Authorization requirements US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Authorization requirements. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Authorization requirements US Medical PG Question 1: An 83-year-old man presents to the gastroenterologist to follow-up on results from a biopsy of a pancreatic head mass, which the clinician was concerned could be pancreatic cancer. After welcoming the patient and his wife to the clinic, the physician begins to discuss the testing and leads into delivering the results, which showed metastatic pancreatic adenocarcinoma. Before she is able to disclose these findings, the patient stops her and exclaims, "Whatever it is, I don't want to know. Please just make me comfortable in my last months alive. I have made up my mind about this." Which of the following is the most appropriate response on the part of the physician?
- A. "If that is your definite wish, then I must honor it" (Correct Answer)
- B. "The cancer has spread to your liver"
- C. "As a physician, I am obligated to disclose these results to you"
- D. "If you don't know what condition you have, I will be unable to be your physician going forward"
- E. "Please, sir, I strongly urge you to reconsider your decision"
Authorization requirements Explanation: ***"If that is your definite wish, then I must honor it"***
- This response respects the patient's **autonomy** and right to refuse information, aligning with ethical principles of patient-centered care.
- The patient has clearly and articulately stated his desire not to know and wishes for **palliative care**, which the physician should respect.
- The patient appears to have **decision-making capacity** based on his clear communication of wishes.
*"The cancer has spread to your liver"*
- This statement violates the patient's explicit request not to be informed of his diagnosis, potentially causing distress and undermining trust.
- Disclosure of information against a patient's wishes is unethical when the patient has **decision-making capacity** and has clearly refused information.
*"As a physician, I am obligated to disclose these results to you"*
- While physicians have a general duty to inform, this is superseded by a **competent patient's right to refuse information**.
- No absolute obligation exists to force information upon a patient who explicitly states a desire not to know, especially when it concerns their own health information.
*"If you don't know what condition you have, I will be unable to be your physician going forward"*
- This response is coercive and threatening, attempting to strong-arm the patient into accepting information he has refused.
- A physician's role includes managing symptoms and providing comfort, even if the patient chooses not to know the full diagnostic details of their condition, particularly in a **palliative care** context.
- This statement could constitute **patient abandonment**, which is unethical.
*"Please, sir, I strongly urge you to reconsider your decision"*
- While it's acceptable to ensure the patient fully understands the implications of their decision, a forceful "urge to reconsider" after a clear refusal can be seen as undermining their **autonomy**.
- The physician should confirm the patient's understanding and offer an opportunity to discuss it later if desired, rather than immediately pressuring them.
Authorization requirements US Medical PG Question 2: A psychiatrist receives a call from a patient who expresses thoughts of harming his ex-girlfriend. The patient describes a detailed plan to attack her at her workplace. Which of the following represents the psychiatrist's most appropriate legal obligation?
- A. Warn the ex-girlfriend and notify law enforcement (Correct Answer)
- B. Only notify the patient's family
- C. Warn only law enforcement
- D. Maintain patient confidentiality
Authorization requirements Explanation: ***Warn the ex-girlfriend and notify law enforcement***
- This scenario directly triggers the **"duty to warn"** and **"duty to protect"** principles, primarily stemming from the **Tarasoff v. Regents of the University of California** case.
- The psychiatrist has a legal obligation to take reasonable steps to protect the identifiable victim, which includes directly warning the intended victim and informing law enforcement.
*Only notify the patient's family*
- Notifying the patient's family alone does not fulfill the **legal obligation to protect** an identifiable third party from a serious threat of harm.
- While family involvement might be part of a comprehensive safety plan, it is insufficient as the sole action in this critical situation.
*Warn only law enforcement*
- While notifying law enforcement is a crucial step, the **Tarasoff duty** specifically mandates warning the **intended victim** directly (or those who can reasonably be expected to notify the victim).
- Relying solely on law enforcement might not ensure the immediate safety of the ex-girlfriend, especially if there's a delay in their response or ability to locate her.
*Maintain patient confidentiality*
- Patient confidentiality is a cornerstone of psychiatric practice, but it is **not absolute** when there is a serious and imminent threat of harm to an identifiable individual.
- The **duty to protect** a potential victim *outweighs* the duty to maintain confidentiality in such extreme circumstances.
Authorization requirements US Medical PG Question 3: A healthy, 16-year-old girl is brought in by her mother for a wellness visit. During the appointment, the patient’s mother brings up concerns about her daughter’s acne. The patient has had acne for 2 years. She washes her face twice a day with benzoyl peroxide and has been on doxycycline for 2 months with only mild improvement. The patient does not feel that the acne is related to her menstrual cycles. The patient’s mother states she does well in school and is the captain of the junior varsity cross-country team. She is worried that the acne is starting to affect her daughter’s self-esteem. The patient states that prom is coming up, and she is considering not going because she hates taking pictures. Upon physical exam, there are multiple open and closed comedones and scattered, red nodules on the patient’s face with evidence of scarring. The patient’s mother says her neighbor’s son tried isotretinoin and wants to know if that may work for her daughter. While talking about the risk factors for isotretinoin, you mention that patient will need to be on 2 forms of birth control. The mother asks, “Is that really necessary? We are a very religious family and my daughter knows our household rule about no sex before marriage.” Which of the following is the next step in management?
- A. Have the patient take a pregnancy test to prove abstinence
- B. Ask the mother to leave the room before talking to the patient about her sexual activity (Correct Answer)
- C. Talk to patient and mother about patient’s sexual activity, since parental permission is needed for isotretinoin
- D. Prescribe the isotretinoin as the patient does not need additional contraception if she is abstinent
- E. Prescribe the isotretinoin after giving the patient a handout about birth control methods
Authorization requirements Explanation: ***Ask the mother to leave the room before talking to the patient about her sexual activity***
- This respects the **adolescent's right to confidentiality** and allows for a candid discussion about sensitive topics like sexual activity and contraception
- A **16-year-old** has the right to private discussions about reproductive health matters, regardless of parental presence
- The **iPLEDGE program** requires comprehensive counseling about contraception for all females of childbearing potential, which is best accomplished in a private setting
- This approach balances the need to respect parental involvement while protecting the minor's confidentiality on sensitive health matters
*Have the patient take a pregnancy test to prove abstinence*
- While a pregnancy test is necessary before starting isotretinoin, it does not confirm or prove abstinence
- This is not the appropriate first step in addressing the mother's concerns or the patient's need for contraception counseling
- iPLEDGE guidelines require monthly negative pregnancy tests but also mandate contraception counseling regardless of pregnancy test results
*Talk to patient and mother about patient's sexual activity, since parental permission is needed for isotretinoin*
- Discussing sexual activity with both the patient and mother present **violates adolescent confidentiality** and may prevent honest disclosure
- Many states allow **mature minors** to consent to contraceptive services without parental involvement
- This approach could damage the therapeutic relationship and compromise the patient's willingness to share sensitive information
*Prescribe the isotretinoin as the patient does not need additional contraception if she is abstinent*
- This is incorrect as the **FDA-mandated iPLEDGE program** requires all females of childbearing potential to use two forms of contraception, regardless of stated abstinence
- The program makes no exception for patients claiming abstinence due to the **extreme teratogenicity** of isotretinoin
- Bypassing this requirement would violate federal regulations and expose the patient to risk of severe congenital malformations if pregnancy occurs
*Prescribe the isotretinoin after giving the patient a handout about birth control methods*
- Simply providing a handout is insufficient for effective contraception counseling required by the **iPLEDGE program**
- The patient needs detailed, private counseling to understand contraceptive options, the risks of isotretinoin, and to ensure adherence
- This approach fails to address the confidentiality issue raised by the mother's presence
Authorization requirements US Medical PG Question 4: A 73-year-old man is brought to the emergency department by ambulance after being found to be non-communicative by his family during dinner. On presentation he appears to be alert, though he is confused and cannot follow instructions. When he tries to speak, he vocalizes a string of fluent but unintelligible syllables. Given this presentation, his physician decides to administer tissue plasminogen activator to this patient. This intervention best represents which of the following principles?
- A. Tertiary prevention
- B. Primary prevention
- C. This does not represent prevention (Correct Answer)
- D. Quaternary prevention
- E. Secondary prevention
Authorization requirements Explanation: ***This does not represent prevention***
- The administration of **tissue plasminogen activator (tPA)** during an **acute stroke** is a **therapeutic intervention**, not a form of prevention.
- **Prevention** refers to actions taken to prevent disease occurrence, detect it early, or prevent complications after recovery. Treating an acute, symptomatic event is **acute treatment**, not prevention.
- This is an active medical intervention to treat an ongoing, symptomatic disease process (acute ischemic stroke), which falls under **therapeutic management** rather than any category of prevention.
*Secondary prevention*
- **Secondary prevention** involves **early detection** and treatment of asymptomatic or minimally symptomatic disease to prevent progression (e.g., screening mammography, colonoscopy).
- For stroke specifically, secondary prevention would include interventions **after** the acute event to **prevent recurrence**, such as starting antiplatelet therapy (aspirin, clopidogrel), anticoagulation for atrial fibrillation, statin therapy, or carotid endarterectomy after TIA.
- tPA is given during the acute symptomatic phase, making it treatment rather than secondary prevention.
*Tertiary prevention*
- **Tertiary prevention** focuses on **rehabilitation** and managing established disease to prevent complications and improve quality of life.
- Examples after stroke include physical therapy, occupational therapy, speech therapy, and managing post-stroke complications like depression or spasticity.
- This occurs in the recovery phase, not during acute treatment.
*Primary prevention*
- **Primary prevention** aims to prevent disease before it occurs in healthy individuals.
- Examples include controlling hypertension, managing diabetes, smoking cessation, exercise, and healthy diet - all interventions that reduce stroke risk **before** any event occurs.
*Quaternary prevention*
- **Quaternary prevention** protects patients from **overmedicalization** and excessive or harmful medical interventions.
- It involves avoiding unnecessary testing or treatment that may cause more harm than benefit.
- Administering tPA for acute stroke (when indicated) is evidence-based treatment, not overtreatment.
Authorization requirements US Medical PG Question 5: A 26-year-old man comes to the emergency department because of a 1-week history of fever, throat pain, and difficulty swallowing. Head and neck examination shows an erythematous pharynx with purulent exudates overlying the palatine tonsils. Microscopic examination of a throat culture shows pink, spherical bacteria arranged in chains. Treatment with amoxicillin is initiated. A day later, a physician colleague from another department approaches the physician in the lobby of the hospital and asks about this patient, saying, "Did you see him? What does he have? He's someone I play football with and he hasn't come to play for the past 5 days. I'm worried about him." Which of the following is the most appropriate action by the physician?
- A. Inform the colleague that they should ask the patient's attending physician
- B. Inform the colleague that they cannot divulge any information about the patient (Correct Answer)
- C. Tell the colleague the patient's case file number so they can look it up themselves
- D. Tell the colleague that they cannot tell them the diagnosis but that their friend was treated with antibiotics
- E. Ask the colleague to meet in the office so they can discuss the patient in private
Authorization requirements Explanation: ***Inform the colleague that they cannot divulge any information about the patient***
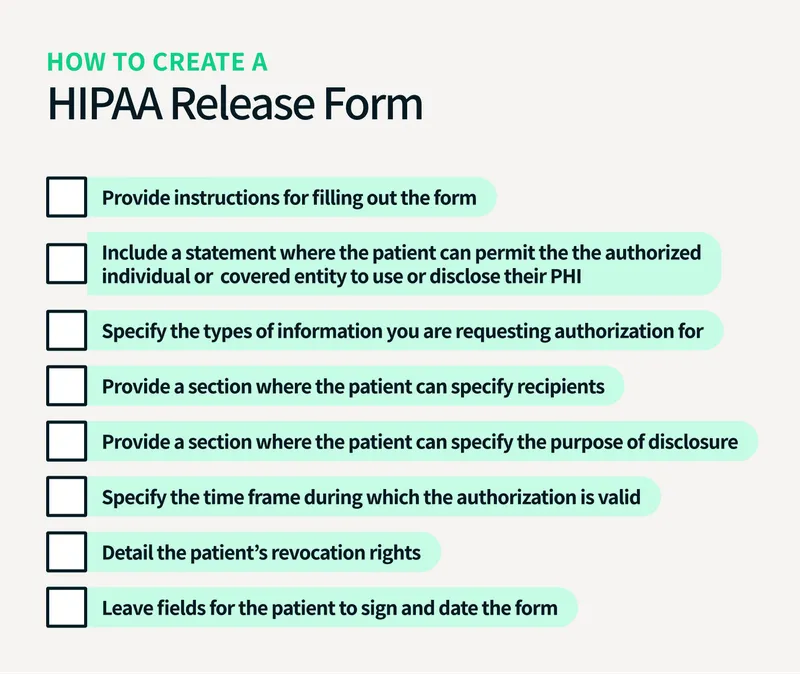
- The **Health Insurance Portability and Accountability Act (HIPAA)** strictly prohibits the disclosure of a patient's **Protected Health Information (PHI)** without their explicit consent.
- Even if the inquirer knows the patient, a physician-patient relationship creates a **duty of confidentiality** that supersedes personal acquaintance.
- Disclosing any information without patient consent, even to another physician, violates HIPAA regulations.
*Tell the colleague the patient's case file number so they can look it up themselves*
- Providing the case file number would enable unauthorized access to the patient's medical records, thereby violating **patient confidentiality** and **HIPAA regulations**.
- This action does not rectify the breach of confidentiality and escalates the potential for further misuse of PHI.
*Inform the colleague that they should ask the patient's attending physician*
- Recommending that the colleague ask the attending physician shifts the burden but does not address the underlying ethical and legal obligation of the current physician to maintain **confidentiality**.
- The attending physician would also be bound by **HIPAA** and ethical guidelines not to disclose information without consent.
*Tell the colleague that they cannot tell them the diagnosis but that their friend was treated with antibiotics*
- While seemingly less specific, stating that the friend was treated with **antibiotics** is still a disclosure of **Protected Health Information (PHI)**.
- This action violates **patient confidentiality** as it reveals a detail of the patient's medical management without consent.
*Ask the colleague to meet in the office so they can discuss the patient in private*
- Moving to a private setting does not negate the fact that discussing the patient's information with an unauthorized individual is a **breach of confidentiality**.
- The location of the conversation does not change the ethical and legal obligations to protect **PHI**.
Authorization requirements US Medical PG Question 6: A 36-year-old man comes to the physician because of a 2-week history of productive cough, weight loss, and intermittent fever. He recently returned from a 6-month medical deployment to Indonesia. He appears tired. Physical examination shows nontender, enlarged, palpable cervical lymph nodes. An x-ray of the chest shows right-sided hilar lymphadenopathy. A sputum smear shows acid-fast bacilli. A diagnosis of pulmonary tuberculosis is made from PCR testing of the sputum. The patient requests that the physician does not inform anyone of this diagnosis because he is worried about losing his job. Which of the following is the most appropriate initial action by the physician?
- A. Request the patient's permission to discuss the diagnosis with an infectious disease specialist
- B. Assure the patient that his diagnosis will remain confidential
- C. Confirm the diagnosis with a sputum culture
- D. Notify all of the patient's household contacts of the diagnosis
- E. Inform the local public health department of the diagnosis (Correct Answer)
Authorization requirements Explanation: ***Inform the local public health department of the diagnosis***
- **Tuberculosis** is a **reportable disease** to public health authorities due to its significant public health implications, including the risk of transmission.
- Physicians have a **legal and ethical obligation** to report such diagnoses to protect the community, even against a patient's wishes for secrecy.
*Request the patient's permission to discuss the diagnosis with an infectious disease specialist*
- While consulting an infectious disease specialist is often beneficial for managing TB, the immediate and most appropriate initial action is related to **public health notification**.
- Delaying notification to seek patient permission first would **compromise public health safety** regarding a reportable disease.
*Assure the patient that his diagnosis will remain confidential*
- This assurance would be **misleading and unethical** because TB is a reportable condition, meaning its confidentiality is necessarily breached for public health purposes.
- Physicians are bound by law to report communicable diseases, which supersedes general confidentiality in this specific context.
*Confirm the diagnosis with a sputum culture*
- The diagnosis of pulmonary tuberculosis has already been established by a **sputum smear showing acid-fast bacilli** and **PCR testing**, which are highly reliable.
- While a sputum culture provides drug susceptibility information, it is not the *initial* most appropriate action regarding the patient's stated concerns about confidentiality in the context of a reportable disease.
*Notify all of the patient's household contacts of the diagnosis*
- While contact tracing is an important part of TB control, it is typically initiated and managed by the **public health department** after notification.
- The physician's primary responsibility is to notify the health department, who then assumes the role of **contact investigation** and management.
Authorization requirements US Medical PG Question 7: An 86-year-old male is admitted to the hospital under your care for management of pneumonia. His hospital course has been relatively uneventful, and he is progressing well. While making morning rounds on your patients, the patient's cousin approaches you in the hallway and asks about the patient's prognosis and potential future discharge date. The patient does not have an advanced directive on file and does not have a medical power of attorney. Which of the following is the best course of action?
- A. Direct the cousin to the patient's room, telling him that you will be by within the hour to discuss the plan.
- B. Explain that you cannot discuss the patient's care without explicit permission from the patient themselves. (Correct Answer)
- C. Provide the cousin with the patient's most recent progress notes and a draft of his discharge summary.
- D. Explain that the patient is progressing well and should be discharged within the next few days.
- E. Refer the cousin to ask the patient's wife about these topics.
Authorization requirements Explanation: ***Explain that you cannot discuss the patient's care without explicit permission from the patient themselves.***
- This is the **correct ethical and legal action** in healthcare to maintain patient confidentiality, as the patient has not designated a medical power of attorney or filed an advance directive.
- The **Health Insurance Portability and Accountability Act (HIPAA)** protects patient health information, requiring explicit patient consent before disclosure to anyone, including family members, unless specific exceptions apply (e.g., immediate threat to safety, treatment purposes directly).
*Direct the cousin to the patient's room, telling him that you will be by within the hour to discuss the plan.*
- While ultimately the patient needs to be involved, directly discussing **private health information** with the cousin without the patient's consent first is a breach of **confidentiality**.
- This approach prematurely assumes the patient will grant permission or wishes for this specific family member to be involved, which might not be true.
*Provide the cousin with the patient's most recent progress notes and a draft of his discharge summary.*
- This action represents a clear and significant **breach of patient confidentiality** and **HIPAA regulations**.
- Without explicit patient consent, sharing detailed medical records with anyone, including family, is strictly prohibited.
*Explain that the patient is progressing well and should be discharged within the next few days.*
- Even a general statement about the patient's condition and discharge plans can be considered a **breach of confidentiality** under HIPAA.
- Such information, while seemingly innocuous, reveals that the individual is indeed a patient and implies details about their health status, which requires patient consent to disclose.
*Refer the cousin to ask the patient's wife about these topics.*
- There is no information provided that the **patient's wife** has legal authority (e.g., **medical power of attorney**) or explicit permission from the patient to discuss his medical information.
- Referring the cousin to the wife without verifying her authority could lead to further breaches of **confidentiality** if the wife is not authorized to share such details.
Authorization requirements US Medical PG Question 8: A 78-year-old woman is brought to the emergency ward by her son for lethargy and generalized weakness. The patient speaks in short utterances and does not make eye contact with the provider or her son throughout the interview and examination. You elicit that the patient lives with her son and daughter-in-law, and she reports vague weakness for the last couple days. The emergency room provider notices 3-4 healing bruises on the patient's upper extremities; otherwise, examination is not revealing. Routine chemistries and blood counts are unremarkable; non-contrast head CT demonstrates normal age-related changes. Which of the following is the most appropriate next step in management?
- A. Ask the patient's son to leave the room (Correct Answer)
- B. Question the patient's son regarding the home situation
- C. Call Adult Protective Services to report the patient's son
- D. Perform lumbar puncture
- E. Question the patient regarding abuse or neglect
Authorization requirements Explanation: ***Ask the patient's son to leave the room***
- The patient's **lethargy**, **non-engagement**, and **healing bruises** raise strong suspicions for elder abuse or neglect. Removing the son allows for a private interview, which is crucial for her to feel safe enough to disclose information.
- In situations of suspected abuse, it is paramount to prioritize the **patient's safety and ability to speak freely** without the presence of the suspected abuser.
*Question the patient's son regarding the home situation*
- Questioning the son directly at this point may escalate the situation or make the patient even less likely to disclose abuse, as she is likely **frightened or coerced**.
- This step is premature and should only occur after a private interview with the patient, and potentially with the involvement of Protective Services.
*Call Adult Protective Services to report the patient's son*
- While reporting to **Adult Protective Services** is a critical step if abuse is confirmed, it is not the immediate first action until a private interview with the patient has been conducted to gather more information.
- Making a report without attempting to speak with the patient alone first can hinder the investigation and potentially jeopardize her safety if the abuser is alerted prematurely.
*Perform lumbar puncture*
- A lumbar puncture is an invasive procedure generally performed to diagnose **central nervous system infections** or **inflammatory conditions**.
- There are no clinical indications (e.g., fever, meningeal signs, focal neurological deficits) to suggest a need for a lumbar puncture, especially given the history and physical findings that point towards abuse.
*Question the patient regarding abuse or neglect*
- While it's important to question the patient about abuse, it must be done in a **safe and private environment** where she feels comfortable speaking freely.
- Questioning her while the suspected abuser (her son) is present would likely yield unhelpful responses due to fear or intimidation, as seen by her lack of eye contact and short utterances.
Authorization requirements US Medical PG Question 9: An 11-month-old girl presents to a pediatrician with her mother who is concerned about a red discoloration with a rectangular shape over the child’s left buttock presenting since the previous night. The mother also mentions that her daughter has been crying excessively. There is no history of decreased breast feeding, fever, joint swelling, vomiting, decreased urine output, or change in color of urine or stools. The mother denies any history of injury. However, she mentions that the infant had suffered from a self-limiting upper respiratory infection three weeks before. There is no history of bruising or bleeding in the past. The mother informs the doctor that she has a brother (the patient’s maternal uncle) with hemophilia A. On physical examination, the girl’s temperature is 37.0°C (98.6°F), pulse rate is 160/min, and respiratory rate is 38/min. The lesion presents over the left buttock and is tender on palpation. What is the most likely diagnosis?
- A. Erythema multiforme minor
- B. Hemophilia
- C. Idiopathic thrombocytopenic purpura
- D. Diaper dermatitis
- E. Abusive bruise (Correct Answer)
Authorization requirements Explanation: ***Abusive bruise***
- The **rectangular shape** of the bruise is a **patterned injury**, highly suggestive of non-accidental trauma (child abuse). Patterned bruises reflect the shape of an object used to inflict injury (e.g., belt, hand, ruler).
- **Location on the buttock** is a common site for abusive injuries, as opposed to accidental bruises which typically occur over bony prominences (shins, knees, forehead).
- **Age of the child** (11 months, pre-ambulatory) makes accidental bruising less likely. Non-mobile infants rarely sustain bruises accidentally.
- **Excessive crying** and **tenderness on palpation** are consistent with recent trauma.
- **Mother's denial of injury** does not rule out abuse by another caregiver.
- This is a **critical patient safety issue** requiring mandatory reporting to child protective services and further investigation.
*Hemophilia*
- While the family history of hemophilia A in a maternal uncle raises the possibility of the child being a carrier, **females with hemophilia A are extremely rare** (requiring extreme lyonization, Turner syndrome, or homozygous state).
- The child has **no prior history of bleeding or bruising**, which would be expected if hemophilia were severe enough to cause spontaneous bruising.
- The **specific rectangular pattern** of this bruise is not consistent with spontaneous bleeding from a coagulopathy, which typically causes diffuse ecchymoses.
- If concerned, coagulation studies (PT, aPTT, factor VIII levels) could be obtained, but the patterned nature of the injury points to trauma.
*Idiopathic thrombocytopenic purpura*
- ITP typically presents with **petechiae and widespread purpura**, not a single discrete rectangular bruise.
- While the recent URI could trigger ITP, the **pattern and location** of this lesion are inconsistent with thrombocytopenic bleeding.
- ITP-related bleeding would not be tender on palpation and would not present in a rectangular shape.
*Erythema multiforme minor*
- Characterized by **target lesions** with concentric rings, typically on extremities and mucous membranes.
- The described lesion is a **tender, rectangular bruise**, not an erythematous target lesion.
- Erythema multiforme is not tender to palpation in the same way as traumatic bruising.
*Diaper dermatitis*
- Presents as **diffuse erythema and irritation** in areas of contact with urine and feces.
- The lesion described is a **discrete, rectangular, tender bruise**, completely inconsistent with the appearance of diaper rash.
- Diaper dermatitis is not typically described as having a specific geometric shape.
Authorization requirements US Medical PG Question 10: A 3-month-old boy is brought to the emergency department by his mom for breathing difficulty after a recent fall. His parents say that he rolled off of the mattress and landed on the hard wood floor earlier today. After an extensive physical exam, he is found to have many purplish bruises and retinal hemorrhages. A non-contrast head CT scan shows a subdural hemorrhage. He was treated in the hospital with full recovery from his symptoms. Which of the following is the most important follow up plan?
- A. Provide parents with anticipatory guidance
- B. Referral to genetics for further testing
- C. Reassurance that accidents are common
- D. Inform child protective services (Correct Answer)
- E. Provide home nursing visits
Authorization requirements Explanation: ***Inform child protective services***
- The combination of **multiple purplish bruises**, **retinal hemorrhages**, and **subdural hemorrhage** in a 3-month-old infant after a minor fall (rolling off a mattress) is highly suggestive of **abusive head trauma** (shaken baby syndrome).
- Healthcare professionals have a **legal and ethical obligation** to report suspected child abuse to Child Protective Services (CPS) to ensure the child's safety and initiate an investigation.
*Provide parents with anticipatory guidance*
- While anticipatory guidance on child safety and development is generally important, it is **insufficient and inappropriate** as the primary follow-up in a case of suspected child abuse.
- Focusing solely on guidance would **neglect the immediate safety concerns** and the need for investigation into the injuries.
*Referral to genetics for further testing*
- While some genetic conditions can predispose to easy bruising or bleeding, the specific pattern of injuries (**retinal hemorrhages, subdural hemorrhage, multiple bruises, and a history inconsistent with the severity of injuries**) overwhelmingly points to trauma, not a genetic disorder.
- Genetic testing would be a secondary consideration, if at all, after abuse has been ruled out or addressed.
*Reassurance that accidents are common*
- Reassuring parents that "accidents are common" would be **medically negligent and dangerous** in this scenario, as the injuries sustained are typically not caused by a simple fall from a mattress in an infant of this age.
- This response would dismiss critical signs of potential abuse and leave the child at risk.
*Provide home nursing visits*
- Home nursing visits might be beneficial for monitoring general health and development, but they do **not address the immediate and grave concern** of potential child abuse.
- The primary need is for an investigation into the cause of the injuries and protection for the child, which falls under the purview of CPS.
More Authorization requirements US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.