Ethical frameworks for decision-making US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Ethical frameworks for decision-making. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Ethical frameworks for decision-making US Medical PG Question 1: A 68-year-old man comes to the physician for a follow-up examination, accompanied by his daughter. Two years ago, he was diagnosed with localized prostate cancer, for which he underwent radiation therapy. He moved to the area 1 month ago to be closer to his daughter but continues to live independently. He was recently diagnosed with osteoblastic metastases to the spine and is scheduled to initiate therapy next week. In private, the patient’s daughter says that he has been losing weight and wetting the bed, and she tearfully asks the physician if his prostate cancer has returned. She says that her father has not spoken with her about his health recently. The patient has previously expressed to the physician that he does not want his family members to know about his condition because they “would worry too much.” Which of the following initial statements by the physician is most appropriate?
- A. “As your father's physician, I think that it's important that you know that his prostate cancer has returned. However, we are confident that he will respond well to treatment.”
- B. “I'm sorry, I can't discuss any information with you without his permission. I recommend that you have an open discussion with your father.” (Correct Answer)
- C. “It concerns me that he's not speaking openly with you. I recommend that you seek medical power of attorney for your father. Then, we can legally discuss his diagnosis and treatment options together.”
- D. “It’s difficult to deal with parents aging, but I have experience helping families cope. We should sit down with your father and discuss this situation together.”
- E. “Your father is very ill and may not want you to know the details. I can imagine it's frustrating for you, but you have to respect his discretion.”
Ethical frameworks for decision-making Explanation: ***“I'm sorry, I can't discuss any information with you without his permission. I recommend that you have an open discussion with your father.”***
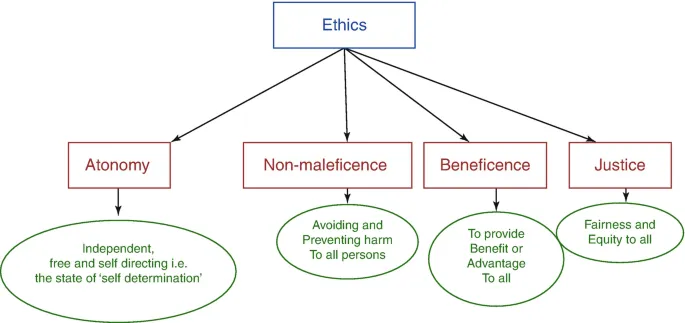
- This statement upholds **patient confidentiality** and **autonomy**, as the patient explicitly stated he did not want his family to know about his condition.
- It encourages communication between the patient and his daughter, which is the most appropriate way for her to learn about his health status.
*“As your father's physician, I think that it's important that you know that his prostate cancer has returned. However, we are confident that he will respond well to treatment.”*
- This violates the patient's **confidentiality** and explicit wish to keep his medical information private from his family.
- Sharing medical information without explicit consent, even with family, is a breach of ethical and legal guidelines (e.g., **HIPAA** in the United States).
*“It concerns me that he's not speaking openly with you. I recommend that you seek medical power of attorney for your father. Then, we can legally discuss his diagnosis and treatment options together.”*
- While seeking medical power of attorney is an option for future decision-making, it is **premature and inappropriate** to suggest it solely to bypass the patient's current desire for confidentiality, especially when he is still competent to make his own decisions.
- This suggestion could undermine the patient's autonomy and trust in his physician.
*“It’s difficult to deal with parents aging, but I have experience helping families cope. We should sit down with your father and discuss this situation together.”*
- This statement, while empathetic, still risks undermining the patient's **autonomy** by pushing for a joint discussion against his explicit wishes to keep his family unaware.
- The physician's primary obligation is to the patient's stated preferences regarding his medical information.
*“Your father is very ill and may not want you to know the details. I can imagine it's frustrating for you, but you have to respect his discretion.”*
- While this statement acknowledges the daughter's feelings and respects the patient's discretion, it uses a somewhat **judgmental tone** ("very ill") and the phrasing "you have to respect his discretion" can come across as abrupt or dismissive rather than purely informative or guiding.
- The most appropriate initial response should focus on the **physician's inability to share information** due to confidentiality rather than attributing motives to the patient's decision or explicitly telling the daughter how to feel.
Ethical frameworks for decision-making US Medical PG Question 2: A 29-year-old man is admitted to the emergency department following a motorcycle accident. The patient is severely injured and requires life support after splenectomy and evacuation of a subdural hematoma. Past medical history is unremarkable. The patient’s family members, including wife, parents, siblings, and grandparents, are informed about the patient’s condition. The patient has no living will and there is no durable power of attorney. The patient must be put in an induced coma for an undetermined period of time. Which of the following is responsible for making medical decisions for the incapacitated patient?
- A. The spouse (Correct Answer)
- B. An older sibling
- C. Physician
- D. Legal guardian
- E. The parents
Ethical frameworks for decision-making Explanation: ***The spouse***
- In the absence of a **living will** or **durable power of attorney**, the law typically designates the **spouse** as the primary decision-maker for an incapacitated patient.
- This hierarchy is established to ensure decisions are made by the individual most intimately connected and presumed to understand the patient's wishes.
*An older sibling*
- Siblings are generally further down the **hierarchy of surrogate decision-makers** than a spouse or parents.
- They would typically only be considered if higher-priority family members are unavailable or unwilling to make decisions.
*Physician*
- The physician's role is to provide medical care and guidance, not to make medical decisions for an incapacitated patient when family surrogates are available.
- Physicians only make decisions in **emergency situations** when no surrogate is immediately available and treatment is immediately necessary to save the patient's life or prevent serious harm.
*Legal guardian*
- A legal guardian is usually appointed by a **court** when there is no appropriate family member available or when there is a dispute among family members.
- In this scenario, with a spouse and other close family members present, a legal guardian would not be the first choice.
*The parents*
- While parents are close family members, they are typically considered **secondary to the spouse** in the hierarchy of surrogate decision-makers for an adult patient.
- They would usually only be the decision-makers if the patient were unmarried or the spouse were unavailable.
Ethical frameworks for decision-making US Medical PG Question 3: A 19-year-old man presents to an orthopedic surgeon to discuss repair of his torn anterior cruciate ligament. He suffered the injury during a college basketball game 1 week ago and has been using a knee immobilizer since the accident. His past medical history is significant for an emergency appendectomy when he was 12 years of age. At that time, he said that he never wanted to have surgery again. At this visit, the physician explains the procedure to him in detail including potential risks and complications. The patient acknowledges and communicates his understanding of both the diagnosis as well as the surgery and decides to proceed with the surgery in 3 weeks. Afterward, he signs a form giving consent for the operation. Which of the following statements is true about this patient?
- A. He cannot provide consent because he lacks capacity
- B. He has the right to revoke his consent at any time (Correct Answer)
- C. His parents also need to give consent to this operation
- D. He did not need to provide consent for this procedure since it is obviously beneficial
- E. His consent is invalid because his decision is not stable over time
Ethical frameworks for decision-making Explanation: ***He has the right to revoke his consent at any time***
- **Informed consent** for medical procedures is an ongoing process, and a patient retains the right to **withdraw consent** at any point, even after initially signing the consent form.
- This right is a fundamental aspect of patient autonomy and ensures that medical interventions are only performed with a patient's current and willing agreement.
*He cannot provide consent because he lacks capacity*
- The patient is 19 years old, which in most jurisdictions (including the US where the age of majority is typically 18) means he is considered an **adult** and legally capable of providing his own consent.
- The scenario explicitly states he "communicates his understanding of both the diagnosis as well as the surgery," indicating he possesses the **mental capacity** to make an informed decision.
*His parents also need to give consent to this operation*
- As a 19-year-old, the patient has reached the **age of majority** and is legally entitled to make his own medical decisions, including consenting to surgery.
- Parental consent is generally required for minors (individuals under the age of majority), but not for adults like this patient.
*He did not need to provide consent for this procedure since it is obviously beneficial*
- Even for procedures that are clearly **beneficial**, informed consent is ethically and legally mandatory to uphold **patient autonomy** and ensure respect for individual rights.
- The concept of "obviously beneficial" does not negate the requirement for a patient's explicit agreement to a medical intervention.
*His consent is invalid because his decision is not stable over time*
- While the patient might have initially hated surgery at age 12, his current decision at age 19 to proceed with the ACL repair is based on current information and his mature understanding.
- The fact that his previous aversion to surgery has changed does not invalidate his current, well-informed decision; it simply indicates a change in perspective based on new circumstances and greater maturity.
Ethical frameworks for decision-making US Medical PG Question 4: A 28-year-old woman dies shortly after receiving a blood transfusion. Autopsy reveals widespread intravascular hemolysis and acute renal failure. Investigation reveals that she received type A blood, but her medical record indicates she was type O. In a malpractice lawsuit, which of the following elements must be proven?
- A. Duty, breach, causation, and damages (Correct Answer)
- B. Only duty and breach
- C. Only breach and causation
- D. Duty, breach, and damages
Ethical frameworks for decision-making Explanation: ***Duty, breach, causation, and damages***
- In a medical malpractice lawsuit, all four elements—**duty, breach, causation, and damages**—must be proven for a successful claim.
- The healthcare provider had a **duty** to provide competent care, they **breached** that duty by administering the wrong blood type, this breach **caused** the patient's death and renal failure, and these injuries constitute **damages**.
*Only duty and breach*
- While **duty** and **breach** are necessary components, proving only these two is insufficient for a malpractice claim.
- It must also be demonstrated that the breach directly led to the patient's harm and resulted in legally recognized damages.
*Only breach and causation*
- This option omits the crucial elements of professional **duty** owed to the patient and the resulting **damages**.
- A claim cannot succeed without establishing that a duty existed and that quantifiable harm occurred.
*Duty, breach, and damages*
- This option misses the critical element of **causation**, which links the provider's breach of duty to the patient's injuries.
- Without proving that the breach *caused* the damages, even if a duty was owed and breached, and damages occurred, the claim would fail.
Ethical frameworks for decision-making US Medical PG Question 5: A 13-year-old boy is brought to the emergency department after being involved in a motor vehicle accident in which he was a restrained passenger. He is confused and appears anxious. His pulse is 131/min, respirations are 29/min, and blood pressure is 95/49 mm Hg. Physical examination shows ecchymosis over the upper abdomen, with tenderness to palpation over the left upper quadrant. There is no guarding or rigidity. Abdominal ultrasound shows free intraperitoneal fluid and a splenic rupture. Intravenous fluids and vasopressors are administered. A blood transfusion and exploratory laparotomy are scheduled. The patient's mother arrives and insists that her son should not receive a blood transfusion because he is a Jehovah's Witness. The physician proceeds with the blood transfusion regardless of the mother's wishes. The physician's behavior is an example of which of the following principles of medical ethics?
- A. Autonomy
- B. Nonmaleficence
- C. Informed consent
- D. Justice
- E. Beneficence (Correct Answer)
Ethical frameworks for decision-making Explanation: ***Beneficence***
- The physician prioritized the patient's immediate survival and well-being, which is the core principle of **beneficence** (acting in the best interest of the patient).
- In cases of life-threatening emergencies, especially with minors, the duty to preserve life often outweighs other considerations like parental wishes, particularly when the patient lacks the capacity for **informed refusal**.
*Autonomy*
- The physician’s action directly overrides the mother's wishes, which would be an infringement of surrogate autonomy for a minor.
- While patient autonomy is a fundamental principle, it was superseded by the immediate need to save the patient's life.
*Nonmaleficence*
- **Nonmaleficence** means "do no harm." While transfusions have risks, refusing one in this critical situation would cause more harm (death) than performing it.
- The physician acted to prevent immediate harm (death from hemorrhage), even if it meant overriding a family's wishes regarding the specific treatment method.
*Informed consent*
- **Informed consent** requires obtaining permission from a capacitated patient (or legal guardian for a minor) after explaining the risks and benefits of a treatment.
- In this emergency scenario, the patient is a minor and incapacitated, and the urgent need for a life-saving intervention (blood transfusion for a splenic rupture) did not allow for full informed consent or negotiation with the mother, who was refusing a life-saving measure.
*Justice*
- **Justice** refers to the fair and equitable distribution of healthcare resources and equal treatment, which is not the primary ethical concern in this personal patient-physician interaction.
- The scenario focuses on the individual patient's treatment decision, not broader societal resource allocation or fairness in access to care.
Ethical frameworks for decision-making US Medical PG Question 6: A psychiatrist receives a call from a patient who expresses thoughts of harming his ex-girlfriend. The patient describes a detailed plan to attack her at her workplace. Which of the following represents the psychiatrist's most appropriate legal obligation?
- A. Warn the ex-girlfriend and notify law enforcement (Correct Answer)
- B. Only notify the patient's family
- C. Warn only law enforcement
- D. Maintain patient confidentiality
Ethical frameworks for decision-making Explanation: ***Warn the ex-girlfriend and notify law enforcement***
- This scenario directly triggers the **"duty to warn"** and **"duty to protect"** principles, primarily stemming from the **Tarasoff v. Regents of the University of California** case.
- The psychiatrist has a legal obligation to take reasonable steps to protect the identifiable victim, which includes directly warning the intended victim and informing law enforcement.
*Only notify the patient's family*
- Notifying the patient's family alone does not fulfill the **legal obligation to protect** an identifiable third party from a serious threat of harm.
- While family involvement might be part of a comprehensive safety plan, it is insufficient as the sole action in this critical situation.
*Warn only law enforcement*
- While notifying law enforcement is a crucial step, the **Tarasoff duty** specifically mandates warning the **intended victim** directly (or those who can reasonably be expected to notify the victim).
- Relying solely on law enforcement might not ensure the immediate safety of the ex-girlfriend, especially if there's a delay in their response or ability to locate her.
*Maintain patient confidentiality*
- Patient confidentiality is a cornerstone of psychiatric practice, but it is **not absolute** when there is a serious and imminent threat of harm to an identifiable individual.
- The **duty to protect** a potential victim *outweighs* the duty to maintain confidentiality in such extreme circumstances.
Ethical frameworks for decision-making US Medical PG Question 7: A 23-year-old woman presents to the emergency department with acute alcohol intoxication. Her blood alcohol level is 280 mg/dL. She becomes increasingly agitated and attempts to leave against medical advice. Which of the following determines her capacity to refuse treatment?
- A. Age of the patient
- B. Family's wishes
- C. Blood alcohol level
- D. Understanding of risks and benefits (Correct Answer)
Ethical frameworks for decision-making Explanation: ***Understanding of risks and benefits***
- A patient's capacity to refuse treatment is primarily determined by their **ability to understand the nature of their condition**, the proposed treatment, and the **potential risks and benefits** of both accepting and refusing treatment.
- Even with intoxication, if a patient can demonstrate this understanding, they technically have the capacity to make decisions, though the intoxication itself often impairs this ability.
- Capacity assessment includes four key elements: understanding information, appreciating how it applies to their situation, reasoning through options, and communicating a choice.
*Age of the patient*
- While age is a factor in pediatric care (requiring parental consent for minors), for adults, it does not solely determine capacity; an adult of any age can be deemed to lack capacity for various reasons.
- The patient's age (23 years old) indicates she is legally an adult, but it does not automatically confer or deny treatment capacity, which is assessed based on mental status.
*Family's wishes*
- Family wishes are important for patients who **lack decision-making capacity** and have no advance directives, but they do not override the decisions of a fully capacitated patient.
- In situations where capacity is questionable, family input might be considered, but the direct assessment of the patient's understanding remains paramount.
*Blood alcohol level*
- A high blood alcohol level strongly suggests impaired judgment and cognitive function, making it a red flag for potential lack of capacity, but it is not a direct measure of capacity itself.
- Some individuals may maintain a degree of understanding even with high levels, so a direct assessment of their comprehension is still necessary, not just assuming based on the level alone.
Ethical frameworks for decision-making US Medical PG Question 8: A 73-year-old man is admitted to the hospital for jaundice and weight loss. He is an immigrant from the Dominican Republic and speaks little English. A CT scan is performed showing a large mass at the head of the pancreas. When you enter the room to discuss these results with the patient, his daughter and son ask to speak with you outside of the patient's room. They express their desire to keep these results from their father. What is the appropriate response in this situation?
- A. Consult the hospital ethics committee
- B. Deliver the information in Spanish
- C. Respect the children's wishes to hold prognosis information
- D. Tell the children that you are obligated to tell the father
- E. Explore the reasoning behind the children's request (Correct Answer)
Ethical frameworks for decision-making Explanation: ***Explore the reasoning behind the children's request***
- Understanding the family's cultural background, including beliefs about illness and communication, is crucial for navigating this sensitive situation.
- This approach allows the healthcare provider to assess whether the family's request stems from a protective desire rooted in their culture or a misunderstanding, which can inform the next steps.
*Consult the hospital ethics committee*
- While an ethics consultation may be necessary if an impasse is reached, it is not the immediate first step.
- Initial direct communication and exploration with the family are preferable to first understand the context before escalating to an ethics committee.
*Deliver the information in Spanish*
- This addresses the language barrier but does not resolve the ethical dilemma of withholding information from the patient at the family's request.
- Providing the information in Spanish without first understanding the family's wishes might violate their cultural norms or inadvertently cause distress.
*Respect the children's wishes to hold prognosis information*
- Respecting the children's wishes without understanding their rationale could violate the patient's right to **autonomy** and **informed consent**.
- In most Western medical ethics frameworks, the patient has the primary right to receive information about their health, even if it is distressing.
*Tell the children that you are obligated to tell the father*
- Immediately stating an obligation without understanding the family's perspective can come across as abrupt and culturally insensitive.
- This approach might create an adversarial dynamic, making it harder to build trust and find a mutually agreeable solution.
Ethical frameworks for decision-making US Medical PG Question 9: A 12-year-old boy and his mother are brought to the emergency department after a motor vehicle accident. The boy was an unrestrained passenger in a head-on collision and was ejected from the front seat. The patient's mother was the driver and she is currently being resuscitated. Neither the child nor the mother are conscious; however, it is documented that the family are all Jehovah's witnesses and would not want a transfusion in an acute situation. The husband/father arrives to the trauma bay and confirms this wish that everyone in the family would not want a transfusion in accordance with their beliefs. The father is confirmed as the official healthcare proxy. Which of the following is the best next step in management?
- A. Consult the hospital ethics committee
- B. Do not transfuse the boy or the mother
- C. Do not transfuse the mother and transfuse the boy (Correct Answer)
- D. Do not transfuse the boy and transfuse the mother
- E. Transfuse the boy and mother
Ethical frameworks for decision-making Explanation: ***Do not transfuse the mother and transfuse the boy***
- While the **mother's wishes** for no transfusion must be respected, the boy's status as a **minor** (12 years old) allows for medical intervention to save his life, particularly in an emergency.
- In situations where a parent's religious beliefs conflict with a minor's best interest for life-saving treatment, the **state's interest in protecting children** often overrides parental autonomy.
*Consult the hospital ethics committee*
- While an ethics consultation may be appropriate in non-emergent or complex cases, in an **acute, life-threatening emergency** for a minor, delaying treatment to consult an ethics committee could be detrimental.
- The immediate priority is to provide **life-saving treatment** to the minor.
*Do not transfuse the boy or the mother*
- Refusing transfusion for the mother is consistent with her advance directives and the father's confirmed wishes, respecting her **autonomy**.
- However, refusing transfusion for the minor boy, given his age and the life-threatening situation, would prioritize parental religious beliefs over the **child's right to life-saving care**.
*Do not transfuse the boy and transfuse the mother*
- This option incorrectly applies the principles of autonomy and best interest. The mother, as an adult, has the right to refuse care, but the **minor child's right to life-saving treatment** generally takes precedence over parental refusal in emergencies.
- Transfusing the mother against her stated wishes and confirmed by her healthcare proxy would be a violation of her **autonomy**.
*Transfuse the boy and mother*
- Transfusing the boy is generally appropriate given his minor status and life-threatening condition in an emergency.
- However, transfusing the mother against her documented wishes and the confirmed consent of her healthcare proxy would be a **violation of her autonomy and right to refuse medical treatment**.
Ethical frameworks for decision-making US Medical PG Question 10: A 36-year-old man comes to the physician because of a 2-week history of productive cough, weight loss, and intermittent fever. He recently returned from a 6-month medical deployment to Indonesia. He appears tired. Physical examination shows nontender, enlarged, palpable cervical lymph nodes. An x-ray of the chest shows right-sided hilar lymphadenopathy. A sputum smear shows acid-fast bacilli. A diagnosis of pulmonary tuberculosis is made from PCR testing of the sputum. The patient requests that the physician does not inform anyone of this diagnosis because he is worried about losing his job. Which of the following is the most appropriate initial action by the physician?
- A. Request the patient's permission to discuss the diagnosis with an infectious disease specialist
- B. Assure the patient that his diagnosis will remain confidential
- C. Confirm the diagnosis with a sputum culture
- D. Notify all of the patient's household contacts of the diagnosis
- E. Inform the local public health department of the diagnosis (Correct Answer)
Ethical frameworks for decision-making Explanation: ***Inform the local public health department of the diagnosis***
- **Tuberculosis** is a **reportable disease** to public health authorities due to its significant public health implications, including the risk of transmission.
- Physicians have a **legal and ethical obligation** to report such diagnoses to protect the community, even against a patient's wishes for secrecy.
*Request the patient's permission to discuss the diagnosis with an infectious disease specialist*
- While consulting an infectious disease specialist is often beneficial for managing TB, the immediate and most appropriate initial action is related to **public health notification**.
- Delaying notification to seek patient permission first would **compromise public health safety** regarding a reportable disease.
*Assure the patient that his diagnosis will remain confidential*
- This assurance would be **misleading and unethical** because TB is a reportable condition, meaning its confidentiality is necessarily breached for public health purposes.
- Physicians are bound by law to report communicable diseases, which supersedes general confidentiality in this specific context.
*Confirm the diagnosis with a sputum culture*
- The diagnosis of pulmonary tuberculosis has already been established by a **sputum smear showing acid-fast bacilli** and **PCR testing**, which are highly reliable.
- While a sputum culture provides drug susceptibility information, it is not the *initial* most appropriate action regarding the patient's stated concerns about confidentiality in the context of a reportable disease.
*Notify all of the patient's household contacts of the diagnosis*
- While contact tracing is an important part of TB control, it is typically initiated and managed by the **public health department** after notification.
- The physician's primary responsibility is to notify the health department, who then assumes the role of **contact investigation** and management.
More Ethical frameworks for decision-making US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.