Security Rule requirements US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Security Rule requirements. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Security Rule requirements US Medical PG Question 1: A 79-year-old male presents to your office for his annual flu shot. On physical exam you note several linear bruises on his back. Upon further questioning he denies abuse from his daughter and son-in-law, who live in the same house. The patient states he does not want this information shared with anyone. What is the most appropriate next step, paired with its justification?
- A. Breach patient confidentiality, as this patient's care should be discussed with the daughter as she is his primary caregiver
- B. See the patient back in 2 weeks and assess whether the patient's condition has improved, as his condition is not severe
- C. Do not break patient confidentiality, as elder abuse reporting is not mandatory
- D. Do not break patient confidentiality, as this would potentially worsen the situation
- E. Breach patient confidentiality, as this patient is a potential victim of elder abuse and reporting is mandated in most states (Correct Answer)
Security Rule requirements Explanation: ***Breach patient confidentiality, as this patient is a potential victim of elder abuse and reporting is mandated in most states***
- As a physician, there is a **legal and ethical obligation** to report suspected elder abuse in most US states, even when the patient denies it and requests confidentiality.
- Physicians are typically **mandatory reporters** under state law, and must report to Adult Protective Services or law enforcement when elder abuse is suspected.
- The patient's safety and legal requirements outweigh the right to confidentiality in jurisdictions with mandatory reporting laws.
*Breach patient confidentiality, as this patient's care should be discussed with the daughter as she is his primary caregiver*
- Breaching confidentiality to discuss this with the daughter would be inappropriate, especially since the daughter and son-in-law are the **suspected abusers**.
- Discussing with the primary caregiver is only appropriate if the patient has given **explicit consent** and there are no suspicions of abuse from that caregiver.
*See the patient back in 2 weeks and assess whether the patient's condition has improved, as his condition is not severe*
- This option is inappropriate because it delays intervention in a potentially **dangerous situation**.
- Suspected abuse warrants **immediate action** to ensure the patient's safety, regardless of the perceived severity of current injuries.
*Do not break patient confidentiality, as elder abuse reporting is not mandatory*
- In **most states**, physicians have **mandatory reporting laws** for elder abuse, making this statement generally incorrect.
- Physicians are typically considered "mandated reporters" and are legally required to report suspected abuse to the appropriate authorities in their jurisdiction.
*Do not break patient confidentiality, as this would potentially worsen the situation*
- While this is a valid concern in some situations, the **primary responsibility** of a physician is to protect vulnerable patients from harm.
- Reporting suspected abuse initiates protective measures and is legally required in most states, as the potential benefit of intervention outweighs the risk of worsening the situation.
Security Rule requirements US Medical PG Question 2: The surgical equipment used during a craniectomy is sterilized using pressurized steam at 121°C for 15 minutes. Reuse of these instruments can cause transmission of which of the following pathogens?
- A. Non-enveloped viruses
- B. Sporulating bacteria
- C. Prions (Correct Answer)
- D. Enveloped viruses
- E. Yeasts
Security Rule requirements Explanation: ***Prions***
- Prions are **abnormally folded proteins** that are highly resistant to standard sterilization methods like steam autoclaving at 121°C, making them a risk for transmission through reused surgical instruments.
- They cause transmissible spongiform encephalopathies (TSEs) like **Creutzfeldt-Jakob disease**, where even trace amounts can be highly infectious.
*Non-enveloped viruses*
- Non-enveloped viruses are generally **more resistant to heat and disinfectants** than enveloped viruses but are typically inactivated by recommended steam sterilization protocols.
- Standard autoclaving conditions are effective in destroying most non-enveloped viruses.
*Sporulating bacteria*
- **Bacterial spores**, such as those from *Clostridium* or *Bacillus*, are known for their high resistance to heat and chemicals, but are usually **inactivated by steam sterilization at 121°C** for 15 minutes.
- This method is specifically designed to kill bacterial spores effectively.
*Enveloped viruses*
- Enveloped viruses are the **least resistant to heat and chemical disinfectants** due to their lipid envelope.
- They are readily **inactivated by standard steam sterilization** at 121°C.
*Yeasts*
- **Yeasts** are eukaryotic microorganisms that are typically **susceptible to heat sterilization**.
- They are effectively killed by typical steam autoclaving conditions used for surgical instruments.
Security Rule requirements US Medical PG Question 3: A 38-year-old project manager is told by her boss that her team will need to work on an additional project in the coming week for a very important client. This frustrates the woman, who already feels that she works too many hours. Instead of discussing her feelings directly with her boss, the woman leaves a voice message for her boss the next day and deceitfully says she cannot come to work for the next week because of a family emergency. Which of the following psychological defense mechanisms is this individual demonstrating?
- A. Displacement
- B. Acting out
- C. Malingering
- D. Passive aggression (Correct Answer)
- E. Blocking
Security Rule requirements Explanation: ***Passive aggression***
- This defense mechanism involves expressing negative feelings indirectly instead of openly addressing the conflict or frustrating situation. The woman's **deceitful excuse** avoids confrontation while still 'punishing' the boss by not being available.
- It often stems from a fear of direct confrontation and a need to control the situation without appearing openly hostile, manifesting as **procrastination, stubbornness, or intentional inefficiency**.
*Displacement*
- **Displacement** occurs when a person redirects uncomfortable feelings from the source of frustration to a safer, less threatening target.
- In this scenario, the woman did not redirect her frustration onto another person or object; instead, she acted on the source of the frustration indirectly.
*Acting out*
- **Acting out** involves expressing unconscious emotional conflicts or stressors through immediate physical actions, often impulsive or destructive.
- The woman's behavior, while deceitful, is a calculated avoidance rather than an uncontrolled emotional outburst.
*Malingering*
- **Malingering** is the intentional production of false or grossly exaggerated physical or psychological symptoms, motivated by external incentives like avoiding work or obtaining financial compensation.
- While there is an element of deceit, the primary motivation described is her frustration and desire to avoid the extra work, not necessarily an external material gain typically associated with malingering.
*Blocking*
- **Blocking** is a defense mechanism characterized by a temporary but sudden and complete loss of thought, often due to an emotional conflict. The individual's mind goes blank.
- The woman is not experiencing a loss of thought but is actively fabricating an excuse to avoid a difficult situation.
Security Rule requirements US Medical PG Question 4: A 45-year-old man is brought to the emergency department by his friends because of a 1-hour history of shortness of breath and squeezing chest pain. They were at a party where cocaine was consumed. A diagnosis of acute myocardial infarction is made. The physician stabilizes the patient and transfers him to the inpatient unit. Six hours later, his wife arrives at the emergency department and requests information about her husband's condition. Which of the following is the most appropriate action by the physician?
- A. Ask the wife for a marriage certificate
- B. Inform the wife about her husband's condition
- C. Consult the hospital ethics committee
- D. Obtain authorization from the patient to release information (Correct Answer)
- E. Request the patient's durable power of attorney document
Security Rule requirements Explanation: ***Obtain authorization from the patient to release information***
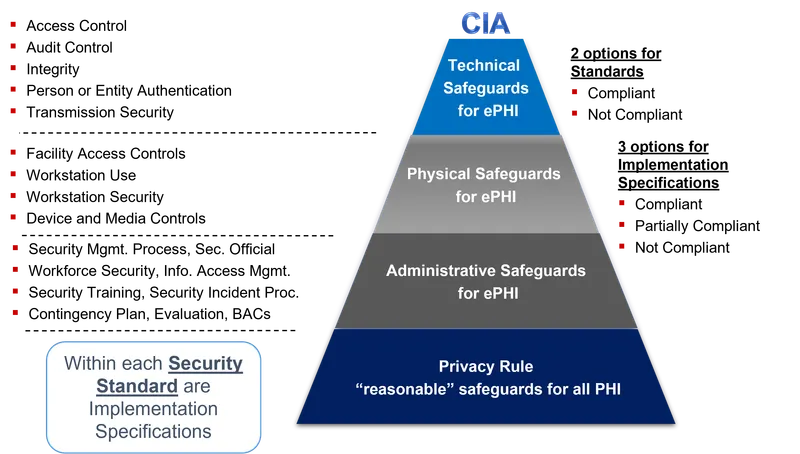
- Under **HIPAA (Health Insurance Portability and Accountability Act)**, patient information is confidential and cannot be shared without their express consent, even with close family members like a spouse, once the patient is **conscious and able to make decisions**.
- The patient, being stabilized, is likely **competent** to authorize the release of his medical information to his wife, ensuring his **autonomy** and privacy are respected.
*Ask the wife for a marriage certificate*
- A marriage certificate does not automatically grant access to a spouse's medical information if the patient is **competent** and has not provided consent.
- Requesting such documentation is generally **not standard practice** and does not supersede the need for patient authorization under HIPAA.
*Inform the wife about her husband's condition*
- Releasing medical information without the patient's explicit consent would be a direct **violation of patient confidentiality** and **HIPAA regulations**, even if the individual is a spouse.
- Although well-intentioned, this action could have legal and ethical repercussions for the physician and the hospital.
*Consult the hospital ethics committee*
- While ethics committees handle complex ethical dilemmas, this situation is a straightforward matter of **patient confidentiality** and **HIPAA compliance**.
- The direct course of action is to seek patient authorization, rather than escalating to an ethics committee for a clearly defined privacy issue.
*Request the patient's durable power of attorney document*
- A **durable power of attorney (DPOA)** for healthcare is only activated when a patient is **incapacitated** and unable to make decisions for themselves.
- Since the patient is stabilized and presumably competent to make decisions about his care, a DPOA is not relevant at this time.
Security Rule requirements US Medical PG Question 5: A 62-year-old man comes to his primary care physician with a 3-month history of insomnia and severe work anxiety. He says that he is unable to retire because he has no financial resources; however, the stress level at his work has been causing him to have worsening performance and he is afraid of being fired. He thinks that he would be able to resume work normally if he was able to decrease his level of anxiety. His physician prescribes him a trial 1-month regimen of benzodiazepine therapy and schedules a follow-up appointment to see whether this treatment has been effective. Three weeks later, the patient's wife calls and says "My husband was fired from work and it's your fault for prescribing that medication! I know he must have been taking too much of that drug. Don't you know that he had a horrible problem with drug abuse in his 30s?" Which of the following is the most appropriate first action for the physician to take?
- A. Discharge the patient for inappropriate use of medication
- B. Contact the physician's medical practice insurance company regarding a potential claim
- C. Refer the patient to a substance abuse program
- D. Contact the patient directly to discuss the situation (Correct Answer)
- E. Inform the patient's wife that patient information cannot be disclosed to her due to HIPAA
Security Rule requirements Explanation: ***Contact the patient directly to discuss the situation***
- The physician's immediate priority is to address the patient's well-being and medication use directly with the patient, as the patient-doctor relationship is paramount and confidential.
- This allows the physician to gather information directly from the patient, assess the current situation, and plan appropriate next steps, which may include medication adjustment, referral, or relapse prevention depending on the patient's account.
*Discharge the patient for inappropriate use of medication*
- Discharging the patient based solely on a third-party report, especially without direct communication with the patient, would be premature and could be interpreted as **patient abandonment**.
- This action does not prioritize the patient's immediate medical and psychological needs and could worsen their situation by removing them from care.
*Contact the physician's medical practice insurance company regarding a potential claim*
- While potential legal implications exist, contacting the insurance company is not the **first and most appropriate medical action** to take.
- The immediate priority is the patient's health and safety, and managing potential legal risks can be addressed after ensuring the patient's well-being.
*Refer the patient to a substance abuse program*
- Although the patient's history and the wife's concerns suggest a potential for substance abuse, a direct referral without first assessing the patient and confirming misuse would be premature.
- The physician needs to **personally evaluate the patient** to determine the appropriate course of action, which might include such a referral, but it shouldn't be the very first step based on indirect information.
*Inform the patient's wife that patient information cannot be disclosed to her due to HIPAA*
- While the physician can listen to the wife's concerns (HIPAA does not prohibit receiving information from third parties), the physician **cannot discuss the patient's care or confirm treatment details** without the patient's authorization.
- However, simply informing the wife about confidentiality restrictions without taking action to contact and assess the patient is not the most appropriate first step—the priority is patient care, not just explaining privacy rules.
Security Rule requirements US Medical PG Question 6: A 26-year-old man comes to the emergency department because of a 1-week history of fever, throat pain, and difficulty swallowing. Head and neck examination shows an erythematous pharynx with purulent exudates overlying the palatine tonsils. Microscopic examination of a throat culture shows pink, spherical bacteria arranged in chains. Treatment with amoxicillin is initiated. A day later, a physician colleague from another department approaches the physician in the lobby of the hospital and asks about this patient, saying, "Did you see him? What does he have? He's someone I play football with and he hasn't come to play for the past 5 days. I'm worried about him." Which of the following is the most appropriate action by the physician?
- A. Inform the colleague that they should ask the patient's attending physician
- B. Inform the colleague that they cannot divulge any information about the patient (Correct Answer)
- C. Tell the colleague the patient's case file number so they can look it up themselves
- D. Tell the colleague that they cannot tell them the diagnosis but that their friend was treated with antibiotics
- E. Ask the colleague to meet in the office so they can discuss the patient in private
Security Rule requirements Explanation: ***Inform the colleague that they cannot divulge any information about the patient***
- The **Health Insurance Portability and Accountability Act (HIPAA)** strictly prohibits the disclosure of a patient's **Protected Health Information (PHI)** without their explicit consent.
- Even if the inquirer knows the patient, a physician-patient relationship creates a **duty of confidentiality** that supersedes personal acquaintance.
- Disclosing any information without patient consent, even to another physician, violates HIPAA regulations.
*Tell the colleague the patient's case file number so they can look it up themselves*
- Providing the case file number would enable unauthorized access to the patient's medical records, thereby violating **patient confidentiality** and **HIPAA regulations**.
- This action does not rectify the breach of confidentiality and escalates the potential for further misuse of PHI.
*Inform the colleague that they should ask the patient's attending physician*
- Recommending that the colleague ask the attending physician shifts the burden but does not address the underlying ethical and legal obligation of the current physician to maintain **confidentiality**.
- The attending physician would also be bound by **HIPAA** and ethical guidelines not to disclose information without consent.
*Tell the colleague that they cannot tell them the diagnosis but that their friend was treated with antibiotics*
- While seemingly less specific, stating that the friend was treated with **antibiotics** is still a disclosure of **Protected Health Information (PHI)**.
- This action violates **patient confidentiality** as it reveals a detail of the patient's medical management without consent.
*Ask the colleague to meet in the office so they can discuss the patient in private*
- Moving to a private setting does not negate the fact that discussing the patient's information with an unauthorized individual is a **breach of confidentiality**.
- The location of the conversation does not change the ethical and legal obligations to protect **PHI**.
Security Rule requirements US Medical PG Question 7: An 86-year-old man is admitted to the hospital for management of pneumonia. His hospital course has been relatively uneventful, and he is progressing well. On morning rounds nearing the end of the patient's hospital stay, the patient's cousin finally arrives to the hospital for the first time after not being present for most of the patient's hospitalization. He asks about the patient's prognosis and potential future discharge date as he is the primary caretaker of the patient and needs to plan for his arrival home. The patient is doing well and can likely be discharged in the next few days. Which of the following is the most appropriate course of action?
- A. Bring the cousin to the room and explain the plan to both the patient and cousin
- B. Explain the plan to discharge the patient in the next few days
- C. Explain that you cannot discuss the patient's care at this time
- D. Tell the cousin that you do not know the patient's course well
- E. Bring the cousin to the room and ask the patient if it is acceptable to disclose his course (Correct Answer)
Security Rule requirements Explanation: ***Bring the cousin to the room and ask the patient if it is acceptable to disclose his course***
- This option prioritizes **patient autonomy** and privacy by allowing the patient to decide if their medical information can be shared with the cousin.
- Even if the cousin is the primary caretaker, explicit permission from the patient is required under **HIPAA** rules before disclosing protected health information.
- This approach balances **confidentiality protection** with practical discharge planning needs.
*Bring the cousin to the room and explain the plan to both the patient and cousin*
- This option prematurely assumes the patient's consent to share information with the cousin, which may violate **patient privacy**.
- While it facilitates communication, it bypasses the critical step of confirming the patient's willingness to disclose their medical details.
- This constitutes a **HIPAA violation** by disclosing information before obtaining consent.
*Explain the plan to discharge the patient in the next few days*
- Disclosing this information solely to the cousin without the patient's explicit permission constitutes a **breach of confidentiality**.
- This action violates **HIPAA regulations**, even if the cousin is identified as the primary caretaker.
- Protected health information (PHI) cannot be shared with family members without patient authorization.
*Explain that you cannot discuss the patient's care at this time*
- While protecting patient privacy, this response is overly abrupt and unhelpful, potentially creating **frustration** and hindering discharge planning.
- It does not offer a constructive path toward obtaining consent or addressing the cousin's legitimate concerns as a caretaker.
- A better approach involves facilitating consent rather than simply refusing communication.
*Tell the cousin that you do not know the patient's course well*
- This statement is **untruthful** and unprofessional, as the physician on rounds is expected to be knowledgeable about their patient's condition.
- It undermines trust and misrepresents the physician's duty to provide accurate information when appropriate.
- Dishonesty is never an acceptable approach to navigating privacy concerns.
Security Rule requirements US Medical PG Question 8: A 28-year-old male presents to his primary care physician with complaints of intermittent abdominal pain and alternating bouts of constipation and diarrhea. His medical chart is not significant for any past medical problems or prior surgeries. He is not prescribed any current medications. Which of the following questions would be the most useful next question in eliciting further history from this patient?
- A. "Does the diarrhea typically precede the constipation, or vice-versa?"
- B. "Is the diarrhea foul-smelling?"
- C. "Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life"
- D. "Are the symptoms worse in the morning or at night?"
- E. "Can you tell me more about the symptoms you have been experiencing?" (Correct Answer)
Security Rule requirements Explanation: ***Can you tell me more about the symptoms you have been experiencing?***
- This **open-ended question** encourages the patient to provide a **comprehensive narrative** of their symptoms, including details about onset, frequency, duration, alleviating/aggravating factors, and associated symptoms, which is crucial for diagnosis.
- In a patient presenting with vague, intermittent symptoms like alternating constipation and diarrhea, allowing them to elaborate freely can reveal important clues that might not be captured by more targeted questions.
*Does the diarrhea typically precede the constipation, or vice-versa?*
- While knowing the sequence of symptoms can be helpful in understanding the **pattern of bowel dysfunction**, it is a very specific question that might overlook other important aspects of the patient's experience.
- It prematurely narrows the focus without first obtaining a broad understanding of the patient's overall symptomatic picture.
*Is the diarrhea foul-smelling?*
- Foul-smelling diarrhea can indicate **malabsorption** or **bacterial overgrowth**, which are important to consider in some gastrointestinal conditions.
- However, this is a **specific symptom inquiry** that should follow a more general exploration of the patient's symptoms, as it may not be relevant if other crucial details are missed.
*Please rate your abdominal pain on a scale of 1-10, with 10 being the worst pain of your life*
- Quantifying pain intensity is useful for assessing the **severity of discomfort** and monitoring changes over time.
- However, for a patient with intermittent rather than acute, severe pain, understanding the **character, location, and triggers** of the pain is often more diagnostically valuable than just a numerical rating initially.
*Are the symptoms worse in the morning or at night?*
- Diurnal variation can be relevant in certain conditions, such as inflammatory bowel diseases where nocturnal symptoms might be more concerning, or functional disorders whose symptoms might be stress-related.
- This is another **specific question** that should come after gathering a more complete initial picture of the patient's symptoms to ensure no key information is overlooked.
Security Rule requirements US Medical PG Question 9: A 72-year-old woman is brought to the emergency department with dyspnea for 2 days. She is on regular hemodialysis at 3 sessions a week but missed her last session due to an unexpected trip. She has a history of congestive heart failure. After urgent hemodialysis, the patient’s dyspnea does not improve as expected. The cardiologist is consulted. After evaluation of the patient, he notes in the patient’s electronic record: “the patient does not have a chronic heart condition and a cardiac cause of dyspnea is unlikely.” The following morning, the nurse finds the cardiologist’s notes about the patient not having congestive heart failure odd. The patient had a clear history of congestive heart failure with an ejection fraction of 35%. After further investigation, the nurse realizes that the cardiologist evaluated the patient’s roommate. She is an elderly woman with a similar first name. She is also on chronic hemodialysis. To prevent similar future errors, the most appropriate strategy is to use which of the following?
- A. Two patient identifiers at every nurse-patient encounter
- B. A patient’s medical identification number at every encounter by any healthcare provider
- C. Two patient identifiers at every patient encounter by any healthcare provider (Correct Answer)
- D. Two patient identifiers at every physician-patient encounter
- E. A patient’s medical identification number at every physician-patient encounter
Security Rule requirements Explanation: ***Two patient identifiers at every patient encounter by any healthcare provider***
- This strategy ensures that **all healthcare providers**, not just nurses or physicians, verify the patient's identity using at least **two distinct identifiers** before any interaction, greatly reducing the risk of mix-ups.
- This comprehensive approach prevents errors like the one described, where a cardiologist evaluated the wrong patient due to similar names and circumstances, ensuring **patient safety** and appropriate care delivery.
*Two patient identifiers at every nurse-patient encounter*
- While important, limiting identification to nurse-patient encounters would **miss opportunities for error by other healthcare providers**, such as physicians, technicians, or pharmacists.
- The scenario explicitly states the error was made by a **cardiologist**, indicating that relying solely on nurses for identification is insufficient.
*A patient’s medical identification number at every encounter by any healthcare provider*
- Although the **medical identification number** is a valid identifier, relying on a *single* identifier still carries a risk, especially if typed or read incorrectly.
- **Two distinct identifiers** (e.g., name and date of birth, or name and medical record number) are the **gold standard** to minimize errors.
*Two patient identifiers at every physician-patient encounter*
- This option, while improving physician encounters, **fails to cover interactions with other crucial healthcare team members** (e.g., nurses, phlebotomists, imaging technicians) where patient misidentification can still occur.
- A comprehensive patient safety strategy must extend beyond physician interactions to **all points of care**.
*A patient’s medical identification number at every physician-patient encounter*
- This option combines the weaknesses of using only a **single identifier** and limiting the scope to **only physician encounters**, leaving multiple vulnerabilities for patient misidentification throughout the healthcare process.
- The **Joint Commission's National Patient Safety Goals** explicitly recommend using at least **two patient identifiers**.
Security Rule requirements US Medical PG Question 10: On a Sunday afternoon, a surgical oncologist and his family attend a football game in the city where he practices. While at the game, he runs into a physician colleague that works at the same institution. After some casual small talk, his colleague inquires, "Are you taking care of Mr. Clarke, my personal trainer? I heard through the grapevine that he has melanoma, and I didn't know if you have started him on any chemotherapy or performed any surgical intervention yet. Hopefully you'll be able to take very good care of him." In this situation, the surgical oncologist may confirm which of the following?
- A. The patient's name
- B. The patient's diagnosis
- C. The patient's treatment plan
- D. Only that Mr. Clarke is his patient
- E. No information at all (Correct Answer)
Security Rule requirements Explanation: *Incorrect: The patient's name*
- Confirming the patient's name would still be a breach of **confidentiality** under **HIPAA**, as it acknowledges the individual is a patient with the inquiring physician.
- Even if the name is already known to the colleague, confirming it from the treating physician implies an **established patient relationship**, which is PHI.
*Incorrect: The patient's diagnosis*
- Disclosing the patient's diagnosis is a direct violation of **HIPAA** rules, as it releases specific **protected health information** without the patient's explicit consent.
- This information is highly sensitive and directly related to the individual's health status, which must be kept confidential.
*Incorrect: The patient's treatment plan*
- Sharing details about the **treatment plan** is a clear breach of **patient privacy** and **HIPAA regulations**.
- This information is considered **protected health information (PHI)** and can only be shared with those directly involved in the patient's care or with patient consent.
*Incorrect: Only that Mr. Clarke is his patient*
- Even confirming that Mr. Clarke is a patient constitutes a breach of **confidentiality** and **HIPAA**.
- Acknowledging a patient-physician relationship is considered releasing **protected health information** because it implicitly confirms health services are being rendered to that individual.
***Correct: No information at all***
- Disclosure of any protected health information (PHI) to unauthorized individuals, even other healthcare professionals, is a violation of **HIPAA**.
- The colleague did not establish a **physician-patient relationship** with Mr. Clarke, nor did they have a legitimate need to know this information for treatment, payment, or healthcare operations.
- Without patient authorization or a legitimate purpose under the **Privacy Rule**, the surgical oncologist must not confirm any PHI, including the mere existence of a patient-physician relationship.
More Security Rule requirements US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.