Diagnostic approach to pediatric malignancies US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Diagnostic approach to pediatric malignancies. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Diagnostic approach to pediatric malignancies US Medical PG Question 1: A 24-year-old woman complains of intermittent fever and joint pain. She says that these symptoms have been present for the past month. Before that, she had no signs or symptoms and was completely healthy. She has also lost her appetite and some weight. A complete blood count (CBC) showed severe pancytopenia. What is the next best step in evaluating this patient?
- A. Repeated CBCs for several weeks and reassess
- B. Treatment with corticosteroids
- C. Treatment with antibiotics
- D. Treatment for acute leukemia
- E. Bone marrow examination (Correct Answer)
Diagnostic approach to pediatric malignancies Explanation: ***Bone marrow examination***
- The combination of **fever**, **joint pain**, **weight loss**, and **pancytopenia** in a previously healthy young woman raises suspicion for serious hematologic conditions like **aplastic anemia** or **acute leukemia**.
- A **bone marrow examination** is crucial for definitive diagnosis by evaluating the cellularity, morphology, and presence of abnormal cells.
*Repeated CBCs for several weeks and reassess*
- This approach is inappropriate given the **severe pancytopenia** and progressive symptoms, which indicate an urgent underlying pathology.
- Delaying diagnosis could worsen the patient's condition and compromise treatment outcomes due to the potential for severe infections or bleeding.
*Treatment with corticosteroids*
- While corticosteroids might be used in some autoimmune conditions causing pancytopenia, initiating treatment without a definitive diagnosis is premature and could mask the underlying cause, especially in cases of malignancy.
- There is no specific indication for corticosteroid use in this scenario without further diagnostic information.
*Treatment with antibiotics*
- Although **fever** is present, there's no clear evidence of an infection (like localized symptoms or positive cultures), and **pancytopenia** is not primarily managed with antibiotics.
- Administering antibiotics empirically without a confirmed infection addresses a symptom rather than the underlying progressive hematological disorder.
*Treatment for acute leukemia*
- While **acute leukemia** is a strong possibility, definitive treatment should only commence after a confirmed diagnosis through **bone marrow examination**, as misdiagnosis can lead to inappropriate and harmful therapy.
- Other conditions like severe aplastic anemia also present with similar features but require different management strategies.
Diagnostic approach to pediatric malignancies US Medical PG Question 2: A 3-year-old girl is brought to her pediatrician with 2 days of fever and abdominal pain. She has also been crying and complaining of pain while urinating. She was born at term without incident and was previously healthy at regular checkups. On presentation, her temperature is 102.2°F (39°C), blood pressure is 137/85 mmHg, pulse is 122/min, and respirations are 24/min. Physical exam reveals a palpable, painless, abdominal mass that does not cross the midline. Which of the following additional findings would be associated with this patient's disorder?
- A. Ash leaf spots
- B. Opsoclonus myoclonus
- C. Epstein-Barr virus
- D. 11;22 chromosome translocation
- E. Aniridia (Correct Answer)
Diagnostic approach to pediatric malignancies Explanation: ***Aniridia***
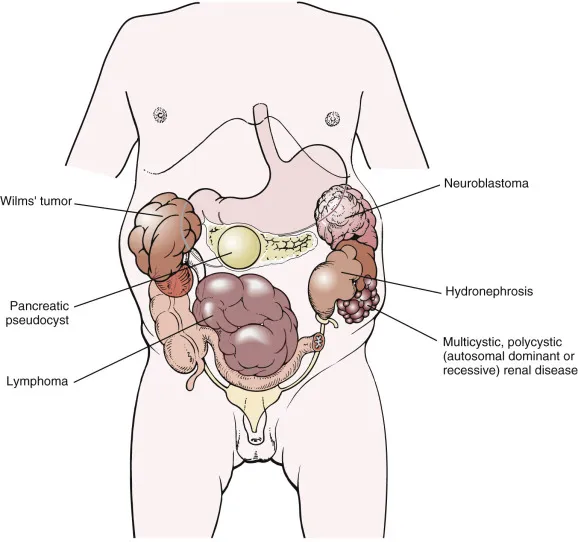
- The clinical presentation of a **palpable, painless abdominal mass** that does not cross the midline, along with **hypertension** and symptoms suggesting a urinary tract infection (fever, dysuria, abdominal pain) in a 3-year-old girl, is highly indicative of **Wilms tumor (nephroblastoma)**.
- **Aniridia** (absence of the iris) is a congenital anomaly strongly associated with **Wilms tumor**, particularly as part of the **WAGR syndrome** (Wilms tumor, Aniridia, Genitourinary anomalies, and intellectual disability), caused by a deletion on chromosome 11 that includes the *WT1* gene.
*Ash leaf spots*
- **Ash leaf spots** are hypopigmented macules characteristic of **tuberous sclerosis complex**, a genetic disorder associated with hamartomas in various organs, including the brain, kidney, heart, and skin.
- While tuberous sclerosis can be associated with kidney lesions (e.g., angiomyolipomas), it does not typically present with a solitary renal mass like a Wilms tumor, nor are ash leaf spots directly linked to nephroblastoma.
*Opsoclonus myoclonus*
- **Opsoclonus-myoclonus syndrome (OMS)**, also known as **dancing eyes-dancing feet syndrome**, is a rare neurological disorder characterized by rapid, chaotic eye movements (opsoclonus) and involuntary muscle jerks (myoclonus).
- In children, OMS is most commonly a **paraneoplastic syndrome associated with neuroblastoma**, a tumor of the sympathetic nervous system, which typically presents with an abdominal mass that **often crosses the midline** and can present with systemic symptoms like pallor and periorbital ecchymoses, rather than the specific renal origin suggested by the lack of midline crossing.
*Epstein-Barr virus*
- The **Epstein-Barr virus (EBV)** is the causative agent of **infectious mononucleosis** and is implicated in various lymphoproliferative disorders and certain cancers, such as **Burkitt lymphoma** and nasopharyngeal carcinoma.
- While Burkitt lymphoma can present as an abdominal mass, EBV is not directly associated with Wilms tumor.
*11;22 chromosome translocation*
- The **t(11;22)(q24;q12) translocation** is the characteristic cytogenetic abnormality found in **Ewing sarcoma**, a highly aggressive malignant tumor of bone and soft tissue.
- Ewing sarcoma can present as a soft tissue mass, but it is not a renal tumor and does not typically present with the specific clinical features of Wilms tumor such as severe hypertension or aniridia.
Diagnostic approach to pediatric malignancies US Medical PG Question 3: An 18-month-old boy is brought to the doctor’s office for evaluation of abdominal pain. The boy looks emaciated and he is now significantly below his growth chart predicted weight. The family history is non-contributory. The vital signs are unremarkable. On physical examination, a non-tender mass is felt in the upper part of the abdomen. A magnetic resonance image (MRI) scan of his abdomen demonstrates a mass in his right adrenal gland. Biopsy of the mass demonstrates an abundance of small round blue cells. With this biopsy result, which 1 of the following findings would confirm the diagnosis?
- A. Elevation of vanillylmandelic acid in the urine (Correct Answer)
- B. MRI showing the intrarenal origin of the mass
- C. Increased lactic dehydrogenase
- D. Increased alpha-fetoprotein
- E. Radiograph of the bone showing the presence of lytic bone lesion with periosteal reaction
Diagnostic approach to pediatric malignancies Explanation: ***Elevation of vanillylmandelic acid in the urine***
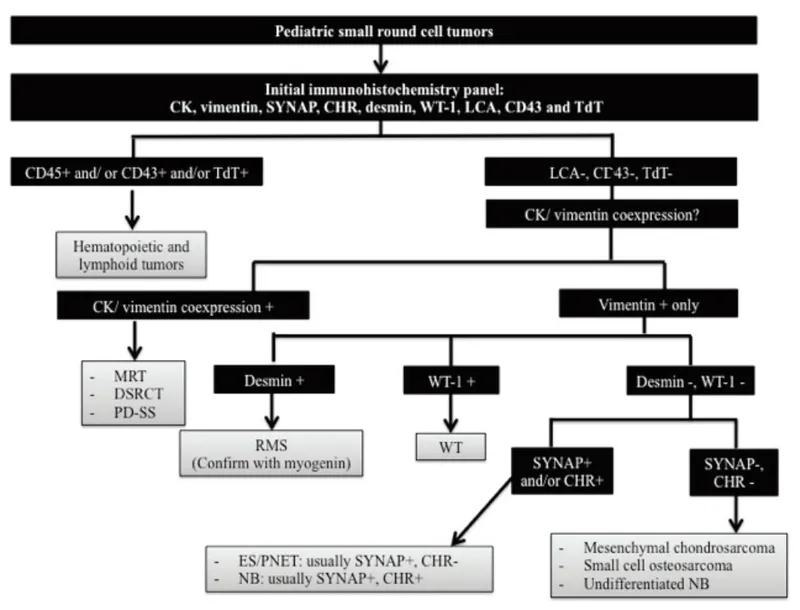
- The clinical presentation (abdominal mass, emaciation, age) and biopsy finding of **small round blue cells** in the adrenal gland are highly suggestive of **neuroblastoma**.
- **Neuroblastomas** arise from neural crest cells and characteristically produce **catecholamines**, leading to elevated urinary levels of their metabolites like **vanillylmandelic acid (VMA)** and **homovanillic acid (HVA)**.
*MRI showing the intrarenal origin of the mass*
- An **intrarenal origin** of the mass would suggest a **Wilms tumor** (nephroblastoma), which is another common pediatric abdominal malignancy.
- However, the mass is described as being in the **adrenal gland**, and the biopsy shows small round blue cells, which are characteristic of neuroblastoma rather than Wilms tumor.
*Increased lactic dehydrogenase*
- Elevated **lactic dehydrogenase (LDH)** is a non-specific tumor marker often associated with a high tumor burden and rapid cell turnover in various malignancies, including neuroblastoma.
- While it can be elevated in neuroblastoma, it is not a specific diagnostic marker and would not confirm the diagnosis over other pediatric cancers.
*Increased alpha-fetoprotein*
- Elevated **alpha-fetoprotein (AFP)** is primarily associated with **hepatoblastoma** and **germ cell tumors**.
- It is not typically elevated in neuroblastoma and would therefore not confirm this diagnosis.
*Radiograph of the bone showing the presence of lytic bone lesion with periosteal reaction*
- While **neuroblastoma** can metastasize to bones, causing **lytic bone lesions** and a periosteal reaction, these findings indicate metastatic disease rather than confirming the primary diagnosis.
- A bone radiograph showing such lesions points to advanced disease but doesn't specifically confirm neuroblastoma as the primary tumor type.
Diagnostic approach to pediatric malignancies US Medical PG Question 4: A 6-month-old boy is brought to the emergency department by his mother, who informs the doctor that her alcoholic husband hit the boy hard on his back. The blow was followed by excessive crying for several minutes and the development of redness in the area. On physical examination, the boy is dehydrated, dirty, and irritable and when the vital signs are checked, they reveal tachycardia. He cries immediately upon the physician touching the area around his left scapula. The doctor strongly suspects a fracture of the 6th, 7th, or 8th retroscapular posterior ribs. Evaluation of his skeletal survey is normal. The clinician is concerned about child abuse in this case. Which of the following is the most preferred imaging technique as the next step in the diagnostic evaluation of the infant?
- A. Bedside ultrasonography
- B. Magnetic resonance imaging
- C. Babygram
- D. Chest computed tomography scan
- E. Skeletal survey in 2 weeks (Correct Answer)
Diagnostic approach to pediatric malignancies Explanation: ***Skeletal survey in 2 weeks***
- A repeat **skeletal survey in 2 weeks** is the most appropriate next step in suspected child abuse cases with an initial normal survey, as it allows for the detection of **healing fractures** that may not be apparent immediately after injury.
- New bone formation and callus development around a fracture site become radiographically visible after approximately 7 to 14 days, improving the detection rate of subtle or undisplaced fractures.
*Bedside ultrasonography*
- While **ultrasonography** can detect acute fractures, especially in cartilage and non-ossified bones, its utility in a comprehensive assessment for multiple non-displaced rib fractures as part of a child abuse workup is limited.
- It is highly **operator-dependent** and may not provide the full skeletal overview required in suspected child abuse.
*Magnetic resonance imaging*
- **MRI** is excellent for evaluating soft tissue injuries, bone marrow edema, and non-ossified cartilaginous structures. However, it is not the primary imaging modality for detecting acute or subacute fractures of ossified bone and requires **sedation** in infants, making it less practical for routine skeletal screening.
- The **high cost** and limited availability of MRI also make it less suitable as a first-line diagnostic tool for rib fractures in this context.
*Babygram*
- A **babygram** is a single large radiograph of an infant's entire body, often used to rapidly assess for gross developmental anomalies or immediate concerns.
- It provides **less detailed imaging** of individual bones compared to a standard skeletal survey and is insufficient for reliably detecting subtle or non-displaced rib fractures.
*Chest computed tomography scan*
- A **chest CT scan** is highly sensitive for detecting acute rib fractures, even subtle ones. However, it exposes the infant to **significant radiation** and is usually reserved for specific clinical indications, such as suspected internal organ injury, rather than as a primary screening tool for rib fractures in child abuse in an otherwise stable patient.
- It does not provide a comprehensive view of the entire skeleton, which is crucial for identifying other potential abuse-related injuries elsewhere.
Diagnostic approach to pediatric malignancies US Medical PG Question 5: A 7-year-old boy presents to his primary care physician for a general checkup. The patient has been feeling poorly for the past several weeks and has been losing weight. He states that he often feels weak and too tired to play with his friends. He is no longer interested in many recreational activities he used to be interested in. The patient's parents state that a few of their child's friends have been sick lately. His temperature is 102°F (38.9°C), blood pressure is 77/48 mmHg, pulse is 110/min, respirations are 24/min, and oxygen saturation is 98% on room air. On exam, you note a fatigued appearing child who has lost 10 pounds since his last appointment. Left upper quadrant tenderness and a mass is noted on abdominal exam. Which of the following best describes the most likely diagnosis?
- A. Smudge cells on peripheral smear
- B. TdT positive cells (Correct Answer)
- C. Infection sensitive to oseltamivir
- D. Auer rods on peripheral smear
- E. Parental mistreatment of the child
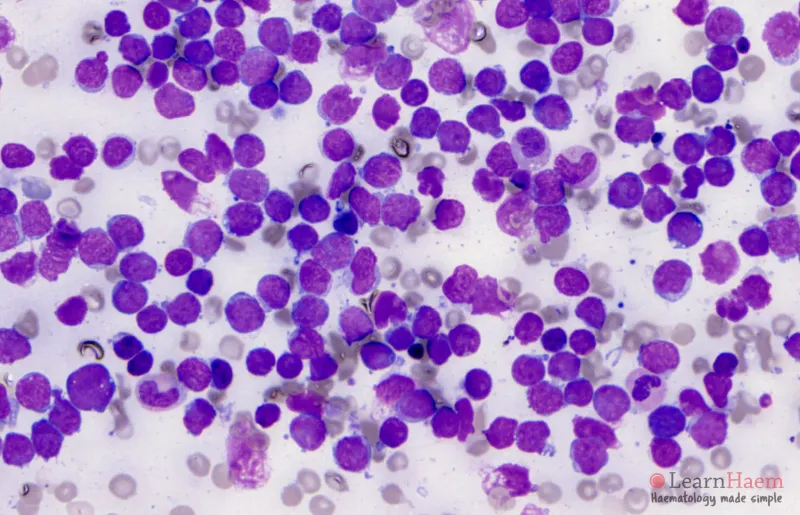
Diagnostic approach to pediatric malignancies Explanation: ***TdT positive cells***
- This patient's symptoms, including **fever**, **weight loss**, **fatigue**, and **splenomegaly** (left upper quadrant tenderness and mass), are highly suggestive of **Acute Lymphoblastic Leukemia (ALL)**.
- **Terminal deoxynucleotidyl transferase (TdT)** is a DNA polymerase found in immature lymphocytes (blasts) and is a key marker for diagnosing ALL.
- ALL is the **most common childhood malignancy**, particularly prevalent in children aged 2-10 years.
*Smudge cells on peripheral smear*
- **Smudge cells** are characteristic of **Chronic Lymphocytic Leukemia (CLL)**, which predominantly affects older adults and is rare in children.
- The clinical picture of rapid decline and significant systemic symptoms in a child is inconsistent with CLL.
*Infection sensitive to oseltamivir*
- Oseltamivir is an **antiviral medication for influenza**, and while the child has a fever, the profound **weight loss**, **fatigue**, and **abdominal mass** point towards a hematologic malignancy, not a typical viral infection.
- Viral infections rarely present with such a significant abdominal mass or sustained constitutional symptoms for several weeks.
*Auer rods on peripheral smear*
- **Auer rods** are cytoplasmic inclusions pathognomonic for **Acute Myeloid Leukemia (AML)**.
- While AML can occur in children, **ALL is far more common in this age group** (85% of childhood leukemias), and the presentation is highly classic for ALL, making TdT positivity the best diagnostic marker.
*Parental mistreatment of the child*
- While some symptoms (weight loss, fatigue) could potentially be seen in neglect, the presence of **fever**, **splenomegaly** (abdominal mass), and **hypotension** points strongly to a severe underlying medical condition.
- Objective signs of systemic illness necessitate a thorough medical workup rather than suspicion of abuse.
Diagnostic approach to pediatric malignancies US Medical PG Question 6: An inconsolable mother brings her 2-year-old son to the emergency room after finding a large amount of bright red blood in his diaper, an hour ago. She states that for the past week her son has been having crying fits while curling his legs towards his chest in a fetal position. His crying resolves either after vomiting or passing fecal material. Currently, the child is in no apparent distress. Physical examination with palpation in the gastric region demonstrates no acute findings. X-ray of the abdominal area demonstrates no acute findings. His current temperature is 36.5°C (97.8°F), heart rate is 93/min, blood pressure is 100/64 mm Hg, and respiratory rate is 26/min. His weight is 10.8 kg (24.0 lb), and height is 88.9 cm (35.0 in). Laboratory tests show the following:
RBC count 5 million/mm3
Hematocrit 36%
Hemoglobin 12 g/dL
WBC count 6,000/mm3
Mean corpuscular volume 78 fL
What is the most likely underlying embryological cause predisposing to this condition?
- A. Failure of the vitelline duct to close (Correct Answer)
- B. Failure of the vitelline duct to open
- C. Elevated anti-mitochondrial antibodies
- D. Problem with bilirubin conjugation
- E. Problem with bilirubin uptake
Diagnostic approach to pediatric malignancies Explanation: ***Failure of the vitelline duct to close***
- The clinical presentation of a 2-year-old with recurrent episodes of abdominal pain, crying spells (curling legs to chest), and the passage of bright red blood in the diaper is highly suggestive of **intussusception**. This can be transiently relieved when the "curled" bowel straightens itself out, or gas/fecal matter is passed. The presence of **bright red blood** (often referred to as **currant jelly stools** when mixed with mucus) further supports this diagnosis, indicating ischemic bowel.
- In children, intussusception is often idiopathic, but in a small percentage of cases, especially in older infants and children, an **anatomical lead point** can cause it. The most common anatomical lead point is a **Meckel's diverticulum**, which results from the **incomplete obliteration of the vitelline duct** (also known as the omphalomesenteric duct) during embryological development. The diverticulum can act as a foreign body that then telescopes into the adjacent bowel, causing intussusception.
*Failure of the vitelline duct to open*
- The vitelline duct should normally regress and disappear. Therefore, a "failure to open" is not a recognized embryological anomaly or pathology.
- Problems related to the vitelline duct involve either its **incomplete closure** (leading to Meckel's diverticulum, vitelline cysts, or fistulas) or other abnormal remnants, not a failure to open.
*Elevated anti-mitochondrial uptake*
- This option refers to **anti-mitochondrial antibodies (AMAs)**, which are characteristic markers for **primary biliary cholangitis (PBC)**, an autoimmune disease primarily affecting the liver.
- PBC is an adult-onset condition and is not associated with intussusception or the gastrointestinal symptoms described in the child.
*Problem with bilirubin conjugation*
- Issues with **bilirubin conjugation** primarily manifest as different types of **jaundice** (e.g., Crigler-Najjar syndrome, Gilbert's syndrome) due to the accumulation of unconjugated bilirubin.
- These conditions do not cause abdominal pain, intussusception, or bloody stools.
*Problem with bilirubin uptake*
- Problems with **bilirubin uptake** by hepatocytes also lead to **unconjugated hyperbilirubinemia** and jaundice.
- This condition is unrelated to acute abdominal emergencies like intussusception or gastrointestinal bleeding.
Diagnostic approach to pediatric malignancies US Medical PG Question 7: A 68-year-old man presents to the emergency department complaining of difficulty in breathing for the past 2 days. He has had recurrent episodes of bacterial pneumonia in the right lower lobe during the last 6 months. His last episode of pneumonia started 7 days ago for which he is being treated with antibiotics. He has a 35-pack-year smoking history. Past medical history is significant for hypertension for which he takes lisinopril. Physical examination reveals decreased breath sounds and dullness to percussion in the right lung base. Chest X-ray reveals a large right-sided pleural effusion, and chest CT scan shows a large mass near the hilum of the right lung. Cytologic examination of pleural fluid shows evidence of malignancy. Which of the following is the most likely diagnosis of this patient?
- A. Small cell lung cancer
- B. Non-small cell lung cancer (Correct Answer)
- C. Metastatic lung disease
- D. Pulmonary hamartoma
- E. Mesothelioma
Diagnostic approach to pediatric malignancies Explanation: ***Non-small cell lung cancer***
- The patient's **35-pack-year smoking history**, recurrent **right lower lobe pneumonia**, large **pleural effusion**, and a **hilar mass** with **malignant cells** in the pleural fluid are highly suggestive of **non-small cell lung cancer (NSCLC)**.
- NSCLC is the most common type of lung cancer and often presents with features like **post-obstructive pneumonia** due to airway obstruction by the tumor, and **pleural effusions** indicating advanced disease.
*Small cell lung cancer*
- While associated with smoking and can present with hilar masses, **small cell lung cancer (SCLC)** typically has a more aggressive course with earlier onset of paraneoplastic syndromes and widespread metastases at diagnosis.
- The presenting features in this case, particularly the recurrent pneumonia and large pleural effusion, are more commonly seen with NSCLC.
*Metastatic lung disease*
- Metastatic lung disease would imply cancer originating from another primary site, but the presence of a **large hilar mass** points to a lung primary.
- While metastases can cause pleural effusions, the clinical picture strongly favors a **primary lung malignancy** in a heavy smoker.
*Pulmonary hamartoma*
- A **pulmonary hamartoma** is a benign tumor and would not cause a large pleural effusion with malignant cells or recurrent pneumonia due to airway obstruction.
- They are typically asymptomatic and discovered incidentally.
*Mesothelioma*
- **Mesothelioma** is a rare cancer primarily associated with **asbestos exposure**, which is not mentioned in the patient's history.
- It arises from the pleura and often presents with a diffuse pleural thickening rather than a distinct hilar mass.
Diagnostic approach to pediatric malignancies US Medical PG Question 8: A 75-year-old man presents to the physician because of bloody urine, which has occurred several times over the past month. He has no dysuria, flank pain, nausea, or vomiting. He has no history of serious illness and takes no medications. He is a 40-pack-year smoker. The vital signs are within normal limits. Physical exam shows no abnormalities except generalized lung wheezing. The laboratory test results are as follows:
Urine
Blood 3+
RBC > 100/hpf
WBC 1–2/hpf
RBC casts Negative
Bacteria Not seen
Which of the following is the most appropriate diagnostic study at this time?
- A. Intravenous (IV) pyelography
- B. Computed tomography (CT) urogram
- C. Cystoscopy (Correct Answer)
- D. Chest X-ray
- E. Ureteroscopy
Diagnostic approach to pediatric malignancies Explanation: ***Cystoscopy***
- Given the patient's age, history of **40-pack-year smoking**, and **painless gross hematuria** without signs of infection or renal disease, there is a high suspicion for **bladder cancer**.
- **Cystoscopy** is the **most appropriate initial diagnostic study** because it allows **direct visualization of the bladder mucosa** and enables **immediate biopsy** of any suspicious lesions.
- The clinical presentation (painless hematuria + smoking history + absence of upper tract symptoms) strongly suggests a **bladder origin**, making cystoscopy the highest-yield diagnostic test.
- Per **AUA guidelines**, cystoscopy is essential for all patients with gross hematuria and risk factors for urothelial malignancy.
*Intravenous (IV) pyelography*
- This older imaging modality has been **largely replaced by CT urogram** due to lower sensitivity and poorer visualization of both upper and lower urinary tract structures.
- It cannot provide direct mucosal visualization or tissue diagnosis.
*Computed tomography (CT) urogram*
- A **CT urogram** is excellent for evaluating the **upper urinary tract** (kidneys, ureters) and is typically part of a complete hematuria workup.
- However, when the clinical picture strongly suggests **bladder pathology** (as in this case), **cystoscopy is the more direct and definitive diagnostic test**.
- CT urogram would be complementary imaging but cannot replace cystoscopy for evaluating the bladder mucosa and obtaining tissue diagnosis.
- In practice, both studies are often performed, but cystoscopy is the **most appropriate initial study** for suspected bladder cancer.
*Chest X-ray*
- While the patient has **wheezing** (likely related to his smoking history), a chest X-ray does not evaluate the source of **hematuria**.
- It might be useful for staging if bladder cancer is confirmed, but it is not the appropriate diagnostic study for evaluating urinary tract bleeding.
*Ureteroscopy*
- **Ureteroscopy** is indicated for evaluating and treating lesions within the **ureters or renal pelvis**, typically after imaging suggests an upper tract abnormality.
- It is more invasive than cystoscopy and is not the first-line approach when clinical features point to a **bladder source**.
- There are no signs suggesting upper tract pathology (no flank pain, no hydronephrosis).
Diagnostic approach to pediatric malignancies US Medical PG Question 9: A 2-year-old boy is brought to the physician because of progressive difficulty breathing and a productive cough for the past 2 days. During the past 6 months, he has had recurrent episodes of pneumonia treated with antibiotics. He has not gained weight in this time period. His temperature is 38.5°C (101.3°F), pulse is 130/min, respirations are 18/min, and blood pressure is 100/60 mm Hg. Auscultation of the lungs shows decreased breath sounds over the right lung fields. Ocular examination shows periorbital subcutaneous bleeding and bulging of both eyes. His leukocyte count is 16,000/mm3. An x-ray of the chest shows a right-sided opacity and a collapsed right lung. An MRI of the chest shows a heterogeneous mass in the posterior mediastinum that compresses the heart and the great vessels to the left side. Further evaluation is most likely to show which of the following?
- A. Unregulated B-cell proliferation in the mediastinum
- B. Acid-fast bacteria on sputum microscopy
- C. Increased lymphoblast count in the bone marrow
- D. Overexpression of the N-myc oncogene (Correct Answer)
- E. Autoantibodies against nicotinic acetylcholine receptors
Diagnostic approach to pediatric malignancies Explanation: ***Overexpression of the N-myc oncogene***
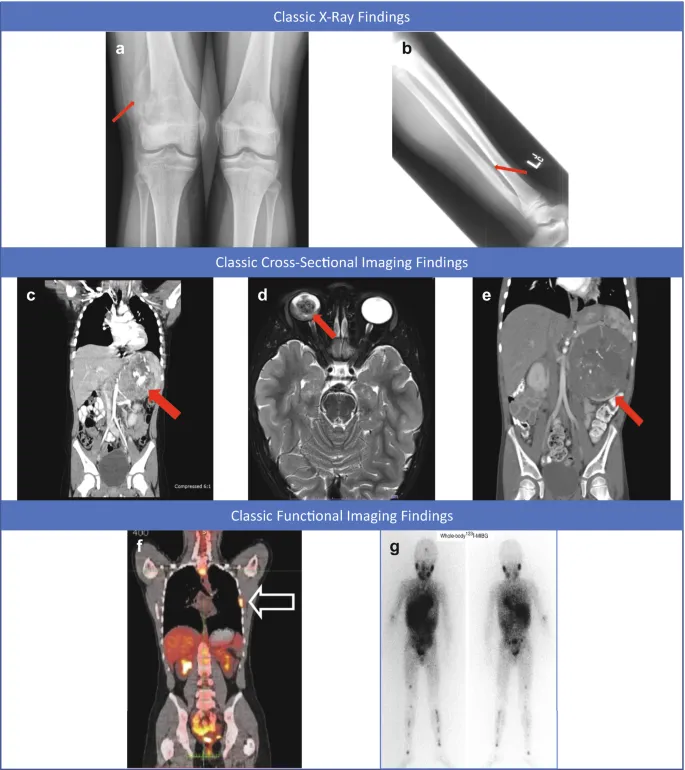
- The combination of a posterior mediastinal mass, periorbital bruising (**raccoon eyes**), and proptosis in a 2-year-old child with recurrent infections and failure to thrive is highly suggestive of **neuroblastoma**.
- **N-myc oncogene amplification** is a common genetic abnormality found in high-risk neuroblastoma and correlates with aggressive disease and poor prognosis.
*Unregulated B-cell proliferation in the mediastinum*
- This would suggest a **lymphoma**, which typically presents with anterior or superior mediastinal masses and often involves lymphadenopathy.
- The specific ocular findings of periorbital ecchymoses and proptosis are not characteristic of lymphoma but are classic for metastatic neuroblastoma.
*Acid-fast bacteria on sputum microscopy*
- This finding is indicative of **tuberculosis**, which can cause mediastinal lymphadenopathy and pulmonary symptoms.
- However, tuberculosis would not typically cause a large heterogeneous posterior mediastinal mass with associated periorbital ecchymoses and proptosis.
*Increased lymphoblast count in the bone marrow*
- This points to **acute lymphoblastic leukemia (ALL)**. While ALL can cause mediastinal masses (T-cell ALL often presents with an anterior mediastinal mass) and systemic symptoms, the **periorbital bruising and proptosis** are specific features that distinguish neuroblastoma.
- Also, a significantly increased lymphoblast count in the bone marrow is the defining diagnostic criterion for leukemia, which is not directly suggested by the initial presentation beyond general systemic illness.
*Autoantibodies against nicotinic acetylcholine receptors*
- This finding is characteristic of **myasthenia gravis**, an autoimmune neuromuscular disorder.
- Myasthenia gravis presents with **muscle weakness and fatigue**, not a posterior mediastinal mass, recurrent pneumonia, failure to thrive, or ocular bulging/bruising as described.
Diagnostic approach to pediatric malignancies US Medical PG Question 10: A 5-year-old boy is brought to the pediatric clinic for evaluation of fever, pain, swelling in the left leg, and limping. Review of systems and history is otherwise unremarkable. The vital signs include: pulse 110/min, temperature 38.1°C (100.6°F), and blood pressure 100/70 mm Hg. On examination, there is a tender swelling over the lower part of his left leg. Which 1 of the following X-ray findings is most suggestive of Ewing’s sarcoma?
- A. Mixed lytic and blastic appearance in the X-ray
- B. X-ray showing broad-based projections from the surface of the bone
- C. X-ray showing lytic bone lesion with periosteal reaction (Correct Answer)
- D. X-ray showing a sharply marginated radiolucent area within the apophysis
- E. X-ray showing deep muscle plane displacement from the metaphysis
Diagnostic approach to pediatric malignancies Explanation: ***X-ray showing lytic bone lesion with periosteal reaction***
- **Ewing's sarcoma** typically presents as a **lytic bone lesion** with an **aggressive periosteal reaction**, often described as an **"onion-skin" appearance** due to layers of new bone formation.
- The combination of fever, localized pain, swelling, and limping in a child, along with a lytic lesion and periosteal reaction on X-ray, is highly suggestive of this diagnosis.
*Mixed lytic and blastic appearance in the X-ray*
- A mixed lytic and blastic appearance is more characteristic of metastatic disease or certain other bone tumors like osteosarcoma in later stages, but less specific for primary Ewing's sarcoma.
- While some blastic components can occur, the primary hallmark of Ewing's is its lytic and destructive nature with typical periosteal reactions.
*X-ray showing broad-based projections from the surface of the bone*
- Broad-based projections from the bone surface are characteristic of **osteochondromas**, which are benign bone tumors.
- These are typically painless unless they impinge on nerves or blood vessels, and do not usually present with systemic symptoms like fever.
*X-ray showing a sharply marginated radiolucent area within the apophysis*
- A sharply marginated radiolucent area within the apophysis could suggest a benign lesion like a **fibrous cortical defect** or a **non-ossifying fibroma**, particularly if it is well-defined and non-aggressive.
- It does not indicate the aggressive, destructive nature seen with Ewing's sarcoma.
*X-ray showing deep muscle plane displacement from the metaphysis*
- Deep muscle plane displacement can indicate a significant soft tissue mass, but it is a **non-specific finding** and does not point directly to the bony destruction or characteristic periosteal reaction of Ewing's sarcoma.
- This finding could be associated with various soft tissue tumors, hematomas, or infections.
More Diagnostic approach to pediatric malignancies US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.