DNR/DNAR orders US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for DNR/DNAR orders. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
DNR/DNAR orders US Medical PG Question 1: A 76-year-old man is brought to the hospital after having a stroke. Head CT is done in the emergency department and shows intracranial hemorrhage. Upon arrival to the ED he is verbally non-responsive and withdraws only to pain. He does not open his eyes. He is transferred to the medical ICU for further management and intubated for airway protection. During his second day in the ICU, his blood pressure is measured as 91/54 mmHg and pulse is 120/min. He is given fluids and antibiotics, but he progresses to renal failure and his mental status deteriorates. The physicians in the ICU ask the patient’s family what his wishes are for end-of-life care. His wife tells the team that she is durable power of attorney for the patient and provides appropriate documentation. She mentions that he did not have a living will, but she believes that he would want care withdrawn in this situation, and therefore asks the team to withdraw care at this point. The patient’s daughter vehemently disagrees and believes it is in the best interest of her father, the patient, to continue all care. Based on this information, what is the best course of action for the physician team?
- A. Call other family members and consult them for their opinions
- B. Listen to the patient’s daughter’s wishes and continue all care
- C. Compromise between the wife and daughter and withdraw the fluids and antibiotics but keep the patient intubated
- D. Listen to the patient’s wife’s wishes and withdraw care (Correct Answer)
- E. Consult the hospital ethics committee and continue all care until a decision is reached
DNR/DNAR orders Explanation: ***Listen to the patient’s wife’s wishes and withdraw care***
- The **durable power of attorney for healthcare** legally designates the wife as the patient's surrogate decision-maker when the patient lacks capacity, overriding other family opinions.
- In the absence of a living will, the **surrogate's interpretation of the patient's best interests** and previously expressed wishes is legally and ethically binding.
*Call other family members and consult them for their opinions*
- While involving family is good practice in general, the presence of a **legally appointed durable power of attorney** means that other family members' opinions do not supersede the designated surrogate's decisions.
- Consulting other family members could **create more conflict and delay** crucial decisions, as the wife holds the legal authority.
*Listen to the patient’s daughter’s wishes and continue all care*
- The daughter's wishes, while understandable, **do not hold legal authority** over the decisions of the legally appointed durable power of attorney.
- Disregarding the wife's authority would be a **breach of ethical and legal obligations** in patient care.
*Compromise between the wife and daughter and withdraw the fluids and antibiotics but keep the patient intubated*
- A compromise that goes against the legal surrogate's explicitly stated decision (to withdraw all care) is **ethically problematic and legally unsound**.
- Healthcare decisions should be based on the patient's best interest as interpreted by the **authorized surrogate**, not on attempting to please all family members.
*Consult the hospital ethics committee and continue all care until a decision is reached*
- While an ethics committee consult is appropriate if there's **disagreement over the interpretation of the patient's wishes** *among legally designated surrogates* or concerns about the surrogate's decision-making capacity, it's not the first step when a clear legal surrogate with documentation is present and makes a decision.
- Continuing all care against the wishes of the **legal proxy** would be contrary to patient autonomy and the principles of substituted judgment.
DNR/DNAR orders US Medical PG Question 2: A 63-year-old woman is brought to the emergency department because of severe abdominal pain and vomiting for 3 hours. She had previous episodes of abdominal pain that lasted for 10–15 minutes and resolved with antacids. She lives with her daughter and grandchildren. She divorced her husband last year. She is alert and oriented. Her temperature is 37.3°C (99.1°F), pulse is 134/min, and blood pressure is 90/70 mm Hg. The abdomen is rigid and diffusely tender. Guarding and rebound tenderness are present. Rectal examination shows a collapsed rectum. Infusion of 0.9% saline is begun and a CT of the abdomen shows intestinal perforation. The surgeon discusses the need for emergent exploratory laparotomy with the patient and she agrees to it. Written informed consent is obtained. While in the holding area awaiting emergent transport to the operating room, she calls for the surgeon and informs him that she no longer wants the surgery. He explains the risks of not performing the surgery to her and she indicates she understands but is adamant about not proceeding with surgery. Which of the following is the most appropriate next step in management?
- A. Consult hospital ethics committee
- B. Obtain consent from the patient's daughter
- C. Obtain consent from the patient's ex-husband
- D. Continue with emergency life-saving surgery
- E. Cancel the surgery (Correct Answer)
DNR/DNAR orders Explanation: ***Cancel the surgery***
- The patient is **alert and oriented** and has indicated she understands the risks of refusing surgery, demonstrating **decision-making capacity**. An adult with intact capacity has the right to refuse medical treatment, even if it is life-saving.
- While the decision may seem medically unwise, **patient autonomy** is a fundamental ethical principle that must be respected once capacity is confirmed.
*Consult hospital ethics committee*
- An ethics committee consultation is typically reserved for situations where there is **uncertainty about a patient's capacity**, a conflict among healthcare providers, or a difficult ethical dilemma where principles of patient care are in clear conflict.
- In this case, the patient's capacity seems clear, and her refusal is unequivocal.
*Obtain consent from the patient's daughter*
- The patient's daughter cannot provide consent for her mother if the mother is **competent and able to make her own decisions**. **Surrogate decision-makers** are only legally authorized when the patient lacks capacity.
- The patient's expressed wishes directly override any potential preferences of her next-of-kin.
*Obtain consent from the patient's ex-husband*
- As the patient is divorced, her ex-husband has **no legal standing** to make medical decisions on her behalf.
- Even if they were still married, a spouse can only act as a surrogate if the patient lacks decision-making capacity.
*Continue with emergency life-saving surgery*
- Performing surgery against a **competent patient's explicit refusal** would be an act of **battery** and a violation of her **autonomy**.
- Even in life-threatening situations, a patient with capacity has the right to refuse treatment.
DNR/DNAR orders US Medical PG Question 3: A 35-year-old woman with no significant past medical history is brought in by ambulance after a major motor vehicle collision. Temperature is 97.8 deg F (36.5 deg C), blood pressure is 76/40, pulse is 110/min, and respirations are 12/min. She arouses to painful stimuli and makes incomprehensible sounds, but is unable to answer questions. Her abdomen is distended and diffusely tender to palpation. Bedside ultrasound shows blood in the peritoneal cavity. Her husband rushes to the bedside and states she is a Jehovah’s Witness and will refuse blood products. No documentation of blood refusal is available for the patient. What is the most appropriate next step in management?
- A. In accordance with the husband's wishes, do not transfuse any blood products
- B. Observe and reassess mental status in an hour to see if patient can consent for herself
- C. Attempt to contact the patient’s parents for additional collateral information
- D. Consult the hospital ethics committee
- E. Administer blood products (Correct Answer)
DNR/DNAR orders Explanation: **Administer blood products**
- In emergency situations where a patient is incapacitated and there is no **advance directive** or **legal proxy** explicitly refusing treatment, the principle of **presumed consent** applies, allowing life-saving interventions.
- The patient's husband's statement is not legally binding without a living will or medical power of attorney, especially when the patient's capacity to consent or refuse treatment is compromised due to critical injury.
*In accordance with the husband's wishes, do not transfuse any blood products*
- The husband's stated wishes are not legally sufficient to refuse life-saving treatment for an incapacitated adult unless he holds **durable power of attorney for health care** specifically outlining these wishes, which is not stated here.
- Deferring necessary treatment based solely on the husband's assertion could lead to the patient's death and potentially expose the medical team to **malpractice liability**.
*Observe and reassess mental status in an hour to see if patient can consent for herself*
- The patient presents with **severe hypovolemic shock** (BP 76/40, HR 110/min) and signs of significant hemorrhage, indicating an urgent, life-threatening situation.
- Delaying emergent treatment to wait for a change in mental status would likely result in irreversible harm or death, as her condition is rapidly deteriorating.
*Attempt to contact the patient’s parents for additional collateral information*
- Contacting other family members for more information would cause a **critical delay** in a life-threatening situation.
- Even if parents confirm the patient's faith, their input is still not a legally binding refusal of treatment without proper documentation or court order.
*Consult the hospital ethics committee*
- Ethics committee consultations are appropriate for complex ethical dilemmas that are not immediately life-threatening or when there is sufficient time for deliberation.
- In this **critical emergency** with an actively hemorrhaging patient in shock, consulting the ethics committee would cause an unacceptable delay in life-saving treatment.
DNR/DNAR orders US Medical PG Question 4: A 29-year-old man is admitted to the emergency department following a motorcycle accident. The patient is severely injured and requires life support after splenectomy and evacuation of a subdural hematoma. Past medical history is unremarkable. The patient’s family members, including wife, parents, siblings, and grandparents, are informed about the patient’s condition. The patient has no living will and there is no durable power of attorney. The patient must be put in an induced coma for an undetermined period of time. Which of the following is responsible for making medical decisions for the incapacitated patient?
- A. The spouse (Correct Answer)
- B. An older sibling
- C. Physician
- D. Legal guardian
- E. The parents
DNR/DNAR orders Explanation: ***The spouse***
- In the absence of a **living will** or **durable power of attorney**, the law typically designates the **spouse** as the primary decision-maker for an incapacitated patient.
- This hierarchy is established to ensure decisions are made by the individual most intimately connected and presumed to understand the patient's wishes.
*An older sibling*
- Siblings are generally further down the **hierarchy of surrogate decision-makers** than a spouse or parents.
- They would typically only be considered if higher-priority family members are unavailable or unwilling to make decisions.
*Physician*
- The physician's role is to provide medical care and guidance, not to make medical decisions for an incapacitated patient when family surrogates are available.
- Physicians only make decisions in **emergency situations** when no surrogate is immediately available and treatment is immediately necessary to save the patient's life or prevent serious harm.
*Legal guardian*
- A legal guardian is usually appointed by a **court** when there is no appropriate family member available or when there is a dispute among family members.
- In this scenario, with a spouse and other close family members present, a legal guardian would not be the first choice.
*The parents*
- While parents are close family members, they are typically considered **secondary to the spouse** in the hierarchy of surrogate decision-makers for an adult patient.
- They would usually only be the decision-makers if the patient were unmarried or the spouse were unavailable.
DNR/DNAR orders US Medical PG Question 5: A 43-year-old woman presents to her primary care physician with complaints of mild shortness of breath and right-sided chest pain for three days. She reports that lately she has had a nagging nonproductive cough and low-grade fevers. On examination, her vital signs are: temperature 99.1 deg F (37.3 deg C), blood pressure is 115/70 mmHg, pulse is 91/min, respirations are 17/min, and oxygen saturation 97% on room air. She is well-appearing, with normal work of breathing, and no leg swelling. She is otherwise healthy, with no prior medical or surgical history, currently taking no medications. The attending has a low suspicion for the most concerning diagnosis and would like to exclude it with a very sensitive though non-specific test. Which of the following should this physician order?
- A. Obtain chest radiograph
- B. Obtain spiral CT chest with IV contrast
- C. Order a lower extremity ultrasound
- D. Order a D-dimer (Correct Answer)
- E. Obtain ventilation-perfusion scan
DNR/DNAR orders Explanation: ***Order a D-dimer***
- The physician has a **low suspicion based on clinical assessment** and wants to **exclude** a concerning diagnosis (likely **pulmonary embolism** or PE) using a **sensitive test**. A negative D-dimer test can effectively rule out PE in patients with a low pre-test probability.
- The D-dimer is a product of **fibrin degradation** and its elevation indicates recent or ongoing **thrombus formation** and lysis. It is highly sensitive for PE but has low specificity.
*Obtain chest radiograph*
- A chest radiograph is often **normal in pulmonary embolism** or may show non-specific findings, making it unsuitable for ruling out PE.
- While useful for diagnosing other conditions like pneumonia or pleural effusions, it is **not sensitive enough to exclude PE**.
*Obtain spiral CT chest with IV contrast*
- A **spiral CT chest with IV contrast (CT pulmonary angiography)** is the gold standard for diagnosing PE, but it is **not a sensitive rule-out test** for low-probability cases.
- It involves **radiation exposure** and **contrast administration**, which are generally avoided if a less invasive, equally effective rule-out test is available for low-risk patients.
*Order a lower extremity ultrasound*
- Lower extremity ultrasound is used to diagnose **deep vein thrombosis (DVT)**, which is a common source of PE.
- While DVT can lead to PE, a negative lower extremity ultrasound **does not rule out PE** itself, as the clot may have already embolized or originated from elsewhere.
*Obtain ventilation-perfusion scan*
- A **ventilation-perfusion (V/Q) scan** is an alternative to CT angiography for diagnosing PE, particularly in patients with contraindications to contrast.
- However, it is **less definitive than CTPA** and is typically used when suspicion for PE is moderate or higher, rather than as a primary rule-out test for low-probability patients.
DNR/DNAR orders US Medical PG Question 6: A psychiatrist receives a call from a patient who expresses thoughts of harming his ex-girlfriend. The patient describes a detailed plan to attack her at her workplace. Which of the following represents the psychiatrist's most appropriate legal obligation?
- A. Warn the ex-girlfriend and notify law enforcement (Correct Answer)
- B. Only notify the patient's family
- C. Warn only law enforcement
- D. Maintain patient confidentiality
DNR/DNAR orders Explanation: ***Warn the ex-girlfriend and notify law enforcement***
- This scenario directly triggers the **"duty to warn"** and **"duty to protect"** principles, primarily stemming from the **Tarasoff v. Regents of the University of California** case.
- The psychiatrist has a legal obligation to take reasonable steps to protect the identifiable victim, which includes directly warning the intended victim and informing law enforcement.
*Only notify the patient's family*
- Notifying the patient's family alone does not fulfill the **legal obligation to protect** an identifiable third party from a serious threat of harm.
- While family involvement might be part of a comprehensive safety plan, it is insufficient as the sole action in this critical situation.
*Warn only law enforcement*
- While notifying law enforcement is a crucial step, the **Tarasoff duty** specifically mandates warning the **intended victim** directly (or those who can reasonably be expected to notify the victim).
- Relying solely on law enforcement might not ensure the immediate safety of the ex-girlfriend, especially if there's a delay in their response or ability to locate her.
*Maintain patient confidentiality*
- Patient confidentiality is a cornerstone of psychiatric practice, but it is **not absolute** when there is a serious and imminent threat of harm to an identifiable individual.
- The **duty to protect** a potential victim *outweighs* the duty to maintain confidentiality in such extreme circumstances.
DNR/DNAR orders US Medical PG Question 7: A 68-year-old woman was recently diagnosed with pancreatic cancer. At what point should her physician initiate a discussion with her regarding advance directive planning?
- A. Once she enters hospice
- B. Now that she is ill, speaking about advance directives is no longer an option
- C. Only if her curative surgical and medical treatment fails
- D. Only if she initiates the conversation
- E. At this visit (Correct Answer)
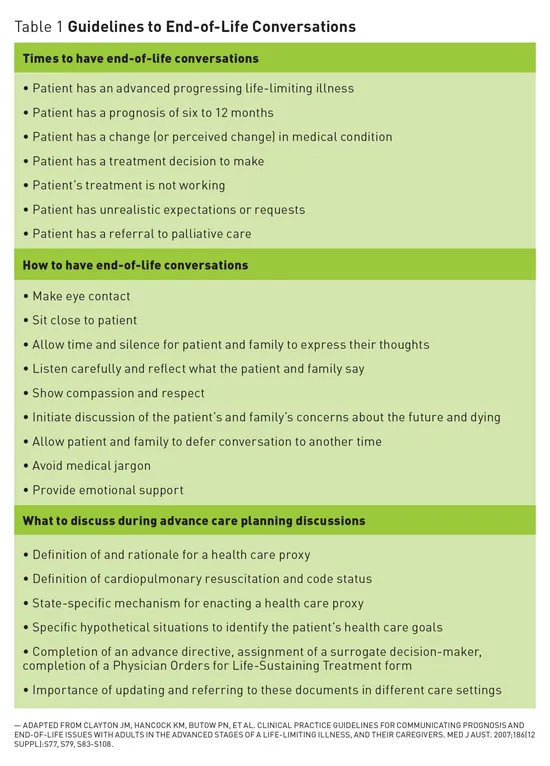
DNR/DNAR orders Explanation: ***At this visit***
- Advance care planning should ideally be initiated as soon as a **serious illness** like pancreatic cancer is diagnosed, while the patient still has the capacity to make informed decisions.
- This allows the patient to clearly state their **wishes** for future medical care and designate a **surrogate decision-maker**.
*Once she enters hospice*
- Delaying discussions until hospice care often means the patient's condition has significantly deteriorated, potentially impacting their ability to actively participate in **decision-making**.
- While advance directives are crucial for hospice patients, starting earlier ensures their preferences guide all stages of their care, not just the end-of-life phase.
*Now that she is ill, speaking about advance directives is no longer an option*
- This statement is incorrect as illness is often the **catalyst** for initiating advance care planning, not a barrier.
- Patients often appreciate the opportunity to discuss their wishes, especially when facing a serious diagnosis, to maintain a sense of **control** and ensure their autonomy.
*Only if her curative surgical and medical treatment fails*
- Waiting until treatment failure is too late as the patient's condition may have worsened to a point where they are no longer able to engage in **meaningful discussions** or have decreased mental capacity.
- Advance care planning is about preparing for potential future scenarios, not just reacting to immediate failures; it provides a framework for care regardless of **treatment outcomes**.
*Only if she initiates the conversation*
- While patient initiation is ideal, it is the physician's responsibility to bring up these important discussions, especially with a new diagnosis of a serious illness like **pancreatic cancer**.
- Many patients may not know about advance directives or feel comfortable initiating such a sensitive conversation, so the physician should proactively offer the **opportunity**.
DNR/DNAR orders US Medical PG Question 8: A terminally ill patient with advanced cancer requests that no resuscitation be performed in the event of cardiac arrest. The patient is mentally competent and has completed advance directives. A family member later demands full resuscitation efforts. Which of the following is the most appropriate response?
- A. Honor the patient's DNR (Correct Answer)
- B. Obtain court order
- C. Follow the family's wishes
- D. Consult ethics committee
DNR/DNAR orders Explanation: ***Honor the patient's DNR***
- The patient is **mentally competent** and has legally documented their wishes through **advance directives** (DNR), which must be respected.
- A competent patient's right to **autonomy** in making decisions about their medical care takes precedence over the wishes of family members.
*Obtain court order*
- Seeking a court order is **unnecessary** and **inappropriate** when a competent patient's wishes are clearly documented in advance directives.
- This option would cause **undue delay** and legal entanglement, potentially going against the patient's immediate medical needs and preferences.
*Follow the family's wishes*
- Following the family's wishes would **override the patient's autonomy** and legally binding advance directives.
- The family's emotional distress does not negate the patient's right to determine their own medical care, especially when they are competent.
*Consult ethics committee*
- While an ethics committee can be helpful in complex cases with **unclear directives** or patient capacity issues, it's not the first step here.
- The patient's competence and clear advance directives make the decision straightforward; a committee consultation could cause delay and unnecessary burden.
DNR/DNAR orders US Medical PG Question 9: A 23-year-old woman presents to the emergency department with acute alcohol intoxication. Her blood alcohol level is 280 mg/dL. She becomes increasingly agitated and attempts to leave against medical advice. Which of the following determines her capacity to refuse treatment?
- A. Age of the patient
- B. Family's wishes
- C. Blood alcohol level
- D. Understanding of risks and benefits (Correct Answer)
DNR/DNAR orders Explanation: ***Understanding of risks and benefits***
- A patient's capacity to refuse treatment is primarily determined by their **ability to understand the nature of their condition**, the proposed treatment, and the **potential risks and benefits** of both accepting and refusing treatment.
- Even with intoxication, if a patient can demonstrate this understanding, they technically have the capacity to make decisions, though the intoxication itself often impairs this ability.
- Capacity assessment includes four key elements: understanding information, appreciating how it applies to their situation, reasoning through options, and communicating a choice.
*Age of the patient*
- While age is a factor in pediatric care (requiring parental consent for minors), for adults, it does not solely determine capacity; an adult of any age can be deemed to lack capacity for various reasons.
- The patient's age (23 years old) indicates she is legally an adult, but it does not automatically confer or deny treatment capacity, which is assessed based on mental status.
*Family's wishes*
- Family wishes are important for patients who **lack decision-making capacity** and have no advance directives, but they do not override the decisions of a fully capacitated patient.
- In situations where capacity is questionable, family input might be considered, but the direct assessment of the patient's understanding remains paramount.
*Blood alcohol level*
- A high blood alcohol level strongly suggests impaired judgment and cognitive function, making it a red flag for potential lack of capacity, but it is not a direct measure of capacity itself.
- Some individuals may maintain a degree of understanding even with high levels, so a direct assessment of their comprehension is still necessary, not just assuming based on the level alone.
DNR/DNAR orders US Medical PG Question 10: A 32-year-old woman is brought to the emergency department by her husband because of an episode of hematemesis 2 hours ago. She has had dyspepsia for 2 years. Her medications include occasional ibuprofen for headaches. After initial stabilization, the risks and benefits of upper endoscopy and alternative treatments, including no therapy, are explained thoroughly. She shows a good understanding of her condition and an appreciation of endoscopic treatment and its complications. She decides that she wants to have an endoscopy to find the source of bleeding and appropriately manage the ulcer. Her medical records show advance directives that she signed 3 years ago; her sister, who is a nurse, has a durable power of attorney. Regarding obtaining informed consent, which of the following is the most accurate conclusion for providing endoscopic treatment for this patient?
- A. There are reasons to believe that she may not have decision-making capacity
- B. Endoscopic treatment may be performed without further action
- C. Her sister must sign the consent form
- D. Documentation of her decision prior to treatment is required (Correct Answer)
- E. Her decision to have an endoscopy is not voluntary
DNR/DNAR orders Explanation: **Documentation of her decision prior to treatment is required**
- The patient has been fully informed, understands her condition, and has expressed a clear desire for the procedure, demonstrating **decision-making capacity**.
- To ensure ethical and legal compliance, her **informed consent** must be accurately documented in her medical record before any invasive treatment, including endoscopy, is performed.
*There are reasons to believe that she may not have decision-making capacity*
- The patient has clearly demonstrated **understanding of her condition, treatment options, and potential complications**, which indicates preserved decision-making capacity.
- Despite the acute medical situation, her ability to articulate her preference after a thorough discussion confirms her competence for informed consent.
*Endoscopic treatment may be performed without further action*
- While the patient has consented verbally, this does not negate the need for proper **documentation of informed consent** before initiating the procedure.
- Legally and ethically, a verbal agreement alone is insufficient; a signed consent form or detailed chart note confirming her understanding and decision is essential.
*Her sister must sign the consent form*
- Her sister, holding a **durable power of attorney**, would only be authorized to make medical decisions if the patient were deemed to lack **decision-making capacity**.
- Since the patient clearly demonstrates the ability to make her own medical decisions, her sister's consent is not required and would override the patient's autonomy.
*Her decision to have an endoscopy is not voluntary*
- The scenario explicitly states that the risks and benefits were **thoroughly explained**, and she shows a "good understanding" and "appreciation of endoscopic treatment."
- Her decision to "want to have an endoscopy" despite knowing the alternatives suggests a **voluntary and informed choice**, not coercion.
More DNR/DNAR orders US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.