Pain management at end of life US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Pain management at end of life. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
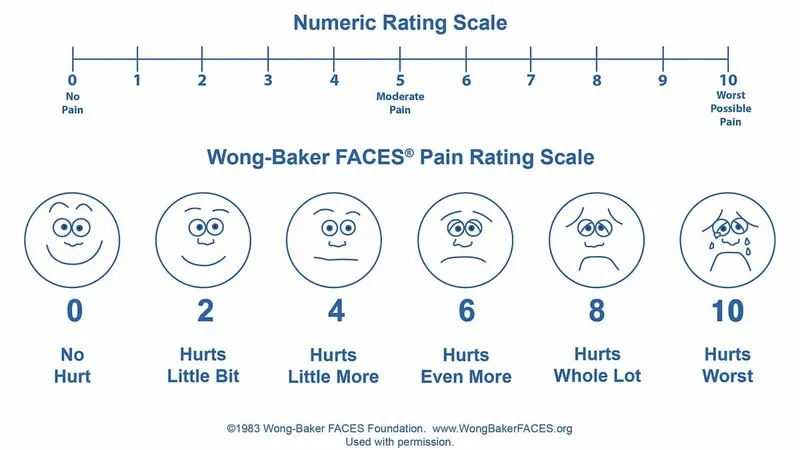
Pain management at end of life US Medical PG Question 1: A 72-year-old woman with metastatic ovarian cancer is brought to the physician by her son because she is in immense pain and cries all the time. On a 10-point scale, she rates the pain as an 8 to 9. One week ago, a decision to shift to palliative care was made after she failed to respond to 2 years of multiple chemotherapy regimens. She is now off chemotherapy drugs and has been in hospice care. Current medications include 2 mg morphine intravenously every 2 hours and 650 mg of acetaminophen every 4 to 6 hours. The son is concerned because he read online that increasing the dose of morphine would endanger her breathing. Which of the following is the most appropriate next step in management?
- A. Counsel patient and continue same opioid dose
- B. Increase dosage of morphine (Correct Answer)
- C. Change morphine to a non-opioid analgesic
- D. Initiate palliative radiotherapy
- E. Initiate cognitive behavioral therapy
Pain management at end of life Explanation: ***Increase dosage of morphine***
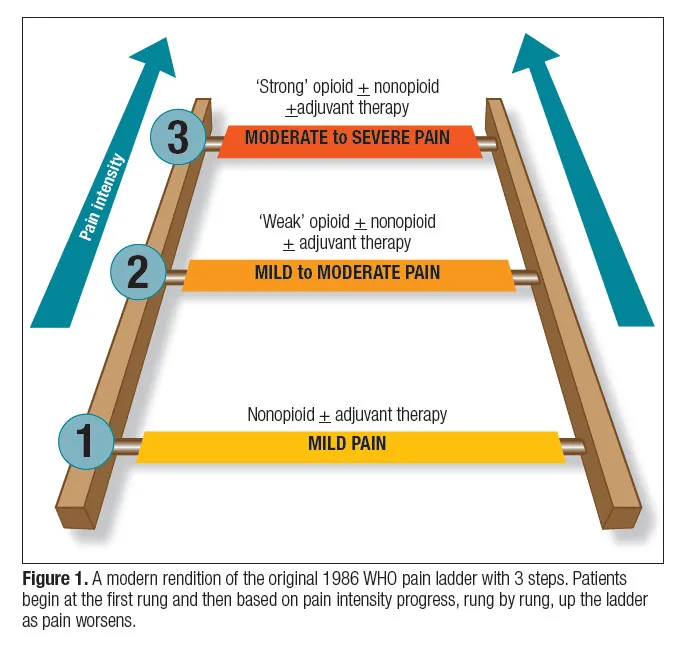
- The patient is experiencing severe, **uncontrolled pain** (8-9/10), indicating her current morphine dose is inadequate. In palliative care, the goal is to provide maximum comfort, and **opioid dose escalation** is appropriate to achieve this.
- While respiratory depression is a concern with opioids, in patients with chronic pain who are already on opioids, **tolerance to respiratory depressant effects** develops more quickly than tolerance to analgesic effects. Careful titration and monitoring can safely increase pain relief.
*Counsel patient and continue same opioid dose*
- The patient's pain is severe and unmanaged, so simply counseling her without addressing the **inadequate analgesia** would be inappropriate and unethical.
- Continuing the same dose would perpetuate her suffering, as the current regimen is clearly **insufficient for pain control**.
*Change morphine to a non-opioid analgesic*
- For severe cancer pain (8-9/10), **non-opioid analgesics** alone are typically ineffective.
- Switching to a non-opioid would likely lead to even poorer pain control and increased suffering, as opioids are the **cornerstone of severe cancer pain management**.
*Initiate palliative radiotherapy*
- While **radiotherapy** can be effective for localized pain caused by bone metastases, its onset of action is not immediate, and the primary issue here is urgent, **uncontrolled systemic pain**.
- It is not an appropriate initial step for immediate pain relief in a patient already in hospice with widespread metastatic disease and severe current pain.
*Initiate cognitive behavioral therapy*
- **Cognitive behavioral therapy (CBT)** can be a useful adjunct in chronic pain management to help with coping strategies and psychological distress.
- However, it does not directly address the severe, acute physical pain the patient is experiencing and is not a substitute for **pharmacological pain control** in this context.
Pain management at end of life US Medical PG Question 2: A 35-year-old male is picked up by paramedics presenting with respiratory depression, pupillary constriction, and seizures. Within a few minutes, the male dies. On autopsy, fresh tracks marks are seen on both arms. Administration of which of the following medications would have been appropriate for this patient?
- A. Methadone
- B. Flumazenil
- C. Bupropion
- D. Naloxone (Correct Answer)
- E. Diazepam
Pain management at end of life Explanation: ***Naloxone***
- The patient's presentation with **respiratory depression**, **pupillary constriction**, and **fresh track marks** is highly indicative of an **opioid overdose**.
- **Naloxone** is a potent **opioid receptor antagonist** that rapidly reverses the effects of opioid overdose, including respiratory depression.
*Methadone*
- **Methadone** is a **long-acting opioid agonist** used for pain management and **opioid dependence treatment**.
- Administering methadone would worsen an opioid overdose by increasing the opioid effect, potentially deepening respiratory depression.
*Flumazenil*
- **Flumazenil** is an **antidote for benzodiazepine overdose**, acting as a competitive antagonist at the GABA-A receptor.
- It would not be effective in reversing an opioid overdose, as the patient's symptoms are not consistent with benzodiazepine intoxication.
*Bupropion*
- **Bupropion** is an **antidepressant** and **smoking cessation aid** that works by inhibiting the reuptake of norepinephrine and dopamine.
- It has no role in the acute management of opioid overdose and would not address the life-threatening respiratory depression.
*Diazepam*
- **Diazepam** is a **benzodiazepine** that has sedative, anxiolytic, anticonvulsant, and muscle relaxant properties.
- While it could address seizures, it would exacerbate the underlying respiratory depression in an opioid overdose.
Pain management at end of life US Medical PG Question 3: A 29-year-old man is admitted to the emergency department following a motorcycle accident. The patient is severely injured and requires life support after splenectomy and evacuation of a subdural hematoma. Past medical history is unremarkable. The patient’s family members, including wife, parents, siblings, and grandparents, are informed about the patient’s condition. The patient has no living will and there is no durable power of attorney. The patient must be put in an induced coma for an undetermined period of time. Which of the following is responsible for making medical decisions for the incapacitated patient?
- A. The spouse (Correct Answer)
- B. An older sibling
- C. Physician
- D. Legal guardian
- E. The parents
Pain management at end of life Explanation: ***The spouse***
- In the absence of a **living will** or **durable power of attorney**, the law typically designates the **spouse** as the primary decision-maker for an incapacitated patient.
- This hierarchy is established to ensure decisions are made by the individual most intimately connected and presumed to understand the patient's wishes.
*An older sibling*
- Siblings are generally further down the **hierarchy of surrogate decision-makers** than a spouse or parents.
- They would typically only be considered if higher-priority family members are unavailable or unwilling to make decisions.
*Physician*
- The physician's role is to provide medical care and guidance, not to make medical decisions for an incapacitated patient when family surrogates are available.
- Physicians only make decisions in **emergency situations** when no surrogate is immediately available and treatment is immediately necessary to save the patient's life or prevent serious harm.
*Legal guardian*
- A legal guardian is usually appointed by a **court** when there is no appropriate family member available or when there is a dispute among family members.
- In this scenario, with a spouse and other close family members present, a legal guardian would not be the first choice.
*The parents*
- While parents are close family members, they are typically considered **secondary to the spouse** in the hierarchy of surrogate decision-makers for an adult patient.
- They would usually only be the decision-makers if the patient were unmarried or the spouse were unavailable.
Pain management at end of life US Medical PG Question 4: A 25-year-old man comes to the physician for severe back pain. He describes the pain as shooting and stabbing. On a 10-point scale, he rates the pain as a 9 to 10. The pain started after he lifted a heavy box at work; he works at a supermarket and recently switched from being a cashier to a storekeeper. The patient appears to be in severe distress. Vital signs are within normal limits. On physical examination, the spine is nontender without paravertebral muscle spasms. Range of motion is normal. A straight-leg raise test is negative. After the physical examination has been completed, the patient asks for a letter to his employer attesting to his inability to work as a storekeeper. Which of the following is the most appropriate response?
- A. “Yes. Since work may worsen your condition, I would prefer that you stay home a few days. I will write a letter to your employer to explain the situation.”
- B. You say you are in severe pain. However, the physical examination findings do not suggest a physical problem that can be addressed with medications or surgery. I'd like to meet on a regular basis to see how you're doing.
- C. I understand that you are uncomfortable, but the findings do not match the severity of your symptoms. Let's talk about the recent changes at your job. (Correct Answer)
- D. The physical exam findings do not match your symptoms, which suggests a psychological problem. I would be happy to refer you to a mental health professional.
- E. The physical exam findings suggest a psychological rather than a physical problem. But there is a good chance that we can address it with cognitive-behavioral therapy.
Pain management at end of life Explanation: ***"I understand that you are uncomfortable, but the findings do not match the severity of your symptoms. Let's talk about the recent changes at your job."***
- This response acknowledges the patient's reported discomfort while gently highlighting the **discrepancy between symptoms and objective findings**, which is crucial in cases of suspected **somatoform or functional pain**.
- It also opens communication about potential **psychosocial stressors** related to his job change, which could be contributing to his symptoms, without dismissing his pain or making a premature diagnosis.
*"You say you are in severe pain. However, the physical examination findings do not suggest a physical problem that can be addressed with medications or surgery. I'd like to meet on a regular basis to see how you're doing."*
- While this option correctly identifies the lack of physical findings, it can be perceived as dismissive of the patient's pain, potentially damaging the **physician-patient relationship**.
- Suggesting regular meetings without a clear plan for addressing his immediate concerns or exploring underlying issues might not be the most effective initial approach.
*“Yes. Since work may worsen your condition, I would prefer that you stay home a few days. I will write a letter to your employer to explain the situation.”*
- This response would **validate the patient's claim of severe pain** without objective evidence, potentially reinforcing illness behavior and avoiding addressing the underlying issue.
- Providing a doctor's note for inability to work without a clear diagnostic basis or understanding of the pain's origin is **medically inappropriate** and could set a precedent for future such requests.
*"The physical exam findings do not match your symptoms, which suggests a psychological problem. I would be happy to refer you to a mental health professional."*
- Directly labeling the problem as "psychological" can be **stigmatizing and alienating** to the patient, leading to distrust and resistance to care.
- While a psychological component might be present, immediately referring to mental health without further exploration of the patient's situation or current stressors is premature and lacks empathy.
*"The physical exam findings suggest a psychological rather than a physical problem. But there is a good chance that we can address it with cognitive-behavioral therapy."*
- Similar to the previous option, explicitly stating a "psychological problem" can be **stigmatizing**.
- Jumping directly to recommending **cognitive-behavioral therapy (CBT)** without a comprehensive discussion and patient buy-in is premature and may lead to non-compliance.
Pain management at end of life US Medical PG Question 5: A 25-year-old man is brought to the emergency department after his girlfriend discovered him at home in a minimally responsive state. He has a history of drinking alcohol excessively and using illicit drugs. On arrival, he does not respond to commands but withdraws all extremities to pain. His pulse is 90/min, respirations are 8/min, and blood pressure is 130/90 mm Hg. Pulse oximetry while receiving bag-valve-mask ventilation shows an oxygen saturation of 95%. Examination shows cool, dry skin, with scattered track marks on his arms and legs. The pupils are pinpoint and react sluggishly to light. His serum blood glucose level is 80 mg/dL. The most appropriate next step in management is intravenous administration of which of the following?
- A. Fomepizole
- B. Naltrexone
- C. Methadone
- D. Naloxone (Correct Answer)
- E. Phentolamine
Pain management at end of life Explanation: ***Naloxone***
- The patient presents with classic signs of **opioid overdose**: altered mental status, **respiratory depression** (8/min), and **pinpoint pupils**.
- **Naloxone** is an opioid antagonist that rapidly reverses the effects of opioid toxicity and is the most appropriate first-line treatment in this scenario.
*Fomepizole*
- This medication is used as an antidote for **methanol** and **ethylene glycol poisoning**, which typically present with metabolic acidosis and renal failure, not pinpoint pupils and respiratory depression.
- There are no clinical signs in this patient indicative of methanol or ethylene glycol ingestion.
*Naltrexone*
- **Naltrexone** is an opioid antagonist used for long-term management of opioid use disorder or alcohol dependence, but it is not used in acute overdose resuscitation due to its slower onset and formulation (oral or long-acting injectable).
- Its primary role is to prevent relapse, not to reverse acute respiratory depression.
*Methadone*
- **Methadone** is a long-acting opioid agonist used for opioid replacement therapy and chronic pain management.
- Administering methadone would worsen the patient's opioid-induced respiratory depression and central nervous system depression.
*Phentolamine*
- **Phentolamine** is an alpha-adrenergic blocker used to treat hypertensive crises, particularly those caused by pheochromocytoma or extravasation of vasopressors.
- It has no role in managing opioid overdose and could lead to hypotension in this patient.
Pain management at end of life US Medical PG Question 6: An 83-year-old man with advanced-stage prostate cancer comes to the physician because of a 1-week history of worsening lower back and hip pain. The patient's analgesic regimen includes oxycodone, ibuprofen, and alendronic acid. Physical examination shows localized tenderness over the lumbar spine and right hip. His current pain management requires opioid dose escalation. Which of the following opioid side effects is most likely to remain unaffected by the mechanism underlying this patient's need for a higher drug dose?
- A. Pruritus
- B. Constipation (Correct Answer)
- C. Mydriasis
- D. Respiratory depression
- E. Nausea
Pain management at end of life Explanation: ***Constipation***
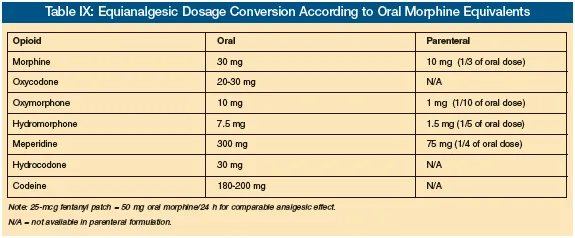
- **Opioid-induced constipation** is mediated by direct opioid receptor activation in the **enteric nervous system**, reducing gut motility.
- Unlike most other opioid side effects, the body generally does not develop **tolerance** to this effect, meaning it persists even with chronic use and dose escalation.
*Pruritus*
- **Opioid-induced pruritus** is often due to **histamine release** from mast cells, which is a common side effect of opioid administration.
- **Tolerance** can develop to pruritus over time, meaning it may lessen or resolve with chronic opioid use or dose escalation as the body adapts.
*Mydriasis*
- **Mydriasis** (pupil dilation) is not a typical opioid side effect; rather, **miosis** (pinpoint pupils) is characteristic of opioid use.
- Furthermore, **miosis** itself can exhibit some degree of **tolerance** with chronic opioid use, though it is often one of the more persistent effects.
*Respiratory depression*
- **Respiratory depression** is a serious and dose-dependent opioid side effect caused by decreased sensitivity of the respiratory center in the brainstem to CO2.
- While it is a dangerous effect, **tolerance** can develop to respiratory depression with chronic opioid use, reducing its severity over time.
*Nausea*
- **Opioid-induced nausea** is thought to be mediated by the **chemoreceptor trigger zone (CTZ)** in the brain and slowed gastric emptying.
- The body often develops **tolerance** to opioid-induced nausea within a few days to weeks of consistent opioid use.
Pain management at end of life US Medical PG Question 7: A 55-year-old man comes to the physician because of a 2-month history of gradually worsening pain and burning in his feet that is impairing his ability to sleep. He also has a non-healing, painless ulcer on the bottom of his right toe, which has been progressively increasing in size despite the application of bandages and antiseptic creams at home. He has a 7-year history of type II diabetes mellitus treated with oral metformin. He also has narrow-angle glaucoma treated with timolol eye drops and chronic back pain due to a motorcycle accident a few years ago, which is treated with tramadol. Vital signs are within normal limits. Physical examination shows a 3-cm, painless ulcer on the plantar surface of the right toe. The ulcer base is dry, with no associated erythema, edema, or purulent discharge. Neurological examination shows loss of touch, pinprick sensation, proprioception, and vibration sense of bilateral hands and feet. These sensations are preserved in the proximal portions of the limbs. Muscle strength is normal. Bilateral ankle reflexes are absent. A diabetic screening panel is done and shows a fasting blood sugar of 206 mg/dL. An ECG shows a left bundle branch block. Which of the following is the most appropriate next step in the management of this patient's pain?
- A. Oxycodone
- B. Pregabalin (Correct Answer)
- C. Injectable insulin
- D. Amitriptyline
- E. Ulcer debridement
Pain management at end of life Explanation: ***Pregabalin***
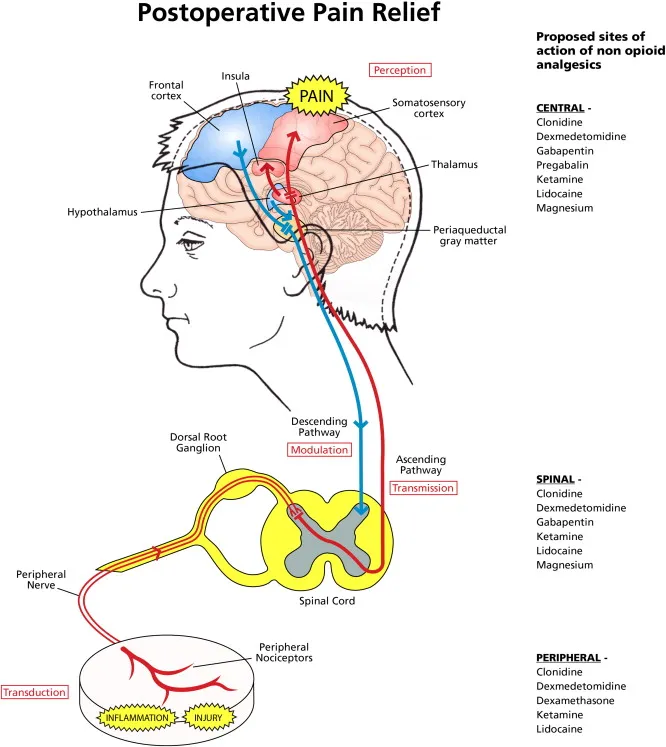
- This patient presents with symptoms highly suggestive of **diabetic peripheral neuropathy**, including burning pain in the feet, a painless neuropathic ulcer, and loss of sensation in a stocking-glove distribution with absent ankle reflexes. **Pregabalin** is a first-line agent for neuropathic pain.
- It works by binding to the **α2δ subunit of voltage-gated calcium channels**, reducing the release of excitatory neurotransmitters.
- Pregabalin is **preferred over amitriptyline** in this patient due to his cardiac conduction abnormality (LBBB) and age-related concerns with anticholinergic effects.
*Oxycodone*
- **Opioids like oxycodone** are generally not recommended as first-line treatment for chronic neuropathic pain due to concerns about tolerance, dependence, and side effects.
- While it may provide some pain relief, the **risks often outweigh the benefits** for long-term management of diabetic neuropathy.
*Injectable insulin*
- Poorly controlled **diabetes mellitus** is the underlying cause for the patient's neuropathy and ulcer, and optimizing glycemic control (e.g., with insulin) is crucial for preventing progression and complications.
- However, **injectable insulin** is not a direct treatment for the symptomatic **neuropathic pain or burning sensation** the patient is experiencing.
- While important for long-term management, it does not address the immediate complaint of pain.
*Amitriptyline*
- **Amitriptyline**, a tricyclic antidepressant, is another first-line medication for **neuropathic pain**.
- However, it is **relatively contraindicated** in this patient due to his **left bundle branch block (LBBB)**, as tricyclic antidepressants can worsen cardiac conduction abnormalities and increase the risk of arrhythmias.
- Additionally, as an **anticholinergic** agent, it is generally less preferred in older patients due to potential side effects like urinary retention, constipation, dry mouth, dizziness, and confusion.
*Ulcer debridement*
- **Ulcer debridement** is an important step in the management of the non-healing ulcer to promote healing and prevent infection.
- While crucial for ulcer management, it does not directly address the primary complaint of **burning neuropathic pain** in the feet.
Pain management at end of life US Medical PG Question 8: A 72-year-old woman is brought to the emergency department by ambulance after an unexpected fall at home 1 hour ago. She was resuscitated at the scene by paramedics before being transferred to the hospital. She has a history of ischemic heart disease and type 2 diabetes mellitus. She has not taken any sedative medications. Her GCS is 6. She is connected to a mechanical ventilator. Her medical records show that she signed a living will 5 years ago, which indicates her refusal to receive any type of cardiopulmonary resuscitation, intubation, or maintenance of life support on mechanical ventilation. Her son, who has a durable power-of-attorney for her healthcare decisions, objects to the discontinuation of mechanical ventilation and wishes that his mother be kept alive without suffering in the chance that she might recover. Which of the following is the most appropriate response to her son regarding his wishes for his mother?
- A. “We will take every measure necessary to prolong her life.”
- B. “She may be eligible for hospice care.”
- C. “The opinion of her primary care physician must be obtained regarding further steps in management.”
- D. “Based on her wishes, mechanical ventilation must be discontinued.” (Correct Answer)
- E. “Further management decisions will be referred to the hospital’s ethics committee.”
Pain management at end of life Explanation: ***Based on her wishes, mechanical ventilation must be discontinued.***
- A **living will** is a legally binding document that outlines a patient's wishes regarding medical treatment, including **refusal of life support**.
- In this scenario, the patient’s clear and documented wishes in her living will take precedence over the son's objections, even though he holds **durable power of attorney for healthcare** (DPA).
*“We will take every measure necessary to prolong her life.”*
- This statement directly contradicts the patient's **documented wishes** in her living will to refuse intubation and maintenance on mechanical ventilation.
- Ignoring a patient's advance directive can lead to ethical and legal issues, as it undermines the principle of **patient autonomy**.
*“She may be eligible for hospice care.”*
- While hospice care is a relevant consideration for patients with terminal illnesses, suggesting it prematurely without addressing the immediate issue of the **living will** can be dismissive of the patient's explicit directives.
- The primary concern is upholding the patient's autonomy, which includes addressing her advance directive regarding **withdrawal of life support**.
*“The opinion of her primary care physician must be obtained regarding further steps in management.”*
- While the **primary care physician's** input is valuable for understanding the patient's overall health and discussing goals of care, the existence of a clear and legally binding **living will** simplifies the decision-making process concerning life support.
- The patient's advance directive is paramount and generally does not require further medical negotiation unless there's ambiguity or new information suggesting a change in her wishes.
*“Further management decisions will be referred to the hospital’s ethics committee.”*
- An **ethics committee** consultation may be appropriate in cases of ambiguity surrounding an advance directive, conflict among surrogates, or uncertainty about the patient's capacity at the time of signing the directive.
- However, in this case, the **living will** explicitly states her wishes regarding mechanical ventilation, making the patient's intent clear and generally overriding the need for an ethics committee in the initial response.
Pain management at end of life US Medical PG Question 9: A 67-year-old man comes to the clinic for establishment of care. He recently retired and moved to Florida with his wife. His past medical history includes hypertension, diabetes, chronic back pain, and hyperlipidemia. According to the patient, he takes lisinopril, metformin, atorvastatin, acetaminophen, and methadone. His previous doctor prescribed methadone for breakthrough pain as he has been having more severe pain episodes due to the recent move. He is currently out of his methadone and asks for a refill on the prescription. A physical examination is unremarkable except for mild lower extremity edema bilaterally and diffuse lower back pain upon palpation. What is the best initial step in the management of this patient?
- A. Refer the patient to a pain management clinic
- B. Inform the patient that methadone is not the best option and do not prescribe
- C. Encourage the patient to switch to duloxetine
- D. Assess the patient's pain medication history (Correct Answer)
- E. Prescribe a limited dose of methadone for breakthrough back pain
Pain management at end of life Explanation: ***Assess the patient's pain medication history***
- It is crucial to gather a comprehensive **pain medication history** for a new patient on long-term opioids, especially when they are requesting a refill for a potentially high-risk medication like **methadone**. This includes understanding the duration of use, previous dosages, other medications tried, and the effectiveness of prior treatments.
- A comprehensive assessment helps to identify potential risks, such as **opioid tolerance**, dependence, or drug-drug interactions, and allows the physician to make an informed decision regarding the patient's ongoing pain management plan in accordance with **CDC guidelines** on opioid prescribing.
*Refer the patient to a pain management clinic*
- While referral to a pain management clinic may be appropriate later, the **initial step** should involve a thorough assessment by the primary care physician to understand the patient's immediate needs and history, especially given the new patient encounter.
- A direct referral without an initial evaluation could delay critical care decisions related to safe opioid prescribing and **withdrawal prevention**.
*Inform the patient that methadone is not the best option and do not prescribe*
- Simply refusing to prescribe methadone without a proper assessment and alternative plan can lead to **opioid withdrawal** and non-adherence to care, which can be dangerous for the patient.
- While methadone has significant risks, abruptly discontinuing it without a transition plan is generally discouraged, as it can cause severe **rebound pain** and withdrawal symptoms.
*Encourage the patient to switch to duloxetine*
- Duloxetine is an appropriate medication for **neuropathic pain** and **chronic musculoskeletal pain**, but it's not an immediate solution for breakthrough pain in a patient accustomed to methadone and should only be considered after a full assessment and discussion of risks and benefits.
- Switching to duloxetine without a clear understanding of the patient's current pain control, opioid dependence, and potential for withdrawal is premature and could exacerbate the patient's pain and lead to severe **withdrawal symptoms**.
*Prescribe a limited dose of methadone for breakthrough back pain*
- Prescribing methadone without a complete and thorough assessment of the patient's pain history, current dosage, and potential interactions with other medications is not safe practice, especially for a **new patient**.
- Methadone has a **long and variable half-life**, making it prone to accumulation and overdose, and requires careful titration and monitoring, which cannot be done without a full history.
Pain management at end of life US Medical PG Question 10: A 67-year-old man comes to the physician for a follow-up examination. He has had lower back pain for several months. The pain radiates down the right leg to the foot. He has no history of any serious illness and takes no medications. His pain increases after activity. The straight leg test is positive on the right. The results of the laboratory studies show:
Laboratory test
Hemoglobin 14 g/d
Leukocyte count 5,500/mm3 with a normal differential
Platelet count 350,000/mm3
Serum
Calcium 9.0 mg/dL
Albumin 3.8 g/dL
Urea nitrogen 14 mg/dL
Creatinine 0.9 mg/dL
Serum immunoelectrophoresis shows an immunoglobulin G (IgG) type monoclonal component of 40 g/L. Bone marrow plasma cells return at 20%. Skeletal survey shows no bone lesions. Magnetic resonance imaging (MRI) shows a herniated disc at the L5. Which of the following is the most appropriate next step?
- A. Dexamethasone
- B. Thalidomide
- C. Physical therapy (Correct Answer)
- D. Autologous stem cell transplantation
- E. Plasmapheresis
Pain management at end of life Explanation: ***Physical therapy***
- The patient's symptoms of radiated lower back pain, positive straight leg test, and MRI findings of a **herniated disc at L5** are classic for **radiculopathy** caused by disc herniation.
- **Conservative management**, including physical therapy, is the most appropriate initial step for symptomatic lumbar disc herniation, aiming to reduce pain and improve function.
*Dexamethasone*
- While corticosteroids like dexamethasone can reduce inflammation and pain, they are typically considered for **short-term relief** in severe cases or as an adjunct, not as the primary or sole treatment for herniated disc.
- In the context of the elevated IgG monoclonal component and plasma cells, dexamethasone is part of treatment regimens for **multiple myeloma**, but the primary issue presented is disc herniation.
*Thalidomide*
- Thalidomide is an **immunomodulatory drug** used in the treatment of multiple myeloma, particularly in combination with dexamethasone.
- It has no role in the management of **lumbar disc herniation** or radiculopathy.
*Autologous stem cell transplantation*
- This is a treatment option for **multiple myeloma** once a patient achieves remission, especially in younger, fitter patients.
- It is an aggressive procedure and **not indicated** for the treatment of a herniated disc, nor as an initial step for myeloma given the current presentation.
*Plasmapheresis*
- Plasmapheresis is used to remove **excess proteins** or antibodies from the blood, often in conditions like hyperviscosity syndrome or specific autoimmune diseases.
- It is **not a treatment** for herniated disc and would only be considered for multiple myeloma in cases of severe hyperviscosity, which is not indicated by the current lab values.
More Pain management at end of life US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.