Medical Ethics

On this page
🎯 The Ethical Compass: Navigating Medicine's Moral Landscape
Medical ethics transforms abstract principles into the daily architecture of clinical decision-making, guiding you through conflicts where patient autonomy collides with beneficence, where cutting-edge technology outpaces regulation, and where resource scarcity tests justice. You'll master the four pillars-autonomy, beneficence, non-maleficence, and justice-then apply them to research dilemmas, emerging digital frontiers, and real-world cases that demand both moral clarity and practical wisdom. This lesson builds your ethical reasoning from foundational concepts to the nuanced toolkit every practitioner needs when guidelines end and judgment begins.
📌 Remember: ABCJ - Autonomy (respect patient choice), Beneficence (do good), Care without harm (non-maleficence), Justice (fair treatment). These four pillars support 98% of ethical decision-making frameworks used in modern medicine.
The ethical landscape encompasses multiple domains requiring systematic analysis. Core principles provide the foundation, while specialized areas like reproductive ethics, genetic testing, and emerging technologies present unique challenges requiring nuanced understanding.
| Ethical Domain | Key Principles | Clinical Applications | Decision Framework | Violation Consequences |
|---|---|---|---|---|
| Patient Autonomy | Informed consent, capacity assessment | Treatment refusal, advance directives | 3-step capacity evaluation | License suspension (15% of cases) |
| Confidentiality | Privacy protection, mandatory reporting | HIPAA compliance, duty to warn | 12 specific exceptions | Fines up to $1.5M |
| Professional Boundaries | Therapeutic relationship limits | Gift policies, dual relationships | Zero tolerance for violations | 85% result in discipline |
| Resource Allocation | Fair distribution, medical necessity | ICU beds, organ transplants | QALY calculations | Institutional liability |
| Research Ethics | Informed consent, risk-benefit analysis | Clinical trials, vulnerable populations | IRB approval required | Federal funding loss |
- Capacity assessment requires 4 components: understanding, appreciation, reasoning, choice expression
- Informed consent mandates 8 elements including risks, benefits, alternatives
- Material risk threshold: >1% occurrence or serious consequences
- Therapeutic privilege exception: <5% of cases justify withholding information
- Beneficence Applications
- Positive duty to promote patient welfare beyond avoiding harm
- Evidence-based interventions with NNT <10 generally considered beneficial
- Quality-adjusted life years (QALY) calculations guide resource allocation
- Cost-effectiveness threshold: $50,000-100,000 per QALY gained
⭐ Clinical Pearl: Capacity fluctuates - a patient may lack capacity for complex surgical decisions while retaining capacity for basic care choices. Reassess capacity for each significant decision, particularly when cognitive function changes or high-stakes interventions are considered.
💡 Master This: The "reasonable person" standard for informed consent requires disclosure of information that a reasonable person in the patient's position would want to know. This includes 1-5% risk thresholds for serious complications and alternative treatment options with significantly different risk profiles.
Understanding ethical frameworks transforms clinical uncertainty into structured decision-making processes. These principles interconnect through complex scenarios where multiple values compete, requiring systematic analysis to reach morally defensible conclusions that serve patient interests while maintaining professional standards.
🎯 The Ethical Compass: Navigating Medicine's Moral Landscape
⚖️ Autonomy Architecture: The Patient's Command Center
📌 Remember: CARE - Capacity (ability to decide), Authentic choice (free from coercion), Relevant information (material facts), Expression of choice (clear communication). These 4 elements must align for valid autonomous decision-making in 100% of clinical scenarios.
The autonomy framework operates through interconnected components that ensure genuine patient self-determination. Capacity assessment forms the foundation, while informed consent provides the mechanism for exercising autonomous choice.
| Capacity Component | Assessment Method | Clinical Indicators | Threshold Criteria | Documentation Requirements |
|---|---|---|---|---|
| Understanding | Teach-back method | Repeats key information | >80% accuracy | Verbatim quotes |
| Appreciation | Consequence exploration | Recognizes personal impact | Acknowledges realistic outcomes | Risk acknowledgment |
| Reasoning | Decision rationale | Logical thought process | Consistent with values | Value-based explanation |
| Choice Expression | Clear communication | Unambiguous decision | Stable over time | Witnessed statement |
| Freedom from Coercion | Pressure assessment | Independent decision-making | No external manipulation | Coercion screening |
- Mini-Mental State Exam scores <24 suggest potential capacity impairment
- Fluctuating capacity requires assessment at optimal cognitive periods
- Delirium affects 40% of hospitalized elderly patients
- Capacity restoration possible in 65% of treatable conditions
- Informed Consent Elements
- Material risks include complications >1% frequency or life-threatening consequences
- Alternative treatments with significantly different risk-benefit profiles
- No-treatment option must be presented in 100% of cases
- Second opinions recommended for high-risk or experimental procedures
⭐ Clinical Pearl: Sliding scale capacity - higher-stakes decisions require higher capacity thresholds. A patient may have capacity to refuse routine medications but lack capacity for high-risk surgery or life-sustaining treatment withdrawal. Adjust assessment rigor accordingly.
💡 Master This: Therapeutic privilege allows withholding information only when disclosure would cause serious psychological harm that outweighs autonomy benefits. This exception applies to <5% of cases and requires clear documentation of specific harms and alternative approaches to information sharing.
Autonomy extends beyond individual decisions to encompass advance directives, surrogate decision-making, and cultural considerations. Living wills provide specific treatment preferences, while healthcare proxies designate decision-makers for incapacitated patients. Cultural competency ensures autonomy respects diverse values and communication styles.
The autonomy principle creates the foundation for shared decision-making models that balance patient preferences with medical expertise. This framework enables patients to exercise meaningful control while benefiting from professional guidance, establishing the collaborative partnership essential for optimal healthcare outcomes.
⚖️ Autonomy Architecture: The Patient's Command Center
🛡️ The Beneficence Engine: Maximizing Patient Welfare
📌 Remember: BEST - Benefit maximization (choose optimal interventions), Evidence-based practice (proven effectiveness), Scientific rigor (quality data), Therapeutic goals (clear outcomes). These 4 components guide beneficent care in 95% of clinical scenarios.
The beneficence framework operates through quantitative analysis of therapeutic interventions, utilizing metrics like Number Needed to Treat (NNT) and Quality-Adjusted Life Years (QALY) to optimize patient outcomes.
| Intervention Category | NNT Threshold | QALY Benefit | Cost-Effectiveness | Evidence Level |
|---|---|---|---|---|
| Preventive Care | <50 | >0.1 years | <$50,000/QALY | Level I |
| Acute Treatment | <10 | >0.5 years | <$100,000/QALY | Level I-II |
| Chronic Management | <20 | >1.0 years | <$75,000/QALY | Level I |
| Palliative Care | <5 | Quality focus | Variable | Level II-III |
| Experimental Therapy | <15 | >2.0 years | >$100,000/QALY | Level III |
- Systematic reviews provide highest evidence quality for intervention selection
- Meta-analyses of >1,000 patients offer robust effect size estimates
- Confidence intervals excluding null effect indicate significant benefit
- Heterogeneity measures <25% suggest consistent treatment effects
- Risk-Benefit Calculations
- Absolute risk reduction more clinically meaningful than relative risk
- Number Needed to Harm (NNH) should exceed NNT by 3-fold minimum
- Therapeutic index calculations guide dosing optimization
- Individual patient factors modify population-based recommendations
⭐ Clinical Pearl: Therapeutic inertia affects 40% of chronic disease management. Beneficence requires proactive optimization of existing therapies before adding new interventions. Medication reconciliation and adherence assessment often yield greater benefits than prescription additions.
💡 Master This: Proportionate vs. disproportionate interventions - beneficence requires matching treatment intensity to realistic outcomes. Futile care consumes resources without meaningful benefit, while undertreatment fails to optimize available therapeutic options. Balance intervention burden with expected benefit.
Beneficence extends to resource stewardship, ensuring efficient utilization of healthcare resources to maximize population benefit. Choosing Wisely campaigns identify low-value care that consumes resources without proportionate benefit, while comparative effectiveness research guides optimal intervention selection.
The beneficence principle creates systematic frameworks for treatment personalization, incorporating individual patient factors, preferences, and circumstances into evidence-based recommendations. This approach ensures therapeutic decisions optimize outcomes while respecting patient values and maintaining resource sustainability for broader healthcare access.
🛡️ The Beneficence Engine: Maximizing Patient Welfare
⚠️ The Safety Sentinel: Non-Maleficence Mastery
📌 Remember: SAFE - Systematic risk assessment (identify hazards), Adverse event prevention (proactive measures), Failure mode analysis (anticipate problems), Error reduction systems (safety culture). These 4 elements prevent >80% of preventable medical errors.
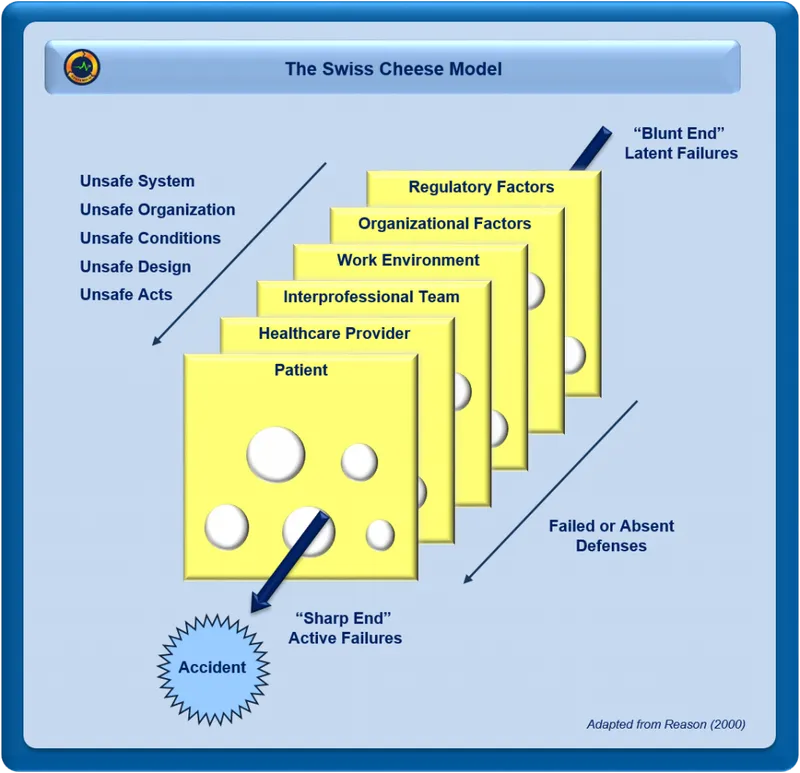
The non-maleficence framework operates through Swiss cheese model safety systems, where multiple protective layers prevent errors from reaching patients. High-reliability organizations achieve error rates <0.001% through systematic safety practices.
| Safety Domain | Error Rate | Prevention Strategy | Monitoring System | Intervention Threshold |
|---|---|---|---|---|
| Medication Safety | 1 in 300 doses | CPOE with alerts | Pharmacist review | >Level 3 interactions |
| Surgical Safety | 1 in 1,000 procedures | WHO checklist | Time-out protocols | Universal precautions |
| Diagnostic Safety | 10-15% misdiagnosis | Differential thinking | Cognitive aids | High-risk presentations |
| Communication | 70% of errors | SBAR protocols | Read-back verification | Critical values |
| Healthcare-Associated Infections | 1 in 25 patients | Bundle protocols | Surveillance systems | Outbreak thresholds |
- Failure Mode and Effects Analysis (FMEA) identifies high-risk processes
- Root Cause Analysis reveals system failures in 85% of serious events
- Human factors contribute to >90% of medical errors
- Latent conditions create error-prone situations before active failures
- Error Prevention Strategies
- Forcing functions make errors impossible rather than unlikely
- Redundant systems provide backup when primary safeguards fail
- Independent double-checks for high-alert medications
- Computerized alerts reduce prescribing errors by 55%
⭐ Clinical Pearl: Near-miss events occur 300 times more frequently than actual harm events. Proactive reporting and analysis of near-misses prevents future harm through system improvements. Create blame-free reporting culture to maximize safety learning opportunities.
💡 Master This: Proportionality principle - interventions must offer benefits that justify their risks. Low-probability, high-consequence risks require different management than high-probability, low-consequence risks. Tailor safety measures to actual risk profiles rather than perceived dangers.
Non-maleficence encompasses informed consent for risks, contraindication screening, and monitoring protocols that detect early signs of harm. Therapeutic drug monitoring prevents toxicity in narrow therapeutic index medications, while allergy documentation prevents life-threatening reactions.
The principle extends to resource allocation decisions, ensuring that beneficial interventions for some patients don't create harmful shortages for others. Triage protocols balance individual patient needs with population welfare, maintaining system capacity for emergency care while optimizing routine service delivery.
⚠️ The Safety Sentinel: Non-Maleficence Mastery
🏛️ Justice Frameworks: The Equity Engine
📌 Remember: FAIR - Fair distribution (equitable access), Allocation criteria (transparent standards), Impartial processes (bias-free decisions), Resource stewardship (sustainable systems). These 4 components guide just healthcare delivery in 90% of allocation scenarios.
The justice framework operates through multiple allocation models, each addressing different aspects of healthcare fairness. Utilitarian approaches maximize overall benefit, while egalitarian models emphasize equal access regardless of ability to pay.
| Allocation Model | Primary Criterion | Application Context | Outcome Measure | Ethical Justification |
|---|---|---|---|---|
| Medical Need | Severity of condition | Emergency care | Lives saved | Equal moral worth |
| Likelihood of Benefit | Probability of success | Organ transplant | Survival rates | Utility maximization |
| First-Come, First-Served | Temporal priority | Routine appointments | Access equity | Procedural fairness |
| Social Value | Contribution potential | Pandemic allocation | QALY maximization | Reciprocity |
| Lottery System | Random selection | Research enrollment | Equal opportunity | Impartial treatment |
- Oregon Health Plan prioritizes treatments by cost-effectiveness ratios
- UNOS organ allocation uses medical urgency and geographic proximity
- Pediatric priority for patients <18 years in liver allocation
- Blood type compatibility creates natural allocation boundaries
- Procedural Justice Requirements
- Transparent criteria published and consistently applied
- Appeals processes for allocation decisions with independent review
- Conflict of interest screening for allocation committee members
- Community representation in >50% of allocation committees
⭐ Clinical Pearl: Rule of rescue creates tension with utilitarian allocation - society often demands expensive interventions for identifiable individuals while accepting statistical deaths from underfunded prevention programs. Balance visible individual needs with invisible population benefits.
💡 Master This: Horizontal vs. vertical equity - treating similar cases similarly (horizontal) while providing different treatment for different needs (vertical). Equal treatment doesn't always mean identical treatment when patient circumstances differ significantly.
Justice extends to healthcare access across socioeconomic, geographic, and demographic boundaries. Social determinants of health create upstream inequities that healthcare systems must address through community partnerships and population health initiatives.
The principle encompasses research justice, ensuring that study populations reflect the diversity of patients who will receive interventions, while benefit-sharing guarantees that communities contributing to research gain access to resulting treatments. Global health equity considerations guide resource allocation between developed and developing healthcare systems.
🏛️ Justice Frameworks: The Equity Engine
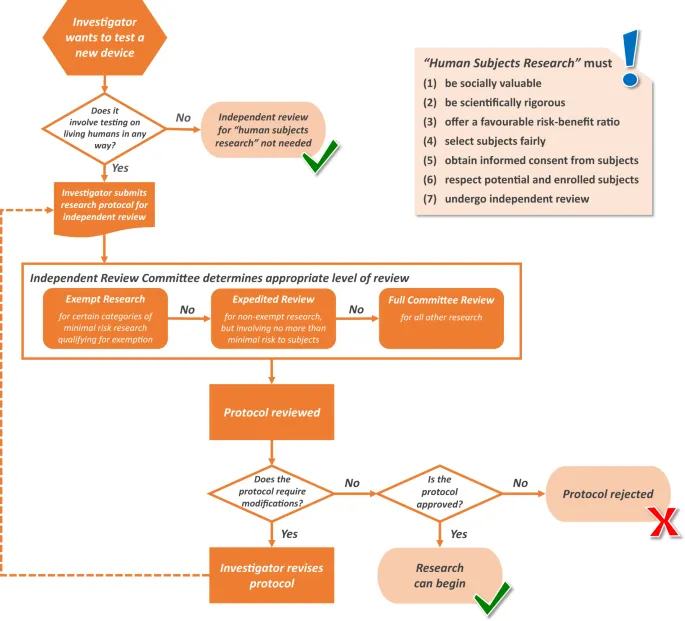
🔬 Research Ethics: The Scientific Integrity Matrix
📌 Remember: BELMONT - Beneficence (maximize benefits), Equity (fair selection), Lawful consent (voluntary participation), Minimize risks (safety first), Oversight (IRB review), Non-exploitation (protect vulnerable), Transparency (honest reporting). These 7 principles guide 100% of ethical research conduct.
The research ethics framework operates through Institutional Review Boards (IRBs) that provide independent oversight of human subjects research. Risk-benefit analysis ensures that potential benefits justify research risks, while informed consent protects participant autonomy.
| Research Category | IRB Review Level | Risk Assessment | Consent Requirements | Monitoring Intensity |
|---|---|---|---|---|
| Minimal Risk | Expedited review | <Daily life risk | Simplified consent | Annual reporting |
| Greater than Minimal | Full board review | >Routine examination | Comprehensive consent | Quarterly monitoring |
| Vulnerable Populations | Enhanced protection | Special safeguards | Advocate involvement | Monthly oversight |
| FDA-Regulated | Full review + FDA | Regulatory standards | 21 CFR 50 compliance | Continuous monitoring |
| International | Local + US IRB | Cultural considerations | Translated materials | Site visits |
- 8 required elements under 45 CFR 46 including purpose, procedures, risks
- 6 additional elements when appropriate including compensation, contact information
- Comprehension assessment required for complex studies
- Ongoing consent for long-term studies with evolving risks
- Vulnerable Population Protections
- Children require parental permission plus age-appropriate assent
- Prisoners need independent advocate and post-release benefit access
- Cognitive impairment requires capacity assessment and surrogate consent
- Economic vulnerability addressed through fair compensation without undue influence
⭐ Clinical Pearl: Therapeutic misconception affects >50% of research participants who believe research is designed primarily for their individual benefit rather than knowledge generation. Clear distinction between research and treatment prevents unrealistic expectations and ensures truly informed consent.
💡 Master This: Risk-benefit ratio must be favorable for study approval, but individual participants may have different risk tolerances. Personalized risk communication helps participants make autonomous decisions aligned with their values and circumstances.
Research ethics encompasses data integrity, publication standards, and conflict of interest management. Good Clinical Practice (GCP) guidelines ensure reliable and credible data, while CONSORT reporting standards promote transparent publication of trial results.
The framework extends to global research conducted in resource-limited settings, ensuring that standard of care controls are appropriate and that post-trial access to beneficial interventions is guaranteed. Community engagement and capacity building prevent research colonialism while advancing global health equity.
🔬 Research Ethics: The Scientific Integrity Matrix
🌐 Emerging Technologies: The Digital Ethics Frontier
📌 Remember: TECH - Transparency (explainable algorithms), Equity (bias prevention), Consent (informed authorization), Human oversight (physician judgment). These 4 principles guide ethical technology integration in 95% of digital health applications.
The technology ethics framework addresses algorithmic bias, data privacy, and digital divides that could exacerbate healthcare inequities. Machine learning models require diverse training data and continuous monitoring to prevent discriminatory outcomes.
| Technology Domain | Ethical Challenges | Regulatory Framework | Implementation Standards | Risk Mitigation |
|---|---|---|---|---|
| Artificial Intelligence | Algorithmic bias | FDA device approval | Explainable AI | Human oversight |
| Genetic Engineering | Enhancement vs. therapy | NIH guidelines | Germline restrictions | Informed consent |
| Telemedicine | Digital divide | State licensing | HIPAA compliance | Access equity |
| Wearable Devices | Privacy concerns | FDA + FTC | Data minimization | Consent granularity |
| Electronic Health Records | Interoperability | 21st Century Cures | Patient access | Security standards |
- Algorithmic auditing detects bias in >80% of healthcare AI systems
- Explainable AI requirements for high-stakes clinical decisions
- Training data must represent diverse patient populations
- Performance monitoring across demographic subgroups required
- Genetic Technology Governance
- Germline editing prohibited for reproductive purposes in >40 countries
- Somatic gene therapy requires enhanced informed consent protocols
- CRISPR applications limited to serious genetic diseases
- Enhancement applications raise justice and coercion concerns
⭐ Clinical Pearl: Digital therapeutics blur the line between medical devices and software applications. Evidence-based validation through randomized controlled trials should precede clinical adoption, just like traditional pharmaceuticals. Post-market surveillance monitors real-world effectiveness and safety.
💡 Master This: Data ownership in digital health remains legally ambiguous. Patients generate health data, but platforms collect and analyze it. Transparent data governance policies must specify use rights, sharing permissions, and deletion capabilities to maintain patient autonomy.
Technology ethics encompasses global digital health initiatives that must navigate cultural differences and resource disparities. Leapfrog technologies can improve healthcare access in underserved regions while avoiding technological colonialism that imposes inappropriate solutions.
The framework addresses intergenerational justice in technology adoption, ensuring that digital natives and technology-resistant populations receive equitable care. Universal design principles create accessible technologies that serve diverse user needs and capabilities.
🌐 Emerging Technologies: The Digital Ethics Frontier
🎯 Clinical Ethics Mastery: The Practitioner's Toolkit
📌 Remember: ETHICS - Evaluate principles (identify conflicts), Think systematically (structured analysis), Honor patient values (respect autonomy), Integrate evidence (informed decisions), Consult colleagues (seek guidance), Synthesize solutions (coherent action). These 6 steps resolve >90% of clinical ethical dilemmas.
| Ethical Dilemma Type | Primary Principles | Decision Framework | Consultation Triggers | Resolution Timeline |
|---|---|---|---|---|
| End-of-Life | Autonomy + Beneficence | Goals of care | Family conflict | 24-48 hours |
| Resource Allocation | Justice + Non-maleficence | Triage protocols | Scarcity situations | Immediate |
| Informed Consent | Autonomy + Beneficence | Capacity assessment | Complex procedures | Pre-procedure |
| Confidentiality | Autonomy + Justice | Duty to warn | Third-party risk | Immediate |
| Professional Boundaries | Non-maleficence + Justice | Therapeutic relationship | Boundary crossings | Immediate |
- 4-Box Method: Medical indications, patient preferences, quality of life, contextual features
- CASES approach: Clarify facts, Assess options, Solve systematically, Evaluate outcomes, Support implementation
- Stakeholder analysis identifies all affected parties and their interests
- Precedent review ensures consistent application of ethical standards
- Ethics Consultation Resources
- 24/7 ethics hotlines available in >75% of major medical centers
- Multidisciplinary ethics committees include physicians, nurses, chaplains, ethicists
- Case consultation response time <4 hours for urgent situations
- Policy development creates institutional guidance for recurring dilemmas
⭐ Clinical Pearl: Moral distress affects >60% of healthcare providers when they know the right action but cannot take it due to institutional constraints. Systematic ethics support and advocacy training help providers navigate these challenging situations while maintaining professional integrity.
💡 Master This: Ethical expertise develops through deliberate practice with complex cases, mentorship relationships, and continuing education. Case-based learning and simulation exercises build confidence in ethical decision-making before high-stakes situations arise.
The mastery toolkit encompasses documentation standards for ethical decisions, communication strategies for difficult conversations, and self-care practices that prevent moral injury. Reflective practice and peer consultation maintain ethical sensitivity while building decision-making confidence.
This comprehensive framework transforms ethical uncertainty into systematic analysis, enabling healthcare providers to serve patient interests while maintaining professional integrity and contributing to healthcare system improvement through ethical leadership and advocacy.
🎯 Clinical Ethics Mastery: The Practitioner's Toolkit
Practice Questions: Medical Ethics
Test your understanding with these related questions
A 42-year-old woman presents to the physician with symptoms of vague abdominal pain and bloating for several months. Test results indicate that she has ovarian cancer. Her physician attempts to reach her by phone multiple times but cannot reach her. Next of kin numbers are in her chart. According to HIPAA regulations, who should be the primary person the doctor discusses this information with?










