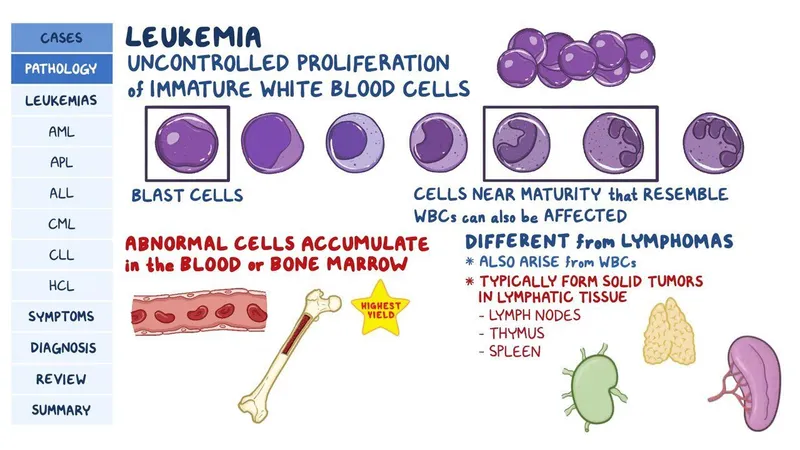
Leukemias in children US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Leukemias in children. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
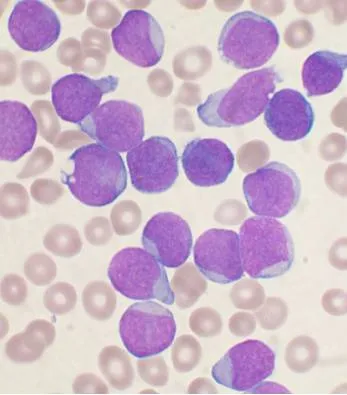
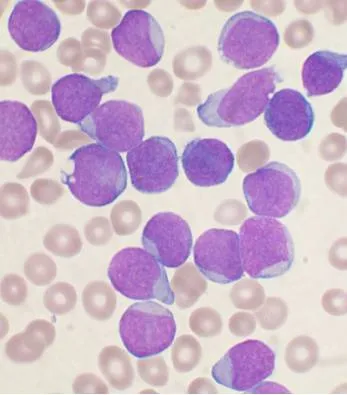
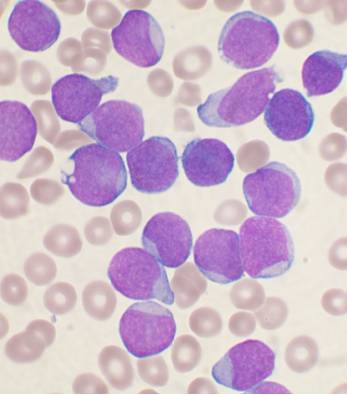
Leukemias in children US Medical PG Question 1: A 7-year-old boy presents to the ER with progressive dysphagia over the course of 3 months and a new onset fever for the past 24 hours. The temperature in the ER was 39.5°C (103.1°F). There are white exudates present on enlarged tonsils (Grade 2). Routine blood work reveals a WBC count of 89,000/mm3, with the automatic differential yielding a high (> 90%) percentage of lymphocytes. A peripheral blood smear is ordered, demonstrating the findings in the accompanying image. The peripheral smear is submitted to pathology for review. After initial assessment, the following results are found on cytologic assessment of the cells:
TdT: positive
CALLA (CD 10): positive
Which of the following cell markers are most likely to be positive as well?
- A. CD 2
- B. CD 19 (Correct Answer)
- C. CD 7
- D. CD 8
- E. CD 5
Leukemias in children Explanation: ***CD 19***
- The presence of **TdT** and **CD10 (CALLA)** in a 7-year-old boy with a high WBC count dominated by lymphocytes strongly indicates **B-cell acute lymphoblastic leukemia (B-ALL)**.
- **CD19** is a pan-B-cell marker, universally expressed on B-lymphocytes from their earliest stages of development, making its positivity highly consistent with B-ALL.
*CD 2*
- **CD2** is a surface glycoprotein commonly found on **T-cells** and **NK cells**, not typically on precursors of normal or leukemic B-cells.
- Its presence would suggest a T-cell lineage rather than the B-cell lineage indicated by CD10 and TdT in this context.
*CD 7*
- **CD7** is an early marker for **T-lymphoid precursors** and **NK cells**, and is consistently expressed in T-cell acute lymphoblastic leukemia (T-ALL).
- It is not associated with B-cell lineage development or B-ALL.
*CD 8*
- **CD8** is a co-receptor for the T-cell receptor (TCR) and is found on **cytotoxic T lymphocytes (CTLs)**, a mature T-cell subset.
- Its presence would indicate a mature T-cell lineage, which is inconsistent with ALL and the other described markers.
*CD 5*
- **CD5** is a transmembrane glycoprotein found on **mature T-cells** and a subset of **B-cells**, particularly associated with chronic lymphocytic leukemia (CLL) or mantle cell lymphoma.
- It is not a characteristic marker for B-ALL and its expression would not be expected in this context.
Leukemias in children US Medical PG Question 2: A 66-year-old man comes to the physician for a 3-month history of fatigue. He has hypertension and hyperlipidemia. He had a transient ischemic attack 3 years ago. He drinks 3 beers a day, and sometimes a couple more on social occasions. He currently takes aspirin, simvastatin, hydrochlorothiazide, and metoprolol. His temperature is 37.1°C (98.8°F), pulse is 78, respirations are 19/min, and oxygen saturation on room air is 97%. He is in no distress but shows marked pallor and has multiple pinpoint, red, nonblanching spots on his extremities. On palpation, his spleen is significantly enlarged. Laboratory studies show a hemoglobin of 8.0 g/dL, a leukocyte count of 80,000/mm3, and a platelet count of 34,000/mm3. A blood smear shows immature cells with large, prominent nucleoli and pink, elongated, needle-shaped cytoplasmic inclusions. Which of the following is the most likely diagnosis?
- A. Cirrhosis
- B. Acute lymphoblastic leukemia
- C. Chronic lymphocytic leukemia
- D. Myelodysplastic syndrome
- E. Acute myelogenous leukemia (Correct Answer)
Leukemias in children Explanation: **Acute myelogenous leukemia**
- The presence of **fatigue**, **marked pallor**, **splenomegaly**, **petechiae** (pinpoint, red, nonblanching spots), and **pancytopenia** (anemia, leukocytosis with immature forms, thrombocytopenia) are highly suggestive of acute leukemia.
- The blood smear findings of **immature cells with large, prominent nucleoli** and **pink, elongated, needle-shaped cytoplasmic inclusions** (likely **Auer rods**) are pathognomonic for **acute myelogenous leukemia (AML)**.
*Cirrhosis*
- While **splenomegaly** and **pancytopenia** can occur in cirrhosis due to portal hypertension and hypersplenism, the specific blood smear findings of **immature cells** and **Auer rods** are not characteristic of cirrhosis.
- The patient's alcohol intake could contribute to cirrhosis, but the hematological picture points definitively away from liver disease as the primary diagnosis.
*Acute lymphoblastic leukemia*
- Although acute lymphoblastic leukemia (ALL) presents with **fatigue**, **pallor**, and **pancytopenia**, the **immature cells** in ALL are lymphoblasts, which **lack Auer rods**.
- The specific morphology described (large, prominent nucleoli, needle-shaped cytoplasmic inclusions) is inconsistent with ALL.
*Chronic lymphocytic leukemia*
- CLL typically presents with **lymphocytosis** (extremely high leukocyte count composed of mature-appearing lymphocytes) and often **splenomegaly**, but usually **without significant anemia or thrombocytopenia** at presentation.
- The presence of **immature cells** and **Auer rods** is inconsistent with CLL, which involves mature B-lymphocytes.
*Myelodysplastic syndrome*
- MDS can cause **cytopenias** and may involve **immature blast forms**, but the blast count is typically less than 20% in the bone marrow (or periphery) and it does **not typically present with Auer rods** in circulating blasts.
- The profound leukocytosis with highly immature cells and specific inclusions points beyond MDS to an acute leukemia.
Leukemias in children US Medical PG Question 3: A 64-year-old woman comes to the physician for her routine health maintenance examination. She feels well. She had cervical cancer and received radiotherapy 8 years ago. Her vital signs are within normal limits. On percussion, the spleen size is 15 cm. Otherwise, the physical examination shows no abnormalities. The laboratory test results are as follows:
Hemoglobin 10 g/dL
Mean corpuscular volume 88 μm3
Leukocyte count 65,000/mm3
Platelet count 500,000/mm3
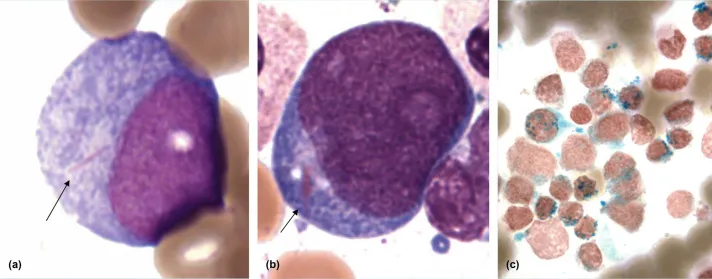
Two images of the peripheral blood smear are shown on the image. Which of the following is the most appropriate next step in management?
- A. Phlebotomy
- B. Rituximab
- C. Watchful waiting
- D. Allogeneic stem cell transplantation
- E. Dasatinib (Correct Answer)
Leukemias in children Explanation: ***Dasatinib***
- The patient's presentation with **anemia**, **marked leukocytosis (65,000/mm³) with predominantly myeloid cells**, **thrombocytosis (500,000/mm³)**, and **splenomegaly (15 cm)** is highly suggestive of **Chronic Myeloid Leukemia (CML)**. The peripheral smear showing **myelocytes, metamyelocytes, and basophils** (indicated by arrows on the image) further supports this diagnosis.
- **Dasatinib** is a second-generation **tyrosine kinase inhibitor (TKI)** that targets the **BCR-ABL fusion protein**, which is the hallmark of CML. TKIs are the first-line treatment for CML.
*Phlebotomy*
- This is primarily used for **polycythemia vera** to reduce red blood cell mass and hematocrit.
- It is not indicated for CML, which is characterized by an overproduction of myeloid cells, not primarily red blood cells.
*Rituximab*
- **Rituximab** is a monoclonal antibody targeting the **CD20 antigen** on B-lymphocytes.
- It is used in the treatment of **B-cell non-Hodgkin lymphoma** and some autoimmune diseases, not CML.
*Watchful waiting*
- Given the patient's clear signs of **CML (leukocytosis, thrombocytosis, splenomegaly, and characteristic peripheral smear)**, active treatment is indicated, not watchful waiting.
- CML, if left untreated, progresses from the chronic phase to accelerated phase and then to **blast crisis**, which is rapidly fatal.
*Allogeneic stem cell transplantation*
- **Allogeneic stem cell transplantation** is a potentially curative treatment for CML.
- However, it is typically reserved for patients who have **failed TKI therapy** or have high-risk features, as **TKIs are the initial first-line treatment** due to their effectiveness and lower toxicity compared to transplantation.
Leukemias in children US Medical PG Question 4: A 59-year-old woman comes to the physician because of a 2-month history of fatigue and abdominal discomfort. Over the past 6 months, she has had a 5.4-kg (12-lb) weight loss. She takes no medications. Her temperature is 37.8°C (100°F), pulse is 70/min, respirations are 13/min, and blood pressure is 125/80 mm Hg. Cardiopulmonary examination shows no abnormalities. The spleen is palpated 3 cm below the left costal margin. Laboratory studies show:
Hemoglobin 9.4 g/dL
Mean corpuscular volume 86 μm3
Leukocyte count 58,000/mm3
Segmented neutrophils 54%
Bands 8%
Lymphocytes 7%
Myelocytes 5%
Metamyelocytes 10%
Promyelocytes 4%
Blasts 5%
Monocytes 1%
Eosinophils 4%
Basophils 2%
Platelet count 850,000/mm3
Serum
Creatinine
0.9 mg/dL
LDH 501 U/L
Bone marrow biopsy shows hyperplastic myelopoiesis with granulocytosis. Which of the following is the most appropriate next step in management?
- A. Serum protein electrophoresis
- B. Cytogenetic studies (Correct Answer)
- C. Observation and follow-up
- D. All-trans retinoic acid
- E. Cytarabine and daunorubicin
Leukemias in children Explanation: ***Cytogenetic studies***
- The patient's presentation with **splenomegaly**, **leukocytosis with a left shift** (including myelocytes, metamyelocytes, and some blasts), **thrombocytosis**, and **fatigue, weight loss, and abdominal discomfort** are highly suggestive of a myeloproliferative neoplasm, specifically **chronic myeloid leukemia (CML)**.
- **Cytogenetic studies** (e.g., FISH or conventional karyotyping) are crucial to confirm CML by detecting the **Philadelphia chromosome (t(9;22))**, which forms the **BCR-ABL1 fusion gene**, the hallmark of this disease.
*Serum protein electrophoresis*
- **Serum protein electrophoresis (SPEP)** is primarily used to diagnose and monitor **monoclonal gammopathies**, such as multiple myeloma or Waldenström macroglobulinemia.
- It is not relevant for the diagnosis of myeloproliferative disorders like CML, which involve myeloid cell lines, not plasma cells.
*Observation and follow-up*
- Given the patient's symptomatic presentation (fatigue, weight loss, abdominal discomfort), significant leukocytosis, thrombocytosis, and splenomegaly, **active intervention and diagnosis are warranted**.
- Observing a patient with suspected CML is not appropriate, as it can progress to an accelerated phase or blast crisis if left untreated.
*All-trans retinoic acid*
- **All-trans retinoic acid (ATRA)** is a specific treatment used for **acute promyelocytic leukemia (APL)**, a subtype of acute myeloid leukemia.
- APL characteristically presents with mature promyelocytes and is associated with the **t(15;17) translocation**, which is distinct from the findings and suspected diagnosis in this patient.
*Cytarabine and daunorubicin*
- **Cytarabine and daunorubicin** constitute a common chemotherapy regimen used for **induction therapy in acute myeloid leukemia (AML)**.
- The patient's blood counts, particularly the lower blast percentage (5%) and prominent left shift with mature myeloid forms, are more consistent with a chronic myeloproliferative disorder like CML, rather than an acute leukemia that would necessitate this aggressive treatment.
Leukemias in children US Medical PG Question 5: A 4-year-old girl is brought to the physician because of a 3-week history of generalized fatigue and easy bruising. During the past week, she has also had fever and severe leg pain that wakes her up at night. Her temperature is 38.3°C (100.9°F), pulse is 120/min, and respirations are 30/min. Examination shows cervical and axillary lymphadenopathy. The abdomen is soft and nontender; the liver is palpated 3 cm below the right costal margin, and the spleen is palpated 2 cm below the left costal margin. Laboratory studies show:
Hemoglobin 10.1 g/dL
Leukocyte count 63,000/mm3
Platelet count 27,000/mm3
A bone marrow aspirate predominantly shows immature cells that stain positive for CD10, CD19, and TdT. Which of the following is the most likely diagnosis?
- A. Aplastic anemia
- B. Hodgkin lymphoma
- C. Acute lymphoblastic leukemia (Correct Answer)
- D. Acute myeloid leukemia
- E. Hairy cell leukemia
Leukemias in children Explanation: ***Acute lymphoblastic leukemia***
- The constellation of **generalized fatigue**, **easy bruising** (due to **thrombocytopenia**), fever, **severe leg pain** (bone marrow infiltration), **hepatosplenomegaly**, and **lymphadenopathy** in a child is highly suggestive of **acute leukemia**.
- The laboratory findings of **anemia** (Hb 10.1 g/dL), **thrombocytopenia** (platelet count 27,000/mm³), and a **markedly elevated leukocyte count** (63,000/mm³) with **immature cells** (blasts) in the bone marrow, staining positive for **CD10, CD19, and TdT**, are pathognomonic for **B-cell acute lymphoblastic leukemia (ALL)**.
*Aplastic anemia*
- This condition is characterized by **pancytopenia** (low levels of all blood cell types) due to bone marrow failure, but it would not typically present with **lymphadenopathy**, **hepatosplenomegaly**, or an extremely high leukocyte count with immature cells.
- The bone marrow would be **hypocellular** rather than hypercellular with blasts, as seen in this patient.
*Hodgkin lymphoma*
- While Hodgkin lymphoma can cause **lymphadenopathy** and systemic symptoms like fever and fatigue (B symptoms), it is less common in this age group and does not present with **pancytopenia** or an overwhelming presence of immature cells in the bone marrow.
- Diagnosis relies on the identification of **Reed-Sternberg cells** in lymph node biopsy.
*Acute myeloid leukemia*
- **AML** can also present with similar symptoms and pancytopenia with elevated blasts, but the immunophenotype would differ, typically showing markers like **CD13, CD33, and myeloid-specific markers**, not **CD10, CD19, and TdT**.
- **TdT** positivity is characteristic of lymphoid progenitors.
*Hairy cell leukemia*
- This is a rare, **chronic B-cell leukemia** primarily affecting older adults, not children, and is characterized by cells with **"hairy" projections**, **massive splenomegaly**, and typically **pancytopenia** without a high blast count.
- The immunophenotype involves **CD11c, CD25, CD103, and CD123**.
Leukemias in children US Medical PG Question 6: An 8-year-old girl is brought to the clinic by her parents for fever and easy bruising. Her parents report that the child has been bruising easily ever since an upper respiratory infection 3 months ago. For example, a bump into the table resulted in a large bruise on the side of her hip for a week. Three days ago, her mother noticed that the child felt warm and subsequently measured a temperature of 101.8°F (38.8°C) that did not respond to acetaminophen. The patient denies any chills, cough, rhinorrhea, pharyngitis, sick contacts, headache, or urinary symptoms. A physical examination demonstrates a nontender, firm, and rubbery node along her left neck and splenomegaly. Laboratory findings are shown below:
Leukocyte count and differential:
Leukocyte count: 19,000/mm³
Neutrophils: 39%
Bands: 12%
Eosinophils: 2%
Basophils: 0.5%
Lymphocytes: 40%
Monocytes: 6.5%
Hemoglobin: 9.7 g/dL
Platelet count: 100,000/mm³
Mean corpuscular hemoglobin concentration: 30%
Mean corpuscular volume: 76 μm³
Reticulocyte count: 0.7%
What cytogenetic abnormality would be most likely in this patient?
- A. t(9;22) - Philadelphia chromosome (BCR-ABL)
- B. t(8;14) - MYC translocation
- C. t(12;21) - TEL-AML1 translocation (Correct Answer)
- D. t(15;17) - PML-RARA translocation
- E. t(4;11) - MLL rearrangement
Leukemias in children Explanation: ***t(12;21) - TEL-AML1 translocation***
- This is the **most common cytogenetic abnormality** in pediatric B-cell acute lymphoblastic leukemia (B-ALL), occurring in approximately **25% of cases**.
- The clinical presentation of an **8-year-old child** with fever, easy bruising, pancytopenia (anemia, thrombocytopenia), lymphadenopathy, and splenomegaly is **classic for B-ALL**.
- TEL-AML1 translocation is associated with a **favorable prognosis** and is most common in children aged **2-10 years**.
- The laboratory findings show leukocytosis with lymphocytosis, anemia, and thrombocytopenia—typical of acute leukemia with bone marrow infiltration.
*t(9;22) - Philadelphia chromosome (BCR-ABL)*
- The Philadelphia chromosome occurs in only **3-5% of pediatric ALL cases** but is more common in adults (~25%).
- While it can present with similar clinical features, it is associated with a **poor prognosis** and is much less common in this age group.
- This translocation is a high-risk feature that often requires more aggressive therapy including tyrosine kinase inhibitors.
*t(8;14) - MYC translocation*
- This translocation is characteristic of **Burkitt lymphoma**, not B-ALL.
- Burkitt lymphoma typically presents with **rapidly growing masses** (often jaw or abdominal masses) rather than the pancytopenia and systemic symptoms seen in this patient.
- The clinical presentation does not fit Burkitt lymphoma.
*t(15;17) - PML-RARA translocation*
- This translocation is **pathognomonic for acute promyelocytic leukemia (APL)**, a subtype of acute myeloid leukemia (AML).
- APL typically presents with severe coagulopathy and DIC, not the lymphoid features seen in this case.
- The patient's age and presentation are not consistent with APL, which is more common in adults.
*t(4;11) - MLL rearrangement*
- MLL rearrangements are associated with **infant ALL** (particularly in children <1 year old) and confer a **poor prognosis**.
- While possible in older children, this is much less common than t(12;21) in the **8-year-old age group**.
- MLL-rearranged ALL often presents with hyperleukocytosis and CNS involvement.
Leukemias in children US Medical PG Question 7: A 5-year-old boy is brought to the physician by his parents because of a 6-week history of increased tiredness, irritability, and worsening leg pain. His parents report that he has been reluctant to walk recently because of the pain in his legs. Examination shows conjunctival pallor and diffuse petechiae. There are palpable, nontender posterior cervical and axillary lymph nodes. His hemoglobin concentration is 8.9 g/dL, leukocyte count is 45,750/mm3, and platelet count is 25,000/mm3. A bone marrow aspiration shows numerous immature cells that stain positive for CD10, CD19, and terminal deoxynucleotidyl transferase (TdT). Which of the following translocations is associated with a favorable prognosis for this patient's condition?
- A. t(15;17)
- B. t(14;18)
- C. t(12;21) (Correct Answer)
- D. t(8;14)
- E. t(9;22)
Leukemias in children Explanation: ***t(12;21)***
- The clinical presentation with **fatigue, irritability, leg pain, pallor, petechiae, lymphadenopathy**, and laboratory findings of **anemia, high leukocyte count, and thrombocytopenia** in a 5-year-old child are highly suggestive of **acute lymphoblastic leukemia (ALL)**. The presence of **CD10, CD19, and TdT positive immature cells** on bone marrow aspiration confirms the diagnosis of **B-cell ALL**.
- The **t(12;21) translocation** is one of the most common cytogenetic abnormalities found in childhood B-cell ALL and is typically associated with a **favorable prognosis** and higher rates of remission, particularly in children.
*t(15;17)*
- This translocation is characteristic of **acute promyelocytic leukemia (APML)**, a subtype of **acute myeloid leukemia (AML)**.
- APML presents with distinct features, including a high risk of **disseminated intravascular coagulation (DIC)**, and is treated with **all-trans retinoic acid (ATRA)**, which does not align with the patient's presentation of ALL.
*t(14;18)*
- This translocation is typically associated with **follicular lymphoma**, a type of **non-Hodgkin lymphoma** that primarily affects adults.
- Follicular lymphoma is a **B-cell malignancy** but presents as a solid tumor of lymphoid tissue rather than a widespread leukemia.
*t(8;14)*
- This translocation is the hallmark of **Burkitt's lymphoma**, another type of **B-cell non-Hodgkin lymphoma**.
- Burkitt's lymphoma is characterized by rapid tumor growth and often presents with an **extranodal mass**, such as in the jaw or abdomen, and is not typically associated with the widespread bone marrow involvement characteristic of ALL.
*t(9;22)*
- The **t(9;22) translocation**, known as the **Philadelphia chromosome**, is characteristic of **chronic myeloid leukemia (CML)** or, less commonly, a subset of ALL with a **poor prognosis**.
- While it can be seen in ALL, its presence generally indicates a **worse prognosis** and necessitates different treatment approaches, contrasting with the favorable outlook of t(12;21).
Leukemias in children US Medical PG Question 8: A 70-year-old retired police officer is being evaluated for fatigue. A peripheral smear shows extremely elevated numbers of immature myeloid cells, which are positive for myeloperoxidase and a translocation t(15,17). Which of the following statements is true regarding his condition?
- A. Myelodysplastic syndromes may give rise to the condition.
- B. This condition is also developed early in life in patients with Down syndrome.
- C. Philadelphia chromosome may be seen and indicates a poor prognosis.
- D. Auer rods are responsible for gum hyperplasia and bleeding.
- E. The patient can be treated with a vitamin A derivative. (Correct Answer)
Leukemias in children Explanation: ***The patient can be treated with a vitamin A derivative.***
- The presence of **immature myeloid cells** positive for **myeloperoxidase (MPO)** and a **t(15;17) translocation** strongly indicates **Acute Promyelocytic Leukemia (APL)**.
- APL is effectively treated with **all-trans retinoic acid (ATRA)**, which is a **vitamin A derivative**, as it induces differentiation of the promyelocytes.
*Myelodysplastic syndromes may give rise to the condition.*
- While myelodysplastic syndromes (MDS) can transform into other types of **acute myeloid leukemia (AML)**, they typically give rise to other subtypes of AML, not specifically APL, which has a distinct genetic translocation.
- MDS would usually show a **dysplastic morphology** in multiple cell lines, which is not described as the primary feature here.
*This condition is also developed early in life in patients with Down syndrome.*
- **Down syndrome** patients have an increased risk of specific leukemias, particularly **Acute Megakaryoblastic Leukemia (AML M7)** in early childhood, and **Acute Lymphoblastic Leukemia (ALL)**.
- APL, characterized by t(15;17), is not specifically associated with Down syndrome.
*Philadelphia chromosome may be seen and indicates a poor prognosis.*
- The **Philadelphia chromosome (t(9;22))** is characteristic of **Chronic Myeloid Leukemia (CML)** and some cases of **B-ALL**, not APL.
- The t(15;17) translocation is the defining feature of APL, and Philadelphia chromosome is not seen in this condition.
*Auer rods are responsible for gum hyperplasia and bleeding.*
- **Auer rods** are indeed characteristic of AML, including APL, and are formed by abnormal fusion of primary granules.
- However, **gum hyperplasia and bleeding** are more distinctly characteristic of **Acute Monocytic Leukemia (AML M5)** due to monocyte infiltration, rather than directly caused by Auer rods.
Leukemias in children US Medical PG Question 9: A 12-year-old boy is brought in by his mother for a routine checkup. The patient’s mother says he is frequently fatigued and looks pale. She also claims that he has recently become “much quieter” than normal and is no longer interested in playing baseball with his friends. The patient’s mother believes it may just be “growing pains.” The patient has no significant medical history. He is the 90th percentile for height and weight and has been meeting all developmental milestones. The patient is afebrile, and his vital signs are within normal limits. Physical examination reveals several small bruises on the patient’s right arm and on both thighs. Laboratory findings are significant for the following:
Sodium 140 mEq/L
Potassium 4.2 mEq/L
Chloride 101 mEq/L
Bicarbonate 27 mEq/L
BUN 16 mg/dL
Creatinine 1.2 mg/dL
Glucose (fasting) 111 mg/dL
WBC 3,400/mm3
RBC 4.20 x 106/mm3
Hematocrit 22%
Hemoglobin 7.1 g/dL
Platelet count 109,000/mm3
A peripheral blood smear reveals myeloblasts. Which of the following is the next best step in the management of this patient?
- A. Packed red blood cell transfusion
- B. Administration of oral ferrous sulfate
- C. Chest radiograph
- D. Referral to social services
- E. Bone marrow biopsy (Correct Answer)
Leukemias in children Explanation: ***Bone marrow biopsy***
- The patient's symptoms (fatigue, pallor, quiet demeanor, bruising), pancytopenia (low WBC, Hemoglobin, Platelets), and especially the presence of **myeloblasts on peripheral blood smear**, are highly suggestive of **acute leukemia**.
- A **bone marrow biopsy** is crucial for confirming the diagnosis of leukemia, classifying its type, and guiding subsequent treatment.
*Packed red blood cell transfusion*
- While the patient has significant anemia (Hb 7.1 g/dL), a transfusion would address the symptom of anemia but not the underlying cause.
- Without a definitive diagnosis, a transfusion is a supportive measure, not the next best diagnostic or management step in this scenario given the strong suspicion of leukemia.
*Administration of oral ferrous sulfate*
- The anemia presented is likely due to bone marrow failure from leukemia, not **iron deficiency**.
- Treating with oral iron would be ineffective and delay the correct diagnosis and treatment of the underlying malignancy.
*Chest radiograph*
- A chest radiograph might be indicated later to assess for mediastinal involvement or infection, but it is not the immediate next step for diagnosing the suspected hematological malignancy.
- The primary diagnostic concern here is the abnormal blood counts and myeloblasts, which point towards a bone marrow issue.
*Referral to social services*
- While the presence of bruises might raise suspicion for abuse in other contexts, the constellation of symptoms here (fatigue, pallor, pancytopenia with myeloblasts) strongly points to an underlying medical condition, specifically **acute leukemia**.
- Focusing on a social work referral at this stage would delay critical medical diagnosis and intervention.
Leukemias in children US Medical PG Question 10: A 7-year-old girl is brought to the physician by her mother because of a 2-week history of generalized fatigue, intermittent fever, and progressively worsening shortness of breath. Physical examination shows pallor, jugular venous distention, and nontender cervical and axillary lymphadenopathy. Inspiratory stridor is heard on auscultation of the chest. The liver is palpated 3 cm below the right costal margin. Her hemoglobin concentration is 9.5 g/dL, leukocyte count is 66,000/mm³, and platelet count is 102,000/mm³. An x-ray of the chest shows a mediastinal mass. A bone marrow aspirate predominantly shows leukocytes and presence of 35% lymphoblasts. Which of the following additional findings is most likely in this patient?
- A. t(8;14) translocation
- B. Positive myeloperoxidase staining
- C. Positive CD3/CD7 staining (Correct Answer)
- D. t(9;22) translocation
- E. Reed-Sternberg cells
Leukemias in children Explanation: ***Positive CD3/CD7 staining***
- The presence of a **mediastinal mass** with **T-cell lymphoblastic leukemia/lymphoma (T-ALL)** is highly associated with a **T-cell immunophenotype**. **CD3** and **CD7** are **T-cell surface markers**.
- The constellation of findings, including **lymphadenopathy**, **hepatomegaly**, **bone marrow involvement** with 35% lymphoblasts, and a **mediastinal mass** causing **stridor**, is classic for T-ALL, which is typically of T-cell origin.
*t(8;14) translocation*
- This translocation is characteristic of **Burkitt lymphoma**, which typically presents as an **extranodal mass** (e.g., jaw, abdomen) rather than a primary mediastinal mass causing stridor.
- While Burkitt lymphoma is also a B-cell non-Hodgkin lymphoma and can have bone marrow involvement, the clinical picture here is not typical for Burkitt lymphoma.
*Positive myeloperoxidase staining*
- **Myeloperoxidase** is an enzyme found in the granules of **myeloid cells**, and its staining is characteristic of **acute myeloid leukemia (AML)**.
- While the patient has leukocytosis and anemia, the predominance of **lymphoblasts** in the bone marrow aspirate points away from AML.
*t(9;22) translocation*
- The **Philadelphia chromosome**, associated with **t(9;22) translocation**, is highly characteristic of **chronic myeloid leukemia (CML)** and can be seen in a subset of **B-cell acute lymphoblastic leukemia (B-ALL)**.
- However, the clinical presentation with a large mediastinal mass causing stridor is more typical of T-ALL, which is not strongly associated with t(9;22).
*Reed-Sternberg cells*
- **Reed-Sternberg cells** are the hallmark of **Hodgkin lymphoma**.
- While Hodgkin lymphoma can present with **mediastinal mass** and **lymphadenopathy**, it typically affects older children/adolescents or young adults, and the presence of **35% lymphoblasts** in the bone marrow indicates leukemia, not Hodgkin lymphoma.
More Leukemias in children US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.