Teach-back method for consent discussions US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Teach-back method for consent discussions. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Teach-back method for consent discussions US Medical PG Question 1: An 83-year-old man presents to the gastroenterologist to follow-up on results from a biopsy of a pancreatic head mass, which the clinician was concerned could be pancreatic cancer. After welcoming the patient and his wife to the clinic, the physician begins to discuss the testing and leads into delivering the results, which showed metastatic pancreatic adenocarcinoma. Before she is able to disclose these findings, the patient stops her and exclaims, "Whatever it is, I don't want to know. Please just make me comfortable in my last months alive. I have made up my mind about this." Which of the following is the most appropriate response on the part of the physician?
- A. "If that is your definite wish, then I must honor it" (Correct Answer)
- B. "The cancer has spread to your liver"
- C. "As a physician, I am obligated to disclose these results to you"
- D. "If you don't know what condition you have, I will be unable to be your physician going forward"
- E. "Please, sir, I strongly urge you to reconsider your decision"
Teach-back method for consent discussions Explanation: ***"If that is your definite wish, then I must honor it"***
- This response respects the patient's **autonomy** and right to refuse information, aligning with ethical principles of patient-centered care.
- The patient has clearly and articulately stated his desire not to know and wishes for **palliative care**, which the physician should respect.
- The patient appears to have **decision-making capacity** based on his clear communication of wishes.
*"The cancer has spread to your liver"*
- This statement violates the patient's explicit request not to be informed of his diagnosis, potentially causing distress and undermining trust.
- Disclosure of information against a patient's wishes is unethical when the patient has **decision-making capacity** and has clearly refused information.
*"As a physician, I am obligated to disclose these results to you"*
- While physicians have a general duty to inform, this is superseded by a **competent patient's right to refuse information**.
- No absolute obligation exists to force information upon a patient who explicitly states a desire not to know, especially when it concerns their own health information.
*"If you don't know what condition you have, I will be unable to be your physician going forward"*
- This response is coercive and threatening, attempting to strong-arm the patient into accepting information he has refused.
- A physician's role includes managing symptoms and providing comfort, even if the patient chooses not to know the full diagnostic details of their condition, particularly in a **palliative care** context.
- This statement could constitute **patient abandonment**, which is unethical.
*"Please, sir, I strongly urge you to reconsider your decision"*
- While it's acceptable to ensure the patient fully understands the implications of their decision, a forceful "urge to reconsider" after a clear refusal can be seen as undermining their **autonomy**.
- The physician should confirm the patient's understanding and offer an opportunity to discuss it later if desired, rather than immediately pressuring them.
Teach-back method for consent discussions US Medical PG Question 2: A 19-year-old man presents to an orthopedic surgeon to discuss repair of his torn anterior cruciate ligament. He suffered the injury during a college basketball game 1 week ago and has been using a knee immobilizer since the accident. His past medical history is significant for an emergency appendectomy when he was 12 years of age. At that time, he said that he never wanted to have surgery again. At this visit, the physician explains the procedure to him in detail including potential risks and complications. The patient acknowledges and communicates his understanding of both the diagnosis as well as the surgery and decides to proceed with the surgery in 3 weeks. Afterward, he signs a form giving consent for the operation. Which of the following statements is true about this patient?
- A. He cannot provide consent because he lacks capacity
- B. He has the right to revoke his consent at any time (Correct Answer)
- C. His parents also need to give consent to this operation
- D. He did not need to provide consent for this procedure since it is obviously beneficial
- E. His consent is invalid because his decision is not stable over time
Teach-back method for consent discussions Explanation: ***He has the right to revoke his consent at any time***
- **Informed consent** for medical procedures is an ongoing process, and a patient retains the right to **withdraw consent** at any point, even after initially signing the consent form.
- This right is a fundamental aspect of patient autonomy and ensures that medical interventions are only performed with a patient's current and willing agreement.
*He cannot provide consent because he lacks capacity*
- The patient is 19 years old, which in most jurisdictions (including the US where the age of majority is typically 18) means he is considered an **adult** and legally capable of providing his own consent.
- The scenario explicitly states he "communicates his understanding of both the diagnosis as well as the surgery," indicating he possesses the **mental capacity** to make an informed decision.
*His parents also need to give consent to this operation*
- As a 19-year-old, the patient has reached the **age of majority** and is legally entitled to make his own medical decisions, including consenting to surgery.
- Parental consent is generally required for minors (individuals under the age of majority), but not for adults like this patient.
*He did not need to provide consent for this procedure since it is obviously beneficial*
- Even for procedures that are clearly **beneficial**, informed consent is ethically and legally mandatory to uphold **patient autonomy** and ensure respect for individual rights.
- The concept of "obviously beneficial" does not negate the requirement for a patient's explicit agreement to a medical intervention.
*His consent is invalid because his decision is not stable over time*
- While the patient might have initially hated surgery at age 12, his current decision at age 19 to proceed with the ACL repair is based on current information and his mature understanding.
- The fact that his previous aversion to surgery has changed does not invalidate his current, well-informed decision; it simply indicates a change in perspective based on new circumstances and greater maturity.
Teach-back method for consent discussions US Medical PG Question 3: A 25-year-old man comes to the physician for severe back pain. He describes the pain as shooting and stabbing. On a 10-point scale, he rates the pain as a 9 to 10. The pain started after he lifted a heavy box at work; he works at a supermarket and recently switched from being a cashier to a storekeeper. The patient appears to be in severe distress. Vital signs are within normal limits. On physical examination, the spine is nontender without paravertebral muscle spasms. Range of motion is normal. A straight-leg raise test is negative. After the physical examination has been completed, the patient asks for a letter to his employer attesting to his inability to work as a storekeeper. Which of the following is the most appropriate response?
- A. “Yes. Since work may worsen your condition, I would prefer that you stay home a few days. I will write a letter to your employer to explain the situation.”
- B. You say you are in severe pain. However, the physical examination findings do not suggest a physical problem that can be addressed with medications or surgery. I'd like to meet on a regular basis to see how you're doing.
- C. I understand that you are uncomfortable, but the findings do not match the severity of your symptoms. Let's talk about the recent changes at your job. (Correct Answer)
- D. The physical exam findings do not match your symptoms, which suggests a psychological problem. I would be happy to refer you to a mental health professional.
- E. The physical exam findings suggest a psychological rather than a physical problem. But there is a good chance that we can address it with cognitive-behavioral therapy.
Teach-back method for consent discussions Explanation: ***"I understand that you are uncomfortable, but the findings do not match the severity of your symptoms. Let's talk about the recent changes at your job."***
- This response acknowledges the patient's reported discomfort while gently highlighting the **discrepancy between symptoms and objective findings**, which is crucial in cases of suspected **somatoform or functional pain**.
- It also opens communication about potential **psychosocial stressors** related to his job change, which could be contributing to his symptoms, without dismissing his pain or making a premature diagnosis.
*"You say you are in severe pain. However, the physical examination findings do not suggest a physical problem that can be addressed with medications or surgery. I'd like to meet on a regular basis to see how you're doing."*
- While this option correctly identifies the lack of physical findings, it can be perceived as dismissive of the patient's pain, potentially damaging the **physician-patient relationship**.
- Suggesting regular meetings without a clear plan for addressing his immediate concerns or exploring underlying issues might not be the most effective initial approach.
*“Yes. Since work may worsen your condition, I would prefer that you stay home a few days. I will write a letter to your employer to explain the situation.”*
- This response would **validate the patient's claim of severe pain** without objective evidence, potentially reinforcing illness behavior and avoiding addressing the underlying issue.
- Providing a doctor's note for inability to work without a clear diagnostic basis or understanding of the pain's origin is **medically inappropriate** and could set a precedent for future such requests.
*"The physical exam findings do not match your symptoms, which suggests a psychological problem. I would be happy to refer you to a mental health professional."*
- Directly labeling the problem as "psychological" can be **stigmatizing and alienating** to the patient, leading to distrust and resistance to care.
- While a psychological component might be present, immediately referring to mental health without further exploration of the patient's situation or current stressors is premature and lacks empathy.
*"The physical exam findings suggest a psychological rather than a physical problem. But there is a good chance that we can address it with cognitive-behavioral therapy."*
- Similar to the previous option, explicitly stating a "psychological problem" can be **stigmatizing**.
- Jumping directly to recommending **cognitive-behavioral therapy (CBT)** without a comprehensive discussion and patient buy-in is premature and may lead to non-compliance.
Teach-back method for consent discussions US Medical PG Question 4: A 15-year-old girl is brought to the physician by her mother for an annual well-child examination. Her mother complains that the patient has a poor diet and spends most of the evening at home texting her friends instead of doing homework. She has been caught smoking cigarettes in the school bathroom several times and appears indifferent to the dean's threats of suspension. Two weeks ago, the patient allowed a friend to pierce her ears with unsterilized safety pins. The mother appeals to the physician to lecture the patient about her behavior and “set her straight.” The patient appears aloof and does not make eye contact. Her grooming is poor. Upon questioning the daughter about her mood, the mother responds “She acts like a rebel. I can't wait until puberty is over.” Which of the following is the most appropriate response?
- A. You should listen to your mother's concerns. You don't want to make poor choices early on or else you might end up on the streets.
- B. Would it be possible for you to step out for a few moments so that I can interview your daughter alone? (Correct Answer)
- C. Let's run a routine urine toxicology screen to make sure your daughter is not doing drugs.
- D. I am very concerned that your daughter is displaying signs of depression, and I'd suggest that she is seen by a psychiatrist.
- E. Your daughter displays normal signs of puberty. Being overly critical of your daughter is not helpful.
Teach-back method for consent discussions Explanation: ***"Would it be possible for you to step out for a few moments so that I can interview your daughter alone?"***
- This approach respects the adolescent's **autonomy** and provides a safe space for her to disclose sensitive information without parental presence.
- Adolescents are more likely to be **candid** about risky behaviors like smoking, substance use, or sexual activity if they feel their privacy is protected.
*"You should listen to your mother's concerns. You don't want to make poor choices early on or else you might end up on the streets."*
- This response is **confrontational** and judgmental, which is likely to alienate the patient and shut down communication.
- It also uses **fear tactics** rather than fostering trust and a therapeutic relationship.
*"Let's run a routine urine toxicology screen to make sure your daughter is not doing drugs."*
- While drug use is a concern given her risky behaviors, immediately suggesting a **toxicology screen** without building rapport can feel accusatory and escalate distrust.
- It's often more effective to establish communication first before moving to definitive testing, especially in a well-child visit where drug use has not been directly admitted.
*"I am very concerned that your daughter is displaying signs of depression, and I'd suggest that she is seen by a psychiatrist."*
- While some of the patient's behaviors (poor grooming, aloofness, indifference) could be consistent with **depression**, immediately jumping to a diagnosis and referral without a direct interview is premature.
- It can also be perceived as labeling and might be rejected by the patient and mother without further exploration.
*"Your daughter displays normal signs of puberty. Being overly critical of your daughter is not helpful."*
- This response dismisses the mother's valid concerns about genuinely **risky behaviors** (smoking, unsterilized piercing, indifference to consequences) as "normal puberty."
- It also implicitly criticizes the mother, which can damage the therapeutic alliance with both the parent and the patient.
Teach-back method for consent discussions US Medical PG Question 5: An orthopaedic surgeon at a local community hospital has noticed that turnover times in the operating room have been unnecessarily long. She believes that the long wait times may be due to inefficient communication between the surgical nursing staff, the staff in the pre-operative area, and the staff in the post-operative receiving area. She believes a secure communication mobile phone app would help to streamline communication between providers and improve efficiency in turnover times. Which of the following methods is most appropriate to evaluate the impact of this intervention in the clinical setting?
- A. Plan-Do-Study-Act cycle (Correct Answer)
- B. Failure modes and effects analysis
- C. Standardization
- D. Forcing function
- E. Root cause analysis
Teach-back method for consent discussions Explanation: ***Plan-Do-Study-Act cycle***
- The **Plan-Do-Study-Act (PDSA) cycle** is a structured, iterative model used for continuous improvement in quality and efficiency, making it ideal for evaluating the impact of a new intervention like a communication app.
- This cycle allows for small-scale testing of changes, observation of results, learning from the observations, and refinement of the intervention before full implementation.
*Failure modes and effects analysis*
- **Failure modes and effects analysis (FMEA)** is a prospective method to identify potential failures in a process, predict their effects, and prioritize actions to prevent them.
- While useful for process improvement, FMEA is typically performed *before* implementing a change to identify risks, rather than to evaluate the impact of an already implemented intervention.
*Standardization*
- **Standardization** involves creating and implementing consistent processes or protocols to reduce variability and improve reliability.
- While the communication app might contribute to standardization, standardization itself is a *method of improvement* rather than a method for *evaluating the impact* of an intervention.
*Forcing function*
- A **forcing function** is a design feature that physically prevents an error from occurring, making it impossible to complete a task incorrectly.
- An app that streamlines communication does not act as a forcing function, as it facilitates a process rather than physically preventing an incorrect action.
*Root cause analysis*
- **Root cause analysis (RCA)** is a retrospective method used to investigate an event that has already occurred (e.g., an adverse event) to identify its underlying causes.
- This method is used *after* a problem has manifested to understand *why* it happened, not to evaluate the *impact* of a new intervention designed to prevent future problems.
Teach-back method for consent discussions US Medical PG Question 6: A 14-year-old girl presents to the emergency room complaining of abdominal pain. She was watching a movie 3 hours prior to presentation when she developed severe non-radiating right lower quadrant pain. The pain has worsened since it started. She also had non-bloody non-bilious emesis 1 hour ago and continues to feel nauseated. Her temperature is 101°F (38.3°C), blood pressure is 130/90 mmHg, pulse is 110/min, and respirations are 22/min. On exam, she has rebound tenderness at McBurney point and a positive Rovsing sign. She is stabilized with intravenous fluids and pain medication and is taken to the operating room to undergo a laparoscopic appendectomy. While in the operating room, the circulating nurse leads the surgical team in a time out to ensure that introductions are made, the patient’s name and date of birth are correct, antibiotics have been given, and the surgical site is marked appropriately. This process is an example of which of the following human factor engineering elements?
- A. Forcing function
- B. Safety culture
- C. Simplification
- D. Standardization (Correct Answer)
- E. Resilience engineering
Teach-back method for consent discussions Explanation: ***Standardization***
- The surgical **time-out** is a prime example of **standardization** in healthcare, as it involves a prescribed, uniform procedure followed in every surgery to enhance safety.
- It ensures critical safety checks—like patient identification, site marking, and antibiotic administration—are consistently performed, thus reducing variability and the potential for errors.
*Forcing function*
- A **forcing function** is a design element that makes it impossible to commit an error, such as a specific connector shape that prevents incorrect device attachment.
- The time-out, while a critical safeguard, still relies on human compliance and does not physically prevent an error from occurring if the steps are not followed.
*Safety culture*
- **Safety culture** refers to the shared beliefs, values, and attitudes that employees have about safety within an organization.
- While a time-out contributes to a strong safety culture, it is a specific process or tool, not the overarching culture itself.
*Simplification*
- **Simplification** aims to reduce complexity in a process to minimize cognitive load and potential for error.
- The time-out adds a structured step rather than simplifying an existing process; its purpose is to ensure all necessary checks are systematically completed.
*Resilience engineering*
- **Resilience engineering** focuses on an organization's ability to anticipate, cope with, and recover from failures, maintaining stability in the face of disruptions.
- While the time-out promotes safety, it primarily addresses error prevention rather than the broader organizational capacity to adapt and recover from system failures.
Teach-back method for consent discussions US Medical PG Question 7: A 16-year-old female presents to her pediatrician's office requesting to be started on an oral contraceptive pill. She has no significant past medical history and is not currently taking any medications. The physician is a devout member of the Roman Catholic church and is strongly opposed to the use of any type of artificial contraception. Which of the following is the most appropriate response to this patient's request?
- A. Suggest that the patient remain abstinent or, if necessary, use an alternative means of birth control
- B. Explain that he will refer the patient to one of his partners who can fulfill this request (Correct Answer)
- C. Refuse to prescribe the oral contraceptive
- D. Tell the patient that he is unable to prescribe this medication without parental consent
- E. The physician is obligated to prescribe the oral contraceptives regardless of his personal beliefs
Teach-back method for consent discussions Explanation: ***Explain that he will refer the patient to one of his partners who can fulfill this request***
- Physicians have a right to **conscientious objection** based on personal beliefs, but they also have an ethical obligation to ensure that patients receive appropriate medical care.
- Referring the patient to another qualified provider for the requested service fulfills both the physician's right to object and the patient's right to care, without imposing the physician's personal beliefs on the patient.
*Suggest that the patient remain abstinent or, if necessary, use an alternative means of birth control*
- While abstinence is a valid choice, suggesting it without offering the requested medical service is imposing the physician's personal beliefs on the patient, which is **unethical** in this context.
- Recommending only "alternative means" without directly addressing the patient's specific request for oral contraceptives does not adequately address her healthcare needs or autonomy.
*Refuse to prescribe the oral contraceptive*
- An outright refusal without providing an alternative option or referral **violates the ethical principle** of beneficence and the patient's right to access medical care.
- This action could be seen as abandoning the patient and is not consistent with professional medical ethics for handling conscientious objections.
*Tell the patient that he is unable to prescribe this medication without parental consent*
- In many jurisdictions, minors are legally allowed to obtain contraception **without parental consent** due to privacy and public health considerations (e.g., prevention of STIs and unintended pregnancies).
- This statement may be **legally incorrect** and serves as an excuse to avoid providing the requested service, rather than addressing the ethical dilemma of conscientious objection appropriately.
*The physician is obligated to prescribe the oral contraceptives regardless of his personal beliefs*
- While physicians have an obligation to provide care, they are generally **not obligated to perform services that violate their deeply held moral or religious beliefs**, provided they ensure the patient can access the service elsewhere.
- This option incorrectly states that personal beliefs must always be overridden for every medical service, ignoring the principle of conscientious objection while ensuring patient access to care.
Teach-back method for consent discussions US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Teach-back method for consent discussions Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Teach-back method for consent discussions US Medical PG Question 9: A 69-year-old woman with acute myeloid leukemia comes to the physician to discuss future treatment plans. She expresses interest in learning more about an experimental therapy being offered for her condition. After the physician explains the mechanism of the drug and describes the risks and benefits, the patient then states that she is not ready to die. When the physician asks her what her understanding of the therapy is, she responds "I don't remember the details, but I just know that I definitely want to try it, because I don't want to die." Which of the following ethical principles is compromised in this physician's interaction with the patient?
- A. Patient competence
- B. Patient autonomy
- C. Decision-making capacity (Correct Answer)
- D. Information disclosure
- E. Therapeutic privilege
Teach-back method for consent discussions Explanation: ***Decision-making capacity***
- This refers to a patient's ability to **understand information relevant to a medical decision**, appreciate their situation, reason through options, and communicate a choice. The patient's statement indicates a lack of understanding of the details of the complex treatment, despite being explained.
- While she expresses a choice, her inability to recall details suggests she cannot adequately **weigh risks and benefits**, which is central to capacity.
*Patient competence*
- **Competence is a legal determination** made by a court, not by a physician in a clinical setting.
- Physicians assess **decision-making capacity**, which is a clinical judgment, whereas legal competence has broader implications.
*Patient autonomy*
- **Autonomy is the right of a patient to make their own choices** about their medical care. While the patient is attempting to exercise a choice, the issue here is whether she is able to make an adequately informed choice.
- For autonomy to be truly upheld, the patient must have the **capacity to make an informed decision**, which is compromised by her stated lack of understanding.
*Information disclosure*
- The physician *did* disclose information about the drug's mechanism, risks, and benefits, indicating that the act of disclosure itself was performed.
- The problem is not that information was withheld, but that the patient **did not retain or understand the disclosed information** sufficiently.
*Therapeutic privilege*
- **Therapeutic privilege** is when a physician withholds information from a patient if they believe the disclosure would cause significant harm.
- In this scenario, the physician *did* explain the treatment, so information was not withheld under privilege.
Teach-back method for consent discussions US Medical PG Question 10: A 34-year-old man presents to the local clinic with a 2 month history of midsternal chest pain following meals. He has a past medical history of hypertension. The patient takes lisinopril daily. He drinks 4–5 cans of 12 ounce beer daily, and chews 2 tins of smokeless tobacco every day. The vital signs are currently stable. Physical examination shows a patient who is alert and oriented to person, place, and time. Palpation of the epigastric region elicits mild tenderness. Percussion is normoresonant in all 4 quadrants. Murphy’s sign is negative. Electrocardiogram shows sinus rhythm with no acute ST segment or T wave changes. The physician decides to initiate a trial of omeprazole to treat the patient’s gastroesophageal reflux disease. How can the physician most effectively assure that this patient will adhere to the medication regimen?
- A. Instruct the patient to purchase a weekly pill organizer
- B. Have the patient repeat back to the physician the name of the medication, dosage, and frequency (Correct Answer)
- C. Provide the patient with details of the medication on a print-out
- D. Contact the pharmacist because they can explain the details more thoroughly
- E. Tell the patient to write the medication name, dosage, and frequency on their calendar at home
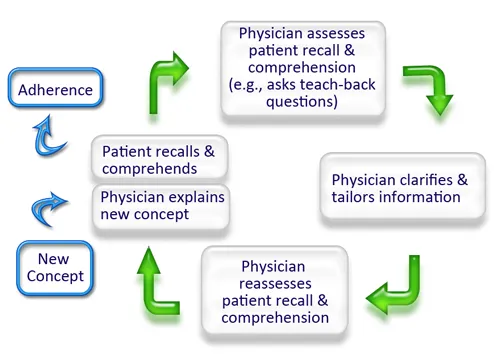
Teach-back method for consent discussions Explanation: ***Have the patient repeat back to the physician the name of the medication, dosage, and frequency***
- The **"teach-back" method** is an effective way to confirm patient understanding and improve adherence by having the patient restate information in their own words.
- This method allows the physician to identify and clarify any misunderstandings immediately, ensuring the patient comprehends the **medication regimen**.
*Instruct the patient to purchase a weekly pill organizer*
- While a **pill organizer** can be helpful for medication organization, simply telling the patient to buy one does not guarantee they will understand or consistently use it.
- It does not address the fundamental issue of ensuring the patient fully comprehends the **medication instructions** and its importance.
*Provide the patient with details of the medication on a print-out*
- A print-out provides information, but merely giving a patient a **document** does not confirm they have read, understood, or retained the information.
- Many patients may not read or fully comprehend written materials, making it less effective than active engagement methods like **teach-back**.
*Contact the pharmacist because they can explain the details more thoroughly*
- Pharmacists play a crucial role in medication education, but delegating the primary explanation entirely removes the physician's opportunity to assess the patient's immediate understanding and address concerns directly.
- The **physician-patient interaction** is a key moment for establishing a shared understanding of the treatment plan.
*Tell the patient to write the medication name, dosage, and frequency on their calendar at home*
- This method relies on the patient's ability and willingness to *independently* record and recall information, which may not be sufficient for comprehensive understanding or adherence.
- It does not provide an immediate feedback loop for the physician to assess the patient's comprehension of the **treatment plan**.
More Teach-back method for consent discussions US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.