Soft tissue tumors US Medical PG Practice Questions and MCQs
Practice US Medical PG questions for Soft tissue tumors. These multiple choice questions (MCQs) cover important concepts and help you prepare for your exams.
Soft tissue tumors US Medical PG Question 1: An 11-year-old boy presents to your clinic after 4 months of pain and swelling in his thigh. His mother states that at first she thought his condition was due to roughhousing, but it hasn’t gone away and now she’s concerned. You perform an X-ray that shows an ‘onion skin’ appearance on the diaphysis of the femur. You are concerned about a malignancy, so you perform a PET scan that reveals lung nodules. Which of the following is most associated with this disease?
- A. Defective mitochondrial DNA
- B. Nonsense mutation to DMD gene
- C. t(11;22) translocation (Correct Answer)
- D. t(9;22) translocation
- E. Rb loss of function mutation
Soft tissue tumors Explanation: ***t(11;22) translocation***
- The clinical presentation, including the age of the patient (11-year-old boy), pain and swelling in the thigh, and the characteristic **"onion skin" appearance** on X-ray, are highly suggestive of **Ewing sarcoma**
- **Ewing sarcoma** is strongly associated with the **t(11;22) chromosomal translocation**, leading to the fusion of the **EWSR1 and FLI1 genes**
- This translocation is found in approximately **85-90% of Ewing sarcoma cases** and is the molecular hallmark of this aggressive pediatric bone malignancy
*Defective mitochondrial DNA*
- This is associated with mitochondrial disorders, which typically present with myopathies, encephalopathies, and other systemic issues, not bone tumors with an "onion skin" appearance
- While sometimes involved in cancer pathogenesis, defective mitochondrial DNA is not the primary genetic hallmark of Ewing sarcoma
*Nonsense mutation to DMD gene*
- A nonsense mutation in the **DMD gene** causes **Duchenne muscular dystrophy**, a genetic disorder characterized by progressive muscle weakness and degeneration
- This condition does not present with bone tumors, thigh pain from malignancy, or an "onion skin" periosteal reaction
*t(9;22) translocation*
- The **t(9;22) translocation**, also known as the **Philadelphia chromosome**, is characteristic of **chronic myeloid leukemia (CML)** and some cases of acute lymphoblastic leukemia (ALL)
- This genetic abnormality is associated with hematologic malignancies, not bone sarcomas like Ewing sarcoma
*Rb loss of function mutation*
- A loss-of-function mutation in the **Rb (retinoblastoma) gene** is associated with **retinoblastoma** and an increased risk of other cancers such as osteosarcoma and small cell lung cancer
- While osteosarcoma is a bone tumor, it typically presents with a "sunburst" or Codman's triangle appearance on X-ray, not the "onion skin" appearance seen in Ewing sarcoma
Soft tissue tumors US Medical PG Question 2: An 82-year-old woman presents to the emergency department because of excruciating right flank pain and fever for the past 2 days. She states that she is having trouble urinating. Her past medical history is unremarkable. A urinalysis is performed and comes back positive for leukocytes and gram-negative bacilli. A contrast computed tomography of the abdomen is performed and reveals a large retroperitoneal mass compressing the right ureter, leading to hydronephrosis of the right kidney. The mass is excised. Histopathologic evaluation of the mass is shown in the image below, and it is determined to be malignant. Which of the following is the most likely diagnosis in this patient?
- A. Rhabdomyosarcoma
- B. Leiomyosarcoma
- C. Lipoma
- D. Teratoma
- E. Liposarcoma (Correct Answer)
Soft tissue tumors Explanation: ***Liposarcoma***
- The **most common primary malignant retroperitoneal tumor** in adults, particularly in elderly patients
- Characteristically presents as a **large retroperitoneal mass** causing compressive symptoms such as hydronephrosis
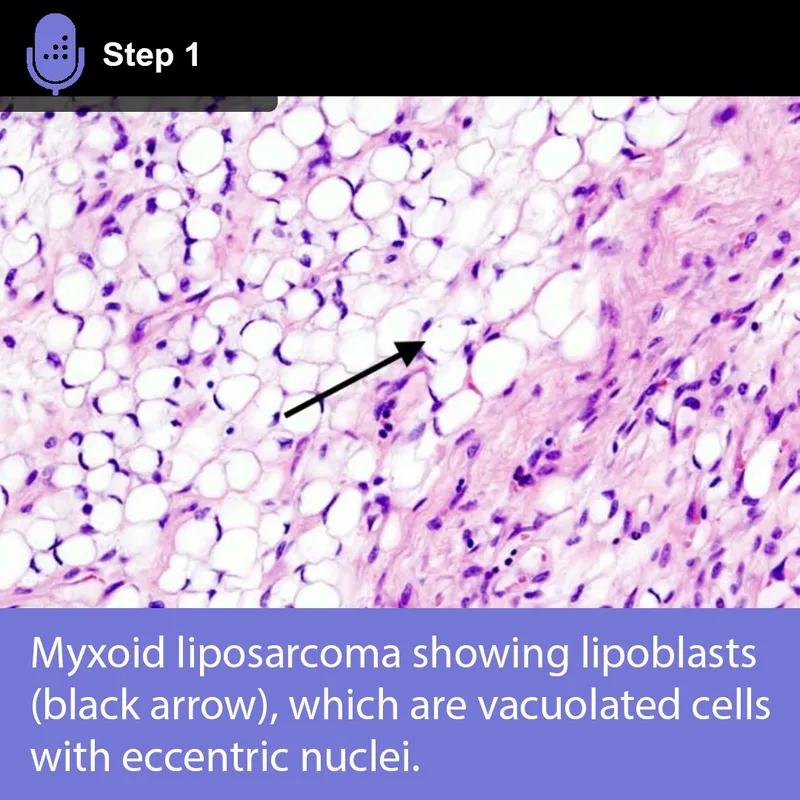
- **Histopathological features** include pleomorphic lipoblasts with varying degrees of differentiation (well-differentiated, dedifferentiated, myxoid, or pleomorphic subtypes)
- The clinical presentation of an elderly patient with a malignant retroperitoneal mass strongly suggests this diagnosis
*Rhabdomyosarcoma*
- Primarily a **pediatric malignancy**, most common in children and young adults under 20 years old
- Most frequently arises in the **head and neck, genitourinary tract, or extremities**, not typically retroperitoneal
- Histologically shows skeletal muscle differentiation with rhabdomyoblasts, not lipoblastic features
*Leiomyosarcoma*
- More commonly found in the **uterus, gastrointestinal tract, or blood vessels**
- While it can occur in the retroperitoneum, it is **less common** than liposarcoma in this location
- Histologically demonstrates **smooth muscle differentiation** with spindle cells, not the lipoblastic features characteristic of the described mass
*Lipoma*
- A **benign tumor** composed of mature adipose tissue without cellular atypia
- Would not present as a **malignant mass** on histopathologic evaluation
- Generally asymptomatic and slow-growing; unlikely to cause severe symptoms like excruciating pain or obstructive hydronephrosis
*Teratoma*
- Contains tissue derived from **all three germ layers** (ectoderm, mesoderm, endoderm)
- More commonly associated with **gonadal or midline structures** (ovaries, testes, mediastinum)
- Rare in the retroperitoneum in elderly patients; histology would show diverse tissue types rather than predominantly lipoblastic features
Soft tissue tumors US Medical PG Question 3: A 14-year-old boy presents as a new patient to your practice. While conducting your physical exam, you observe the findings depicted in Figures A and B. Which of the following additional findings would most likely be found in this patient?
- A. Multiple café-au-lait macules (Correct Answer)
- B. A white tuft of scalp hair since birth
- C. The presence of ash-leaf spots
- D. Facial angiofibromas
- E. A family history of seizures and intellectual disability
Soft tissue tumors Explanation: ***Multiple café-au-lait macules***
- The images show **Lisch nodules** (iris hamartomas), which are pathognomonic for **Neurofibromatosis type 1 (NF1)**.
- **Café-au-lait macules** are the most common and often earliest manifestation of NF1, present in **>99% of patients**.
- Diagnostic criteria require **≥6 café-au-lait macules** (>5mm in diameter prepubertal, >15mm postpubertal).
- This is the **most likely additional finding** in a patient with Lisch nodules.
*A family history of seizures and intellectual disability*
- While **learning disabilities** occur in ~50% of NF1 patients and **seizures** can occur, this is not the most specific or common finding.
- **Café-au-lait macules** and **cutaneous neurofibromas** are far more consistent and diagnostically significant.
*A white tuft of scalp hair since birth*
- A **white tuft of scalp hair** (poliosis) is characteristic of **Waardenburg syndrome**, not NF1.
- Waardenburg syndrome presents with **hearing loss**, **heterochromia iridis**, and **dystopia canthorum**.
*The presence of ash-leaf spots*
- **Ash-leaf spots** (hypopigmented macules) are a hallmark of **Tuberous Sclerosis Complex (TSC)**.
- TSC has different ocular findings like **retinal hamartomas**, not Lisch nodules.
*Facial angiofibromas*
- **Facial angiofibromas** (adenoma sebaceum) are a classic manifestation of **Tuberous Sclerosis Complex (TSC)**, not NF1.
- NF1 typically presents with **cutaneous and plexiform neurofibromas**, not angiofibromas.
Soft tissue tumors US Medical PG Question 4: A 50-year-old man comes to the physician for a routine checkup. He has had a progressively increasing swelling on the nape of his neck for 2 months. He does not have a fever or any discharge from the swelling. He underwent a colectomy for colon cancer at the age of 43 years. He has type 2 diabetes mellitus, hypertension, and osteoarthritis of the left knee. Current medications include insulin glargine, metformin, enalapril, and naproxen. He has worked as a traffic warden for the past 6 years and frequently plays golf. He appears healthy. His temperature is 37.3°C (99.1°F), pulse is 88/min, and blood pressure is 130/86 mm Hg. Examination of the neck shows a 2.5-cm (1-in) firm, mobile, and painless nodule. The skin over the nodule cannot be pinched. The lungs are clear to auscultation. The remainder of the examination shows no abnormalities. A photograph of the lesion is shown. Which of the following is the most likely diagnosis?
- A. Dermatofibroma
- B. Actinic keratosis
- C. Squamous cell carcinoma
- D. Lipoma
- E. Epidermoid cyst (Correct Answer)
Soft tissue tumors Explanation: ***Epidermoid cyst***
- The **inability to pinch the skin over the nodule** is the key diagnostic feature (positive Fothergill sign), indicating the lesion is attached to the overlying skin—characteristic of an **epidermoid cyst**
- Epidermoid cysts present as **firm, mobile, painless nodules** that grow slowly over weeks to months
- The **nape of the neck** is a common location for these benign cysts originating from the epidermal layer
- Absence of fever, discharge, or inflammation indicates an uninfected, benign lesion
*Dermatofibroma*
- Typically presents as a small, **reddish-brown papule** that demonstrates a **"dimple sign"** when the skin is pinched (opposite of this patient's finding)
- Usually smaller than the described 2.5-cm nodule
- The positive Fothergill sign (cannot pinch skin) excludes this diagnosis
*Actinic keratosis*
- Presents as a **rough, scaly patch** with sandpaper-like texture on sun-exposed skin, not a smooth nodule
- Precancerous lesion that does not present as a firm, mobile subcutaneous mass
- Would not produce the inability to pinch skin over the lesion
*Squamous cell carcinoma*
- Usually presents as a **firm nodule with ulceration, crusting, or central depression** that grows more rapidly
- Often fixed or indurated rather than mobile
- The benign clinical features (mobile, painless, no ulceration, slow growth) make this unlikely
*Lipoma*
- Benign tumor of fatty tissue that is characteristically **soft and rubbery**, not firm
- Typically shows **easily mobile skin over the lesion** (negative Fothergill sign)
- The firm consistency and inability to pinch skin exclude this diagnosis
Soft tissue tumors US Medical PG Question 5: A 24-year-old woman with a past medical history significant only for endometriosis presents to the outpatient clinic with a 2-cm left breast mass that she first identified 6 months earlier. On review of systems, the patient states that the mass is not painful and, by her estimation, has not significantly increased in size since she first noticed it. On physical examination, there is a palpable, round, rubbery, mobile mass approximately 2 cm in diameter. Given the lesion’s characteristics and the patient’s demographics, what is the most likely diagnosis?
- A. Fibrocystic change
- B. Invasive breast carcinoma
- C. Fibroadenoma (Correct Answer)
- D. Phyllodes tumor
- E. Ductal carcinoma in situ
Soft tissue tumors Explanation: ***Fibroadenoma***
- This diagnosis is supported by the patient's age (young woman), the **rubbery, mobile, well-circumscribed** nature of the mass, and its slow growth over 6 months without pain.
- Fibroadenomas are **benign tumors** made of both fibrous and glandular tissue, and their characteristics typically match this presentation.
*Fibrocystic change*
- While common in young women, fibrocystic changes often manifest as **multiple cysts**, generalized breast tenderness, or cyclical pain related to menstruation.
- The description of a single, non-tender, rubbery mass is less typical for fibrocystic changes.
*Invasive breast carcinoma*
- Though possible, **invasive breast cancer** in a 24-year-old woman is less common, and typically presents with a **hard, irregular, fixed mass** that may be painful or associated with skin changes.
- The description of a **rubbery, mobile** lesion not significantly increasing in size makes this less likely.
*Phyllodes tumor*
- This tumor is characterized by **rapid growth** and often reaches a large size, which is not consistent with the patient's report of slow growth over 6 months.
- While it can be benign, borderline, or malignant, its typical presentation is **faster-growing** than described.
*Ductal carcinoma in situ*
- **Ductal carcinoma in situ (DCIS)** is a non-invasive form of breast cancer that usually presents as **microcalcifications on mammography** and is often non-palpable.
- When palpable, it is typically a poorly defined lump, not a rubbery, mobile, well-circumscribed mass.
Soft tissue tumors US Medical PG Question 6: A 24-year-old man comes to the physician because of 2 episodes of bleeding from the rectum over the past month. The patient’s father died of colon cancer at the age of 42. The patient has no history of any serious illness and takes no medications. He does not smoke. His vital signs are within normal limits. Physical examination shows a small hard mass over the right mandible that is nontender and fixed to the underlying bone. A similarly hard and painless 5 × 5 mass is palpated over the rectus abdominis muscle. On examination of the rectum, a polypoid mass is palpated at fingertip. Proctosigmoidoscopy shows numerous polyps. Which of the following best explains these findings?
- A. Familial polyposis of the colon
- B. Peutz-Jeghers syndrome
- C. Turcot’s syndrome
- D. Gardner’s syndrome (Correct Answer)
- E. Lynch’s syndrome
Soft tissue tumors Explanation: ***Gardner's syndrome***
- This syndrome is a variant of **familial adenomatous polyposis (FAP)**, characterized by numerous **colonic polyps** (leading to rectal bleeding) in conjunction with **extra-intestinal manifestations**.
- The extra-intestinal features described, such as **osteomas** (small hard mass over the mandible) and **desmoid tumors** (painless 5 × 5 mass over the rectus abdominis muscle), are classic findings of Gardner's syndrome. The family history of colon cancer further supports this diagnosis.
*Familial polyposis of the colon*
- Familial adenomatous polyposis (FAP) primarily involves the development of **hundreds to thousands of adenomatous colonic polyps**, leading to a high risk of colorectal cancer.
- While it explains the rectal polyps and family history, it does **not account for the extra-intestinal manifestations** like osteomas and desmoid tumors, which are key to Gardner's syndrome.
*Peutz-Jeghers syndrome*
- This syndrome is characterized by **hamartomatous polyps** throughout the gastrointestinal tract and **mucocutaneous hyperpigmentation** (dark spots) on the lips, buccal mucosa, and digits.
- The patient's presentation does not include hamartomatous polyps or mucocutaneous pigmentation.
*Turcot's syndrome*
- Turcot's syndrome is a rare condition involving the co-occurrence of **colorectal polyps** (often adenomatous) and **central nervous system (CNS) tumors**, such as medulloblastoma or glioblastoma.
- The patient presents with osteomas and desmoid tumors, which are not CNS manifestations central to Turcot's syndrome.
*Lynch's syndrome*
- Lynch syndrome (hereditary nonpolyposis colorectal cancer, HNPCC) is characterized by an increased risk of developing **colorectal cancer** and other cancers (e.g., endometrial, ovarian) due to defects in **DNA mismatch repair genes**.
- It typically involves fewer polyps than FAP and does not present with the specific extra-intestinal symptoms like osteomas or desmoid tumors seen in this patient.
Soft tissue tumors US Medical PG Question 7: A 67-year-old man presents with pain in both legs. He says the pain is intermittent in nature and has been present for approximately 6 months. The pain increases with walking, especially downhill, and prolonged standing. It is relieved by lying down and leaning forward. Past medical history is significant for type 2 diabetes mellitus, hypercholesterolemia, and osteoarthritis. The patient reports a 56-pack-year history but denies any alcohol or recreational drug use. His vital signs include: blood pressure 142/88 mm Hg, pulse 88/min, respiratory rate 14/min, temperature 37°C (98.6°F). On physical examination, the patient is alert and oriented. Muscle strength is 5/5 in his upper and lower extremities bilaterally. Babinski and Romberg tests are negative. Pulses measure 2+ in upper and lower extremities bilaterally. Which of the following is the next best step in the management of this patient?
- A. MRI of the spine (Correct Answer)
- B. CT angiography of the lower extremities
- C. Ankle-brachial index
- D. Cilostazol
- E. Epidural corticosteroid injection
Soft tissue tumors Explanation: ***MRI of the spine***
- The patient's symptoms of **intermittent leg pain worsened by walking (especially downhill) and prolonged standing**, and **relieved by lying down and leaning forward**, are highly classic for **neurogenic claudication** due to **lumbar spinal stenosis**.
- An **MRI of the spine** is the *gold standard* for diagnosing spinal stenosis, clearly visualizing nerve root compression and the degree of canal narrowing.
*CT angiography of the lower extremities*
- This imaging is used to assess **peripheral artery disease** (PAD) but the patient's symptoms are inconsistent with vascular claudication.
- **Vascular claudication** typically improves with rest, not with specific postures like leaning forward.
*Ankle-brachial index*
- The **ankle-brachial index (ABI)** is a non-invasive test to screen for **peripheral artery disease (PAD)**.
- While the patient has risk factors for PAD (diabetes, hypercholesterolemia, smoking), his symptoms are classic for neurogenic claudication, and his **2+ pulses** in the lower extremities make PAD less likely.
*Cilostazol*
- **Cilostazol** is a phosphodiesterase inhibitor used to treat symptoms of **intermittent claudication** caused by **peripheral artery disease (PAD)**.
- Since the patient's symptoms are more consistent with neurogenic claudication rather than vascular claudication, cilostazol would not be the appropriate initial step.
*Epidural corticosteroid injection*
- An **epidural corticosteroid injection** is a treatment option for symptomatic spinal stenosis but is not the *initial diagnostic step*.
- Diagnosis with an **MRI** is necessary before considering targeted therapeutic interventions like injections.
Soft tissue tumors US Medical PG Question 8: A 36-year-old man is seen in the emergency department for back pain that has been getting progressively worse over the last 4 days. Upon further questioning, he also notes that he has been having a tingling and burning sensation rising up from his feet to his knees bilaterally. The patient states he is having difficulty urinating and having bowel movements over the last several days. His temperature is 97.4°F (36.3°C), blood pressure is 122/80 mmHg, pulse is 85/min, respirations are 14/min, and oxygen saturation is 98% on room air. Physical exam is notable for weak leg flexion bilaterally along with decreased anal sphincter tone. Which of the following is the best next step in management?
- A. Emergency surgery
- B. CT
- C. Pulmonary function tests
- D. Lumbar puncture
- E. MRI (Correct Answer)
Soft tissue tumors Explanation: ***MRI***
- The patient's symptoms (back pain, ascending paresthesias, bladder/bowel dysfunction, and decreased anal sphincter tone) are highly suggestive of **cauda equina syndrome**. An **MRI of the spine** is the gold standard for diagnosing this condition, as it can visualize the spinal cord and nerve roots directly.
- Early diagnosis and intervention with MRI are crucial to prevent **permanent neurological deficits** in cauda equina syndrome.
*Emergency surgery*
- While emergency surgery might be the next step *after* diagnosis, it is **not the initial diagnostic step**. The cause of the cauda equina syndrome (e.g., disc herniation, tumor) must first be identified.
- Performing surgery without proper imaging could lead to operating on the wrong level or for the wrong pathology.
*CT*
- A **CT scan** can provide information about bony structures but is generally **inferior to MRI** for visualizing soft tissue structures like the spinal cord, nerve roots, and intervertebral discs, which are critical in cauda equina syndrome.
- It may miss subtle compressions or pathologies of the nerve roots.
*Pulmonary function tests*
- **Pulmonary function tests** are used to assess lung function and are **irrelevant** to the patient's acute neurological symptoms and back pain.
- This test would not provide any diagnostic information for suspected cauda equina syndrome.
*Lumbar puncture*
- A **lumbar puncture** is primarily used to analyze cerebrospinal fluid for conditions like infection or inflammation (e.g., meningitis, Guillain-Barré syndrome).
- While Guillain-Barré can cause ascending paralysis, the prominent back pain, bowel/bladder dysfunction, and decreased anal sphincter tone make **cauda equina syndrome** a more likely diagnosis, for which LP is not the primary diagnostic tool.
Soft tissue tumors US Medical PG Question 9: A 33-year-old man presents to his primary care physician with shoulder pain. He states that he can't remember a specific instance when the injury occurred. He is a weight lifter and competes in martial arts. The patient has no past medical history and is currently taking a multivitamin. Physical exam demonstrates pain with abduction of the patient's right shoulder and with external rotation of the right arm. There is subacromial tenderness with palpation. His left arm demonstrates 10/10 strength with abduction as compared to 4/10 strength with abduction of the right arm. Which of the following best confirms the underlying diagnosis?
- A. Ultrasound
- B. Radiography
- C. MRI (Correct Answer)
- D. CT
- E. Physical exam and history
Soft tissue tumors Explanation: ***MRI***
- An **MRI is the gold standard** for diagnosing soft tissue injuries of the shoulder, including **rotator cuff pathology**, which is highly suspected given the patient's symptoms (pain with abduction and external rotation, subacromial tenderness, and weakness).
- It provides detailed imaging of tendons, ligaments, and cartilage, allowing for precise identification of **tears, inflammation, or impingement**.
*Ultrasound*
- While ultrasound can assess **rotator cuff integrity** and identify fluid collections, it is highly operator-dependent and may not provide the same level of detail as MRI for complex tears or associated pathologies.
- It can be a good initial screening tool but might **underestimate the extent** of an injury compared to MRI.
*Radiography*
- **Radiography (X-rays)** primarily visualizes bone structures and would be useful for detecting fractures, dislocations, or significant degenerative joint disease.
- It would **not directly visualize** the soft tissue injuries of the rotator cuff or other tendons that are likely causing this patient's symptoms.
*CT*
- **CT scans** provide excellent detail of bone structures and can identify subtle fractures, erosions, or bony impingement.
- However, like X-rays, they are **less effective for visualizing soft tissues** like tendons and ligaments compared to MRI.
*Physical exam and history*
- The **physical exam and history** are crucial for narrowing down the differential diagnosis and guiding further imaging.
- While strongly suggestive of a rotator cuff injury, they alone **cannot definitively confirm the extent or nature** of the underlying soft tissue pathology.
Soft tissue tumors US Medical PG Question 10: A 43-year-old man is brought to the emergency department 40 minutes after falling off a 10-foot ladder. He has severe pain and swelling of his right ankle and is unable to walk. He did not lose consciousness after the fall. He has no nausea. He appears uncomfortable. His temperature is 37°C (98.6°F), pulse is 98/min, respirations are 16/min, and blood pressure is 110/80 mm Hg. He is alert and oriented to person, place, and time. Examination shows multiple abrasions over both lower extremities. There is swelling and tenderness of the right ankle; range of motion is limited by pain. The remainder of the examination shows no abnormalities. An x-ray of the ankle shows an extra-articular calcaneal fracture. Intravenous analgesia is administered. Which of the following is the most appropriate next step in the management of this patient?
- A. Short leg splint and orthopedic consultation
- B. Broad-spectrum antibiotic therapy
- C. MRI of the right ankle
- D. Open reduction and internal fixation
- E. X-ray of the spine (Correct Answer)
Soft tissue tumors Explanation: ***X-ray of the spine***
- A **high-energy calcaneal fracture** (especially from a fall from height) is often associated with other injuries, particularly to the **spine**, due to axial loading.
- Approximately **10% of calcaneal fractures** are associated with **lumbar spine compression fractures**, making imaging of the spine an essential next step to rule out this potentially serious concomitant injury.
*Short leg splint and orthopedic consultation*
- While a **short leg splint** is appropriate for initial immobilization and pain control of the ankle fracture, and **orthopedic consultation** is necessary, these steps do not address the immediate need to exclude other critical injuries like spinal fractures in high-impact trauma.
- This option represents definitive management of the ankle rather than comprehensive early trauma assessment in a high-risk patient.
*Broad-spectrum antibiotic therapy*
- **Antibiotic therapy** is primarily indicated for **open fractures** to prevent infection, or in cases of significant soft tissue injury with high contamination risk; the provided information describes an extra-articular fracture with abrasions, but not explicitly an open fracture requiring immediate broad-spectrum antibiotics.
- The focus should first be on skeletal integrity elsewhere and definitive fracture management rather than presumptive infection prevention unless an open fracture is confirmed.
*MRI of the right ankle*
- While an **MRI** can provide detailed imaging of soft tissues, ligaments, and cartilage, and may be useful later for surgical planning or to assess subtle injuries, a plain **X-ray has already confirmed a calcaneal fracture**.
- The immediate priority after a high-energy trauma is to rule out other significant, potentially disabling or life-threatening bony injuries, particularly to the spine, rather than further detailed imaging of the already-identified ankle fracture.
*Open reduction and internal fixation*
- **Open reduction and internal fixation (ORIF)** is a surgical procedure for definitive management of certain fractures; however, it is not the **immediate next step** in the emergency department for initial patient assessment following trauma.
- Before surgical intervention, a comprehensive assessment to rule out other injuries (especially spinal fractures) and to thoroughly plan the specific surgical approach is required.
More Soft tissue tumors US Medical PG questions available in the OnCourse app. Practice MCQs, flashcards, and get detailed explanations.