Symptom management at end of life US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Symptom management at end of life. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Symptom management at end of life US Medical PG Question 1: A 72-year-old woman with metastatic ovarian cancer is brought to the physician by her son because she is in immense pain and cries all the time. On a 10-point scale, she rates the pain as an 8 to 9. One week ago, a decision to shift to palliative care was made after she failed to respond to 2 years of multiple chemotherapy regimens. She is now off chemotherapy drugs and has been in hospice care. Current medications include 2 mg morphine intravenously every 2 hours and 650 mg of acetaminophen every 4 to 6 hours. The son is concerned because he read online that increasing the dose of morphine would endanger her breathing. Which of the following is the most appropriate next step in management?
- A. Counsel patient and continue same opioid dose
- B. Increase dosage of morphine (Correct Answer)
- C. Change morphine to a non-opioid analgesic
- D. Initiate palliative radiotherapy
- E. Initiate cognitive behavioral therapy
Symptom management at end of life Explanation: ***Increase dosage of morphine***
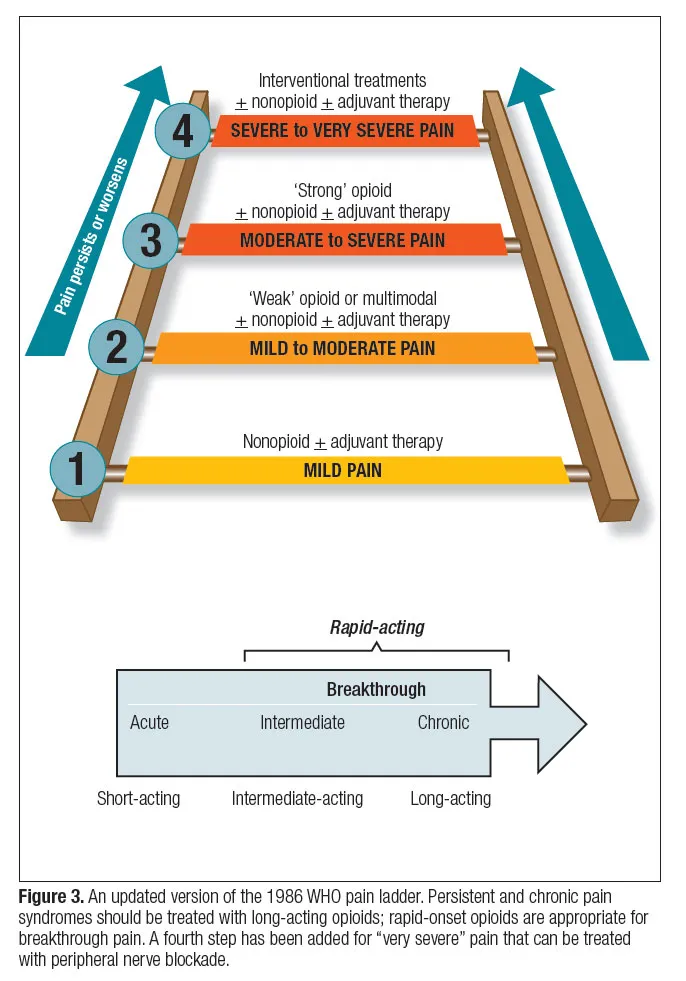
- The patient is experiencing severe, **uncontrolled pain** (8-9/10), indicating her current morphine dose is inadequate. In palliative care, the goal is to provide maximum comfort, and **opioid dose escalation** is appropriate to achieve this.
- While respiratory depression is a concern with opioids, in patients with chronic pain who are already on opioids, **tolerance to respiratory depressant effects** develops more quickly than tolerance to analgesic effects. Careful titration and monitoring can safely increase pain relief.
*Counsel patient and continue same opioid dose*
- The patient's pain is severe and unmanaged, so simply counseling her without addressing the **inadequate analgesia** would be inappropriate and unethical.
- Continuing the same dose would perpetuate her suffering, as the current regimen is clearly **insufficient for pain control**.
*Change morphine to a non-opioid analgesic*
- For severe cancer pain (8-9/10), **non-opioid analgesics** alone are typically ineffective.
- Switching to a non-opioid would likely lead to even poorer pain control and increased suffering, as opioids are the **cornerstone of severe cancer pain management**.
*Initiate palliative radiotherapy*
- While **radiotherapy** can be effective for localized pain caused by bone metastases, its onset of action is not immediate, and the primary issue here is urgent, **uncontrolled systemic pain**.
- It is not an appropriate initial step for immediate pain relief in a patient already in hospice with widespread metastatic disease and severe current pain.
*Initiate cognitive behavioral therapy*
- **Cognitive behavioral therapy (CBT)** can be a useful adjunct in chronic pain management to help with coping strategies and psychological distress.
- However, it does not directly address the severe, acute physical pain the patient is experiencing and is not a substitute for **pharmacological pain control** in this context.
Symptom management at end of life US Medical PG Question 2: A 35-year-old male is picked up by paramedics presenting with respiratory depression, pupillary constriction, and seizures. Within a few minutes, the male dies. On autopsy, fresh tracks marks are seen on both arms. Administration of which of the following medications would have been appropriate for this patient?
- A. Methadone
- B. Flumazenil
- C. Bupropion
- D. Naloxone (Correct Answer)
- E. Diazepam
Symptom management at end of life Explanation: ***Naloxone***
- The patient's presentation with **respiratory depression**, **pupillary constriction**, and **fresh track marks** is highly indicative of an **opioid overdose**.
- **Naloxone** is a potent **opioid receptor antagonist** that rapidly reverses the effects of opioid overdose, including respiratory depression.
*Methadone*
- **Methadone** is a **long-acting opioid agonist** used for pain management and **opioid dependence treatment**.
- Administering methadone would worsen an opioid overdose by increasing the opioid effect, potentially deepening respiratory depression.
*Flumazenil*
- **Flumazenil** is an **antidote for benzodiazepine overdose**, acting as a competitive antagonist at the GABA-A receptor.
- It would not be effective in reversing an opioid overdose, as the patient's symptoms are not consistent with benzodiazepine intoxication.
*Bupropion*
- **Bupropion** is an **antidepressant** and **smoking cessation aid** that works by inhibiting the reuptake of norepinephrine and dopamine.
- It has no role in the acute management of opioid overdose and would not address the life-threatening respiratory depression.
*Diazepam*
- **Diazepam** is a **benzodiazepine** that has sedative, anxiolytic, anticonvulsant, and muscle relaxant properties.
- While it could address seizures, it would exacerbate the underlying respiratory depression in an opioid overdose.
Symptom management at end of life US Medical PG Question 3: A 69-year-old man with aggressive metastatic cholangiocarcinoma presents after the second round of chemotherapy. He has suffered a great deal of pain from the metastasis to his spine, and he is experiencing side effects from the cytotoxic chemotherapy drugs. Imaging shows no change in the tumor mass and reveals the presence of several new metastatic lesions. The patient is not willing to undergo any more chemotherapy unless he gets something for pain that will “knock him out”. High-dose opioids would be effective, in his case, but carry a risk of bradypnea and sudden respiratory failure. Which of the following is the most appropriate next step in management?
- A. Put him in a medically-induced coma during chemotherapy sessions
- B. Stop chemotherapy
- C. Continue another round of chemotherapy without opioids
- D. Give the high-dose opioids (Correct Answer)
- E. Give a lower dose even though it has less efficacy
Symptom management at end of life Explanation: ***Give the high-dose opioids***
- Given the patient's **aggressive metastatic cholangiocarcinoma**, lack of response to chemotherapy, severe pain, and desire for effective pain relief, providing **high-dose opioids** aligns with the principles of **palliative care** and patient autonomy at the end of life.
- In a situation where cure is not possible and the patient prioritizes pain relief, even with the risk of **bradypnea** or **respiratory failure**, the focus shifts to maximizing comfort and quality of life.
- The **principle of double effect** applies here: the intent is to relieve suffering, not to hasten death, making this ethically appropriate end-of-life care.
*Put him in a medically-induced coma during chemotherapy sessions*
- A medically-induced coma is an extreme measure usually reserved for conditions like severe brain injury or intractable seizures, not for managing pain during **chemotherapy** or preventing awareness of side effects.
- This option does not address the underlying issue of the **chemotherapy's ineffectiveness** and adds significant risks and complications without clear benefit in this scenario.
*Stop chemotherapy*
- While chemotherapy has been ineffective and caused side effects, the decision to **stop chemotherapy** solely based on patient symptoms or ineffective treatment should be a shared decision, but the question specifically asks for the next step regarding pain management.
- Stopping chemotherapy without addressing the patient's severe pain and his direct request for effective pain relief would be incomplete in this context.
*Continue another round of chemotherapy without opioids*
- The patient has expressed unwillingness to continue chemotherapy without effective pain relief, stating he needs "something for pain that will knock him out," making this option directly contradictory to his wishes.
- Continuing ineffective chemotherapy while denying proper pain management would cause further suffering without benefit, violating principles of **palliative care** and **patient autonomy**.
*Give a lower dose even though it has less efficacy*
- The patient explicitly stated his desire for pain relief that will "knock him out," indicating dissatisfaction with current or sub-therapeutic pain management.
- Providing a **lower, less effective dose of opioids** would go against the patient's expressed wishes and would likely fail to alleviate his severe pain adequately, diminishing his quality of life in his final days.
Symptom management at end of life US Medical PG Question 4: A 42-year-old man is discovered unconscious by local police while patrolling in a park. He is unresponsive to stimulation. Syringes were found scattered around him. His heart rate is 70/min and respiratory rate is 6/min. Physical examination reveals a disheveled man with track marks on both arms. His glasgow coma scale is 8. Pupillary examination reveals miosis. An ambulance is called and a reversing agent is administered. Which of the following is most accurate regarding the reversal agent most likely administered to this patient?
- A. Works on dopamine receptors
- B. Has a short half-life
- C. Can be given per oral
- D. Results in acute withdrawal (Correct Answer)
- E. Is a non-competitive inhibitor
Symptom management at end of life Explanation: ***Results in acute withdrawal***
- The patient's presentation (unconscious, track marks, miosis, bradypnea) is characteristic of **opioid overdose**. The reversal agent, **naloxone**, rapidly displaces opioids from their receptors, leading to an abrupt onset of withdrawal symptoms.
- **Acute opioid withdrawal** can manifest with symptoms like nausea, vomiting, diarrhea, muscle cramps, and agitation, as the body suddenly lacks the opioid-induced suppression.
- This is the **most clinically significant** characteristic of naloxone in the acute overdose setting, as it explains the immediate physiological response patients experience.
*Works on dopamine receptors*
- **Naloxone** primarily acts as an **opioid receptor antagonist**, particularly at the mu-opioid receptor.
- It does not significantly interact with or exert its primary effects through **dopamine receptors**.
*Has a short half-life*
- While this statement is **factually true** (naloxone has a half-life of 30-81 minutes), it describes a **pharmacokinetic property** rather than a characteristic of its reversal mechanism.
- The question asks about the reversal agent in the context of immediate administration, where the **acute precipitation of withdrawal** is the most defining and immediate clinical consequence.
- The short half-life is clinically relevant for monitoring (patients may re-sedate), but it is not the most accurate statement regarding what happens when the reversal agent is administered.
*Can be given per oral*
- Although **naloxone** can be administered orally, its **bioavailability via the oral route is very low** (less than 3%) due to extensive first-pass metabolism.
- For acute overdose reversal, it is typically administered via intravenous, intramuscular, subcutaneous, or intranasal routes for rapid and effective absorption.
*Is a non-competitive inhibitor*
- **Naloxone** is a **competitive antagonist** of opioid receptors, meaning it competes with opioids for binding sites.
- It does not bind to an allosteric site to reduce the opioid's efficiency (non-competitive inhibition); rather, it directly blocks the receptor.
Symptom management at end of life US Medical PG Question 5: A 67-year-old woman is brought by ambulance from home to the emergency department after she developed weakness of her left arm and left face droop. According to her husband, she has a history of COPD, hypertension, and hyperlipidemia. She takes hydrochlorothiazide, albuterol, and atorvastatin. She is not on oxygen at home. She is an active smoker and has smoked a pack a day for 20 years. Her mother died of a heart attack at age 60 and her father died of prostate cancer at age 55. By the time the ambulance arrived, she was having difficulty speaking. Once in the emergency department, she is no longer responsive. Her blood pressure is 125/85 mm Hg, the temperature is 37.2°C (99°F), the heart rate is 77/min, and her breathing is irregular, and she is taking progressively deeper inspirations interrupted with periods of apnea. Of the following, what is the next best step?
- A. Start tissue plasminogen activator (tPA)
- B. Intubate the patient (Correct Answer)
- C. Consult a cardiologist
- D. Obtain an MRI of brain
- E. Obtain non-contrast enhanced CT of brain
Symptom management at end of life Explanation: ***Intubate the patient***
- The patient's **irregular breathing pattern with progressively deeper inspirations interrupted by periods of apnea** (known as **Cheyne-Stokes respiration**) combined with unresponsiveness due to probable acute stroke indicates imminent respiratory failure and the need for **airway protection**.
- **Intubation** secures the airway, ensures adequate ventilation, and prevents aspiration during a neurological emergency.
*Start tissue plasminogen activator (tPA)*
- Although this patient likely has an **acute ischemic stroke**, the first priority is managing the **compromised airway and breathing**.
- **tPA** administration is time-sensitive but requires stabilization of vital signs and exclusion of hemorrhage via neuroimaging, which hasn't occurred yet.
*Consult a cardiologist*
- While the patient has significant **cardiovascular risk factors** (**hypertension, hyperlipidemia, smoking, COPD, family history**), an acute cardiac event is not the immediate concern.
- The pressing issue is **acute neurological deterioration with respiratory compromise**.
*Obtain an MRI of brain*
- An **MRI** offers detailed imaging for stroke but is **time-consuming** and **less accessible** in an emergency compared to CT.
- The patient's critical respiratory status requires immediate intervention before non-urgent diagnostic imaging.
*Obtain non-contrast enhanced CT of brain*
- A **non-contrast CT scan of the brain** is crucial for differentiating between **ischemic** and **hemorrhagic stroke** and guiding treatment, specifically for tPA administration.
- However, ensuring a **patent airway and stable ventilation** takes precedence over imaging in a patient with impending respiratory arrest.
Symptom management at end of life US Medical PG Question 6: An 83-year-old man is being seen in the hospital for confusion. The patient was admitted 4 days ago for pneumonia. He has been improving on ceftriaxone and azithromycin. Then 2 nights ago he had an episode of confusion. He was unsure where he was and attempted to leave. He was calmed down by nurses with redirection. He had a chest radiograph that was stable from admission, a normal EKG, and a normal urinalysis. This morning he was alert and oriented. Then this evening he became confused and agitated again. The patient has a history of benign prostatic hyperplasia, severe dementia, and osteoarthritis. He takes tamsulosin in addition to the newly started antibiotics. Upon physical examination, the patient is alert but orientated only to name. He tries to get up, falls back onto the bed, and grabs his right knee. He states, “I need to get to work. My boss is waiting, but my knee hurts.” He tries to walk again, threatens the nurse who stops him, and throws a plate at the wall. In addition to reorientation, which of the following is the next best step in management?
- A. Morphine
- B. Lorazepam
- C. Haloperidol (Correct Answer)
- D. Rivastigmine
- E. Physical restraints
Symptom management at end of life Explanation: ***Haloperidol***
- The patient exhibits **delirium** with acute agitation, threatening behavior, and violent actions (throwing objects), representing an **imminent safety risk** to himself and staff.
- After **non-pharmacological interventions** (reorientation) have failed, **low-dose haloperidol** is appropriate for managing **severe agitation** in delirium when there is risk of harm.
- While antipsychotics have an FDA black box warning for increased mortality in elderly patients with dementia and recent evidence questions their efficacy in delirium, they remain indicated for **acute agitation with safety concerns** as a short-term intervention.
- Haloperidol is preferred over atypical antipsychotics in acute hospital settings due to availability in parenteral forms and lower anticholinergic burden.
*Morphine*
- While the patient mentions knee pain (likely from osteoarthritis), his **primary issue** is acute agitation and delirium, not pain management.
- **Opioids** can worsen delirium and confusion in elderly patients through anticholinergic effects and sedation.
- Pain should be addressed, but not as the primary intervention for violent, agitated behavior.
*Lorazepam*
- **Benzodiazepines** are generally **contraindicated in delirium** as they worsen confusion, increase fall risk, and can cause paradoxical agitation in elderly patients.
- The **only exceptions** are delirium from alcohol or benzodiazepine withdrawal, or seizures—none of which apply to this patient.
- Lorazepam would likely exacerbate rather than improve this patient's mental status.
*Rivastigmine*
- **Rivastigmine** is an acetylcholinesterase inhibitor for chronic management of **dementia symptoms**, not acute delirium.
- It has **no role** in managing acute behavioral disturbances and takes weeks to show any effect.
- Studies have not shown benefit of cholinesterase inhibitors in preventing or treating delirium.
*Physical restraints*
- Physical restraints should be used only as a **last resort** when pharmacological and non-pharmacological interventions have failed and there is immediate, serious risk of harm.
- Restraints can **increase agitation**, cause injuries, lead to delirium worsening, and are associated with increased morbidity and mortality.
- They do not address the underlying cause and should be avoided when other options are available.
Symptom management at end of life US Medical PG Question 7: A father calls the pediatrician because his 7-year-old son began wetting the bed days after the birth of his newborn sister. He punished his son for bedwetting but it only made the situation worse. The pediatrician advised him to talk with his son about how he feels, refrain from drinking water near bedtime, and praise his son when he keeps the bed dry. Which of the following best describes the reappearance of bedwetting?
- A. Isolation of affect
- B. Repression
- C. Regression (Correct Answer)
- D. Rationalization
- E. Identification
Symptom management at end of life Explanation: ***Regression***
- This **best describes this behavior** as the child is reverting to an earlier developmental stage (bedwetting) in response to stress (the birth of a new sibling).
- **Regression** is a common defense mechanism where an individual unconsciously escapes from present difficulties by returning to an earlier, less demanding stage of development.
*Isolation of affect*
- This defense mechanism involves separating the **emotion** from a painful event or memory, intellectualizing the situation without feeling the associated impact.
- The child is clearly experiencing the emotional impact, as evidenced by the bedwetting, rather than isolating it.
*Repression*
- **Repression** involves the unconscious blocking of unacceptable thoughts, feelings, or impulses from conscious awareness.
- While the birth of a sibling can lead to repressed feelings, the bedwetting is an *expression* of distress, not a full blocking of the experience.
*Rationalization*
- **Rationalization** is a defense mechanism where an individual attempts to explain or justify their behavior or feelings in a seemingly logical or acceptable way, avoiding the true reasons.
- The child's bedwetting is an involuntary physical response to stress, not a cognitive attempt to justify behavior.
*Identification*
- **Identification** is a defense mechanism where an individual unconsciously takes on the characteristics, attitudes, or behaviors of another person, often someone they admire or fear.
- The child's bedwetting is not an attempt to emulate or become like someone else.
Symptom management at end of life US Medical PG Question 8: A 72-year-old man presents to the emergency department with chest pain and shortness of breath. An EKG demonstrates an ST elevation myocardial infarction, and he is managed appropriately. The patient suffers from multiple comorbidities and was recently hospitalized for a myocardial infarction. The patient has a documented living will, which specifies that he does wish to receive resuscitative measures and blood products but refuses intubation in any circumstance. The patient is stabilized and transferred to the medical floor. On day 2, the patient presents with ventricular fibrillation and a resuscitative effort occurs. He is successfully resuscitated, but his pulmonary parameters warrant intervention and are acutely worsening. The patient's wife, son, and daughter are present and state that the patient should be intubated. The patient's prognosis even with intubation is very poor. Which of the following describes the best course of action?
- A. Intubate the patient - the family is representing the patient's most recent and accurate wishes
- B. Consult the hospital ethics committee
- C. Do not intubate the patient given his living will (Correct Answer)
- D. Intubate the patient - a patient's next of kin take precedence over a living will
- E. Do not intubate the patient as his prognosis is poor even with intubation
Symptom management at end of life Explanation: ***Do not intubate the patient given his living will***
- A **living will** or **advance directive** is a legally binding document that outlines a patient's wishes regarding medical treatment, including refusal of specific interventions like intubation.
- When the patient is **competent**, their stated wishes are paramount; when they are **incapacitated**, their advance directive becomes the primary guide for care decisions.
*Intubate the patient - the family is representing the patient's most recent and accurate wishes*
- While family input is valuable, a **legally executed living will** takes precedence over family opinions, especially when there's a conflict regarding specific life-sustaining treatments like intubation.
- There is no evidence presented that the patient has **revoked or updated** his living will.
*Consult the hospital ethics committee*
- While an ethics committee can provide guidance in complex cases, the patient's living will provides **clear instructions** that should be followed directly, making an immediate ethics committee consultation less necessary for this specific decision.
- The primary role of the ethics committee is to address **ambiguity or conflict** in patient care, which is not present regarding the patient's explicit refusal of intubation.
*Intubate the patient - a patient's next of kin take precedence over a living will*
- This statement is incorrect; a **valid living will** *takes precedence* over the wishes of the next of kin when the patient is unable to express their current desires.
- The next of kin's role is to act as a **surrogate decision-maker** only when a patient lacks capacity and has no advance directive that covers the specific situation.
*Do not intubate the patient as his prognosis is poor even with intubation*
- While a **poor prognosis** can be a factor in end-of-life discussions, the primary reason for not intubating in this scenario is the patient's explicit refusal documented in his **living will**, not solely the prognosis.
- Relying *only* on prognosis without considering the patient's prior stated wishes can undermine **patient autonomy**.
Symptom management at end of life US Medical PG Question 9: An 85-year-old man with terminal stage colon cancer formally designates his best friend as his medical durable power of attorney. After several courses of chemotherapy and surgical intervention, the patient’s condition does not improve, and he soon develops respiratory failure. He is then placed on a ventilator in a comatose condition. His friend with the medical power of attorney tells the care provider that the patient would not want to be on life support. The patient’s daughter disputes this and says that her father needs to keep receiving care, in case there should be any possibility of recovery. Additionally, there is a copy of the patient’s living will in the medical record which states that, if necessary, he should be placed on life support until full recovery. Which of the following is the most appropriate course of action?
- A. Withdraw the life support since the patient’s chances of recovery are very low
- B. Contact other family members to get their input for the patient
- C. Act according to the patient’s living will
- D. The durable medical power of attorney’s decision should be followed. (Correct Answer)
- E. Follow the daughter’s decision for the patient
Symptom management at end of life Explanation: ***The durable medical power of attorney's decision should be followed***
- The patient designated his friend as his **durable power of attorney for healthcare (DPOA)**, giving him legal authority to make medical decisions when the patient cannot communicate.
- While the living will states life support "until full recovery," the patient has **terminal stage colon cancer** - full recovery is **medically impossible**. The living will's condition cannot be fulfilled.
- When advance directive language is ambiguous or cannot be applied to actual clinical circumstances, the **DPOA's interpretive authority** is essential. The DPOA is expected to apply the patient's values to the real situation.
- The DPOA states the patient would not want to be on life support - this reflects the patient's **values and wishes** as understood by his chosen decision-maker, applied to the actual terminal situation.
- This honors both **patient autonomy** (through his chosen proxy) and the reality that advance directives cannot anticipate every clinical scenario.
*Act according to the patient's living will*
- While a living will expresses patient wishes, it states life support should continue "**until full recovery**" - but the patient has terminal cancer with no possibility of recovery.
- Literal adherence to an advance directive whose conditions are **medically impossible** does not serve the patient's true interests or autonomy.
- Living wills and DPOAs work **together** - the DPOA interprets and applies the living will to actual circumstances, especially when literal application is impossible or the situation wasn't anticipated.
*Withdraw the life support since the patient's chances of recovery are very low*
- While this may align with the DPOA's interpretation of the patient's wishes, unilateral physician decision-making without following the proper **decision-making hierarchy** is inappropriate.
- The physician should work **with the DPOA** rather than make independent decisions about life support withdrawal.
*Contact other family members to get their input for the patient*
- The patient **legally designated** his friend as DPOA, indicating his trust in this person's judgment over family members.
- While family input can be valuable, seeking additional opinions when there is a **legally appointed decision-maker** undermines the patient's explicit choice.
- The daughter has no legal standing to override the DPOA's decisions.
*Follow the daughter's decision for the patient*
- The daughter was **not designated** as the healthcare decision-maker; the friend was explicitly chosen as DPOA.
- Following the daughter's wishes would **violate** the patient's autonomous choice of decision-maker.
- Family relationship alone does not override a formal DPOA designation.
Symptom management at end of life US Medical PG Question 10: A 67-year-old man presents to the emergency department following an episode of chest pain and a loss of consciousness. The patient is in critical condition and his vital signs are rapidly deteriorating. It is known that the patient is currently undergoing chemotherapy for Hodgkin’s lymphoma. The patient is accompanied by his wife, who wants the medical staff to do everything to resuscitate the patient and bring him back. The patient also has 2 daughters, who are on their way to the hospital. The patient’s written advance directive states that the patient does not wish to be resuscitated or have any sort of life support. Which of the following is the appropriate course of action?
- A. Consult a judge
- B. Respect the patient’s advance directive orders (Correct Answer)
- C. Contact the patient’s siblings or other first-degree relatives
- D. Take into account the best medical decision made by the physician for the patient
- E. Respect the wife’s wishes and resuscitate the patient
Symptom management at end of life Explanation: ***Respect the patient’s advance directive orders***
- **Advance directives** legally document a patient's wishes regarding medical treatment, including end-of-life care, and must be honored if the patient is unable to make decisions.
- The patient's previously expressed autonomous decision, through a **written advance directive**, carries legal and ethical precedence over the wishes of family members or medical staff.
*Consult a judge*
- Consulting a judge is typically reserved for situations where there is **ambiguity or dispute** regarding the interpretation of an advance directive, or when no advance directive exists and family members disagree.
- In this case, the **written advance directive is clear**, making judicial intervention unnecessary.
*Contact the patient’s siblings or other first-degree relatives*
- Although family input can be valuable in some medical decisions, it does not **override a legally binding advance directive** made by the patient.
- The **patient's own wishes** are paramount, especially when clearly documented.
*Take into account the best medical decision made by the physician for the patient*
- While physicians provide medical expertise, patient **autonomy and established advance directives** take precedence over a physician's "best medical decision," especially regarding resuscitation.
- The physician's role here is to **implement the patient's documented wishes**, not to countermand them.
*Respect the wife’s wishes and resuscitate the patient*
- The wife's wishes, while important for emotional support, **do not legally or ethically supersede** the patient's explicit, written advance directive regarding resuscitation.
- Honoring the wife's request would violate the patient's **right to self-determination** and their previously stated wishes.
More Symptom management at end of life US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.