Protected health information (PHI) US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Protected health information (PHI). These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Protected health information (PHI) US Medical PG Question 1: A 68-year-old man comes to the physician for a follow-up examination, accompanied by his daughter. Two years ago, he was diagnosed with localized prostate cancer, for which he underwent radiation therapy. He moved to the area 1 month ago to be closer to his daughter but continues to live independently. He was recently diagnosed with osteoblastic metastases to the spine and is scheduled to initiate therapy next week. In private, the patient’s daughter says that he has been losing weight and wetting the bed, and she tearfully asks the physician if his prostate cancer has returned. She says that her father has not spoken with her about his health recently. The patient has previously expressed to the physician that he does not want his family members to know about his condition because they “would worry too much.” Which of the following initial statements by the physician is most appropriate?
- A. “As your father's physician, I think that it's important that you know that his prostate cancer has returned. However, we are confident that he will respond well to treatment.”
- B. “I'm sorry, I can't discuss any information with you without his permission. I recommend that you have an open discussion with your father.” (Correct Answer)
- C. “It concerns me that he's not speaking openly with you. I recommend that you seek medical power of attorney for your father. Then, we can legally discuss his diagnosis and treatment options together.”
- D. “It’s difficult to deal with parents aging, but I have experience helping families cope. We should sit down with your father and discuss this situation together.”
- E. “Your father is very ill and may not want you to know the details. I can imagine it's frustrating for you, but you have to respect his discretion.”
Protected health information (PHI) Explanation: ***“I'm sorry, I can't discuss any information with you without his permission. I recommend that you have an open discussion with your father.”***
- This statement upholds **patient confidentiality** and **autonomy**, as the patient explicitly stated he did not want his family to know about his condition.
- It encourages communication between the patient and his daughter, which is the most appropriate way for her to learn about his health status.
*“As your father's physician, I think that it's important that you know that his prostate cancer has returned. However, we are confident that he will respond well to treatment.”*
- This violates the patient's **confidentiality** and explicit wish to keep his medical information private from his family.
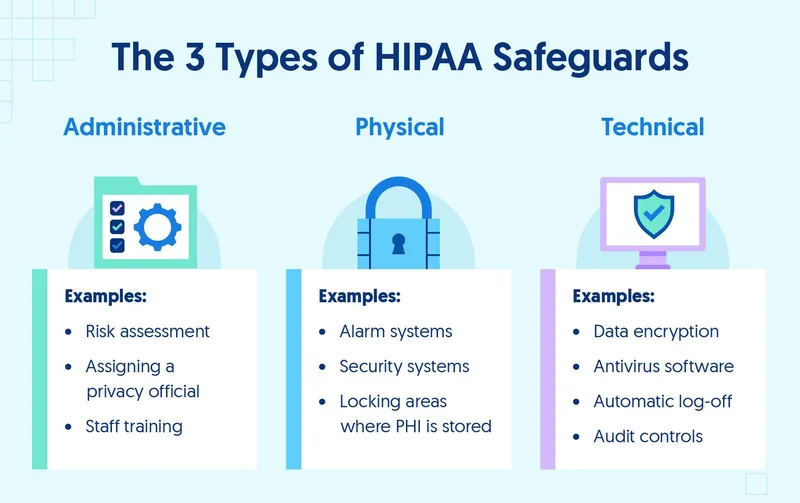
- Sharing medical information without explicit consent, even with family, is a breach of ethical and legal guidelines (e.g., **HIPAA** in the United States).
*“It concerns me that he's not speaking openly with you. I recommend that you seek medical power of attorney for your father. Then, we can legally discuss his diagnosis and treatment options together.”*
- While seeking medical power of attorney is an option for future decision-making, it is **premature and inappropriate** to suggest it solely to bypass the patient's current desire for confidentiality, especially when he is still competent to make his own decisions.
- This suggestion could undermine the patient's autonomy and trust in his physician.
*“It’s difficult to deal with parents aging, but I have experience helping families cope. We should sit down with your father and discuss this situation together.”*
- This statement, while empathetic, still risks undermining the patient's **autonomy** by pushing for a joint discussion against his explicit wishes to keep his family unaware.
- The physician's primary obligation is to the patient's stated preferences regarding his medical information.
*“Your father is very ill and may not want you to know the details. I can imagine it's frustrating for you, but you have to respect his discretion.”*
- While this statement acknowledges the daughter's feelings and respects the patient's discretion, it uses a somewhat **judgmental tone** ("very ill") and the phrasing "you have to respect his discretion" can come across as abrupt or dismissive rather than purely informative or guiding.
- The most appropriate initial response should focus on the **physician's inability to share information** due to confidentiality rather than attributing motives to the patient's decision or explicitly telling the daughter how to feel.
Protected health information (PHI) US Medical PG Question 2: A 42-year-old woman presents to the physician with symptoms of vague abdominal pain and bloating for several months. Test results indicate that she has ovarian cancer. Her physician attempts to reach her by phone multiple times but cannot reach her. Next of kin numbers are in her chart. According to HIPAA regulations, who should be the primary person the doctor discusses this information with?
- A. The patient's brother
- B. The patient's husband
- C. The patient's daughter
- D. All of the options
- E. The patient (Correct Answer)
Protected health information (PHI) Explanation: ***The patient***
- Under **HIPAA**, the patient has the **right to privacy** regarding their protected health information (PHI). Therefore, the physician must make all reasonable attempts to contact the patient directly to convey their diagnosis.
- Sharing sensitive medical information like a cancer diagnosis with anyone other than the patient, without their explicit consent, would be a **violation of HIPAA regulations**.
*The patient's brother*
- The patient's brother is not automatically authorized to receive her medical information, even if listed as **next of kin**, without the patient's explicit consent or a documented **healthcare power of attorney**.
- Discussing the diagnosis with the brother without the patient's direct consent would be a **breach of patient confidentiality**.
*The patient's husband*
- Even a spouse does not automatically have the right to access a patient's **PHI** without the patient's express permission, according to **HIPAA**.
- While often a trusted contact, without explicit consent, revealing the diagnosis to the husband would still violate the patient's **privacy rights**.
*The patient's daughter*
- Similar to other family members, the patient's daughter is not legally entitled to receive her mother's confidential medical information without explicit authorization or a medical **power of attorney**.
- The physician's primary responsibility is to the patient herself, ensuring her **privacy** is maintained.
*All of the options*
- According to **HIPAA**, sharing the patient's diagnosis with any family member without her explicit consent would be a **breach of confidentiality**.
- This option incorrectly assumes that **next of kin** automatically have the right to receive sensitive medical information.
Protected health information (PHI) US Medical PG Question 3: A 19-year-old man presents to an orthopedic surgeon to discuss repair of his torn anterior cruciate ligament. He suffered the injury during a college basketball game 1 week ago and has been using a knee immobilizer since the accident. His past medical history is significant for an emergency appendectomy when he was 12 years of age. At that time, he said that he never wanted to have surgery again. At this visit, the physician explains the procedure to him in detail including potential risks and complications. The patient acknowledges and communicates his understanding of both the diagnosis as well as the surgery and decides to proceed with the surgery in 3 weeks. Afterward, he signs a form giving consent for the operation. Which of the following statements is true about this patient?
- A. He cannot provide consent because he lacks capacity
- B. He has the right to revoke his consent at any time (Correct Answer)
- C. His parents also need to give consent to this operation
- D. He did not need to provide consent for this procedure since it is obviously beneficial
- E. His consent is invalid because his decision is not stable over time
Protected health information (PHI) Explanation: ***He has the right to revoke his consent at any time***
- **Informed consent** for medical procedures is an ongoing process, and a patient retains the right to **withdraw consent** at any point, even after initially signing the consent form.
- This right is a fundamental aspect of patient autonomy and ensures that medical interventions are only performed with a patient's current and willing agreement.
*He cannot provide consent because he lacks capacity*
- The patient is 19 years old, which in most jurisdictions (including the US where the age of majority is typically 18) means he is considered an **adult** and legally capable of providing his own consent.
- The scenario explicitly states he "communicates his understanding of both the diagnosis as well as the surgery," indicating he possesses the **mental capacity** to make an informed decision.
*His parents also need to give consent to this operation*
- As a 19-year-old, the patient has reached the **age of majority** and is legally entitled to make his own medical decisions, including consenting to surgery.
- Parental consent is generally required for minors (individuals under the age of majority), but not for adults like this patient.
*He did not need to provide consent for this procedure since it is obviously beneficial*
- Even for procedures that are clearly **beneficial**, informed consent is ethically and legally mandatory to uphold **patient autonomy** and ensure respect for individual rights.
- The concept of "obviously beneficial" does not negate the requirement for a patient's explicit agreement to a medical intervention.
*His consent is invalid because his decision is not stable over time*
- While the patient might have initially hated surgery at age 12, his current decision at age 19 to proceed with the ACL repair is based on current information and his mature understanding.
- The fact that his previous aversion to surgery has changed does not invalidate his current, well-informed decision; it simply indicates a change in perspective based on new circumstances and greater maturity.
Protected health information (PHI) US Medical PG Question 4: A psychiatrist receives a call from a patient who expresses thoughts of harming his ex-girlfriend. The patient describes a detailed plan to attack her at her workplace. Which of the following represents the psychiatrist's most appropriate legal obligation?
- A. Warn the ex-girlfriend and notify law enforcement (Correct Answer)
- B. Only notify the patient's family
- C. Warn only law enforcement
- D. Maintain patient confidentiality
Protected health information (PHI) Explanation: ***Warn the ex-girlfriend and notify law enforcement***
- This scenario directly triggers the **"duty to warn"** and **"duty to protect"** principles, primarily stemming from the **Tarasoff v. Regents of the University of California** case.
- The psychiatrist has a legal obligation to take reasonable steps to protect the identifiable victim, which includes directly warning the intended victim and informing law enforcement.
*Only notify the patient's family*
- Notifying the patient's family alone does not fulfill the **legal obligation to protect** an identifiable third party from a serious threat of harm.
- While family involvement might be part of a comprehensive safety plan, it is insufficient as the sole action in this critical situation.
*Warn only law enforcement*
- While notifying law enforcement is a crucial step, the **Tarasoff duty** specifically mandates warning the **intended victim** directly (or those who can reasonably be expected to notify the victim).
- Relying solely on law enforcement might not ensure the immediate safety of the ex-girlfriend, especially if there's a delay in their response or ability to locate her.
*Maintain patient confidentiality*
- Patient confidentiality is a cornerstone of psychiatric practice, but it is **not absolute** when there is a serious and imminent threat of harm to an identifiable individual.
- The **duty to protect** a potential victim *outweighs* the duty to maintain confidentiality in such extreme circumstances.
Protected health information (PHI) US Medical PG Question 5: A 72-year-old woman is brought to the emergency department with dyspnea for 2 days. She is on regular hemodialysis at 3 sessions a week but missed her last session due to an unexpected trip. She has a history of congestive heart failure. After urgent hemodialysis, the patient’s dyspnea does not improve as expected. The cardiologist is consulted. After evaluation of the patient, he notes in the patient’s electronic record: “the patient does not have a chronic heart condition and a cardiac cause of dyspnea is unlikely.” The following morning, the nurse finds the cardiologist’s notes about the patient not having congestive heart failure odd. The patient had a clear history of congestive heart failure with an ejection fraction of 35%. After further investigation, the nurse realizes that the cardiologist evaluated the patient’s roommate. She is an elderly woman with a similar first name. She is also on chronic hemodialysis. To prevent similar future errors, the most appropriate strategy is to use which of the following?
- A. Two patient identifiers at every nurse-patient encounter
- B. A patient’s medical identification number at every encounter by any healthcare provider
- C. Two patient identifiers at every patient encounter by any healthcare provider (Correct Answer)
- D. Two patient identifiers at every physician-patient encounter
- E. A patient’s medical identification number at every physician-patient encounter
Protected health information (PHI) Explanation: ***Two patient identifiers at every patient encounter by any healthcare provider***
- This strategy ensures that **all healthcare providers**, not just nurses or physicians, verify the patient's identity using at least **two distinct identifiers** before any interaction, greatly reducing the risk of mix-ups.
- This comprehensive approach prevents errors like the one described, where a cardiologist evaluated the wrong patient due to similar names and circumstances, ensuring **patient safety** and appropriate care delivery.
*Two patient identifiers at every nurse-patient encounter*
- While important, limiting identification to nurse-patient encounters would **miss opportunities for error by other healthcare providers**, such as physicians, technicians, or pharmacists.
- The scenario explicitly states the error was made by a **cardiologist**, indicating that relying solely on nurses for identification is insufficient.
*A patient’s medical identification number at every encounter by any healthcare provider*
- Although the **medical identification number** is a valid identifier, relying on a *single* identifier still carries a risk, especially if typed or read incorrectly.
- **Two distinct identifiers** (e.g., name and date of birth, or name and medical record number) are the **gold standard** to minimize errors.
*Two patient identifiers at every physician-patient encounter*
- This option, while improving physician encounters, **fails to cover interactions with other crucial healthcare team members** (e.g., nurses, phlebotomists, imaging technicians) where patient misidentification can still occur.
- A comprehensive patient safety strategy must extend beyond physician interactions to **all points of care**.
*A patient’s medical identification number at every physician-patient encounter*
- This option combines the weaknesses of using only a **single identifier** and limiting the scope to **only physician encounters**, leaving multiple vulnerabilities for patient misidentification throughout the healthcare process.
- The **Joint Commission's National Patient Safety Goals** explicitly recommend using at least **two patient identifiers**.
Protected health information (PHI) US Medical PG Question 6: An 86-year-old man is admitted to the hospital for management of pneumonia. His hospital course has been relatively uneventful, and he is progressing well. On morning rounds nearing the end of the patient's hospital stay, the patient's cousin finally arrives to the hospital for the first time after not being present for most of the patient's hospitalization. He asks about the patient's prognosis and potential future discharge date as he is the primary caretaker of the patient and needs to plan for his arrival home. The patient is doing well and can likely be discharged in the next few days. Which of the following is the most appropriate course of action?
- A. Bring the cousin to the room and explain the plan to both the patient and cousin
- B. Explain the plan to discharge the patient in the next few days
- C. Explain that you cannot discuss the patient's care at this time
- D. Tell the cousin that you do not know the patient's course well
- E. Bring the cousin to the room and ask the patient if it is acceptable to disclose his course (Correct Answer)
Protected health information (PHI) Explanation: ***Bring the cousin to the room and ask the patient if it is acceptable to disclose his course***
- This option prioritizes **patient autonomy** and privacy by allowing the patient to decide if their medical information can be shared with the cousin.
- Even if the cousin is the primary caretaker, explicit permission from the patient is required under **HIPAA** rules before disclosing protected health information.
- This approach balances **confidentiality protection** with practical discharge planning needs.
*Bring the cousin to the room and explain the plan to both the patient and cousin*
- This option prematurely assumes the patient's consent to share information with the cousin, which may violate **patient privacy**.
- While it facilitates communication, it bypasses the critical step of confirming the patient's willingness to disclose their medical details.
- This constitutes a **HIPAA violation** by disclosing information before obtaining consent.
*Explain the plan to discharge the patient in the next few days*
- Disclosing this information solely to the cousin without the patient's explicit permission constitutes a **breach of confidentiality**.
- This action violates **HIPAA regulations**, even if the cousin is identified as the primary caretaker.
- Protected health information (PHI) cannot be shared with family members without patient authorization.
*Explain that you cannot discuss the patient's care at this time*
- While protecting patient privacy, this response is overly abrupt and unhelpful, potentially creating **frustration** and hindering discharge planning.
- It does not offer a constructive path toward obtaining consent or addressing the cousin's legitimate concerns as a caretaker.
- A better approach involves facilitating consent rather than simply refusing communication.
*Tell the cousin that you do not know the patient's course well*
- This statement is **untruthful** and unprofessional, as the physician on rounds is expected to be knowledgeable about their patient's condition.
- It undermines trust and misrepresents the physician's duty to provide accurate information when appropriate.
- Dishonesty is never an acceptable approach to navigating privacy concerns.
Protected health information (PHI) US Medical PG Question 7: A 26-year-old man comes to the emergency department because of a 1-week history of fever, throat pain, and difficulty swallowing. Head and neck examination shows an erythematous pharynx with purulent exudates overlying the palatine tonsils. Microscopic examination of a throat culture shows pink, spherical bacteria arranged in chains. Treatment with amoxicillin is initiated. A day later, a physician colleague from another department approaches the physician in the lobby of the hospital and asks about this patient, saying, "Did you see him? What does he have? He's someone I play football with and he hasn't come to play for the past 5 days. I'm worried about him." Which of the following is the most appropriate action by the physician?
- A. Inform the colleague that they should ask the patient's attending physician
- B. Inform the colleague that they cannot divulge any information about the patient (Correct Answer)
- C. Tell the colleague the patient's case file number so they can look it up themselves
- D. Tell the colleague that they cannot tell them the diagnosis but that their friend was treated with antibiotics
- E. Ask the colleague to meet in the office so they can discuss the patient in private
Protected health information (PHI) Explanation: ***Inform the colleague that they cannot divulge any information about the patient***
- The **Health Insurance Portability and Accountability Act (HIPAA)** strictly prohibits the disclosure of a patient's **Protected Health Information (PHI)** without their explicit consent.
- Even if the inquirer knows the patient, a physician-patient relationship creates a **duty of confidentiality** that supersedes personal acquaintance.
- Disclosing any information without patient consent, even to another physician, violates HIPAA regulations.
*Tell the colleague the patient's case file number so they can look it up themselves*
- Providing the case file number would enable unauthorized access to the patient's medical records, thereby violating **patient confidentiality** and **HIPAA regulations**.
- This action does not rectify the breach of confidentiality and escalates the potential for further misuse of PHI.
*Inform the colleague that they should ask the patient's attending physician*
- Recommending that the colleague ask the attending physician shifts the burden but does not address the underlying ethical and legal obligation of the current physician to maintain **confidentiality**.
- The attending physician would also be bound by **HIPAA** and ethical guidelines not to disclose information without consent.
*Tell the colleague that they cannot tell them the diagnosis but that their friend was treated with antibiotics*
- While seemingly less specific, stating that the friend was treated with **antibiotics** is still a disclosure of **Protected Health Information (PHI)**.
- This action violates **patient confidentiality** as it reveals a detail of the patient's medical management without consent.
*Ask the colleague to meet in the office so they can discuss the patient in private*
- Moving to a private setting does not negate the fact that discussing the patient's information with an unauthorized individual is a **breach of confidentiality**.
- The location of the conversation does not change the ethical and legal obligations to protect **PHI**.
Protected health information (PHI) US Medical PG Question 8: A 36-year-old man comes to the physician because of a 2-week history of productive cough, weight loss, and intermittent fever. He recently returned from a 6-month medical deployment to Indonesia. He appears tired. Physical examination shows nontender, enlarged, palpable cervical lymph nodes. An x-ray of the chest shows right-sided hilar lymphadenopathy. A sputum smear shows acid-fast bacilli. A diagnosis of pulmonary tuberculosis is made from PCR testing of the sputum. The patient requests that the physician does not inform anyone of this diagnosis because he is worried about losing his job. Which of the following is the most appropriate initial action by the physician?
- A. Request the patient's permission to discuss the diagnosis with an infectious disease specialist
- B. Assure the patient that his diagnosis will remain confidential
- C. Confirm the diagnosis with a sputum culture
- D. Notify all of the patient's household contacts of the diagnosis
- E. Inform the local public health department of the diagnosis (Correct Answer)
Protected health information (PHI) Explanation: ***Inform the local public health department of the diagnosis***
- **Tuberculosis** is a **reportable disease** to public health authorities due to its significant public health implications, including the risk of transmission.
- Physicians have a **legal and ethical obligation** to report such diagnoses to protect the community, even against a patient's wishes for secrecy.
*Request the patient's permission to discuss the diagnosis with an infectious disease specialist*
- While consulting an infectious disease specialist is often beneficial for managing TB, the immediate and most appropriate initial action is related to **public health notification**.
- Delaying notification to seek patient permission first would **compromise public health safety** regarding a reportable disease.
*Assure the patient that his diagnosis will remain confidential*
- This assurance would be **misleading and unethical** because TB is a reportable condition, meaning its confidentiality is necessarily breached for public health purposes.
- Physicians are bound by law to report communicable diseases, which supersedes general confidentiality in this specific context.
*Confirm the diagnosis with a sputum culture*
- The diagnosis of pulmonary tuberculosis has already been established by a **sputum smear showing acid-fast bacilli** and **PCR testing**, which are highly reliable.
- While a sputum culture provides drug susceptibility information, it is not the *initial* most appropriate action regarding the patient's stated concerns about confidentiality in the context of a reportable disease.
*Notify all of the patient's household contacts of the diagnosis*
- While contact tracing is an important part of TB control, it is typically initiated and managed by the **public health department** after notification.
- The physician's primary responsibility is to notify the health department, who then assumes the role of **contact investigation** and management.
Protected health information (PHI) US Medical PG Question 9: On a Sunday afternoon, a surgical oncologist and his family attend a football game in the city where he practices. While at the game, he runs into a physician colleague that works at the same institution. After some casual small talk, his colleague inquires, "Are you taking care of Mr. Clarke, my personal trainer? I heard through the grapevine that he has melanoma, and I didn't know if you have started him on any chemotherapy or performed any surgical intervention yet. Hopefully you'll be able to take very good care of him." In this situation, the surgical oncologist may confirm which of the following?
- A. The patient's name
- B. The patient's diagnosis
- C. The patient's treatment plan
- D. Only that Mr. Clarke is his patient
- E. No information at all (Correct Answer)
Protected health information (PHI) Explanation: *Incorrect: The patient's name*
- Confirming the patient's name would still be a breach of **confidentiality** under **HIPAA**, as it acknowledges the individual is a patient with the inquiring physician.
- Even if the name is already known to the colleague, confirming it from the treating physician implies an **established patient relationship**, which is PHI.
*Incorrect: The patient's diagnosis*
- Disclosing the patient's diagnosis is a direct violation of **HIPAA** rules, as it releases specific **protected health information** without the patient's explicit consent.
- This information is highly sensitive and directly related to the individual's health status, which must be kept confidential.
*Incorrect: The patient's treatment plan*
- Sharing details about the **treatment plan** is a clear breach of **patient privacy** and **HIPAA regulations**.
- This information is considered **protected health information (PHI)** and can only be shared with those directly involved in the patient's care or with patient consent.
*Incorrect: Only that Mr. Clarke is his patient*
- Even confirming that Mr. Clarke is a patient constitutes a breach of **confidentiality** and **HIPAA**.
- Acknowledging a patient-physician relationship is considered releasing **protected health information** because it implicitly confirms health services are being rendered to that individual.
***Correct: No information at all***
- Disclosure of any protected health information (PHI) to unauthorized individuals, even other healthcare professionals, is a violation of **HIPAA**.
- The colleague did not establish a **physician-patient relationship** with Mr. Clarke, nor did they have a legitimate need to know this information for treatment, payment, or healthcare operations.
- Without patient authorization or a legitimate purpose under the **Privacy Rule**, the surgical oncologist must not confirm any PHI, including the mere existence of a patient-physician relationship.
Protected health information (PHI) US Medical PG Question 10: A 17-year-old male, accompanied by his uncle, presents to a doctor with his arm in a sling. There is blood dripping down his shirt. He pleads with the physician to not report this injury to authorities, offering to pay extra for his visit, as he is afraid of retaliation from his rival gang. The physician examines the wound, which appears to be a stabbing injury to his left anterior deltoid. This case study in medical ethics asks: How should the physician best handle this patient's request?
- A. Maintain confidentiality, as reporting stab wounds is not required
- B. Breach confidentiality and discuss the injury with the uncle
- C. Breach confidentiality and report the stab wound to the police (Correct Answer)
- D. Maintain confidentiality and schedule a follow-up visit with the patient
- E. Maintain confidentiality, as retaliation may result in greater harm to the patient
Protected health information (PHI) Explanation: ***Breach confidentiality and report the stab wound to the police***
- Physicians in the United States have a **mandatory reporting obligation** for injuries resulting from violent crimes, including stab wounds, regardless of the patient's wishes.
- **State laws** require reporting of suspected criminal activity involving weapons, and physicians are **legally protected** from liability when making good-faith mandatory reports.
- While the principle of **non-maleficence** is important, **legal duties** take precedence, and physicians cannot selectively choose when to comply with mandatory reporting laws based on patient circumstances.
- The physician should explain to the patient that reporting is required by law, provide compassionate care, and potentially connect the patient with **social services** or **law enforcement victim support** to address safety concerns.
*Maintain confidentiality, as retaliation may result in greater harm to the patient*
- While concern for patient safety is understandable, **mandatory reporting laws do not have exceptions** for fear of retaliation.
- Physicians who fail to report may face **professional discipline**, **civil liability**, and potentially **criminal penalties** depending on jurisdiction.
- The proper approach is to report as required while simultaneously working to ensure patient safety through appropriate **social work intervention** and **victim protection resources**.
*Maintain confidentiality and schedule a follow-up visit with the patient*
- Simply scheduling follow-up care while failing to report violates **mandatory reporting statutes** for violent injuries.
- This approach ignores the physician's **legal obligation** and could result in professional consequences.
- Follow-up care should be provided **in addition to**, not instead of, mandatory reporting.
*Maintain confidentiality, as reporting stab wounds is not required*
- This is **factually incorrect**; virtually all U.S. jurisdictions require reporting of injuries from violent crimes, particularly those involving weapons.
- Failure to report based on this misunderstanding could lead to **licensure sanctions** and legal liability.
*Breach confidentiality and discuss the injury with the uncle*
- The 17-year-old patient is a **minor**, but discussing details with the uncle without explicit consent or confirmed guardianship status is inappropriate.
- The uncle's presence does not automatically grant him **HIPAA authorization** to receive protected health information.
- The correct action is to report to **appropriate authorities** (police), not to involve family members without proper consent or legal authority.
More Protected health information (PHI) US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.