Common pediatric cancers

On this page
🎯 The Pediatric Cancer Landscape: Childhood's Greatest Challenge
Pediatric cancers strike differently than adult malignancies-they emerge from developing tissues, progress rapidly, and demand entirely distinct therapeutic approaches that balance cure with preserving growth potential. You'll master the critical triad of hematologic malignancies, CNS tumors, and solid tissue invaders that account for nearly all childhood cancers, learning to recognize their unique presentations, navigate risk-stratified treatment algorithms, and anticipate the long-term survivorship challenges that follow your young patients into adulthood. This knowledge transforms you from observer to advocate, equipped to deliver precision oncology while safeguarding the futures of your most vulnerable patients.
📌 Remember: CHILD mnemonic for pediatric cancer characteristics - Congenital predisposition, High cure rates, Immature tissue origin, Long-term survivorship issues, Developmental considerations in treatment
Epidemiological Foundation
Pediatric cancers affect approximately 1 in 285 children before age 20, with distinct patterns:
- Peak incidence: Ages 2-5 years (38.2 per 100,000)
- Secondary peak: Adolescence 15-19 years (23.1 per 100,000)
- Male predominance: 1.2:1 ratio across most tumor types
- Survival improvement: From 58% (1970s) to 84% (current era)
| Cancer Type | Peak Age | 5-Year Survival | Incidence Rate | Key Features |
|---|---|---|---|---|
| ALL | 2-5 years | 91% | 26.3/100,000 | B-cell predominant |
| Brain Tumors | 5-9 years | 75% | 21.8/100,000 | Location-dependent |
| Neuroblastoma | <2 years | 81% | 6.2/100,000 | Adrenal primary |
| Wilms Tumor | 2-4 years | 93% | 5.1/100,000 | Renal origin |
| Lymphomas | 10-14 years | 88% | 13.7/100,000 | NHL > HL in children |
Biological Distinctions
Pediatric malignancies demonstrate unique characteristics:
- Embryonal origin: 60% derive from primitive neural crest, mesenchymal, or blastema cells
- Rapid doubling time: 24-48 hours vs 60-200 days in adult cancers
- Chemosensitivity: 85% respond to multiagent protocols
- Metastatic potential: Lower than adult counterparts at diagnosis
💡 Master This: Childhood cancers grow rapidly but respond dramatically to treatment because they retain embryonal characteristics - high mitotic rates, undifferentiated cell types, and preserved apoptotic pathways
Understanding these foundational principles establishes the framework for recognizing specific tumor presentations and optimizing age-appropriate treatment strategies that maximize cure while minimizing long-term sequelae.
🎯 The Pediatric Cancer Landscape: Childhood's Greatest Challenge
🧬 Hematologic Malignancies: The Blood Cell Uprising
📌 Remember: BLASTS mnemonic for leukemia recognition - Bone marrow >20% blasts, Lymphadenopathy, Anemia/bleeding, Splenomegaly, Thrombocytopenia, Systemic symptoms
Acute Lymphoblastic Leukemia (ALL) Mastery
ALL represents 25% of all pediatric cancers with remarkable cure rates:
- Peak incidence: Ages 2-5 years (80% of pediatric leukemias)
- B-cell lineage: 85% of cases
- Hyperdiploidy: 25% of cases (excellent prognosis)
- Philadelphia chromosome: 3-5% (historically poor, improving with TKIs)
| Risk Category | Criteria | Treatment Duration | Cure Rate | Key Features |
|---|---|---|---|---|
| Standard Risk | Age 1-9, WBC <50K | 2-2.5 years | 95% | Hyperdiploidy favorable |
| High Risk | Age >10, WBC >50K | 2.5-3 years | 85% | T-cell lineage |
| Very High Risk | Philadelphia+, MLL+ | 3+ years + BMT | 70% | Intensive protocols |
| Infant ALL | Age <1 year | Variable | 60% | MLL rearrangements |
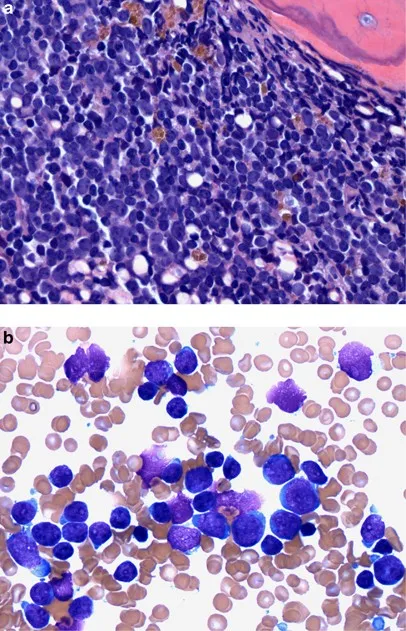
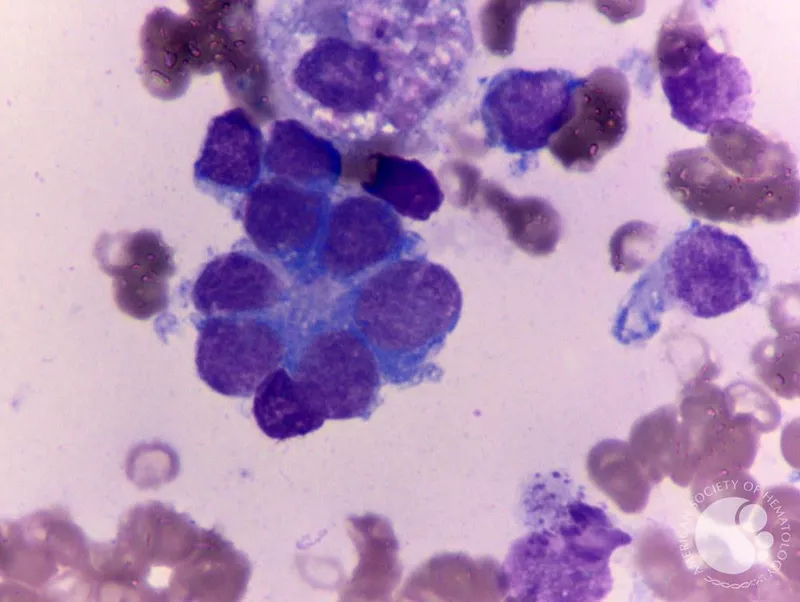
Acute Myeloid Leukemia (AML) Complexity
AML accounts for 15-20% of pediatric leukemias with distinct characteristics:
- Bimodal distribution: Infancy and adolescence peaks
- Cytogenetic importance: 60% have defining abnormalities
- Core binding factor: 25% (favorable prognosis)
- FLT3 mutations: 15% (targeted therapy candidates)
💡 Master This: AML treatment success depends on cytogenetic risk stratification - core binding factor leukemias achieve 85% cure with chemotherapy alone, while 11q23/MLL rearrangements require bone marrow transplantation for optimal outcomes
Lymphoma Landscape
Pediatric lymphomas demonstrate age-related patterns:
Non-Hodgkin Lymphoma (NHL):
- Burkitt lymphoma: 40% of pediatric NHL
- Lymphoblastic lymphoma: 25% (T-cell predominant)
- Large cell lymphoma: 15% (B-cell anaplastic)
- Cure rates: 85-90% with intensive short-duration protocols
Hodgkin Lymphoma:
- Adolescent predominance: Peak 15-19 years
- Nodular sclerosis: 70% of pediatric cases
- Stage I-II: 95% cure rate
- Advanced stage: 85% cure rate
⭐ Clinical Pearl: LDH >2x normal in pediatric lymphoma indicates high tumor burden requiring CNS prophylaxis and intensive protocols, while normal LDH suggests limited disease amenable to reduced-intensity treatment
These hematologic malignancies showcase pediatric oncology's greatest triumphs, with cure rates exceeding 85% through risk-adapted protocols that balance efficacy with long-term survivorship considerations.
🧬 Hematologic Malignancies: The Blood Cell Uprising
🧠 Central Nervous System Tumors: The Neural Command Center
📌 Remember: HICP mnemonic for increased intracranial pressure - Headache (morning, vomiting), Irritability, Cranial nerve palsies, Papilledema
Anatomical Distribution Patterns
Pediatric brain tumors demonstrate age-specific location preferences:
Infratentorial (Posterior Fossa) - 60%:
- Medulloepithelioma: 35% of pediatric brain tumors
- Brainstem gliomas: 15% (predominantly DIPG)
- Ependymomas: 8% (fourth ventricle)
- Cerebellar astrocytomas: 12% (pilocytic type)
Supratentorial - 40%:
- Craniopharyngiomas: 8% (sellar/suprasellar)
- High-grade gliomas: 10% (hemispheric)
- Low-grade gliomas: 15% (hypothalamic/optic)
- Embryonal tumors: 7% (PNET, AT/RT)
| Tumor Type | Peak Age | Location | 5-Year Survival | Treatment Approach |
|---|---|---|---|---|
| Medulloepithelioma | 5-9 years | Cerebellar vermis | 85% | Surgery + RT + Chemo |
| DIPG | 6-8 years | Brainstem | 10% | Radiation only |
| Pilocytic Astrocytoma | 8-12 years | Cerebellum/Optic | 95% | Surgery alone |
| Ependymoma | 2-6 years | Fourth ventricle | 75% | Surgery + RT |
| Craniopharyngioma | 8-12 years | Suprasellar | 90% | Surgery ± RT |
Medulloepithelioma: The Cerebellar Giant
Medulloepithelioma dominates pediatric brain tumor statistics:
- Molecular subgroups: 4 distinct types (WNT, SHH, Group 3, Group 4)
- WNT subgroup: 95% cure rate, no metastases
- Group 3: 50% cure rate, high metastatic potential
- CSF dissemination: 30% at diagnosis
💡 Master This: Molecular subgrouping revolutionized medulloepithelioma treatment - WNT tumors require minimal therapy achieving 95% cure, while Group 3 demands intensive protocols including high-dose chemotherapy and craniospinal radiation
Diffuse Intrinsic Pontine Glioma (DIPG)
DIPG represents pediatric neuro-oncology's greatest challenge:
- Median survival: 9-11 months (unchanged for 40 years)
- H3K27M mutation: 80% of cases
- Biopsy indication: Research protocols only
- Radiation response: 70% show temporary improvement
⚠️ Warning: Cranial nerve palsies with ataxia and long tract signs in school-age children indicate DIPG until proven otherwise - biopsy contraindicated outside research protocols
Treatment Paradigms
Modern pediatric neuro-oncology emphasizes:
Surgical Principles:
- Gross total resection: >95% removal when feasible
- Functional preservation: Eloquent area mapping
- CSF staging: Lumbar puncture post-operatively
Radiation Therapy:
- Craniospinal irradiation: 23.4 Gy + boost for disseminated disease
- Focal radiation: 54 Gy for localized tumors
- Age restrictions: <3 years avoid radiation when possible
Chemotherapy Integration:
- Alkylating agents: Lomustine, temozolomide
- Platinum compounds: Carboplatin, cisplatin
- Targeted therapy: mTOR inhibitors, BRAF inhibitors
These CNS malignancies demand multidisciplinary expertise combining neurosurgical precision, radiation oncology, and molecular-targeted therapy to optimize functional outcomes while maximizing cure potential in developing brains.
🧠 Central Nervous System Tumors: The Neural Command Center
🦴 Solid Tumors: The Tissue Invaders
📌 Remember: SOLID mnemonic for pediatric solid tumors - Sarcomas (bone/soft tissue), Osteosarcoma, Lymphomas, Intra-abdominal masses, Dermoid/teratomas
Wilms Tumor: The Renal Champion
Wilms tumor exemplifies pediatric oncology success with 93% overall survival:
- Peak incidence: 2-4 years (90% diagnosed by age 6)
- Bilateral disease: 5-10% of cases
- Syndromic associations: 15% (WAGR, Beckwith-Wiedemann)
- Favorable histology: 90% of cases
Staging System:
- Stage I: Limited to kidney, completely excised (95% cure)
- Stage II: Regional extension, completely excised (95% cure)
- Stage III: Residual tumor, lymph node positive (90% cure)
- Stage IV: Hematogenous metastases (85% cure)
- Stage V: Bilateral renal involvement (80% cure)
| Risk Group | Histology | Stage | Treatment | Survival |
|---|---|---|---|---|
| Very Low | Favorable | I, <2 years | Surgery + 18 weeks chemo | 99% |
| Standard | Favorable | I-II | Surgery + 18 weeks chemo | 95% |
| Intermediate | Favorable | III-IV | Surgery + RT + 24 weeks | 90% |
| High | Anaplastic | Any | Intensive multiagent | 70% |
| Very High | Anaplastic | IV | Intensive + RT + BMT | 50% |
Neuroblastoma: The Great Masquerader
Neuroblastoma demonstrates the widest spectrum of behaviors in pediatric oncology:
- Neural crest origin: Sympathetic nervous system
- Age distribution: 90% diagnosed by 5 years
- Spontaneous regression: 10% in infants
- MYCN amplification: 25% (poor prognosis marker)
Risk Stratification:
- Low risk: >95% survival (observation often sufficient)
- Intermediate risk: 85-95% survival (moderate chemotherapy)
- High risk: 50% survival (intensive multimodal therapy)
💡 Master This: MYCN amplification overrides age and stage in neuroblastoma risk assessment - even localized tumors with MYCN amplification require intensive therapy due to high relapse potential
Bone Sarcomas: The Skeletal Warriors
Osteosarcoma and Ewing sarcoma dominate pediatric bone malignancies:
Osteosarcoma Characteristics:
- Peak incidence: 10-14 years (growth spurt correlation)
- Location: Metaphyses of long bones (60% around knee)
- Alkaline phosphatase: Elevated in 80% (prognostic marker)
- Pulmonary metastases: 20% at diagnosis
Ewing Sarcoma Features:
- Age range: 5-25 years (broader than osteosarcoma)
- Location: Diaphyseal and flat bones (40% axial skeleton)
- EWS-FLI1 fusion: 85% of cases
- Systemic symptoms: 25% present with fever
| Sarcoma Type | Peak Age | Location | 5-Year Survival | Key Features |
|---|---|---|---|---|
| Osteosarcoma | 13-16 years | Metaphyses | 70% | Alkaline phosphatase ↑ |
| Ewing Sarcoma | 10-20 years | Diaphyses | 65% | Fever, systemic symptoms |
| Chondrosarcoma | Rare <20 years | Pelvis/ribs | 80% | Cartilage matrix |
| Fibrosarcoma | <5 years | Extremities | 85% | Infantile type favorable |
Soft Tissue Sarcomas
Rhabdomyosarcoma leads pediatric soft tissue malignancies:
- Embryonal subtype: 60% (better prognosis)
- Alveolar subtype: 25% (PAX-FOXO1 fusion)
- Head/neck primary: 40% of cases
- Genitourinary: 25% (bladder/prostate/vagina)
Treatment Principles:
- Complete surgical resection: When feasible without functional compromise
- Radiation therapy: Local control for microscopic residual
- Chemotherapy: VAC protocol (vincristine, actinomycin-D, cyclophosphamide)
- Cure rates: 70-85% depending on site and stage
These solid tumors demonstrate pediatric oncology's evolution toward risk-adapted therapy, function preservation, and long-term survivorship focus, achieving remarkable cure rates while minimizing treatment-related morbidity through precision surgical techniques and targeted therapeutic approaches.
🦴 Solid Tumors: The Tissue Invaders
⚖️ Treatment Algorithms: The Therapeutic Precision Matrix
📌 Remember: TREAT mnemonic for protocol selection - Tumor biology, Risk stratification, Early response, Age considerations, Toxicity profile
Risk-Adapted Protocol Framework
Contemporary pediatric oncology stratifies patients using multi-parameter algorithms:
Risk Stratification Parameters:
- Age: <1 year or >10 years often higher risk
- Stage/Extent: Localized vs metastatic disease
- Biology: Cytogenetics, molecular markers, histology
- Response: Day 8, Day 15, End-induction assessments
| Risk Category | Survival Target | Treatment Duration | Intensity Level | Monitoring Frequency |
|---|---|---|---|---|
| Very Low | >95% | 6-12 months | Minimal | Monthly |
| Low | 90-95% | 12-18 months | Reduced | Bi-weekly |
| Standard | 80-90% | 18-24 months | Standard | Weekly |
| High | 60-80% | 24-36 months | Intensive | Daily inpatient |
| Very High | 40-60% | 36+ months | Maximal + BMT | Continuous monitoring |
Chemotherapy Precision Dosing
Pediatric chemotherapy requires weight-based calculations with organ function adjustments:
Dosing Calculations:
- Body Surface Area: Mosteller formula = √(height × weight/3600)
- Renal adjustment: Creatinine clearance <60 mL/min requires dose reduction
- Hepatic adjustment: Bilirubin >3 mg/dL necessitates 50% reduction
- Genetic polymorphisms: TPMT deficiency requires thiopurine dose reduction
Common Pediatric Protocols:
ALL Treatment (Standard Risk):
- Induction: Vincristine 1.5 mg/m² weekly × 4, Daunorubicin 25 mg/m² × 4, L-asparaginase 6,000 units/m² × 9, Prednisone 40 mg/m² × 28 days
- Consolidation: High-dose methotrexate 5 g/m² × 4 cycles
- Maintenance: Mercaptopurine 75 mg/m² daily, Methotrexate 20 mg/m² weekly × 2 years
💡 Master This: Therapeutic drug monitoring in pediatric oncology prevents under-dosing (treatment failure) and over-dosing (excessive toxicity) - methotrexate levels guide leucovorin rescue, while busulfan levels optimize conditioning regimens
Radiation Therapy Considerations
Pediatric radiation requires specialized techniques to minimize growth and development impacts:
Age-Related Restrictions:
- <3 years: Avoid cranial radiation when possible
- 3-7 years: Reduced doses with conformal techniques
- >7 years: Standard doses with growth plate protection
Technical Approaches:
- Proton therapy: 50% reduction in integral dose
- IMRT: Organ-sparing techniques
- Stereotactic radiosurgery: Single-fraction for small targets
- Brachytherapy: Internal radiation for localized tumors
| Age Group | CNS Dose Limit | Growth Impact | Fertility Risk | Secondary Cancer Risk |
|---|---|---|---|---|
| <3 years | Avoid if possible | Severe | Moderate | High |
| 3-7 years | 18-23.4 Gy | Moderate | Low-Moderate | Moderate |
| 7-12 years | 23.4-36 Gy | Mild | Low | Low-Moderate |
| >12 years | Standard doses | Minimal | Minimal | Low |
Surgical Timing and Techniques
Pediatric oncologic surgery balances complete resection with functional preservation:
Timing Strategies:
- Upfront surgery: Wilms tumor, neuroblastoma (when resectable)
- Delayed surgery: After neoadjuvant chemotherapy for size reduction
- Second-look surgery: Reassessment after initial chemotherapy
Surgical Principles:
- En bloc resection: Tumor-free margins when feasible
- Lymph node sampling: Staging and prognostic information
- Organ preservation: Limb salvage, fertility preservation
- Reconstruction: Immediate when possible for functional outcomes
Supportive Care Integration
Infection Prevention:
- ANC <500: Neutropenic precautions, empiric antibiotics
- Prophylaxis: PCP, fungal, viral based on protocol intensity
- Immunizations: Live vaccines contraindicated during treatment
Nutritional Support:
- Enteral nutrition: Preferred when GI tract functional
- Parenteral nutrition: Short-term for severe mucositis
- Growth monitoring: Height/weight velocity assessment
These treatment algorithms represent evidence-based medicine at its finest, incorporating decades of clinical trial data to optimize cure rates while preserving quality of life through precision therapeutic approaches tailored to individual patient characteristics and tumor biology.
⚖️ Treatment Algorithms: The Therapeutic Precision Matrix
🔗 Multi-System Integration: The Survivorship Paradigm
📌 Remember: SURVIVOR mnemonic for late effects monitoring - Second cancers, Unfertility, Radiation effects, Vascular disease, Immune dysfunction, Vision/hearing loss, Organ dysfunction, Reproductive issues
Cardiovascular Late Effects
Anthracycline cardiotoxicity represents the most life-threatening late effect:
- Cumulative dose relationship: >300 mg/m² doxorubicin equivalent
- Subclinical dysfunction: 40% of survivors by 10 years
- Clinical heart failure: 5% by 20 years post-treatment
- Radiation potentiation: Mediastinal radiation increases risk 3-fold
Surveillance Protocols:
- Echocardiography: Every 2 years for high-risk patients
- MUGA scans: Quantitative assessment when echo inadequate
- Biomarkers: BNP, troponin for early detection
- Exercise testing: Functional capacity assessment
| Risk Factor | Relative Risk | Screening Interval | Intervention Threshold |
|---|---|---|---|
| Doxorubicin >300 mg/m² | 8.2x | Annual | LVEF <50% |
| Chest radiation >30 Gy | 6.1x | Annual | Wall motion abnormality |
| Combined therapy | 15.3x | Every 6 months | Symptoms + dysfunction |
| Age <5 at treatment | 4.7x | Biennial | Biomarker elevation |
Endocrine Dysfunction Spectrum
Growth and development complications affect multiple endocrine axes:
Growth Hormone Deficiency:
- Cranial radiation >18 Gy: 90% incidence
- Spinal radiation: Sitting height disproportionately affected
- Chemotherapy: Glucocorticoids cause growth velocity reduction
- Treatment: Recombinant GH when tumor-free >2 years
Thyroid Dysfunction:
- Neck radiation: 50% develop hypothyroidism
- Total body irradiation: 80% require thyroid replacement
- Secondary thyroid cancer: 18-fold increased risk
- Surveillance: Annual TSH, neck examination
💡 Master This: Precocious puberty occurs in 20% of cranial radiation survivors due to hypothalamic dysfunction, requiring GnRH agonist therapy to preserve final adult height and psychological well-being
Neurocognitive and Psychosocial Outcomes
CNS treatment creates lifelong learning challenges:
Cognitive Late Effects:
- IQ decline: 10-15 points after cranial radiation
- Processing speed: Most sensitive cognitive domain
- Executive function: Planning, organization deficits
- Memory: Working memory particularly affected
Academic Interventions:
- Neuropsychological testing: Baseline and serial assessments
- Educational accommodations: Extended time, reduced distractions
- Cognitive rehabilitation: Computer-based training programs
- Stimulant medications: Methylphenidate for attention deficits
Psychosocial Considerations:
- PTSD prevalence: 15-25% in survivors and families
- Depression/anxiety: 2-3 fold increased risk
- Social isolation: Peer relationship difficulties
- Employment: Lower rates of full-time employment
Second Malignancy Risk
Treatment-related cancers represent leading cause of late mortality:
Radiation-Induced Cancers:
- Latency period: 5-10 years for leukemia, 10-20 years for solid tumors
- Breast cancer: 75-fold increased risk after chest radiation
- Thyroid cancer: 18-fold increased risk after neck radiation
- Sarcomas: In-field radiation sarcomas after >10 years
Chemotherapy-Related Malignancies:
- Secondary leukemia: Alkylating agents (5-7 years), topoisomerase II inhibitors (2-3 years)
- Cumulative incidence: 3-12% by 20 years depending on treatment intensity
| Treatment Exposure | Cancer Type | Latency | Cumulative Risk | Screening Recommendation |
|---|---|---|---|---|
| Chest radiation | Breast cancer | 8-10 years | 13-20% | Annual MRI age 25+ |
| Alkylating agents | Bladder cancer | 10-15 years | 2-5% | Annual urinalysis |
| Anthracyclines | Cardiomyopathy | 5-20 years | 5-10% | Echo every 2 years |
| Cranial radiation | Brain tumors | 10-20 years | 1-3% | MRI every 5 years |
Fertility and Reproductive Health
Gonadal dysfunction affects family planning and quality of life:
Male Fertility:
- Alkylating agent dose-dependent oligospermia/azoospermia
- Recovery potential: Varies by age and cumulative dose
- Sperm banking: Pre-treatment when age-appropriate
- Testosterone deficiency: Leydig cell dysfunction after testicular radiation
Female Fertility:
- Ovarian failure: Age-dependent sensitivity to chemotherapy
- Premature menopause: Cyclophosphamide >7.5 g/m²
- Pregnancy outcomes: Generally favorable in fertile survivors
- Fertility preservation: Oocyte/embryo cryopreservation, ovarian tissue banking
This multi-system integration approach transforms childhood cancer survivors from patients to partners in lifelong health management, emphasizing prevention, early detection, and quality of life optimization through evidence-based survivorship care.
🔗 Multi-System Integration: The Survivorship Paradigm
🎯 Clinical Mastery Arsenal: The Pediatric Oncology Command Center
📌 Remember: URGENT mnemonic for oncologic emergencies - Upper airway obstruction, Raised ICP, GI bleeding, Electrolyte crisis, Neutropenic fever, Tumor lysis syndrome
Rapid Assessment Framework
The 3-Minute Oncology Assessment:
Primary Survey (30 seconds):
- Airway: Stridor, drooling, positioning
- Breathing: Respiratory distress, SVC syndrome
- Circulation: Shock, bleeding, cardiac tamponade
- Disability: Altered mental status, focal deficits
Secondary Survey (2.5 minutes):
- Fever: >38.3°C = neutropenic emergency
- Masses: Mediastinal, abdominal, lymphadenopathy
- Neurologic: Headache, vomiting, papilledema
- Laboratory: CBC, chemistries, LDH, uric acid
| Clinical Scenario | Key Features | Time to Action | Critical Intervention |
|---|---|---|---|
| Neutropenic Fever | ANC <500, Temp >38.3°C | <60 minutes | Broad-spectrum antibiotics |
| Tumor Lysis | K+ >6, Phos >6.5, Ca <7 | <30 minutes | Dialysis consideration |
| SVCS | Facial swelling, stridor | <15 minutes | Airway management |
| Raised ICP | Headache, vomiting, bradycardia | <30 minutes | Osmotic therapy |
| Spinal Compression | Back pain, weakness | <4 hours | MRI + steroids |
Essential Laboratory Arsenal
Diagnostic Laboratory Patterns:
Leukemia Indicators:
- Blast cells: >5% in peripheral blood
- Pancytopenia: Anemia + thrombocytopenia + neutropenia
- Hyperleukocytosis: WBC >100,000 (leukostasis risk)
- Coagulopathy: DIC in acute promyelocytic leukemia
Solid Tumor Markers:
- Alpha-fetoprotein: >500 ng/mL (hepatoblastoma, germ cell tumors)
- Beta-hCG: >100 mIU/mL (germ cell tumors)
- Catecholamines: VMA/HVA elevated (neuroblastoma)
- LDH: Tumor burden marker across all malignancies
💡 Master This: Tumor lysis syndrome prevention requires aggressive hydration (3 L/m²/day), allopurinol (300 mg/m²), and rasburicase for high-risk patients with LDH >2x normal or large tumor burden
Treatment Response Monitoring
Early Response Indicators:
Day 8 Peripheral Blast Count (ALL):
- <1,000/μL: Excellent response (95% cure probability)
- 1,000-5,000/μL: Good response (85% cure probability)
- >5,000/μL: Poor response (70% cure probability)
Minimal Residual Disease (MRD):
- <0.01%: Molecular remission
- 0.01-0.1%: Low-level disease
- >0.1%: High-risk for relapse
Imaging Response (Solid Tumors):
- Complete response: No measurable disease
- Partial response: >30% size reduction
- Progressive disease: >20% size increase
- Stable disease: Neither PR nor PD criteria
Emergency Management Protocols
Neutropenic Fever Protocol:
- Blood cultures × 2 (peripheral + central line)
- Ceftazidime 50 mg/kg IV q8h OR cefepime 50 mg/kg IV q8h
- Vancomycin if line infection suspected
- Antifungal if fever >96 hours
Tumor Lysis Syndrome Management:
- Hydration: 3 L/m²/day (200 mL/kg/day if <10 kg)
- Allopurinol: 300 mg/m²/day divided q8h
- Rasburicase: 0.2 mg/kg IV daily if high risk
- Monitor: q6h electrolytes, q12h phosphorus/calcium
Superior Vena Cava Syndrome:
- Elevate head of bed 30-45 degrees
- Avoid sedation (respiratory compromise risk)
- Emergent radiation if airway compromise
- Steroids: Dexamethasone 0.6 mg/kg/day
Prognostic Integration Matrix
Risk Stratification Synthesis:
| Factor | Low Risk | Intermediate Risk | High Risk | Very High Risk |
|---|---|---|---|---|
| Age | 1-9 years | <1 or >10 years | Infant | Adolescent |
| WBC | <50,000 | 50-100,000 | >100,000 | >200,000 |
| Cytogenetics | Hyperdiploidy | Normal | Complex | Philadelphia+ |
| Response | Day 8 <1,000 | Day 8 1-5,000 | Day 8 >5,000 | MRD+ End-Induction |
| Treatment | Standard | Intensified | High-intensity | Experimental |
This clinical mastery arsenal transforms pediatric oncology complexity into systematic excellence, enabling rapid recognition, appropriate triage, and optimal outcomes through evidence-based decision making and coordinated multidisciplinary care.
🎯 Clinical Mastery Arsenal: The Pediatric Oncology Command Center
Practice Questions: Common pediatric cancers
Test your understanding with these related questions
A 12-month-old girl is brought to her pediatrician for a checkup and vaccines. The patient’s mother wants to send her to daycare but is worried about exposure to unvaccinated children and other potential sources of infection. The toddler was born at 39 weeks gestation via spontaneous vaginal delivery. She is up to date on all vaccines. She does not walk yet but stands in place and can say a few words. The toddler drinks formula and eats a mixture of soft vegetables and pureed meals. She has no current medications. On physical exam, the vital signs include: temperature 37.0°C (98.6°F), blood pressure 95/50 mm Hg, pulse 130/min, and respiratory rate 28/min. The patient is alert and responsive. The remainder of the exam is unremarkable. Which of the following is most appropriate for this patient at this visit?












