevers, and fatigue for the past 3 weeks. Her temperature is 37.8°C (100°F), pulse is 97/min, and blood pressure is 90/60 mm Hg. Examination of the head and neck shows cervical lymphadenopathy, pharyngeal erythema, enlarged tonsils with exudates, and palatal petechiae. The spleen is palpated 2 cm below the left costal margin. Her leukocyte count is 14,100/mm3 with 54% lymphocytes (12% atypical lymphocytes). Results of a heterophile agglutination test are positive. This patient is at increased risk for which of the following conditions?
- A. Mycotic aneurysm
- B. Hodgkin lymphoma (Correct Answer)
- C. Kaposi sarcoma
- D. Hepatocellular carcinoma
- E. Rheumatic fever
Lymphomas in pediatric population Explanation: ***Correct: Hodgkin lymphoma***
- **Epstein-Barr virus (EBV)**, the causative agent of infectious mononucleosis, is strongly associated with the development of **Hodgkin lymphoma**
- Up to **30-50% of Hodgkin lymphoma cases** are linked to prior EBV infection, particularly the **mixed cellularity** and **lymphocyte-depleted** subtypes
- EBV-positive Reed-Sternberg cells are found in these lymphoma subtypes
*Incorrect: Mycotic aneurysm*
- A mycotic aneurysm is an **infected aneurysm** typically caused by bacterial endocarditis or other systemic infections leading to arterial wall weakening
- There is no direct association between infectious mononucleosis and the development of mycotic aneurysms
*Incorrect: Kaposi sarcoma*
- **Kaposi sarcoma** is caused by **Human Herpesvirus 8 (HHV-8)**, not EBV
- Most commonly seen in immunocompromised individuals, such as those with HIV/AIDS
- Not directly associated with Epstein-Barr virus infection
*Incorrect: Hepatocellular carcinoma*
- **Hepatocellular carcinoma** is primarily associated with chronic liver diseases, such as chronic **hepatitis B** or **hepatitis C** infection, **alcoholic liver disease**, and **nonalcoholic steatohepatitis (NASH)**
- EBV is associated with **nasopharyngeal carcinoma** and **Burkitt lymphoma**, not hepatocellular carcinoma
*Incorrect: Rheumatic fever*
- **Rheumatic fever** is a delayed, non-suppurative complication of untreated **Group A Streptococcus (GAS)** pharyngitis
- The patient's symptoms are consistent with **infectious mononucleosis** (positive heterophile agglutination test, atypical lymphocytes, persistent fatigue, splenomegaly), not GAS pharyngitis
- Monospot test distinguishes EBV from bacterial pharyngitis
Lymphomas in pediatric population US Medical PG Question 7: An inconsolable mother brings her 2-year-old son to the emergency room after finding a large amount of bright red blood in his diaper, an hour ago. She states that for the past week her son has been having crying fits while curling his legs towards his chest in a fetal position. His crying resolves either after vomiting or passing fecal material. Currently, the child is in no apparent distress. Physical examination with palpation in the gastric region demonstrates no acute findings. X-ray of the abdominal area demonstrates no acute findings. His current temperature is 36.5°C (97.8°F), heart rate is 93/min, blood pressure is 100/64 mm Hg, and respiratory rate is 26/min. His weight is 10.8 kg (24.0 lb), and height is 88.9 cm (35.0 in). Laboratory tests show the following:
RBC count 5 million/mm3
Hematocrit 36%
Hemoglobin 12 g/dL
WBC count 6,000/mm3
Mean corpuscular volume 78 fL
What is the most likely underlying embryological cause predisposing to this condition?
- A. Failure of the vitelline duct to close (Correct Answer)
- B. Failure of the vitelline duct to open
- C. Elevated anti-mitochondrial antibodies
- D. Problem with bilirubin conjugation
- E. Problem with bilirubin uptake
Lymphomas in pediatric population Explanation: ***Failure of the vitelline duct to close***
- The clinical presentation of a 2-year-old with recurrent episodes of abdominal pain, crying spells (curling legs to chest), and the passage of bright red blood in the diaper is highly suggestive of **intussusception**. This can be transiently relieved when the "curled" bowel straightens itself out, or gas/fecal matter is passed. The presence of **bright red blood** (often referred to as **currant jelly stools** when mixed with mucus) further supports this diagnosis, indicating ischemic bowel.
- In children, intussusception is often idiopathic, but in a small percentage of cases, especially in older infants and children, an **anatomical lead point** can cause it. The most common anatomical lead point is a **Meckel's diverticulum**, which results from the **incomplete obliteration of the vitelline duct** (also known as the omphalomesenteric duct) during embryological development. The diverticulum can act as a foreign body that then telescopes into the adjacent bowel, causing intussusception.
*Failure of the vitelline duct to open*
- The vitelline duct should normally regress and disappear. Therefore, a "failure to open" is not a recognized embryological anomaly or pathology.
- Problems related to the vitelline duct involve either its **incomplete closure** (leading to Meckel's diverticulum, vitelline cysts, or fistulas) or other abnormal remnants, not a failure to open.
*Elevated anti-mitochondrial uptake*
- This option refers to **anti-mitochondrial antibodies (AMAs)**, which are characteristic markers for **primary biliary cholangitis (PBC)**, an autoimmune disease primarily affecting the liver.
- PBC is an adult-onset condition and is not associated with intussusception or the gastrointestinal symptoms described in the child.
*Problem with bilirubin conjugation*
- Issues with **bilirubin conjugation** primarily manifest as different types of **jaundice** (e.g., Crigler-Najjar syndrome, Gilbert's syndrome) due to the accumulation of unconjugated bilirubin.
- These conditions do not cause abdominal pain, intussusception, or bloody stools.
*Problem with bilirubin uptake*
- Problems with **bilirubin uptake** by hepatocytes also lead to **unconjugated hyperbilirubinemia** and jaundice.
- This condition is unrelated to acute abdominal emergencies like intussusception or gastrointestinal bleeding.
Lymphomas in pediatric population US Medical PG Question 8: An 18-month-old boy is brought to the doctor’s office for evaluation of abdominal pain. The boy looks emaciated and he is now significantly below his growth chart predicted weight. The family history is non-contributory. The vital signs are unremarkable. On physical examination, a non-tender mass is felt in the upper part of the abdomen. A magnetic resonance image (MRI) scan of his abdomen demonstrates a mass in his right adrenal gland. Biopsy of the mass demonstrates an abundance of small round blue cells. With this biopsy result, which 1 of the following findings would confirm the diagnosis?
- A. Elevation of vanillylmandelic acid in the urine (Correct Answer)
- B. MRI showing the intrarenal origin of the mass
- C. Increased lactic dehydrogenase
- D. Increased alpha-fetoprotein
- E. Radiograph of the bone showing the presence of lytic bone lesion with periosteal reaction
Lymphomas in pediatric population Explanation: ***Elevation of vanillylmandelic acid in the urine***
- The clinical presentation (abdominal mass, emaciation, age) and biopsy finding of **small round blue cells** in the adrenal gland are highly suggestive of **neuroblastoma**.
- **Neuroblastomas** arise from neural crest cells and characteristically produce **catecholamines**, leading to elevated urinary levels of their metabolites like **vanillylmandelic acid (VMA)** and **homovanillic acid (HVA)**.
*MRI showing the intrarenal origin of the mass*
- An **intrarenal origin** of the mass would suggest a **Wilms tumor** (nephroblastoma), which is another common pediatric abdominal malignancy.
- However, the mass is described as being in the **adrenal gland**, and the biopsy shows small round blue cells, which are characteristic of neuroblastoma rather than Wilms tumor.
*Increased lactic dehydrogenase*
- Elevated **lactic dehydrogenase (LDH)** is a non-specific tumor marker often associated with a high tumor burden and rapid cell turnover in various malignancies, including neuroblastoma.
- While it can be elevated in neuroblastoma, it is not a specific diagnostic marker and would not confirm the diagnosis over other pediatric cancers.
*Increased alpha-fetoprotein*
- Elevated **alpha-fetoprotein (AFP)** is primarily associated with **hepatoblastoma** and **germ cell tumors**.
- It is not typically elevated in neuroblastoma and would therefore not confirm this diagnosis.
*Radiograph of the bone showing the presence of lytic bone lesion with periosteal reaction*
- While **neuroblastoma** can metastasize to bones, causing **lytic bone lesions** and a periosteal reaction, these findings indicate metastatic disease rather than confirming the primary diagnosis.
- A bone radiograph showing such lesions points to advanced disease but doesn't specifically confirm neuroblastoma as the primary tumor type.
Lymphomas in pediatric population US Medical PG Question 9: A 2-year-old boy is brought to the physician because of progressive difficulty breathing and a productive cough for the past 2 days. During the past 6 months, he has had recurrent episodes of pneumonia treated with antibiotics. He has not gained weight in this time period. His temperature is 38.5°C (101.3°F), pulse is 130/min, respirations are 18/min, and blood pressure is 100/60 mm Hg. Auscultation of the lungs shows decreased breath sounds over the right lung fields. Ocular examination shows periorbital subcutaneous bleeding and bulging of both eyes. His leukocyte count is 16,000/mm3. An x-ray of the chest shows a right-sided opacity and a collapsed right lung. An MRI of the chest shows a heterogeneous mass in the posterior mediastinum that compresses the heart and the great vessels to the left side. Further evaluation is most likely to show which of the following?
- A. Unregulated B-cell proliferation in the mediastinum
- B. Acid-fast bacteria on sputum microscopy
- C. Increased lymphoblast count in the bone marrow
- D. Overexpression of the N-myc oncogene (Correct Answer)
- E. Autoantibodies against nicotinic acetylcholine receptors
Lymphomas in pediatric population Explanation: ***Overexpression of the N-myc oncogene***
- The combination of a posterior mediastinal mass, periorbital bruising (**raccoon eyes**), and proptosis in a 2-year-old child with recurrent infections and failure to thrive is highly suggestive of **neuroblastoma**.
- **N-myc oncogene amplification** is a common genetic abnormality found in high-risk neuroblastoma and correlates with aggressive disease and poor prognosis.
*Unregulated B-cell proliferation in the mediastinum*
- This would suggest a **lymphoma**, which typically presents with anterior or superior mediastinal masses and often involves lymphadenopathy.
- The specific ocular findings of periorbital ecchymoses and proptosis are not characteristic of lymphoma but are classic for metastatic neuroblastoma.
*Acid-fast bacteria on sputum microscopy*
- This finding is indicative of **tuberculosis**, which can cause mediastinal lymphadenopathy and pulmonary symptoms.
- However, tuberculosis would not typically cause a large heterogeneous posterior mediastinal mass with associated periorbital ecchymoses and proptosis.
*Increased lymphoblast count in the bone marrow*
- This points to **acute lymphoblastic leukemia (ALL)**. While ALL can cause mediastinal masses (T-cell ALL often presents with an anterior mediastinal mass) and systemic symptoms, the **periorbital bruising and proptosis** are specific features that distinguish neuroblastoma.
- Also, a significantly increased lymphoblast count in the bone marrow is the defining diagnostic criterion for leukemia, which is not directly suggested by the initial presentation beyond general systemic illness.
*Autoantibodies against nicotinic acetylcholine receptors*
- This finding is characteristic of **myasthenia gravis**, an autoimmune neuromuscular disorder.
- Myasthenia gravis presents with **muscle weakness and fatigue**, not a posterior mediastinal mass, recurrent pneumonia, failure to thrive, or ocular bulging/bruising as described.
Lymphomas in pediatric population US Medical PG Question 10: A 7-year-old girl is brought to the physician by her mother because of a 2-week history of generalized fatigue, intermittent fever, and progressively worsening shortness of breath. Physical examination shows pallor, jugular venous distention, and nontender cervical and axillary lymphadenopathy. Inspiratory stridor is heard on auscultation of the chest. The liver is palpated 3 cm below the right costal margin. Her hemoglobin concentration is 9.5 g/dL, leukocyte count is 66,000/mm³, and platelet count is 102,000/mm³. An x-ray of the chest shows a mediastinal mass. A bone marrow aspirate predominantly shows leukocytes and presence of 35% lymphoblasts. Which of the following additional findings is most likely in this patient?
- A. t(8;14) translocation
- B. Positive myeloperoxidase staining
- C. Positive CD3/CD7 staining (Correct Answer)
- D. t(9;22) translocation
- E. Reed-Sternberg cells
Lymphomas in pediatric population Explanation: ***Positive CD3/CD7 staining***
- The presence of a **mediastinal mass** with **T-cell lymphoblastic leukemia/lymphoma (T-ALL)** is highly associated with a **T-cell immunophenotype**. **CD3** and **CD7** are **T-cell surface markers**.
- The constellation of findings, including **lymphadenopathy**, **hepatomegaly**, **bone marrow involvement** with 35% lymphoblasts, and a **mediastinal mass** causing **stridor**, is classic for T-ALL, which is typically of T-cell origin.
*t(8;14) translocation*
- This translocation is characteristic of **Burkitt lymphoma**, which typically presents as an **extranodal mass** (e.g., jaw, abdomen) rather than a primary mediastinal mass causing stridor.
- While Burkitt lymphoma is also a B-cell non-Hodgkin lymphoma and can have bone marrow involvement, the clinical picture here is not typical for Burkitt lymphoma.
*Positive myeloperoxidase staining*
- **Myeloperoxidase** is an enzyme found in the granules of **myeloid cells**, and its staining is characteristic of **acute myeloid leukemia (AML)**.
- While the patient has leukocytosis and anemia, the predominance of **lymphoblasts** in the bone marrow aspirate points away from AML.
*t(9;22) translocation*
- The **Philadelphia chromosome**, associated with **t(9;22) translocation**, is highly characteristic of **chronic myeloid leukemia (CML)** and can be seen in a subset of **B-cell acute lymphoblastic leukemia (B-ALL)**.
- However, the clinical presentation with a large mediastinal mass causing stridor is more typical of T-ALL, which is not strongly associated with t(9;22).
*Reed-Sternberg cells*
- **Reed-Sternberg cells** are the hallmark of **Hodgkin lymphoma**.
- While Hodgkin lymphoma can present with **mediastinal mass** and **lymphadenopathy**, it typically affects older children/adolescents or young adults, and the presence of **35% lymphoblasts** in the bone marrow indicates leukemia, not Hodgkin lymphoma.
More Lymphomas in pediatric population US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.